Lung Cancer Awareness Month:
The White Ribbon Project
Anne LaPorte
From Nurse to Caregiver to Patient
Story 7 of The White Ribbon Project Stories
Anne was a nurse for 35 years, spending many of those years tending to patients in the Kaiser healthcare system. She was following in her mother’s footsteps as a registered nurse.
But in 2008, she was forced to go from professional to personal caregiver.

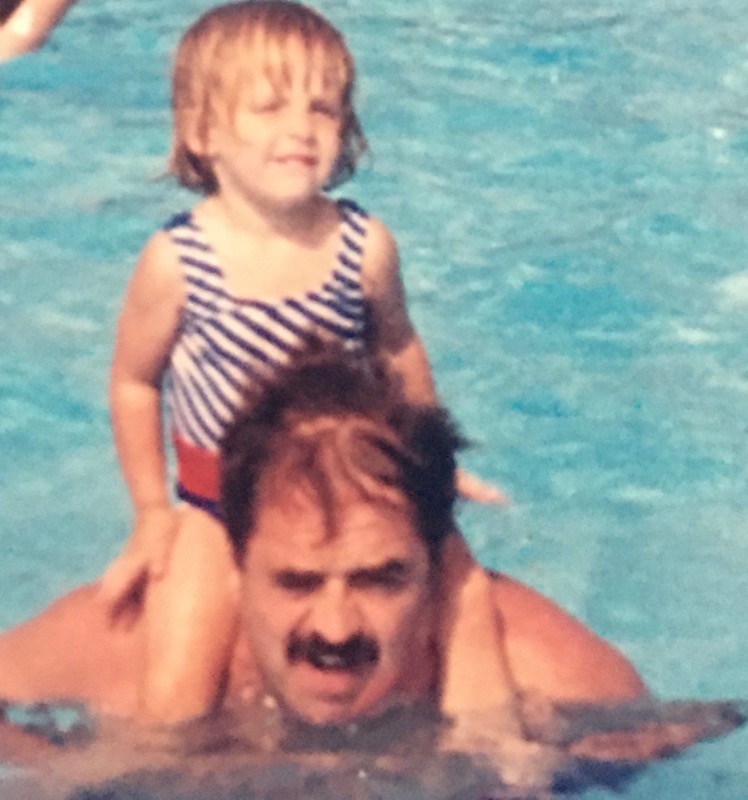
“My father was diagnosed with very advanced lung cancer,” says Anne. “After two rounds of chemotherapy, he had so much swelling and bleeding within his lungs that at the time we opted to move him to hospice so he would have a more peaceful death.”
She and her family decided to gather to try and help him with treatment decisions. Unfortunately, the disease was progressing too quickly.
“Two days before my father passed, I remember sitting on the porch, reminiscing. And he was happy and grateful. No regrets. We were a big, jovial family. And I think, you know, he was grateful that we were all home.”
After her father passed, Anne devoted herself to lung cancer advocacy. She says she threw herself into fundraising for more research, to help others that would be diagnosed with lung cancer after her dad.
“We became very active in the lung cancer community because there were so few options at that time for my father, and he suffered horrifically during those eight weeks from the treatment options that were available,” describes Anne. “I was shocked by what I was learning about lung cancer, how poorly funded it is, how the stigma associated with smoking has limited the amount of research funding it gets.”
As Anne fundraised and fought for more lung cancer awareness, she was hit hard by cancer again. This time, it was her 25-year-old daughter, Brooke.
“My daughter was diagnosed with Stage 4 Hodgkin lymphoma that had metastasized to her right lung,” Anne recounts, tears in her eyes. “Fortunately, Brooke had classical Hodgkin’s which is very treatable with a chemotherapeutic regimen. I felt she had an outstanding oncologist. So Brooke’s been doing very well. She has been in remission the last four years.”
But as Brooke began to recover, Anne began to feel a lot of pain. In 2019, the symptoms started to get worse and worse.


“I started to have back pain that I attributed to training for triathlons. I was having a little bit more mid-back pain. So I just switched it up a bit. I thought maybe I was running too much and it was the impact, but it was getting worse instead of better,” says Anne. “I waited another month and I started to lose sensation in my legs, and the pain was really severe. So I went to the doctor again.”
And each time, Anne was sent home.
Finally, eight months after her 1st symptoms appeared and still with no answers, she fought for an MRI scan.
“But by the time they did my MRI, I had what they called diffuse metastatic disease. So it was throughout my spine, it was throughout my hips. I already had metastasis to my lymph nodes in my liver. So at that time, they offered me very little treatment options.”
Stage 4 lung cancer, just like her father over 10 years before.

Anne went from professional caregiver to personal caregiver – to her father and then daughter – to becoming a stage 4 cancer patient, herself.
She was given 3 to 6 months to live.
She decided to record video messages to family and friends to break the news.
“I just wanted to be able to say goodbye before I got too sick. You know, I really felt at that time that I was dying and I knew things were moving pretty quickly.”
But the hardest video to record was the one for her daughter, Brooke. In that message, she said:

I don’t want to miss the opportunity to let you know that you’re the light of my life. I feel nothing but grateful. To have such a wonderful daughter and you have far exceeded all of my expectations in every way. But most of all, the way you handled cancer, so you are my best role model and it’s helping me stay strong and courageous.
Anne to Brooke in video message, 2020
Part of that strength and courage drove Anne to fight for genetic testing. She tested positive for the EGFR mutation, which allowed her to skip traditional chemotherapy.
“Next generation sequencing testing looks at the mutations in your tumor because there are so many drugs that have been developed since 2015 that, as you can see, looking at me, I’ve only been taking an oral medication up until five weeks ago. So for the first year, I’ve just been taking a pill a day that’s completely different from my father’s experience.”
For Anne, that experience has been drastically different in terms of quality of life. She was able to skip the infusion center and side effects like hair loss thanks to the EGFR+ specific therapies.
“I’ve had wonderful quality of life because I had this marker. I had this blood test drawn. I didn’t have it drawn up my HMO. I had to fight to have it drawn.”
It wasn’t the first time Anne had to fight for her own life. She says she was ignored every time she brought up her family history with lung cancer.
“I always made sure I mentioned it and was always reassured because I was a non-smoker that I was not at risk,” Anne explains.
The message needs to be anybody with lungs can get lung cancer. There is an urgent and absolute urgent need for greater research. And there’s an absolute urgent need for early detection.
Those are the same messages that The White Ribbon Project has also been trying to spread.
Anne has been supporting the grassroots movement that’s trying to rally everyone in the lung cancer community to unify around their shared experiences.
“Your smoking history is irrelevant. You’re welcome in our community. But we now, I feel, have a voice and I think finally people are listening…I hope this helps move us towards our goal, which is, you know, if not finding a cure or making this into a chronic disease and making people feel loved.”
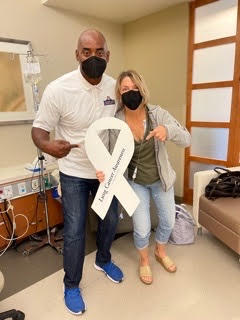
Anne is now in a clinical trial. She’s proof why awareness and funding for research matters in lung cancer. She wants to help push that research forward, in all cancers.
I want to move research as quickly as possible. I don’t know if it may extend my life and I hope it does, but I hope it saves my daughter’s life.
→Back to The White Ribbon Project Stories


Inspired by Anne's story?
Share your story, too!
More non-small cell lung cancer (NSCLC) stories
Stephanie K., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptoms: Persistent and intense cough, general feeling of sluggishness
Treatments: Chemotherapy, targeted therapy through a clinical trial, radiation therapy
Ruchira A., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptoms: Mild intermittent cough while talking, low-grade fever, severe nonstop cough, coughing up blood, collapsed left lung
Treatments: Surgery (lobectomy), targeted therapy
Jennifer M., Lung Cancer, EGFR+, Stage 4 (Metastatic)
Symptoms: None per se; discovered during physical checkup for what seemed to be a sinus infection
Treatments: Radiation therapy (stereotactic body radiation therapy or SBRT), targeted therapy
Dr. Ross Camidge, Non-Small Cell Lung Cancer, Stage 4 (Metastatic)
Symptoms: sore shoulder muscle, breathing sounded different
Laura R., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptoms: Persistent cough, fatigue, bone pain
Treatments: Targeted therapies (tyrosine kinase inhibitors or TKIs, including through a clinical trial)