Lacey’s Chronic Lymphocytic Leukemia Story
Lacey was diagnosed with chronic lymphocytic leukemia, the most common form of leukemia in adults.
She details undergoing chemo, relapsing and going through immunotherapy before remission. Lacey also talks about parenting with cancer, how the diagnosis impacted her marriage and advocating for herself as a patient. Thank you for sharing your story, Lacey!

- Name: Lacey B.
- Diagnosis:
- Chronic lymphocytic leukemia (CLL)
- Non-Hodgkin’s lymphoma subtype
- Staging: N/A
- 1st Symptoms:
- Fatigue
- Elevated WBCs
- Treatment:
- Chemotherapy
- 6 cycles of FCR
- Immunotherapy (plus chemo)
- Veneteoclax + Rituxan
- Venetoclax orally for 2 years
- Rituxan for 6 cycles
- Veneteoclax + Rituxan
- Chemotherapy
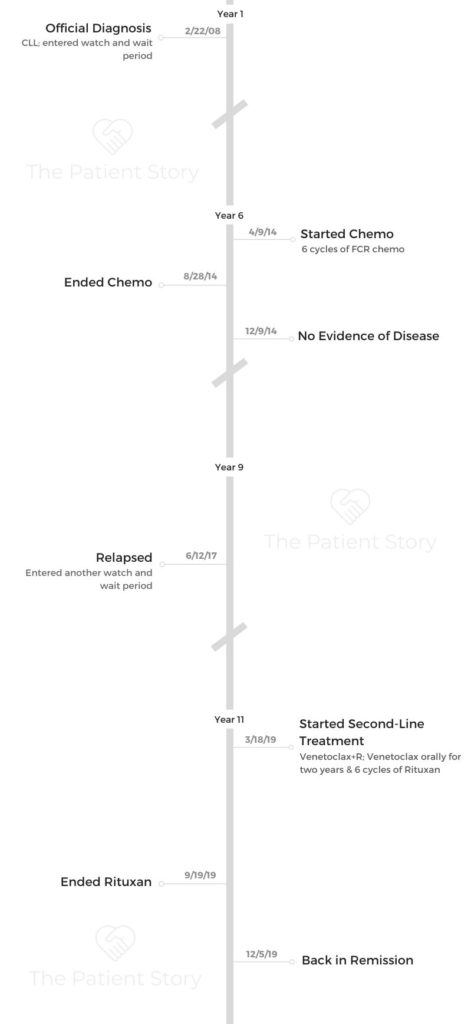
- CLL Diagnosis
- 1st-Line Treatment
- Relapse
- Reflections
- What is your “new normal”?
- How cancer affects your relationship with your spouse?
- What’s it like being a parent with cancer?
- What was the lowest point for you?
- Having a support system during cancer
- How can people can help cancer patients?
- Advocate for yourself as a cancer patient
- Advice for someone who has just been diagnosed
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Realize that this is not a death sentence. One of the phrases I use a lot is that cancer is a speed bump. It’s not a stop sign.
Process your emotions. You will go through the stages of grief. A cancer diagnosis is a grieving process because it can completely alter your life.
Process that, and then find a purpose. Find something that brings you joy.
Lacey B.

CLL Diagnosis
How did you get diagnosed?
I had been going to the doctor for severe fatigue for several years prior to diagnosis. We didn’t know what it was. Thoughts went through our heads that it was possibly chronic fatigue syndrome. Several doctors told me I needed to get more exercise, and that would solve the fatigue problem.
In 2007, I finally got a doctor that decided to run some lab work and found out my white blood cell count was a little high.
They did some more testing and found out I had a UTI. We treated that and did follow-up labs. My count was still high, so they sent me to a hematologist.
She did more specialized testing, and that’s how we came about the CLL diagnosis. She had looked at my fatigue, the elevated white blood cell count, a couple of more tests and eventually a bone marrow biopsy.
What’s a bone marrow biopsy like?
Going into it is kind of scary when they tell you that they’re going to drill into your bone.
You lay facedown on the table. I’ve had 3 done so far. They use a hollow core needle to go into your bone and draw out the fluid from your hip bone on the back. They numb everything up. For me, it was uncomfortable, but it wasn’t painful.
How did you react to your diagnosis?
I had a fantastic diagnosing oncologist. She’s about the same age as me. We kind of had the idea that I would end up with cancer in my lifetime. The leukemia part is what took me by surprise.
My mom and maternal grandmother have had breast cancer, so it wasn’t surprising for us to hear the cancer diagnosis.
I had just always expected it to be breast cancer.
In the beginning, I think I was numb to it. My husband and I left the office together. We had about a 5-minute conversation, and we both went back to work. It took a few weeks for it to really sink in for me.
»MORE: Processing a cancer diagnosis
What are the next steps after diagnosis?
Because CLL is usually slow-growing, it was a watch and wait situation. I had labs and saw my oncologist every 3 months to see if any lymph nodes were enlarging, talk about any symptoms and look at my lab work.
During that interim time, I had a “go big or go home” moment. I got over the anger of the diagnosis, and I decided to make some life changes. I decided I was going to start running.
My oncologist had suggested exercise as a way to help combat the fatigue. She never told me I needed to lose weight, but she did stress the importance of exercise in helping with the fatigue.
At the time of diagnosis, I was obese and not active, and the cancer diagnosis was a wake-up call for me. So, in the interim time before we started treatment, I became a runner.

How did running help you?
I noticed that when I started running, I started losing some of the weight. Because white blood cells are stored in fat cells, the kind of ironic thing was that my count dropped significantly. It was still abnormally high, but it dropped.
It really did help with the level of fatigue. I can’t say it took it away completely, but I was more alert and better focused.
When the diagnosing oncologist gave me the news, she told me it wasn’t a death sentence and was just something I was going to have to acclimate to as my new normal. Running helped me do that.
1st-Line Treatment
Why did you decide to start treatment?
We were tracking my white blood cell count and fatigue primarily. In 2014, my white blood cell count had doubled within a 6-month period.
My fatigue had gotten a lot worse again. I had some lymph nodes that were palpable. You couldn’t see them with your naked eye, but my oncologist could feel them.
She left the decision up to me. She warned me that the chemo would cause side effects.
It came down to the question of when my symptoms were going to become more problematic than the side effects from chemo.

What was your chemo regimen?
I did 6 cycles of fludarabine, cyclophosphamide and rituximab. It was 3 days in a row every 28 days. I would get the FCR chemo for 3 days, and before I left the clinic I would get a Neulasta shot. They’d send me on my way, and I’d come back in 28 days.
What are the side effects from chemo?
I developed an allergic reaction to the rituximab. I scared my chemo nurse half to death. That meant that we had to drop my flow rate. We stopped it completely that day and just infused it much slower the next day.
I thought I was fine, but everyone around me was seeing me go white. My heart rate plummeted, and I got super itchy.
Once we got past that and I tolerated the slower ramp up, the infusion days were not terrible. I watched TV, slept a lot, and tried to color and read, but the pre-meds just made me super sleepy.
The Neulasta shot was terrible. It caused a lot of muscle spasms and bone pain. About a week after each set of chemo is when I felt like it hit me. It was almost like the steroids wore off, and all the drugs were hitting me.
After the first round, I learned I would usually get about 3 or 4 days where I could function normally. Then I would have to sleep for a few days.
I had some nausea, but that was pretty well maintained. I had to have really strong flavors, though. Anything that was mild tasting tasted horrible.
It was almost like they didn’t register on my taste buds, and my brain just couldn’t even decipher what it was. Asian and Mexican foods were great.
When did you have no evidence of disease?
After my second cycle of chemo, my labs were technically showing no evidence of disease. I didn’t get the official statement from my doctor until December.
I finished chemo in August, and in December, we did follow-up scans and a biopsy. That’s when I got the official no evidence of disease declaration.

Relapse
How did you feel when you relapsed?
I had done some research. Because of the chronic nature of the disease, I kind of knew it was going to come back. The chemo was more like a band-aid than anything else. It was giving me a better quality of life for a while.
What surprised my medical team was how fast it came back given how well I had responded to the chemo initially. I got the official declaration of no evidence of disease in 2014, and it came back by June of 2017. It was evident in my labs again at that point.
I really believe the relapse was harder than the diagnosis. At that point, I was training for another half marathon. I felt great. My daughter was starting high school. Life was going really well.
When I got the news that it was back, it was like a slap in the face. I was doing all these good things for my body, but this disease just doesn’t care.
Treatment after relapsing
We discussed starting treatment immediately because of all the new therapies that had come out since I had been on chemo. Chemo was not a second-line treatment for CLL anymore.
Where I was in life, I wasn’t ready to start treatment again. I didn’t want the side effects from the treatment again. My symptoms at that point were not bad enough for me to justify starting treatment.
I had battled the fatigue the entire time. Even when I was technically in remission, I still had fatigue. I had some night sweats, and they’ve kind of stayed, so I wasn’t willing to start treatment if those weren’t unbearable.
Then my labs doubled in 3 months and tripled in 6 months. Then it was time to do something, even though my symptoms weren’t unbearable.

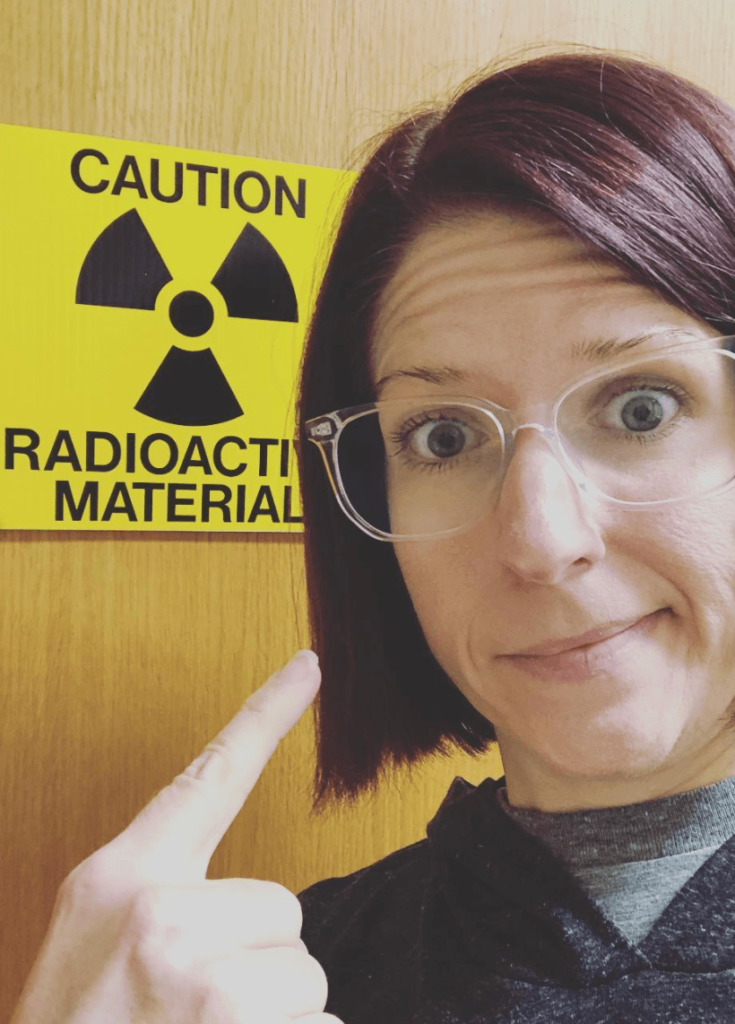
What was your second-line treatment like?
I’m on venetoclax and have finished Rituxan. It is 2 years of oral venetoclax, and it was 6 cycles of infused Rituxan with 1 infusion every 28 days.
To start the treatment, you have to be really cognizant of tumor lysis syndrome. I went inpatient for a little while to start the oral venetoclax.
They do that because it’s really good at nailing the white blood cells in your body. They can overload your kidneys, so they wanted me there to monitor that.
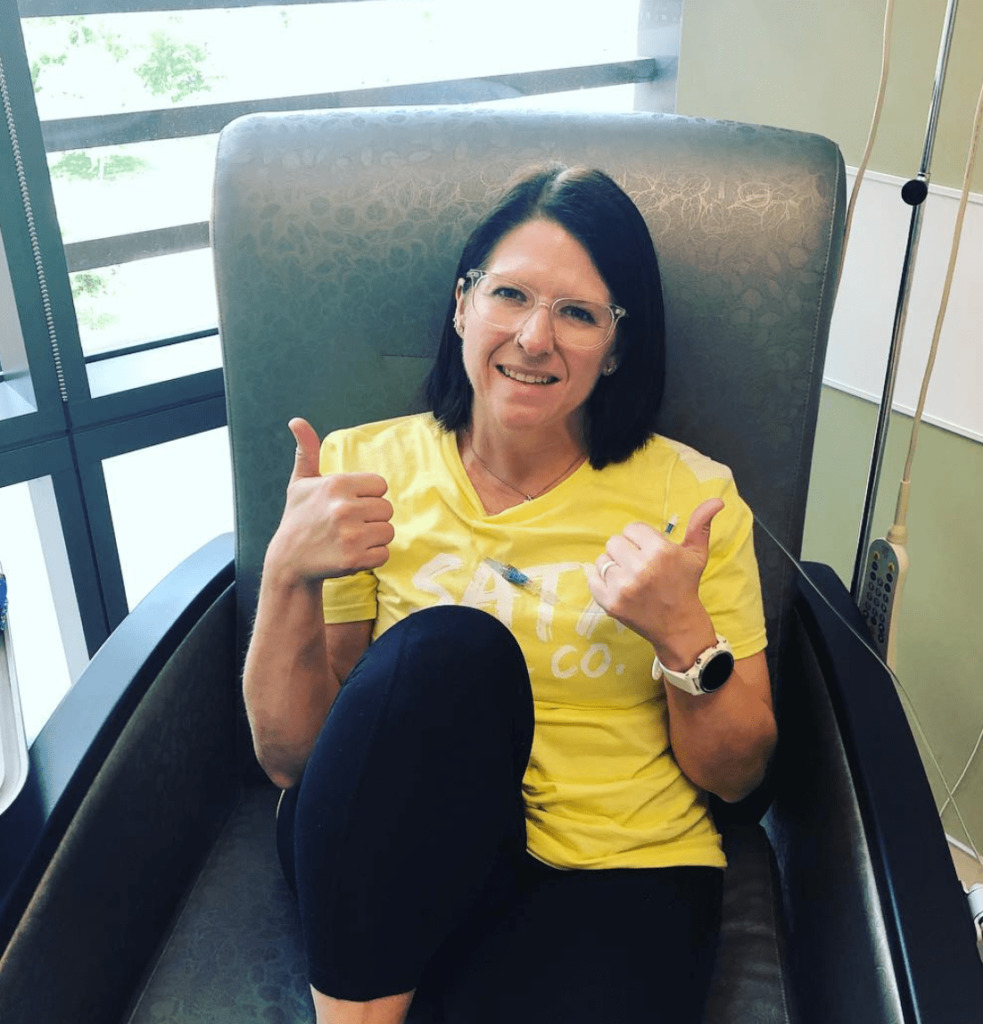
You do a ramp-up phase with your dosage up to 400 mg. Once you hit that top dosage, you start the Rituxan infusions.
Thankfully, I had zero complications getting to full dose. I’m not a very good patient, so the 5 days in the hospital was pure torture for me.
I took every opportunity to speed walk the halls and get out of my room. I felt fine, so I was restless if I had to be in my room.
So far, I’ve only had a couple of issues. The Rituxan infusions caused some GI problems. My body just doesn’t like it. My first infusion, I got the same allergic reaction to it. We had to scale back and ramp up the infusion rate slowly. After that slow time, the next cycles were fine other than the GI issues.
The Venetoclax hasn’t caused any side effects that we know of. I’m still battling the fatigue. The biggest thing that might possibly be attributed to the Venetoclax is that I’ve gotten 3 sinus infections since I started. That’s out of the norm for me.
After treatment
One more year of oral Venetoclax, but for now, I’m pathologically no evidence of disease. They eventually want to do another PET scan and bone marrow biopsy to double-check, but we’re not in any massive rush.
My lab requires me to get my blood work done every month before I pick up my monthly supply of venetoclax.
There are days when the anxiety still hits me. Some days, I think it’s unfair. I know this has affected me. For the most part, it just stays in the back of my mind and doesn’t affect my daily living. I take my meds in the morning, and then I go about my day.
I still get a little bit of anxiety when I see my oncologist because I don’t know how long the venetoclax will keep me where I am now, but it’s not a heavy amount.
Reflections
What is your “new normal”?
The biggest thing that has changed for me is that I try to make sure that everything I do in life has a purpose. I do the things that I always wanted to do.
I try to not let opportunities pass me by. While CLL is not a death sentence, there still is no guarantee for how long we’ll be able to control it.
I just try to have fun and live fulfilled. I’ve taken on some huge challenges with my running. I’ve turned to ultra running. I did my first 100k recently.
Whenever we have the funds to do it, we travel. I like to experience things and have adventures.

How cancer affects your relationship with your spouse?
There have been a lot of positives — and some positives because cancer brings about difficulty in general. He’s always been supportive.
His nature is being a protector. He always has been that way. He’s a provider and a fixer. It’s been hard on him to know he can’t fix this.
He goes to every appointment that his job allows. He went to every chemo session. He tries to put on a happy face, but I know that he hates that he can’t fix it.
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer

What’s it like being a parent with cancer?
It was really hard because you hear ‘cancer,’ and even though my oncologist said it wasn’t a death sentence, I thought, ‘Am I gonna see who she turns out to be?’
When I was diagnosed, she was only 6, so having to try to explain it to her and cope has been challenging.
As we got further along and she realized I was going to be okay other than maybe being a little more sick than usual, or needing her to wash her hands to not bring germs around me, it’s really been our new normal.
We don’t really blink an eye at it too much anymore. We have all garnered a morbid sense of humor.
We make a lot of jokes that people might think are offensive. It’s just our family’s coping mechanism. She’s a senior now, so we’re getting ready for graduation and college.
»MORE: Parenting with cancer
What was the lowest point for you?
Right before I started the first round of chemo. It was hard for me to admit that it was time to start treatment.
My fatigue had gotten so bad that I was not functioning. I would sleep most of the day while my husband and daughter were at work and school simply so I could be alert by the evening. That was really hard.
Even though I had no real control over it, it almost felt like a failure to have to go into treatment. That was probably my lowest point during this journey.
Having a support system during cancer
Being military, we didn’t really live near any family. We didn’t move back to Texas and get near family until 2017.
Even still, throughout the journey, my mom was super involved. She would come up and help with my daughter if I was having a big appointment or something.
We got most of our support from our circle of friends. We had a fantastic church family when I first got diagnosed. They would take my daughter when I needed someone to watch her. We would go out to lunch as a distraction.

When we moved to Las Vegas, that was where I went through my first group of chemo. I had a group of friends there.
Someone sent cupcakes at one point, and to this day, I still don’t know who sent them. They would bring meals when we were going through chemo. That took some pressure off of my husband.
It’s kind of an interesting situation when you get diagnosed with cancer because you find out who your true friends are. There is a loss of some relationships. It’s not that they have anything against you.
It’s just that when a friend or family hears about your cancer diagnosis, it might impact them in regard to their own mortality. They might not be prepared for that.
We did lose some friends along the way, but there were enough true friendships there that we always had support.
Here in San Antonio, I have a fantastic group of running friends who are constantly supporting me. They offered to come to chemo when I started the Rituxan and when I had to be inpatient to start venetoclax. We go out to lunch. We go on long runs if I need to vent. It’s been fantastic.
»MORE: What kind of support cancer patients say helped the most

How can people can help cancer patients?
One of the hard things as a patient is having all these people say, “Let me know what you need.”
A lot of times the patients don’t know what they need, or they don’t want to be a burden on people.
My best advice would be if you know anything about the person, just try to come up with something you can do for them without having to specifically involve them.
If it’s a gift card to a dinner out, offering to babysit or doing laundry — things of that nature that are hands-on are so helpful.
I’ve had friends send email gift cards to my husband so he could pick up food for us. Friends have sent coloring books and pencils to give me something to do during infusion days.
I got blankets, lip balm and care package items. Those are super helpful.
Advocate for yourself as a cancer patient
Make sure that you trust your care team. Being military and moving a lot, I’ve had several different oncologists. I have fired one of them. Don’t be afraid to fire one and find a new one if you don’t trust them completely.
We had moved, and our insurance had chosen a new provider for us. You don’t really get a choice in the beginning. I almost felt like this particular oncologist was scared of me. He didn’t know what to do with me because I was so young.
He wanted to do a lymph node biopsy in my neck, and that was something no one else had said I needed before. I didn’t trust him. I felt like he didn’t know what to do.
No one had any true examples to follow because my case was so unique. They had their best guess for a course of action, and they included me in the conversation if they were conferring with other doctors.
This new oncologist didn’t include me in the conversation. I didn’t like that.
I tried to give him a chance. I saw him for about 6 months. I had a couple of appointments with him. My husband and I had a talk that we needed a change. I just couldn’t put my faith in him as an oncologist. He was not a bad person, but he was just not a good oncologist for me. I ended up loving the next one I went to after him.


Advice for someone who has just been diagnosed
Realize that this is not a death sentence.
One of the phrases I use a lot is that cancer is a speed bump. It’s not a stop sign. Process your emotions. You will go through the stages of grief.
A cancer diagnosis is a grieving process because it can completely alter your life.
Process that, and then find a purpose. Find something that brings you joy. That was running for me. In the beginning, it was not. I hated it and was doing it more just to be healthy. It took me about a year, and I fell in love with running.
The only thing I’ve been told I can’t do in 12 years since my initial diagnosis is scuba dive. That’s only because of the active treatment I’m on right now.
I want people with CLL to realize that there’s not much you can’t do. Try to live life fully.

Inspired by Lacey's story?
Share your story, too!
Chronic Lymphocytic Leukemia (CLL) Stories
Nadia K., Small Lymphocytic Lymphoma (SLL)
Symptoms: Rash, lump under arm, fatigue
Treatments: Ibrutinib and acalabrutinib