LaSonya’s Bladder Cancer Story
As a professor of nursing and as a nurse practitioner, LaSonya was always quick to seek medical help whenever she noticed something was not right, including the day she discovered blood in her urine. She made an appointment with her doctor where she received a CAT scan. The scan revealed a mass on her bladder.
She then made an appointment with a urologist who assumed the mass was superficial bladder cancer. Despite his lack of urgency to have the mass removed, LaSonya pushed for surgery and he agreed. After surgery and sending the mass to pathology, LaSonya was diagnosed with high-grade bladder cancer.
LaSonya’s journey with bladder cancer began just 5 years after her first husband passed away from lymphoma. Her diagnosis also came around the same time as two of her cousins who also received cancer diagnoses and a college friend of hers.
Now cancer-free, LaSonya shares her story with us including the importance of finding a cancer community, how she advocated for herself, why she opted to remove her bladder, her process in deciding on a urinary diversion route, the importance of caring for your mental health, and her encouragement for taking new symptoms seriously.

Name: LaSonya D.
Diagnosis (DX):
Staging:
- High-grade
Symptoms:
- Blood clumps in urine
- Surgery
- Bacillus Calmette-Guerin (BCG) Treatment
- Bladder removal
- Urinary diversion
- Indiana Pouch
Listen to your body. If you feel like something’s not right, it’s not right.
LaSonya D.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Symptoms & Diagnosis
- Processing A Cancer Diagnosis
- Patient Self-Advocacy
- Describe your experience with your urologist
- Preparing for surgery
- Describe how that doctor made you feel
- Deciding to transfer cancer care
- What were the pathology results?
- What did your doctor say about your diagnosis?
- Did your doctor try to get you to stay in his care?
- Describe the impact of doctors making assumptions about their patients
- Switching Medical Care
- Treatment
- Cancer Community
- Bladder Removal
- Quality of Life
- Reflections
Symptoms & Diagnosis
Tell us about yourself
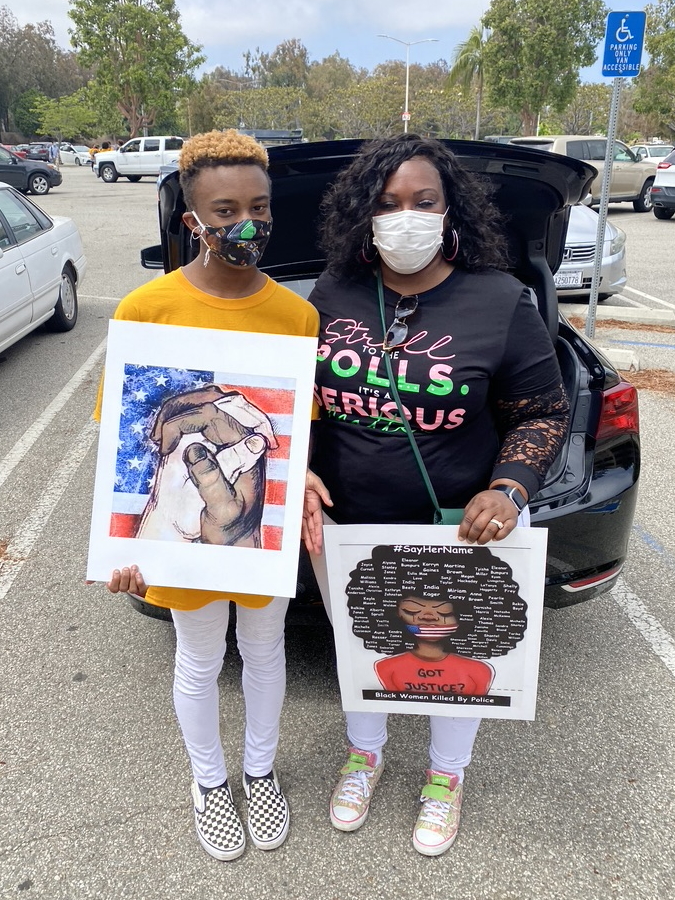
My name is LaSonya. I’m a black woman, that’s the most obvious when you look at me, but I’m also a mother and a wife. I am a professor of nursing and a nurse practitioner of both family and women’s health.
What were your initial symptoms?
I noticed one day that I had blood in my urine and it seemed like a lot of blood. I saw some blood clots.
I’m really in tune with my body. If something is off, I find out what’s going on right away. I don’t waste a whole lot of time trying to figure things out, especially when this happened. I had just recovered from an elective procedure and I was getting ready to go back to my regular work.
I noticed one day that I had blood in my urine and it seemed like a lot of blood. I saw some blood clots and I was thinking, “Well, I know I’m not on my menstrual cycle, so what is going on with this?” I thought, “Well, maybe it’s something from my surgical procedure.” It had been a month prior.
I called my surgeon and I said, “Hey, this is happening to me.” And he said, “Well, it doesn’t seem like this is something that will be related to your surgery, but we’ll go ahead and have you go in for a urine test. Let’s do a urinalysis and see if you have a urinary tract infection.” So I did that. I went in for urinalysis. It came back negative for infection, but positive for blood. He said, “Well, you need to follow up with your primary doctor.”
I called my primary doctor. Fortunately for me, I used to work for my primary doctor, so I know her well. I just called her on her cell phone and I said, “Hey, this is happening.” And she said, “Why don’t I have you go and do a culture? But in the meantime, I think we need to do a CAT scan of your bladder.” I went in for a CAT scan a few days later and it came back that I had a mass in my bladder. Being a nurse practitioner, I knew what that meant.
How did you react to discovering you had a mass?
If it was one of my patients who had blood in their urine, I would have gone down the same road. I would have done the same exact test that my primary doctor did. And for us, we think blood in the urine could be a urinary tract infection. It could be kidney stones. The worst-case scenario is bladder cancer. The way I approach my patients is, tell me why it’s not bladder cancer. When somebody has a headache, why isn’t it not a brain tumor versus ruling in the brain tumor? I was just like, “Well, why is this not bladder cancer?” For myself, I would have done the same thing to my patient.
Finding that I had a mass in my bladder was a devastating thing. It was devastating news. It was like, “How did I get this? No one in my family on either side has a history of cancer. How could this be? I don’t even know one black person that has this type of cancer.” I was just really, really thrown back by it. And I was like, “Could it be a mistake? It could be a cyst. It could be this.” The next step was going to be that I would have to see a urologist.
Making an appointment with a urologist
Well, it happens that the doctor that I currently work with had a good friend who was the head urologist in our healthcare system that we both work for. She phoned him up and told him the situation. And remember this is in January of 2021, so we’re in the midst of COVID too, so there were a lot of delays trying to get surgeries and procedures done. She called him up and said, “Hey, my nurse practitioner had this going on. Could you please see her?” Fortunately, I was able to, the following week, get an appointment and he squeezed me in so I was going to see him at that time.
We went to our appointment with the urologist and he talked to us a little bit about the procedure. He scoped my bladder and we could see the actual mass. He said, in fact, that it was bladder cancer.
Did you suspect that it was cancer?
I think I was already prepping myself mentally for that outcome, but it was still devastating. I was a nervous wreck at that point. I remember having to take off work because my blood pressure was through the roof. I felt so defeated and deflated and I could not believe that this was happening to me. I just could not believe it.

He said, in fact, that it was bladder cancer.
It took me a week or two to get myself together mentally for what was next because the next thing that they needed to do was the biopsy, resect it, and see what stage of cancer it was. I had started doing a lot of reading. I’m a nurse practitioner, so of course I’m going to just do a lot of reading. My biggest concern was, “Is this muscle invasive?” Because if it is, that means that I’m going to have to have my bladder removed, chemo and all this stuff is going to happen really fast.
»MORE: Reacting to a Cancer Diagnosis
Processing A Cancer Diagnosis
Did you tell your family?
One thing that my family had already gone through was my first husband passed away from lymphoma. At that time, it was probably about 5 years prior. My older two kids were in a deep stage of grief after losing their father at 47 years old. He went downhill in a matter of 3 years. So for them to now find out that their mom has cancer, it was really tough.
My youngest son was away at school. He’s a dancer. He was away at the University of North Carolina School of the Arts High School. He was there in 10th grade and we didn’t tell him anything. We didn’t want to tell him until he came home for summer break because we knew it was going to be bad for him. There was no reason to let him know right away other than to get him all upset and worried about it. So it was a rough situation, thinking about your own morbidity and then also your potential mortality, especially when you’re thinking about cancer.
Seeking the help of a therapist
I knew right away that this was going to be very stressful, not just for me but for my family. I knew that in order for me to get through this, I was going to need help. I contacted [my therapist friend] and I asked her if she would take me on as a client and she agreed. I started right away meeting with her once a week. Our meetings continued through my first treatment, so basically from February through May, I would meet with her on a regular weekly basis, which was so helpful for me.
The importance of caring for your mental health
I just think that a lot of times people think that you have to take everything upon yourself, especially being from my culture. Mental health is very taboo. People take it as a weakness when you need to seek out help mentally. You always hear people say, “Be strong. Suck it up. You can do this. Don’t be weak-minded,” those kinds of things. And we are human beings. We are not robots and machines. We have feelings. We have difficulty.
When things come into our lives they’ll say, “Pray about it. Give it to God,” which I’m a very, very spiritual person. I’m a Christian and I very much lean on my faith, which is another thing that helped me get through this. But at the same time, my grandmother used to always say, “The Lord helps those who help themselves.” So it’s important for us to help ourselves. Part of that was me interacting with a therapist who could help me, someone that I could trust, and someone outside of my house, my family, and my life.
It was enough for me to talk to my husband but there were some things that I was going through that I didn’t necessarily want to tell him and burden him with because he had his own burdens of worrying about mortality or morbidity. I wanted to be able to freely talk without having to worry about someone else’s feelings about what I was going through and it was very helpful.
Finding cancer care
Go with your gut. If you feel like something is not quite right, get a second opinion. You’re entitled to a second opinion.

The first thing I did was I looked for a reputable bladder cancer organization. Because you can find anything on the Internet — some of it is true, some of it is false. You can find people that will sell you snake oil and a bucket of sand. At the same time, you can find medically sound information.
Because I am a scholar and also a clinician, the first thing I did was pull research articles and guidelines of practice because I wanted to know what was I to expect. I wanted to know if whoever I was going to see if they were following the correct guidelines to take care of me or not. I never have been one to put all my trust in another human being, so I felt like I needed to do my own research and have my own questions ready so that I know that I’m getting the best care possible.
The experience I have with urologists made it even more clear to me that my approach is the best approach for me. Despite the fact that I was a clinician — I actually worked in the same healthcare organization that he worked in — he did not treat me well as a patient. And thankfully, because I’m a clinician, I was able to identify that right away. But I think that when you’re talking about other people who are not clinicians, just lay people or average people who are going to seek care, go with your gut. If you feel like something is not quite right, get a second opinion. You’re entitled to a second opinion and some insurance will even pay for a third opinion. Do not feel like you’re stuck with that person.
Patient Self-Advocacy
Describe your experience with your urologist
I went in to see this doctor and he scoped my bladder and said, “Oh, it’s bladder cancer. It’s definitely bladder cancer,” matter of factly, “But I think it’s really superficial. It’s probably not a big deal. With COVID, it’s hard to get an OR so we can schedule this out.” And I said, “No. If you can’t do it, I can find a surgeon that can do it. I have very good insurance. I have a PPO. I can go anywhere I need to go. I have something growing inside of me that doesn’t belong here and I want it out.” He said, “Okay, well, I’ll go ahead and do it.”
He had someone come up from downstairs to give me a COVID test because you had to have a COVID test before you could schedule your surgery and he said I can have my surgery in a week. The lady came up and she did my COVID test. I think she was a medical assistant, but I didn’t notice at the time. And when I think back, I didn’t see her label my specimen.
To make a long story short, the COVID test came back positive. How do I have COVID? I’ve been home for 4 weeks. I’ve been in my house because I had had that surgical procedure. My husband’s working from home and we’re the only ones here. We’re very, very careful and cautious. For a whole year, I’ve been working in the field, in the clinic, with patients, some of whom were positive for COVID, but I hadn’t had COVID. So I was like, “Something’s wrong with this.”
I called my clinic, I went down there and I had them do another COVID test, and that COVID test came back negative. When I called them and said, “Hey, I had a false positive test. This new test is negative. I do not have COVID.” They said, “He’s going on vacation.” So he was gone on vacation and I kept calling and advocating for myself to get on the schedule so I was able to get on the schedule for the following week. Three weeks after diagnosis, I was able to have my surgery for the resection.
Preparing for surgery
During the time that I was waiting to have my surgery, I had questions for this doctor so I inter-officed him. It’s provider to provider and within our system. The day of my surgery, I checked into the hospital and during that time, you couldn’t have visitors in the hospital so my husband couldn’t go with me to pre-op. I had to go by myself, which was very nerve-wracking. I didn’t know what was going to happen.
So I go into pre-op, they’re prepping me and if you’ve ever been into pre-op, there’s beds and there’s curtains between them so you’re not in a room by yourself. They’re getting you ready, they’re starting your IV, they’re getting your history, having you sign your consents and all those things.
He came in before it was time for him to have the surgery and he said, “Okay, well, we’re ready to do your surgery. I can tell you’re a highly anxious person.” That’s what he said to me. So I’m thinking, “Should I say what I really want to say? Or should I just not say what I really want to say?” Because this man is getting ready to operate on me. I’m going to be asleep. He’s going to have his instruments inside of me so I’m not going to say anything to put myself at any risk.
»MORE: Signs of Medical Gaslighting as a Cancer Patient
I said, “Yes, I am.” Whatever it takes for you to feel good about yourself to do what you need to do, that was my thought process. And he goes, “Well, you inter-officed me, but please don’t do that again. Do not inter-office me. If you’re going to email me, email me through the patient portal.” And so I’m sitting here listening to him and I’m thinking, “We are in pre-op. You’re getting ready to resect my tumor to find out if I have cancer and if it’s superficial like you say that it is.” And my thought process was, “You don’t know everything. How can you tell me that this is not invasive cancer by looking at it with your eyeballs?”
I thought, “I’m not trusting you saying ‘superficial is enough’ and I want it out now.” And so I’m sitting here thinking, “Okay, now you’re going to chastise me in the pre-op area for something that we could talk about at another time.” And that email had been sent probably a week or two before, so this was not urgent. He was on vacation the whole week before so there was no reason for us to talk about that right then. So I just said, “Okay.” We had the surgery. Everything went well. And then he says, “Well, it’s going to go off to pathology and then we’ll find out what the situation is.” I said, “Okay.”
Describe how that doctor made you feel
I was not his colleague. He did not see me as a colleague. And then the way that he was chastising me in front of my colleagues, fellow nurses, and other patients. It could have been one of my patients that was in there with me. We’re all in the same healthcare system and he had no consideration of that. The little respect that I had left for him, I lost it right there.
My first thought was, “I will never, ever in a million years refer any patients to this person.” I also said, “Wow. He’s going to be a star in my book.” The chapter is probably going to be, “Do Better,” because it was uncalled for.
Deciding to transfer cancer care

If you have to drive an hour and a half or two hours to get the care that you deserve, you need to do that.
When I got home, I talked about it with my husband. And we had already decided that once I got a definitive diagnosis I was going to transfer my care to City of Hope. I decided that I wanted to do that because my great aunt had melanoma skin cancer, and she went to City of Hope and they gave her excellent care. I said, “We have the insurance so we can do it so let’s just do it.”
From where we live, City of Hope is about an hour and a half away. My husband said, “It doesn’t matter how far it is, I’m going to take you wherever you need to go.” That’s something that I can’t express more powerfully. If you have to drive an hour and a half or two hours to get the care that you deserve, you need to do that. I tried to get my ex-husband to transfer his care to City of Hope. I tried to get him to transfer for almost a year. Finally, when he decided that he was ready to transfer to the City of Hope, he could not transfer. He was too ill.
Entry to City of Hope, they don’t have an ER. It’s a whole cancer hospital. But you have to enter it as an outpatient. By the time he decided that he wanted to go, he was an inpatient at UCLA. He could not leave the hospital. He was so ill. He was there for a month and we could never get him in. He came home for one night and was back at the hospital the next day. They never could get him strong enough so that he could be seen there. I kept telling him they were doing a special trial for his type of cancer and he needed to try to get there but he never did. I think the first thing that he said was, “It’s so far.” I said, “It’s only an hour and a half away. How far would you drive for life? And life more abundantly? How far would you go?”
What were the pathology results?
The results came in from my pathology. We went back to the doctor and the doctor said, “I’m so sorry. I thought that this was a superficial situation but you have a high-grade bladder cancer and these types of cancers, even though we removed the tumor, have a very, very high likelihood of returning.”
The good news was that — well, to me — he said that it hadn’t gotten to the muscle, but it was in the lamina propria, which is the lining that’s inside of the bladder and the bladder wall. He said that they took an extra sample just to make sure that they were not missing anything and that it was deeper than they thought it was, but it looked like there was no muscle in the tissue.
When he told us that, me and my husband began to celebrate. We were happy. We were thanking God for that because we knew that if it was in the muscle, that meant chemotherapy, bladder removal — all that was the next step. But if it was not in the muscle. I can at least try another treatment, which would have been BCG installation, so immunotherapy installations into my bladder over a series of times and then maintenance for 3 years. If there was no recurrence of the tumor, then I may be cured at that point.
The doctor said, “I’m so sorry. I thought that this was a superficial situation but you have a high-grade bladder cancer.”

What did your doctor say about your diagnosis?
We started celebrating and he said, “No! No! No! This isn’t anything to get excited about. This is serious. It’s a high-grade cancer,” and blah, blah, blah. I was telling him, “Excuse me. This is something to celebrate because today, I get to keep my bladder. I’m not worried about what’s going to happen in a year, two years, or three years down the line. Today, I get to keep my bladder and that is a blessing.”
Then he was like, “Well, I want you to go and have a second opinion with my colleague at USC.” I was thinking, “Excuse me. The way you have treated me, there’s no way that I will ever go to anybody that is associated with you because they will likely be just like you and I’m not doing it.” So I tell him, “No, thank you. We’re going to City of Hope.” And he said, “Why do you want to go to City of Hope? It’s so far. Is there a particular reason?” I said, “Because that’s where we want to go.” And my husband interjected and said, “I will take her wherever she needs to go. If we have to get on an airplane, we will be doing that.”
I was thinking, “Yes, we are those black people, not the ones that you think we are.” I sat there and thought, “How dare he?” The audacity to try to discourage me from going to an internationally recognized cancer treatment center because of the distance.
Did your doctor try to get you to stay in his care?
He said, “Well, we could do the BCG,” which is the immunotherapy here at the county, “but there is a BCG shortage.” This is true. There’s a national shortage of BCG because only one company makes it because there’s not a lot of money in it. It’s sometimes hard to get. I knew that, but I also knew, that if you’re in a cancer treatment center, they treat all kinds of cancer. These brand new drugs that are coming out that cost thousands and thousands of dollars, this same company makes those drugs also. They’re more likely going to make sure that they give them what they need first. I felt like I was going to get a better chance of getting my BCG and getting it on time if I went there as well.
These are things that we don’t think about as laypeople. Who would think about that? But this is something that I was able to think about and pre-plan. He wasn’t probably too thrilled about that. I said, “Thank you very much. I appreciate all that you have done. Goodbye.”
Describe the impact of doctors making assumptions about their patients
He had a picture in his mind of who I was and what my life was like. He already had his own stereotypical thoughts about who I was. Because if he didn’t, he wouldn’t have treated me that way. Not because I was his colleague, but because I was his patient. Maybe he treats all his patients that way, but as a black woman and seeing the type of health disparities that we have in particular compared to other groups, I thought that he felt he had the right to treat me the way that he did. He didn’t see me as a colleague, even though I was. He was seeing me as a black patient.
Why wouldn’t he say, “Well, you know, City of Hope’s an hour and a half away. Is that going to be a problem for you?” Why not say that? No, he just assumed that we couldn’t do what we needed to do or we wanted to do as far as my care went. My husband should have never had to interject and tell him, “If she needed to get on an airplane to go somewhere to get care, then I’m going to do that for her.” We shouldn’t have even had to have that conversation.

He didn’t see me as a colleague, even though I was. He was seeing me as a black patient.
I had an aortic aneurysm. I had a heart surgery at 39 years old. My doctor, my cardiologist, is a man of color. He is Indian. When I first went to him and was diagnosed and knew that I had to have open heart surgery, the first thing he said to me was, “Now I can do this surgery right here. But because of your age, I want to send you to San Francisco. I don’t know if you know this basketball player.” He was telling me about a basketball player who had the same thing, he had an aneurysm. And he said, “He plays with a vest on. He had his surgery in San Francisco and they did a great job. And I think because of your age, I really want you to go there.”
He never assumed that I wouldn’t be able to go there. He never assumed that we couldn’t afford to go there. He never assumed anything. He didn’t have any assumptions. He said, “In my personal opinion, you would receive the best care here. And this is where I would like for you to go if you could.” And that’s the approach that the other doctor should have taken, not just assuming that, “Why do you want to go there? We could just treat you here. That’s so far away.” Really? It’s only an hour and a half away. That’s not far. How far would you drive for the best chances? With the latest equipment and doctors that are doing research actively on your problem. Why wouldn’t you?
Switching Medical Care
Did that doctor say anything further to you?
He said, “You will never come back here.” I said, “Touché. I’m not coming back here.” He did exactly what we needed him to do — make the initial diagnosis and that was it.
Was your next medical team at City of Hope easier to work with?
Oh, it was so easy. The first thing I did was pull up their different offices. Come to find out, they have clinics all over. The closest clinic to us that has urology was in Santa Clarita. That’s only, from our house, 50 minutes or less. I think it probably takes us 45 to 50 minutes to get there. Right by Magic Mountain, really close. Then if there’s anything that needs to be done, like hospitalizations or anything like that, then you go to the other place or if you go there for a second opinion or something like that. But you can have your regular visits, including the treatment for cancer, right there in that office.
They have offices all over California, not just in Duarte. I just did my own research. I went and called City of Hope. I found out that they had other clinics. And the first thing I did was I looked at all the doctors. I was even willing to go to Duarte if I had to. And I was looking for a doctor that looked like me. Because I felt like I could trust a doctor that looked like me. Fortunately, I found one doctor.
Why is it important to find a doctor that aligns with you holistically as a person?
It’s the things I don’t have to explain—the culture. There are certain things that when you’re holistically looking at a person or a patient, in my perspective, when I’m taking care of patients, I look at them holistically. For example, in the clinic where I have my practice, probably 95% of my patients are Latinx—most of them farmworker families. The majority do not speak any English at all. I speak a little bit of Spanish, but I try to find out everything I can about the culture. I want to learn as much as I can about the culture because those are my patients. Those are the people that I’m seeing.
So when I’m taking care of them, I’m not just taking care of what’s right in front of me. I’m looking at them holistically as people, as a culture, as a community. And that’s what I felt like I needed in my health care. I need someone who knows the culture so I don’t have to explain every little thing to them and they know how to approach me as a person probably because they have some shared experiences with me.
Unfortunately, the doctor I selected was not a urologist. Urogynecologist but was not a uro-oncologist, which is what I needed for my problem so I had to pick someone else. And I did in the same office and it worked out really well for me.
What resources does the City of Hope offer for bladder cancer patients?

What helped me was their bladder cancer advocacy. There’s an organization that gives patients tons of information. It’s like the American Cancer Society for bladder cancer and I was able to go on there, pull articles, look at the actual standards of care, the procedure so I knew what was supposed to happen and that was the next step anyway. That second time, if it comes back negative for a muscle invasion, then at that time, they go ahead and start scheduling you after your bladder recovers, which is about 4 to 6 weeks after. Then they start you on their immunotherapy, which is an installation of the treatment into the bladder. I had to do that for 6 weeks.
The new doctor did the resection. I really liked her a lot. Liked her personality. She was very positive, which is what we were looking for. The resection turned out really well and then we’re going to start the BCG.
Finding a cancer support group
Before the resection, around the time that I transferred my care to the City of Hope, I joined a support group, a bladder cancer support group on Facebook. I started just looking for bladder cancer support and I found a couple of groups. One was women and bladder cancer. The other one was just bladder cancer itself. That experience of connecting with people that were going through the same things that I had gone through, that had gone through what I had gone through, so I could ask questions that could offer me support, that was invaluable. That was invaluable while I was going through my process.
In fact, I’ve met some lifelong friends since I joined the group. The first person I met was a woman who lived in New Jersey and she was diagnosed with the same cancer that I have, high-grade bladder cancer. However, hers was caught at an earlier stage so maybe she did one round of BCG, but she hasn’t had to do anything else. They’re just scoping her. But for me, my path was a little bit different.
Treatment
How did your body react to BCG treatment?
Once they did the first 6 weeks of BCG, during that time, I think I had one bladder infection that delayed the treatment for a week because I had to take antibiotics and then I had to go back and finish. At the end of it, they wait so many weeks and I believe it was 8 weeks and then they scope you.
On the eighth-week scope, we saw an area of my bladder. I had no new tumors that they could see, but they saw a bumpy area. There was a bumpy area and she just wanted to watch it. At that point, you would be having maintenance BCG immunotherapy every 3 months for whatever the prescribed time was going to be. It could be 2 years, 3 years, or 5 years. So maybe 2 years and then in year 3, you do it every 6 months. It just depends on how well your progress is going.
Describe what BCG treatment is
It’s an infusion directly in your bladder. You have to actually hold it in your bladder for 2 hours and then you can pee it out. The thing about it is when you start peeing it out, for the first – I believe it’s 4 hours – you have to put bleach in the toilet and be careful that nobody else uses the toilet because this is a chemical. With chemicals, there are side effects.
What side effects did you experience with BCG?
Some of the side effects I was having were that on the first day, I would be fine and on the second day, I would have joint pain, flu-like symptoms, tiredness, and fatigue. I might have pain with urination, and bladder spasms, and the more treatments I had, the more irritated it became. The BCG was better than chemo, but it was hectic because of the burning with urination. It didn’t matter what they gave you for the burning, it just was not going to do it. It might take the edge off, but that was pretty much it. It’s making your bladder raw on the inside too, to make the environment not conducive to growing the tumor.
»MORE: Cancer Treatment Side Effects
Building friendships through a cancer diagnosis

When I went back and saw the bumpy area, at the same time, I ended up going to New York because my son is a dancer and we went to New York for him to do an intensive. But I also have another son and son-in-law who live there. So we went to go visit them and I was able to actually have lunch with — I call her my cancer wife, my bladder cancer wife. I got to meet her for the first time and we had lunch together and it was the best.
You’d think we’ve known each other for years. It’s the best thing ever. I think we both cried because we had been going through this journey. We got diagnosed weeks apart and we have been going through this journey together, supporting each other. We exchanged numbers after meeting on Facebook and then we just started texting each other back and forth and we became really fast friends and we’ve been friends ever since. Sometimes I found myself calling her before I called my husband. That’s why I said she’s my cancer wife. Before the scan, she’d call me, I call her before her scans. We comfort each other. It’s so funny. This black lady and this little Jewish lady and we’re just like a year apart in age and we have just bonded to one another and she is truly my sister.
I’ve met her and then also Ebony. It was funny because when Ebony came on to the bladder cancer support group, she had posted something and there was something in the background of her picture or something that let me know that she was in the same sorority that I was in. So when I saw that, I got so excited, especially because there were not very many black people at all in the support group. There’s just not a high percentage of black people that have bladder cancer.
One, she’s younger than me, and two, she looks like me. I was so excited. I inboxed her and I said, “You know, I think you’re in my sorority,” and we started talking and then we exchanged numbers. We started texting each other and supporting each other. Across the country, we support each other and became friends on Facebook. She was at the beginning of her journey so it was really nice that I was able to talk to her, encourage her, and let her know what the surgery was like when I was going through the process of that.
I got to meet my friend, and that really solidified our relationship. Then the following month, I was to have my first maintenance dose of BCG, which was for 3 weeks, which is a lot better than the 6 weeks. And then 8 weeks later, I would be scoped.
The importance of making cancer connections
It’s very important. It keeps you going. It empowers you. I call my students, my nursing students, my baby birds and they call me mama bird. I have some students who have graduated and have gone on to have their own careers, one of which I became very close to, and she ended up having breast cancer. I was really supportive of her during her breast cancer journey, which was before I had bladder cancer.
You never know why people come into your life because I really believe that our relationship was orchestrated by God so when I got ready to go through my experience, I actually was going through it with someone who had already been through cancer before. We used to say when she was going through cancer, that I was going to help her write a book and the book was going to be, “You’re Not Helping,” about the things that people say to people that have cancer. The little things that they say, “You’re going to beat this,” little things like that. It’s like, “You’re not helping.” There’s a lot of things that people say and they think that they’re helping, but they’re not helping.
Cancer Community
What you should and shouldn’t tell someone with cancer
There are things that you can say that would be helpful. That’s why when people pass away, the first thing they say, a lot of people say, “I’m sorry for your loss.” And that’s not helpful. Everybody’s sorry. Yes, they’re sorry for your loss. What can you say? “I’m praying that God will support you and will send you peace and understanding.” “Is there anything I can do?” There’s the superficial kind of things that people just naturally say, like “Happy Birthday,” and then there’s the things that people say that have meaning that really go there.
And some people don’t know what to say, right? I have a lot of friends I didn’t even hear from when they first found out. Once they found out I had cancer, I didn’t hear from them anymore. I understand that it’s hard for you to wrap your head around my experience and what I’m going through but at the same time, this is the time that I need you the most. Don’t disappear on me. So having my own community of support outside of my own friends and family also took the pressure off of them. The things that I felt that they should have been doing to support me, I really didn’t need that because I had my community already that was there to support me and they were there to talk. They didn’t care about me talking about cancer for an hour.
How did it feel to find someone with the same diagnosis from your sorority?
I felt a real sisterhood. I felt a special bond with her outside of the cancer, which was nice. And then in my sorority in general, we have a very small chapter here where I live and we have lost, off the top of my head, over the last 15 years I think maybe 6 sorority sisters to cancer of various kinds: cervical cancer, breast cancer, mostly breast cancer, liver or pancreatic cancer. It’s just so strange that so many people from one small sorority have all these cancers that take place and it’s really been rough.
Experiencing loss of loved ones during a cancer diagnosis
During the time of my cancer, one of my sorority sisters here was diagnosed with stage 4 cervical cancer and she, in fact, passed away. When I started my treatment in January, she passed away in September. She and I had been really, really close. I had taken her to the hospital before her initial diagnosis. To be going through that experience and then have someone that you love and that you’re close to pass away from that experience, it’s a lot. That’s why the mental health side of it is even more important.
»MORE: Cancer and Mental Health
Through this journey, I’ve lost a lot of people to cancer. I was diagnosed in January of ’21, so it hasn’t even been 18 months yet and four people that are close to me have died of cancer — one of breast cancer, one of cervical cancer, both my sorority sisters from the same chapter. I had 2 first cousins that died 7 months apart. One we buried last month, stage 4 colon cancer. He’s a year younger than me and his brother died 6 months before that. Pancreatic cancer — 3 weeks from diagnosis to death. These are my first cousins. Like, we took baths together as babies. That was painful.
My cousin, who just passed away last month, and I were close. We were only 13 months apart and we got diagnosed a week apart. He had stage 4 colon cancer and then I had bladder cancer. So we’ve been walking together through this. It’s funny how the tables turn. We’re both encouraging each other on a regular basis, talking to each other every week.
What were the results of your next scope?
When I had my second scope after the three-week BCG maintenance, we went back in and that’s when my treatment took a different turn. When they went in to scope my bladder again, I didn’t have any tumors but that bumpy area had gotten bigger. The doctor said, “I want to take it out.” And I said, “I want you to take it out.” Now, thinking about that, what might someone else have done? You think about, well, if I was seeing this doctor over here or that doctor over there, just because it’s not a tumor, are we going to keep watching it? And keep doing the BCG? I was so happy that she wanted to do the procedure.

She went in, resectioned it, pulled it, took it out, and sent it to pathology. When she was in there, she found another small tumor that wasn’t even detected on the scope so she took that out too, and she sent that to pathology. That area that was flat and bumpy that came back was the same cancer that I originally had. It just wasn’t growing in the bladder. It was growing down. So it still had not reached the muscle yet. Thank God. It had gotten to that layer, but it hadn’t broken through to the muscle wall. Again, that makes the difference between chemotherapy and something else.
She also found another type of bladder cancer, CIS: carcinoma in situ. I had already done some research on that one and I knew that for most people who have that, it just comes back and back and back like it’ll be one now. Next time, it’ll be 3. Next time, it’ll be 5. And eventually, all roads lead to bladder removal for most people.
Bladder Removal
Deciding on the next course of treatment
I said, “Every time you weigh in all these treatments that I’m having, you’re rolling the dice that it’s going to get to the muscle. My bladder is actively trying to kill me. It’s my bladder or me. What’s it going to be?” I decided I’d rather it be my bladder to go. I said, “I’m going to stay here. I’m determined to be here. Right now, if I go ahead and do the surgery, I have choices on the outcome.” If you wait too long, one, it can get into the bladder wall. Two, it could get outside of the bladder wall. The wall of the bladder is very thin. It sits right on top of the uterus. Once it gets out, it goes quickly. People go quickly. You’re taking chances, and I’ve never been one to really take a lot of chances, especially with my life. I know my kids need me. I know my husband needs me. I have a lot of responsibility and I really want to be here. So I made the active decision at that point to have my bladder removed.
I talked to my doctor and when she gave me the final pathology, I said, “I really think that I want to have my bladder out.” And she goes, “You know, I was going to tell you, you could do inter-bladder chemotherapy, not systemic chemotherapy because it’s not in the muscle. We can put the chemo in your bladder but it may not work. It probably won’t, long-term. If it were me, I would do the same thing.” At that particular point, that was the reassurance that I needed. But I already mentally made up my mind that I was going to do it.
My bladder is actively trying to kill me. It’s my bladder or me. What’s it going to be?

Choosing a urinary diversion
At that point, it was a decision as to what type of diversion am I going to have. Did I want to have a bag? I said, “No, I’m 52 years old. Why would I want a bag if I don’t have to?”
The next choice was a neobladder, where they make the bladder out of colon and they put it back to where the old bladder was and you can actually urinate like usual. But there are some challenges with that. The first one is my urethra. I didn’t want to keep my urethra because that could have cancer later. Two was that usually the neobladder works better with men because women tend to have more incontinence and bladder leaking or retention.
If I have bladder retention, that means that I’m going to have to cath myself so I can pee. It doesn’t mean it’s going to happen every time, but it happens a lot. Then there’s leaking – we already have enough bladder leakage after you have so many kids. You’re going to cough, sneeze, pee, and wear Depends or a pad. I was thinking, “After all this, I don’t want to have to deal with any of that.” So for me, that was not the best choice.
The next thing was Indiana Pouch. And I knew that that was an option for me. The problem with Indiana Pouch is a lot of places, the doctors don’t know how to do it. Another thing that I would say when you’re advocating for yourself, think about where you’re going to get your care. Because if they don’t know how to do certain procedures, they’re not going to recommend those to you even if they’re the best things for you. If I don’t do that, then I’m not going to tell you to do that. I’m going to say you can do this or this. That’s left out because when you ask, “Well, can you do the Indiana Pouch?” They’re like, “Well, we don’t do those here.” Then sometimes we say, “Okay, well, I’m not going to do that one.” That’s another reason why I went to City of Hope because I knew that they did everything there and they may be doing some things that I don’t even know about. If it sounds right, I’m going to be down. I decided to do the Indiana Pouch.
Describe your experience with the Indiana Pouch
Great things about it, I can pee standing up. I have a problem with bathrooms, like public restrooms. For now, there is no problem with a public restroom. I can go to the porta-potty. I don’t have to touch anything. I don’t have to do anything in there. I don’t have to sit down. Unless I have to have a bowel movement, I don’t have to sit down in a public restroom.

There is a risk of infection because you are putting the catheter in the little stoma. People have 2 different types of stoma, 3 different types usually. The one that I have is really low, below my bikini line, so I can wear a bikini and you can never even tell. You would never know that I don’t have a bladder. Well, I do have a bladder, but it’s just not the regular bladder. Some people have one above the bikini line so that would show but a lot of times, they just put a waterproof dressing on it, a little small dressing like this, and it’s just on there.
Some people have it in their belly button, so they actually catheter their belly button. For me, that wasn’t an option because I had another surgery that wasn’t going to be a good choice for me. I didn’t think I wanted that anyway because some people end up with a hernia and I don’t want to deal with that either.
I went ahead and decided I would do the Indiana Pouch, so I just have a little catheter. It can fit in the palm of my hand. If I go to the bathroom, I just open it up. It’s all sterile. I can touch it and everything on the outside and I just feed it in. I stand there and I pee. I take it out, throw it in the trash, and I’m on my way. It takes less than 10 minutes. I may not have had that option had I waited because the cancer may have been to a point where that wouldn’t have been an option.
Circling back to your first doctor, what would have happened if you waited to get a resection like he’d wanted?
We could have waited before he did my resection, and in the meantime, it could have gotten bladder-invasive in the wall. Because these things grow fast. You need to have it out within 90 days. She resected my tumor. When I made the decision I was going to have my bladder out, I knew that I had 90 days to have my surgery because that might be a regrowth period and I didn’t want anything to grow back before I had my procedure.
My husband and I had planned to do a trip to the Dominican Republic. I said, “As long as I can go on my trip, the next week when I come back, I’ll be ready to have my bladder out.” And that’s what I did. I think we came back 5 days later and I had my bladder removed.
Quality of Life
Why did you take a trip prior to your surgery?

My thought was this, you never know when you’re having surgery what’s going to happen. I didn’t know. What if something didn’t go just right? I told my husband, “We’re going to go on this trip and we’re going to enjoy ourselves and have the time of our lives because what if we don’t get a chance to do this anymore? I want to make sure that we have a good time.” And we did. Fortunately, everything turned out well. I had a few little setbacks along the way during my recovery period, but I would not change anything. I’m so glad that I made this decision. And really, other than having to go to the bathroom on a schedule — every 4 to 6 hours, I have to go empty my bladder. But most women I know go to the bathroom more than that.
Considering your lifestyle when choosing a urinary diversion
For me, I thought about this. One, I didn’t want the bag so that was going to be out. That was not going to be an option for me. Also, I knew that if my other diversion failed, I could always go to the bag. You could always go to the bag later but you can’t go back once you decide you want the bag.
The other thing I thought about is if I have retention or bladder leaking, what hassle that’s going to be. This is for the rest of my life. Who’s going to catheter me when I can’t see down there? My husband? He won’t be able to see either. So who’s going to do it? But if I have the Indiana Pouch, if someone’s taking care of me, it’s really easy for them to take care of me. Someone else could do it really easily. It’s not difficult. They don’t have to go down there and try to find where to catheter me.
I thought about a variety of things. I thought about the right now. I thought about the future. I thought about the things that I like to do. My husband and I love to go to concerts, outdoor venues, and festivals. Usually, there are porta-potties involved. Is that going to be conducive to my lifestyle now? What about when we travel? We like to travel. We like to go overseas. Is that going to be a problem? All of these things are manageable with my diversion.
How has your diagnosis affected your love life?
Fortunately — and this is another reason why the support groups are really important — during the course of the support group when they do a surgery of this nature, it’s major. They not only remove your bladder, but they remove your ovaries, they remove part of your vagina because your bladder sits right on top of your vagina so there’s part of it that has to be removed. In some cases, they remove most of the vagina, especially if they think there’s a possibility that cancer has gotten through that. They take out your appendix and lots of lymph nodes.
When you’re thinking about being married, being young, and not having a vagina, that could be traumatic to your relationship. I never would have thought to ask but somebody in my support group brought it up and I talked to her and she became one of my close friends. When she had her bladder removal surgery, they removed all of her vagina except for maybe 2 inches. Which means that she would have to come back later and have a reconstruction of her vagina.
Advocating for vaginal sparing
I said, “Oh no, that is what I’m not doing. I don’t have muscle-invasive disease so it’s not out of my bladder. I do not want to have no vagina.” I talked to my doctor ahead of time and I said, “If I wake up and I don’t have a vagina, all hell’s going to break loose so we need to make sure that I wake up with a vagina.” She said, “We’ll do vagina sparing.” I said, “Yes. I want to make sure I have a working vagina.” It was very nice that I was able to consult with the plastic surgeon.
Another reason to go to these big cancer centers is because they have all that there. All these doctors are there. The plastic surgeon was there and he went through the procedure. I said, “If they get in there and there’s a problem, I expect to wake up and still have a vagina.” He told me the procedure. He said, “If they get in there and they have to remove everything, then I’ll either take part of your muscle from your thigh or from your abdomen and I will make you a vagina. So you’re not going to wake up and not have a vagina no matter what.” I said, “You promise I’m not going to wake up with no vagina?” He said, “No. I will fix it.”
Of course, you can go back. It seems like something small when you have cancer, but it’s not. It’s still quality of life. It’s living your life and living your life abundantly. It’s not just living life, right? I feel like I want it all. If I have to go through all this, I want to make sure that I’m going to have what I need to be happy and all those things.
One of the things I was able to tell Ebony because she was coming behind me was, “Make sure you talk to them about vaginal sparing and you don’t wake up like another friend and you only have a two-inch vagina and nobody told you anything.” She said, “I have a great husband.” There’s been a lot of people on the site whose partners have left them. They have cancer and their partners leave. One, because mentally, they can’t handle it. Or two, this situation. They can’t wrap their head around the fact that their sex life is going to be very different. So this is important. This is quality of life. It’s not just about living. It’s living your life abundantly and having the best life that you can possibly have.
Describe your experience with follow-up treatment
Now that the bladder is gone, I don’t have to worry about bladder cancer but, of course, I’m going to be monitored for the next 5 years. I think for the next 5 years, every 3 to 6 months, I have to be scoped. In fact, in 2 weeks, I have my next scope CAT scan, and then they’ll scope my pouch, because I don’t have a bladder anymore. Then after 5 years, every year for the rest of my life, I’ll be monitored. So scoped and probably CAT scanned to make sure that there’s no recurrence there or anywhere else. That’s a blessing to me.
Reflections
What advice do you have for someone on their cancer journey?
The only thing I have to share is, to listen to your body. If you feel like something’s not right, it’s not right. And it doesn’t matter if they say that, “Oh, everything’s okay.” You have to remember these things. If you die, they’re going to get another patient. When my patient dies, guess what? I get another patient. The only people who are going to be affected by my death are the people who love me, and I love myself.
If I feel like something is not right, I’m going to get a second opinion. Why? Because I’m entitled to one and that’s what I’m going to get. I’m entitled to do research and I’m going to do whatever research I need. Again, going back to, “The Lord helps those who help themselves.” Sometimes we ought to go out and help ourselves.

Get all the information that you possibly can and then you decide what’s best for you.
Don’t think as providers, because I’m a provider, I care about all of my patients. I do the best I can for them. But I am a human being as well. I don’t know everything, so you can’t put 100% of your life into your healthcare provider’s hands all the time. Every situation is different. And if something doesn’t feel right to you, it’s probably something that’s not right. If it doesn’t feel right to you, you’re obligated to find out so that you do feel right about whatever it is. Don’t always listen to what everybody else does. You have to do what’s right for you.
Get all the information that you possibly can and then you decide what’s best for you. You’re the one that’s going to have to live with your decision. I couldn’t let anybody else make this decision for me as to what type of diversion I was going to have because it was my life and I’m the one that’s going to have to deal with it—no one else. No one else cares how I pee. They may have had an opinion about it, but they’re not the ones using a catheter. They’re not the ones getting up in the middle of the night. They’re not the ones who have to see if they have an infection or not. It’s me. I’m the one. That’s what I have to say: put yourself first or whatever it is that you feel. If you feel that something’s wrong, then usually it is wrong. Don’t have expectations that somebody else cares about you more than you do.
More Bladder Cancer Stories
Vickie D., Bladder Cancer
Symptoms: Intermittent pain in the gut and burning sesnsation
Treatments: Chemotherapy (dd-MVAC), surgery (cystectomy)
Michelle R., Recurrent Bladder Cancer, Stage 1
Symptoms: Irregular occurrences of seeing streaks of blood in urine, specific type of pain when bladder is full, unexplained weight loss, urinary urgency, malaise, fatigue
Treatments: Chemotherapy (gemcitabine), surgery (TURBT: transurethral resection of bladder tumor)
Margo W., Bladder Cancer, Stage 1
Symptom: Blood in urine
Treatments: Chemotherapy (methotrexate, vinblastine, doxorubicin & cisplatin), surgery (radical cystectomy)
LaSonya D.
Symptom: Blood in urine
Treatment: BCG immunotherapy, cystectomy (bladder removal surgery)
Symptom: Clumps of blood in urine Treatments: Surgery (bladder removal, Indiana pouch), BCG immunotherapy



