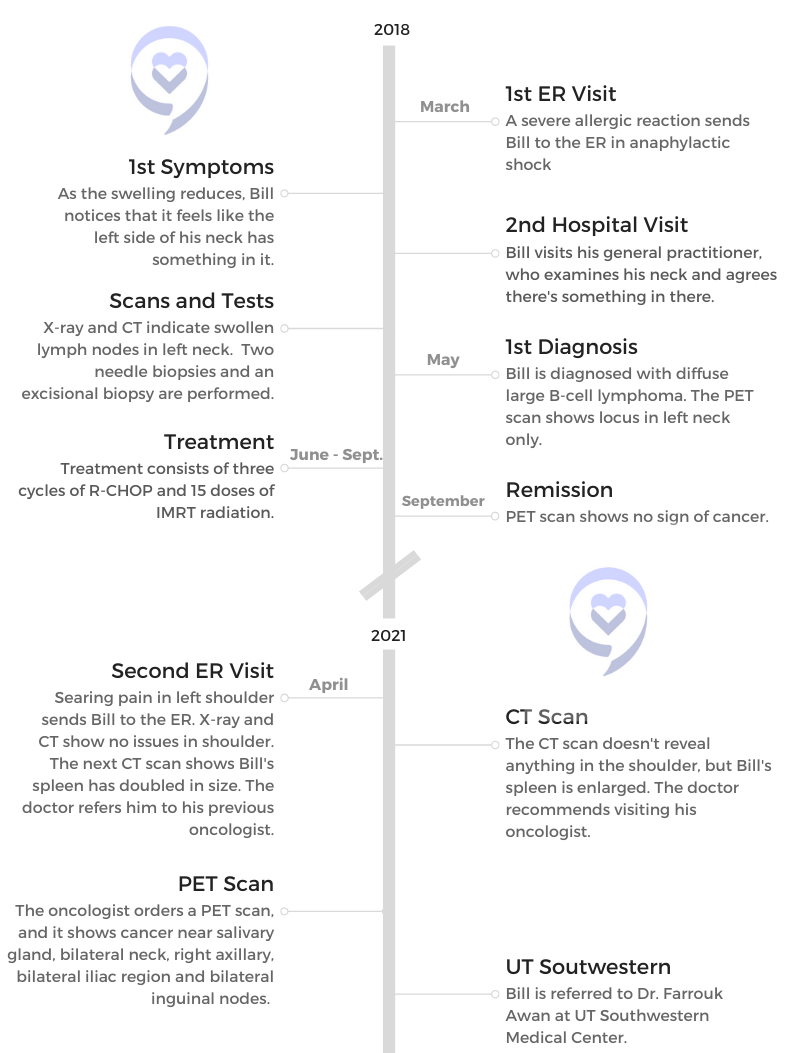
Bill’s Chronic Lymphocytic Leukemia with Richter’s Transformation Story

After an allergic reaction sent Bill to the ER, he noticed lumps in the left side of his neck. A series of tests revealed diffuse large B-cell lymphoma. Then he was in remission for 3 years before another ER visit for severe shoulder pain turned into another diagnosis: chronic lymphocytic leukemia (CLL) with Richter’s transformation.
Bill discusses how his diagnosis intersects with his original misdiagnosis, what it’s like being part of a clinical trial, hope for the future and the important of patient advocacy.
Explore his incredible story below. Thank you so much for sharing, Bill!
- Name: Bill Mouser
- Diagnosis:
- Non-Hodgkin’s lymphoma
- Subtype: Diffuse large B-cell lymphoma
- Subtype: Chronic lymphocytic leukemia with Richter’s transformation
- 1st Diagnosis
- Year: 2018
- Symptoms:
- Tightness and lumps in left side of neck
- Tests for DX:
- X-ray
- CT scan
- 2 needle biopsies and excisional biopsy
- Treatment:
- 3 cycles of R-CHOP
- 15 doses of IMRT radiation
- 2nd Diagnosis
- Year: 2021
- Symptoms:
- Severe pain in left shoulder
- Enlarged spleen
- Tests for DX:
- X-ray
- CT scan
- PET scan
- Treatment:
- 6 cycles of EPOCH
- Currently in clinical trial for DuoHexabody-CD37
- VIDEO: 1st Symptoms & Diagnosis
- VIDEO: CLL Treatment
- VIDEO: Bispecific & CAR T-Cell Therapy Side Effects
- Treatment Side Effects and Records
- What are the CLL therapy side effects?
- Have you noticed any improvements?
- How long will you be undergoing this treatment?
- Do you journal about your experiences?
- How often does the clinical trial team ask questions about how the treatment is affecting you?
- If bispecifics and CAR T had the same efficacy, which would you pick?
- Advocacy and Support
- Treatment Side Effects and Records
- Other CLL Stories
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
VIDEO: 1st Symptoms & Diagnosis
1st Symptoms and Diffuse Large B-Cell Lymphoma
Introduction: Tell us about yourself
I have been in vocational Christian ministry for most of my life. I’m a retired Anglican priest, and for the last 16 years I was the rector of St. Estimation Anglican Church here in Waxahachie, Texas.
What were your first symptoms?
I went to the ER with anaphylaxis. I swelled up like a toad and turned red. The therapy for that usually is some kind of steroids and antihistamines to kind of calm things down. I noticed when all the swelling in my face reduced, the left side of my neck seemed to be a little thicker than the right. I turned my head, and it would be tight.
I thought, “That’s weird.” We went to my general practitioner, a good friend for 30 years, and I said, “John, there’s something in there, I think.” He mashed around, and he said, “Yeah, you got something in there.”

Early on, I thought, ‘Okay, this could be something serious,’ and as the diagnoses proceeded, it was serious.
That led to an X-ray and then a CT, and the radiologist said, “Yeah, you’ve got some swollen lymph nodes in your left neck. You better check that out.” That started some diagnostic stuff — needle biopsies, finally an excisional biopsy — and the verdict came back: diffuse large B-cell lymphoma.
At what point did you realize it was serious?
My Christian faith helped a lot, obviously. I think actually it kind of snuck up on me. I’m one of these guys that wants to read all the radiologist reports before I talk to the doctor. The first one I read used the word “malignancy” at one point, and I thought, “Ah-ha, okay.”
I asked my good friend Dr. John, and he said, “Well, he thinks it’s a malignancy. We don’t know yet, but he sees a lot of it, and that’s what it looks like to him. That’s why he used the word.” But he said, “Let’s keep going.” Early on, I thought, “Okay, this could be something serious,” and as the diagnoses proceeded, it was serious.
Processing the Diagnosis
How did you get through the scanxiety waiting for the results?
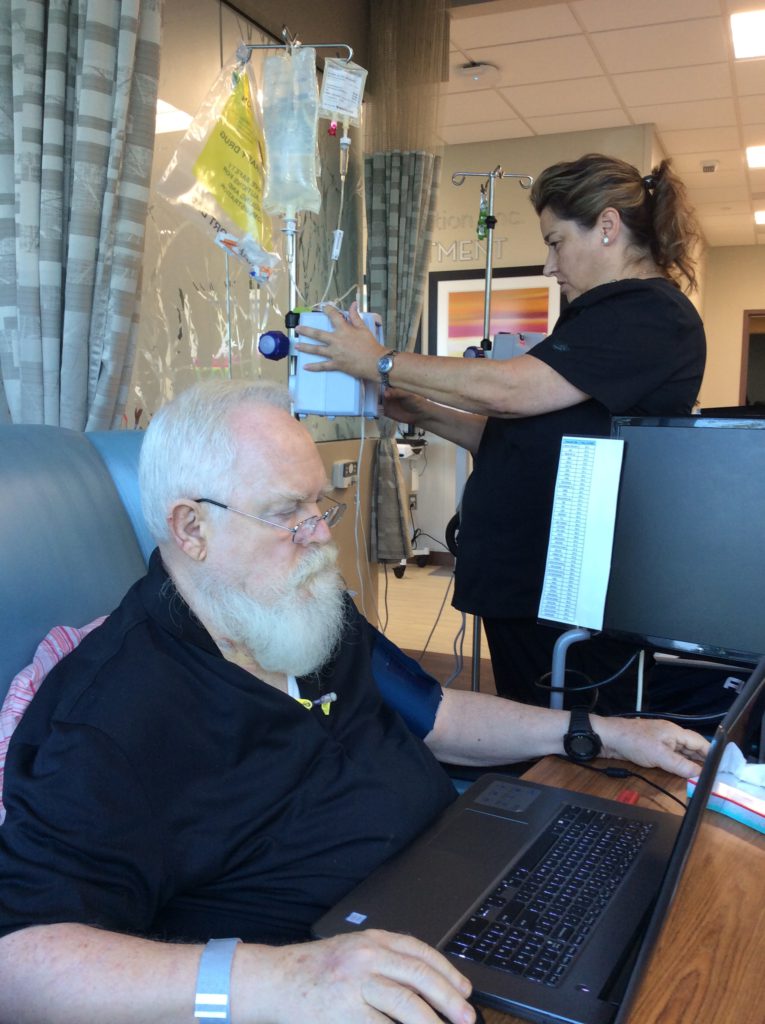
Actually, I had my plate full of things to do. I had not retired from my work, and so there were things on that plate. I have 3 living daughters. At the time I had 5 grandchildren, 4 of them nearby, and there was plenty to do.
I wasn’t just sitting around twiddling my thumbs and worrying. I just kept on keeping on. I felt okay. I didn’t feel sick. I thought, “Okay, we’ll just wait and see what comes down the pipe and deal with it when it gets here.” It stood me in good stead to do that.
»MORE: Patients describe dealing with scanxiety and waiting for results
How did you process knowing that you had cancer?
I kept my wife and children up to speed immediately, of course. We’ve got a pretty close-knit extended family, so everybody was on board, and they were concerned.
The local oncologist was fairly optimistic. He said, “We caught this very early, and it is a version of lymphoma that is quite responsive to therapy.” He said the cure rate is quite high for this type of lymphoma, and especially with catching it so early.
It was only in one spot. We had a PET scan, and that’s the only part that lit up. He was optimistic. He said, “The standard therapies we can do is basically 2. Statistically they’re the same as far as outcomes. You pick.” I did, and we did it, and it worked. Everything went into remission. We got our PET scan at the end of it.
»MORE: Patients share how they processed a cancer diagnosis
Treatment for DLBCL
Why did you choose the mix of chemo and radiation?
I assumed what everybody assumes about chemo: that it makes you sick. I don’t like to feel sick. I thought, “Okay, well, if indeed you can’t distinguish the outcomes statistically, I’ll take the less sicky one.” So I did 3 of the R-CHOP and 15 of the radiation, and it seemed to work just great.
What was the follow-up protocol after the cancer went into remission?
After that, he would see me every 6 months and physically examine me for evidence of swelling lymph nodes where he could palpate and where he expected things to show up, and nothing ever showed up.
The pain was excruciating. I’ve never had pain so severe in my life ever.
I think I had a PET scan about a year later. I’ve had so many of those. It started to run together, but there was just no evidence of the cancer for the next 3 years.
CLL Symptoms and Diagnosis
After 3 years of normalcy, what CLL symptoms sent you back to the ER?
The pain was excruciating. I’ve never had pain so severe in my life ever. I don’t know what is wrong with the ER people that when I showed up, they should have put me in a closet and closed the door because I was howling. I’m in a big waiting room full of people, and I’m just bellowing. I can’t help it.
They finally get me out into the place. They do an X-ray. Nothing. They can’t see anything unusual. They do a CT, and they’re starting to pump me full of morphine and finally get things calmed down.
If it was coming back for me, then okay. Lots of other people have been there and done that. It looks like it’s my turn to be there and do that.
The doctor came back after a bit with the radiologist report. He said, “The radiologist has looked at your CT, and he can’t find anything in your shoulder. Anything. Instead, I recommend you go to an ortho guy to check it out further, but we can’t find anything. However, he does notice that your spleen is twice the size it was a year ago, and he said that it’s crumbling. In view of your earlier treatment for lymphoma, you should probably check back with your oncologist pretty quick and have him follow this up.”
It’s almost like the first occurrence of the cancer. I go to the ER for something else and oops, you see something that turns out to be lymphoma.

What was the impact of having cancer again?
The fact that it was possibly cancer again wasn’t a shock. I know enough people who have been through similar situations. I know people who have fought cancer for years, and so the fact that it keeps coming back is not a surprise. If it was coming back for me, then okay. Lots of other people have been there and done that. It looks like it’s my turn to be there and do that.
I was frankly puzzled by this shoulder business. Much later, when I finally connected with the doctor at UT Southwestern, he said, “Oh, well, I’ll tell you what that was. It was your spleen. The nerve pathways from the spleen and your shoulder travel together. We call it referred pain. Your spleen is really in an uproar, but it’s not going to hurt down there. It hurts up here. I have other patients with the same problem.”
What did the PET scan show?
He did another PET scan, and this time, sure enough, the spleen was greatly enlarged; it glowed like the moon. The sites where there were colonies of lymphoma cells were in both sides of the neck, behind the ears, around the salivary glands, in the abdomen, in the iliac region, the inguinal nodes and over here under my arm.
It had clearly reappeared in a great many places all at once. I was definitely a candidate for something a lot more serious than what was offered in the cancer center locally here. That’s why he wanted to refer me to one of the big hospitals up in Dallas.
VIDEO: CLL Treatment
Treatment for Chronic Lymphocytic Leukemia
How did you choose where to go for treatment?
He didn’t give me a staging number. What I can get out of Google is that it was probably a good stage 3 at least, if not 4. Usually with these things, if you get lymphoma above and below the collarbone, you’re in deep water.
We had a friend of a friend who had consulted a doctor at UT Southwestern, and he was extremely pleased with the outcome and the relationship with the physician. Because we trusted the recommendation and the people making it, we thought, “Okay, providentially, here’s a report that sounds credible and encouraging. Let’s go for that.” That’s what I did.

How did you find out you were misdiagnosed?
He laid out a couple of different scenarios. The first thing was to find out what I had. He was a little suspicious, I think, of the diagnosis.
Dr. Awan actually secured the tissue from the 2018 biopsy, and he started digging around in the DNA. He had resources available to him that my original oncologist did not have.
When he deployed those resources, he said to me at one time, “Well, it’s either mantle cell, or it’s CLL, or it’s a transformation.” He didn’t explain a thing about transformation. He just said it’s going to be 1 of these 3. I could tell he was betting on it probably going to be mantle cell.
Then he went and got the lab work done. He called me back and said, “Mr. Mouser, I am really sorry to tell you that what you have is a transformed CLL. You were actually misdiagnosed in 2018.”
I don’t want to leave the impression that my original oncologist is incompetent. He saw diffuse large B-cell lymphoma, and it was there. But what I actually had was an atypical CLL, chronic lymphocytic leukemia.
It’s atypical because most of the markers for that never showed up in my blood work, and yet the genetics showed that’s what I had. Then about 1 to maybe 5% of CLL patients undergo something called a Richter’s transformation, where the CLL begins to generate a really aggressive diffuse large B-cell lymphoma.
That’s what my original oncologist saw. He saw something. What he saw was really there, and he treated it. What he didn’t see is underneath is this atypical CLL that’s boiling up this aggressive lymphoma. Frankly, an oncologist in his practice might never see that. It’s extremely rare to run across a case of it.
What were the treatment options?
Dr. Awan dug and dug and dug, and he said, “Oh darn, you’ve got that.” I thought, “Okay, what do we do now?” He said, “Okay, here’s what we’re going to do.” He laid out a strategy that starts with the 6 cycles of R-EPOCH. He said, “The first thing we’re going to do is clear out all the junked sites.”
It wasn’t going to cure me. He was quite candid. He said, “R-EPOCH hasn’t cured this in 20 years. It’s never cured it, and it’s not going to cure you now. That’s not what we’re doing it for. We’re doing it to get rid of most of the tumor mass in you, and then we’re going to hit it with something else.”
That’s what we proceeded to do. We went through the 6 cycles, 6 week-long cycles of R-EPOCH. He told me later that he didn’t think I was going to make it through the first 3 because it’s pretty stiff stuff. I guess I’m atypical in a lot of ways, because frankly, I felt best when I was in the hospital.
Maybe I was just flying high on prednisone. I don’t know, but I felt good, and I went right through it without any problem. I didn’t get really sick, and the hair came out. Still, I tolerated it quite well.
At the end of October, I had another dark PET scan. We pushed that stuff so deep away that you couldn’t see it for the PET scan. That part was successful as far as it went.
What was the next phase of treatment?
It was supposed to be a stem cell transplant. I’m not exactly sure why there were delays. Some of it is related. There’s just a lot of delays in the medical profession today with the COVID stuff and the restrictions and the therapies and patients that pile up.
The holidays came up, and they had to do the HLA typing and a lot of tests. Before you do a stem cell transplant, you’ve got to contact donors. I actually discovered I had several donors, so that wasn’t going to be a problem. But then you got to contact donors and see, “Are you still going to be a donor?”
Time passed, and so November and December passed. The 4th of January, I was scratching right there. I thought I felt a lump, and I thought, “Oh, dear. Maybe this was going to be bad.” I sat at the computer and sent a note to the clinic. The next morning, I got a reply that said, “Can you come tomorrow?”
If you have a really serious cancer, you should, if at all possible, use resources in a major research center.
I did. Dr. Awan examined me, and he just kind of rolled his eyes and said, “It’s back.” Of course, by that time, I had discovered the inguinals were swollen, too. Stem cell transplant was off the table. We were off the known areas of the matter. He was thinking; I could see the wheels spinning in his head.
He said, “I think what we’re going to do is BiTE. We’re going to get you in a clinical trial for one of the new BiTE drugs. Then if we can push it back again with those, we’re going to hit it with CAR T.” That’s the current plan right now.
Processing the Second Diagnosis
What are the biggest lessons you learned from this experience?
In one of the videos the Patient Story did with Dr. Awan that I viewed, he made a comment that I certainly endorse, which is this: if you have a really serious cancer, you should, if at all possible, use resources in a major research center. Those are the places where if there is real therapeutic help, cutting-edge therapeutic help, it will be there.
Now, what put me at ease is I am richly blessed with mature, responsible, loving children nearby. If I were to drop dead now, my wife would be well protected and cared for.
It will not be in the outer rural regions. I live in a town of about 30,000, but we’re about 45 miles south of Dallas. We have great medical care here for the ordinary stuff, including heart attacks. For kind of wild and woolly cancers, no.
That’s why as soon as the oncologist that was treating me here saw this new resurgence, he told me, “You need to go to Dallas and see 1 of these 2 centers.” So I did.
That’s what I would say to anybody. Go where the researchers and clinicians are working together to fight this stuff. If there’s true help that’s going to help you, it’s going to be there.

What helped you most through the dark moments?
If I had the biggest worry, it wasn’t dying. I’m not afraid of that. What bothers me about dying now is dying before my wife. We’ve been married 41 years. You dig really, really, really deep reps in 41 years. You run in them, and it’s comfortable and everything works. There’s this wonderful division of labor between the spouses, and you just chug, chug, chug, chug, chug. Take one of them out of the picture, and suddenly it’s not only companionship that’s gone. It’s all kinds of domestic duties and processes that now devolve onto the remaining spouse.
I didn’t want that to happen to her. Now, what put me at ease is I am richly blessed with mature, responsible, loving children nearby. If I were to drop dead now, my wife would be well protected and cared for. She’s competent. She’s not sick. She’d be very lonely and grieve, but we’ve got support. The family is there to carry her on.
I’m greatly comforted by that. That also tends to greatly relieve my anxieties about, “I’m not going to make it through this one.” Anyway, at her age and my age, we’re short timers anyway, but I really wish that she didn’t have to be a widow. I think I would do better as a widower than she would as a widow, but maybe I’m wrong. We’ll see.
VIDEO: CLL Clinical Trial (Bispecifics)
Clinical Trial Types and Requirements
What was your first reaction when he said the term “clinical trial”?
I was familiar with clinical trials. We got our first initiation into cancer therapy 25 years ago when my third daughter at 9 years old contracted a brainstem tumor. The first word I had from a doctor is these don’t heal. He basically said, “We can’t fix this. The only way that there was any hope for her is out in a lab someplace in the research center.”

For my daughter, she pretty much began with clinical trials, and we went through a lot of them. Pediatric brain tumors, I think that’s probably the toughest cancer nut to crack there is. In 25 years, it really hasn’t gotten beyond where it was with her. They’re just so hard.
Anyway, that’s where I got thrown in the deep end of the pool. When Dr. Awan said a clinical trial, I fully understood what he was talking about. I knew the difference between phase 1, phase 2 and phase 3 trials.
I am 1 of 90 people in North America and Europe who are receiving this particular drug for the first time.
I was actually hoping that there was a promising stage 2 or 3 that I could qualify for. It turns out I am participating in a phase 1 trial, which I can say more about in a minute. Clinical trials were not scary. I knew that for really difficult, hard-to-cure diseases, the true therapies that will finally succeed are today going to be in a clinical trial someplace.
Dr. Awan was never unclear about that from the beginning. R-EPOCH was just a cleansing thing before we tried the stem cell transplant. If that didn’t work, then we were off into the clinical trials. That’s where I am.
What are the differences between the phases in a clinical trial?
Phase 1 trial
In a phase 1 trial, they’ve done work in a lab in petri dishes and animal studies and monkeys and things like that. In a phase 1 trial, they’re putting the drug in humans for the first time. I am 1 of 90 people in North America and Europe who are receiving this particular drug for the first time.
The purpose of a phase 1 trial is to see if the drug is safe. Will it hurt the patient? Now, obviously, they have a good idea that it’s going to help the cancer, or they wouldn’t be giving it to a human. They’ve got evidence in animal studies that it attacks and kills the cancer, so that’s good. But you still have to put it in a human body, and sometimes what happens is we go, “Oops. We can’t use this because it’s going to produce something so bad.”
A phase 1 study’s purpose is to see if this will hurt the patient. Now, if it helps the patient also, great. Once they’ve decided it’s safe, then you move into phase 2 studies, where you’re looking not only on the efficacy, but at what dose? You want to know if it’s 1 gram, 2 grams or 10 grams. Once a week, twice a week, once a year? There are all kinds of factors in dosing and timing, and these have to be discovered experimentally.
Phase 2 trial
If you go through phase 2 trials and you can prove efficacy, you can say, “This is an optimal dose.” Then you expand to a great number of much more patients, trying to get more and more data. You can generalize more and more and more about adverse consequences and how to manage them.
The FDA obviously is watching very carefully all this process. If that all goes well, then eventually they have to be able to prove it. Once in a great while, you’ll see some efficacy so spectacular that the FDA will jump in and say they’ll approve it immediately. They say, “It’s unethical to go through all of this when we see how amazingly curative it is.”
»MORE: Read more on FDA approvals of clinical trials
What are the steps to get into a clinical trial?
The criteria for participating in a clinical trial is set by the company that wants the drug to be tested. Dr. Awan had slated me for 1 clinical trial. Then his coordinator started digging into the requirements, and she discovered that the company had specified that the participant could only have 1 therapy post standard therapy. I’d had 2, so I didn’t qualify.
Then we went to a second clinical trial where that wasn’t a factor, and it was the phase 1 of the particular drug I’m being tested on now. I could have 2 therapies post standard therapy, and they would allow me to.
Then of course they want to know my age; they want to check out my heart. They want me standard and healthy enough so that results that come in aren’t complicated by other health problems that I might bring to the participation. That’s understandable.
There were lots of scans and examinations and stuff to verify that I met all the criteria the drug company asked for, and I was approved. We began on March 21st.
Can you describe the financial aspects of a clinical trial?
In clinical trials, the funding for that is really coming from the drug company. That includes the hospitalization if they want you in the hospital, PET scans, anything that is medically necessary to get you through there, or if you have an adverse consequence and they have to medicate you or put you in ICU.
That didn’t happen, but if it did, the drug company pays for that. The patient is contributing his cooperation as a participant, and the drug company is covering all the medical costs.
CLL Clinical Trial Process and Environment
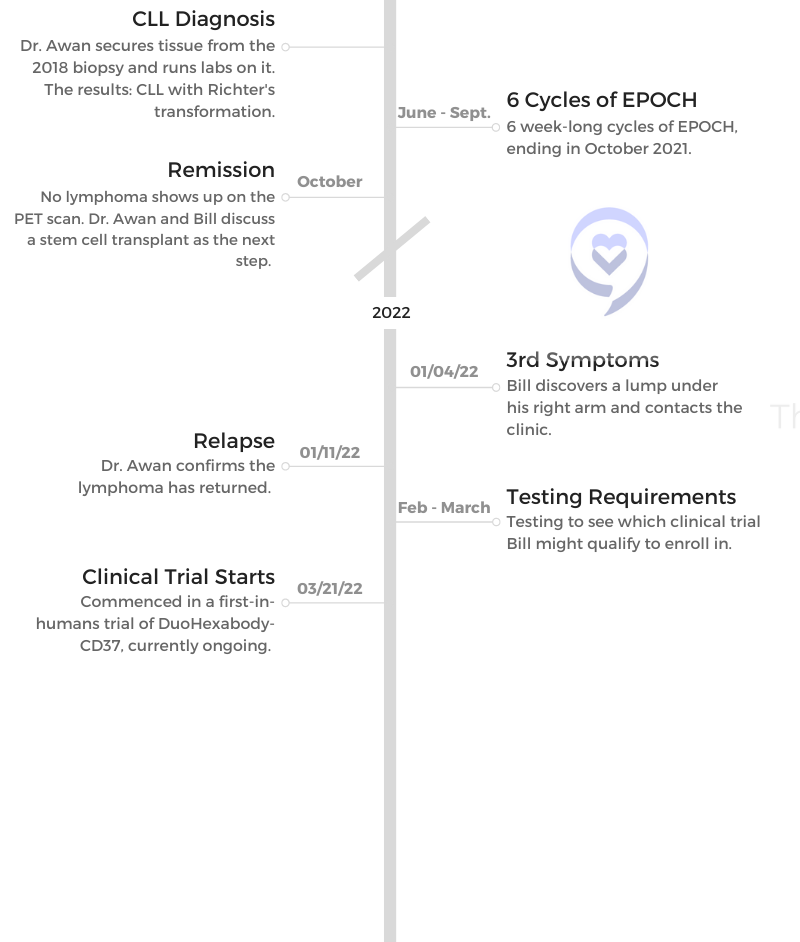
What is the regimen of the CLL clinical trial treatment?
Beginning
It’s pretty intense at the beginning because it is the first time in humans, and there is no data on what’s going to happen. Everybody wants to be super cautious that if something goes off the rails, we can manage it quickly. That means putting me in a hospital setting. I have 1 more week to go as the last 3 weeks have gone.
Current Process
I enter the hospital on a Sunday afternoon and get settled in. Bright and early, they do some blood labs at about 5 in the morning. That is to determine what my white cell count is.
The drug that is going to be administered to me might be adjusted up or down slightly, depending on what my white blood cell count is. Then about 10:00 a.m., they begin some pre-medications: some dexamethasone, a pretty stout steroid, and some Tylenol and an antihistamine.
These are all prophylactic to put a lid on what they think is likely to be a reaction. They don’t know, but they want to be especially careful.
Then they give me this infusion through an IV. I’ve got a PICC line. They hook me up to the IV pole and infuse the drug over a period of 4 hours. At the end of the 4 hours begins another 4-hour observation period. They’re taking EKGs very frequently. They’re doing vitals every 15 minutes for 2 hours.
I wear the pressure cap on my arm or even take it off. Then it’s like every 30 minutes for the next hour, and then it’s every hour. It’s kind of tedious, but I do understand why they need and want to watch so carefully. Frankly, I’m glad. Now nothing is happening, which is great. I’m happy that had anything ever happened, they were right there.
Then I remain in the hospital for 2 more days. I take my laptop. I have work and writing I do. Then on Thursday, we do the whole thing again. Then at the end of the day on Thursday, I’m discharged to go home. I spend Friday and Saturday at home, and then the next Sunday, I’ll go back in again.

Next steps
Next week will be the last hospital stay, and after that infusions will not be twice a week, but just once a week at the clinic. It’ll be an outpatient thing. I don’t know how long that goes — I’d have to check the protocol. It’s probably another month or 2, and eventually it’ll go to an infusion every 2 weeks and then every month.
Meanwhile, they’re taking PET scans all the way through here, watching what’s going on with these swollen lymph nodes. Are they changing? Not changing? If they do change, which direction and how much and how fast? They don’t know.
It’s extremely involved at this point. In phase 1, I think it’s probably extremely involved when they don’t have any roadmap at all. We do need to be careful and very thorough, and they’re watching.
Who is part of the CLL clinical trial team?
There is a research team from Dr. Awan’s clinic. Dr. Awan is the chief investigator, but he has his assistants, who are actually in the hospital managing the paperwork. As these reports are being gathered, they’re sending them to the drug company. I don’t know where it’s located. I think there’s actually an office in the States and in Europe someplace.
Actually doing the infusion is a very simple thing. It’s just an IV infusion. I’m on an isolation floor in this hospital. It’s the place where they do stem cell transplants, CAR T and extended chemo, like I did last summer. It’s highly protected; it has HEPA filters everywhere and negative pressure stuff. I don’t know. There’s stuff in the architecture that is designed to keep that thing as sterile as possible. Nobody can get in there except patients and medical people.
What’s it like being in a controlled environment without friends or family?
It’s not been bad. You and I are talking here face to face. My wife can do this, too. We can talk a couple of times a day by Zoom or phone. She would much prefer me to be here in the evenings, but the fact that we’re separated in different universes — no, that’s not really been the experience.
I got to know most of the floor staff in the 6 weeks I was in that floor last summer. When coming back, it was, “Hi, good to see you again.” I know a lot of them, and so that’s good. I don’t feel lonely.
VIDEO: Bispecific & CAR T-Cell Therapy Side Effects
Treatment Side Effects and Records
What are the CLL therapy side effects?
I had a side effect in the first infusion, and I really do think it was unrelated to the drug. When I had the R-CHOP 3 years ago, they would give me 1 of the earlier BiTE drugs, actually rituximab.
The nurse would always ask me, “Do you feel chills? Do you feel nausea? What’s your temperature like?” I had no problems. They would give it to me in small amounts, and then as long as I didn’t react, they’d up the rate until it was gone. Same thing here, but this time I had a reaction.
There’s something called rigors. It’s like severe chills, and it’s not uncommon as a reaction to any infusion. I just never had one of those. They gave me Demerol and Benadryl, and within 5 minutes it was gone. It never came back. It never happened again. I don’t think it was related to the drug.
Have you noticed any improvements?
As far as what I see about the drug, I’ll just report I can’t judge this drug. I’m not the doctor, I’m not the researcher, and I’m not the clinician. I do know that when I went in, I had a lump about the size of an apricot pit right here in front of my ear and another very painful lump under my ear lobe. It was the lymphoma side.
Within 2 days after the first infusion, it disappeared. Of course, I was like, “Whoa, that’s amazing.” I have this big thing under here. Today, after 3 infusions, it’s now about 50% of what it was. I told Dr. Awan this. I said, “I am flabbergasted at the speed of the changes.”
I’ve thought a lot about what he said, because he looked at me and said, “Well, it’s early days.” That’s about all he said. I’ve thought about that a lot. Here’s my supposition. He’s done lots of clinical trials. He’s probably seen many immediate improvements that over time didn’t pan out, so my enthusiasm is not something he’s going to join in.
Now, am I hopeful? Of course. Do I, reflecting on it, think that I’m going to get over this by this road? I hope so, but I don’t know yet. We’re going to find out. In the meantime, I’m having fun because it is, quite frankly, a delight to get a medicine and see something as dramatic as that. I think, “Wow, this stuff is amazing.” Right now, for me, it is amazing.
How long will you be undergoing this treatment?
I haven’t got anything specific, but I think the trial that I’m participating in, I’ll continue with that until it either stops working — in other words, PET scans show that there are no changes or it starts progressing again — or it disappears and the PET scan comes back clean. Then he would probably want to say, “Okay, now let’s throw the CAR T at it.”
After the twice-a-week infusions, they’re going to do a PET scan and see. I know they’re going to see a shrinkage because I can see a shrinkage. I can’t see a shrinkage in my spleen or the iliac region of my gut, but I can see where the nodes are close to the surface. I can palpate the inguinals in here. They’re gone here and going away here.
Do you journal about your experiences?
The closest to journaling that I do is that I have a pretty extensive list of people from family and previous parishes I’ve served who are praying for me. I write to them updates periodically, explaining what’s going on and what kind of challenges I’m facing and specific things I want them to entreat the Lord about. That is my journaling.
How often does the clinical trial team ask questions about how the treatment is affecting you?
It happens pretty frequently. On that floor with the kind of therapies they’re doing for patients, there can be central nervous system complications, especially when you get into stem cell transplants or CAR T.
When the nurse comes in for those patients, it’s to say, “Tell me your name and your birthday. Where are you? What day is this? What town are you in? Recite the months of the year backward.” Things like that.
I was chatting with one of the nurses one day about this. I said, “You do this every time. I’ve got these months memorized. Can’t you come up with something different?”
She laughed. She said, “I had a patient about a year ago. I walked into her room, and she was chatting just like you are with me. I said, ‘Who’s the president?’ And she said, ‘William McKinley.’ I thought she was joking. I said, ‘What year is it?’ And she said, ‘I think it’s 1830.'”
Anyway, the woman was lucid but totally in a different place. They check up there and regularly are asking to be sure that I’m still compos mentis.
If bispecifics and CAR T had the same efficacy, which would you pick?
If both outcomes are the same, what I’m doing now is obviously preferable. It’s an infusion. It’s not painful. CAR T puts you in the hospital for at least 2 to 3 weeks, and if you have complications, that could go to 4 to 5 weeks. CAR T is still evolving.
I was talking with Dr. Awan a couple of weeks ago about the CRISPR technology. What’s going on in the research centers with CRISPR is the ability to take T-cells from a healthy donor. Then they use those T-cells. They edit the DNA in those healthy T-cells from the donor so that when they are infused in a patient, they do not attack the patient’s body. Graft host disease gets eliminated. They become like blood plasma. They can be given to anybody, not just one person.
CAR T right now works on me, but it wouldn’t work on you. CAR T is specifically individualized right now. It’s not scalable very easily, but they’re working on a different approach, where it will be scalable.
He says they can build kill switches in these T-cells so that when they insert a certain trigger chemical, an innocuous thing in the patient, all these special T-cells will just die.
It’s amazing what they’re working on here. None of these have hit human trials yet, but they’re in the works. If you know where to look in the scholarly work, scholarly journals, you’ll find reports about these kinds of things. It’s just mind boggling what they’re going to be able to do.
Advocacy and Support
Why is advocacy important?
Advocacy is best done by somebody other than the patient, if possible. That’s hard because it’s 2 people involved in the whole process. I was my daughter’s advocate, and that’s how I learned how critical it is, especially for children, to have an adult advocate all the time because they’re vulnerable. They don’t know anything. They can’t contend for themselves.
Adults are the same way, and many of them are vulnerable. Any patient is going to feel a kind of vulnerability in that setting. If you have a complaint or you think something’s not right somehow, it’s difficult to complain or challenge the people that are supposed to be helping you.
That’s why an advocate that’s not the patient is really the best, because then the patient can be a patient and the advocate can contend for the patient as needed.
The best advice I would give to somebody going into something like this is to search diligently for a good support group of people who are in the same setting, the same battle.
Never, never, never cease to ask questions of your doctor.
I’ve been part of 2 different support groups that had both patients and caregivers and medical personnel. All of them were participating, and those were wonderful because then patients can compare notes as they run into questions they have.
They can devise strategies many times about workarounds that a disease might throw at you. It’s hard to do certain things. How do you work this out? People are pretty good about helping each other.
What support groups do you want to share?
The first one I ran into is still functioning. It’s called BRAINTMR. When I ran into it, it was an email list thing back in the late ’90s. I think they’ve got a forum now, but it’s a fantastic group.
Then recently I ran across 2 Facebook groups. One is devoted to stem cell transplant patients, and the other one to people with Richter’s. That group is pretty interesting. Mostly what we’re learning is all of the different novel immunotherapies that are out there being tested. It’s really exciting to hear what’s going on.
I’m very hopeful I might actually lick this thing. I’m in it for the long haul.
If you’re hit with cancer and you don’t know anything medical, doggone it, there’s a learning curve there that’s pretty steep. If you can find anybody in a support group to help guide you on sources of information, that’s going to get you in the stream pretty fast and allow you to talk intelligently to your doctor and ask intelligent questions. Never, never, never cease to ask questions of your doctor.

Anything else you’d like to share?
I’m very hopeful for myself and hopeful for people who have the problem I’ve got. This is one of the nastier ones to have than the more ordinary kinds of lymphomas.
When I first checked out with my cardiologist about a year ago, he kind of rolled his eyes. He said, “The advances in hematology and blood cancer, we don’t have anything like that in cardiology.”
He said, “You’re very fortunate if you’re going to be really sick to have that sickness, because there’s a lot of help that’s just coming down the pipe real fast.” I agree from what I’ve seen, and I’m very hopeful I might actually lick this thing. I’m in it for the long haul.

Inspired by Bill's story?
Share your story, too!
Other CLL Stories
Serena V., Chronic Lymphocytic Leukemia (CLL)
Symptoms: Night sweats, extreme fatigue, severe leg cramps, ovarian cramps, appearance of knots on body, hormonal acne
Treatment: Surgery (lymphadenectomy)
Margie H., Chronic Lymphocytic Leukemia
Symptoms: Large lymph node in her neck, fatigue as the disease progressed
Treatment: Targeted therapy
Nicole B., Chronic Lymphocytic Leukemia
Symptoms: Extreme fatigue, night sweats, lumps on neck, rash, shortness of breath
Treatments: BCL-2 inhibitor, monoclonal antibody
Symptoms of CLL
Learn about how some of the common CLL symptoms first present themselves from patients who have been diagnosed with CLL.




