Manda’s Stage 2B Relapsed Hodgkin’s Lymphoma Story

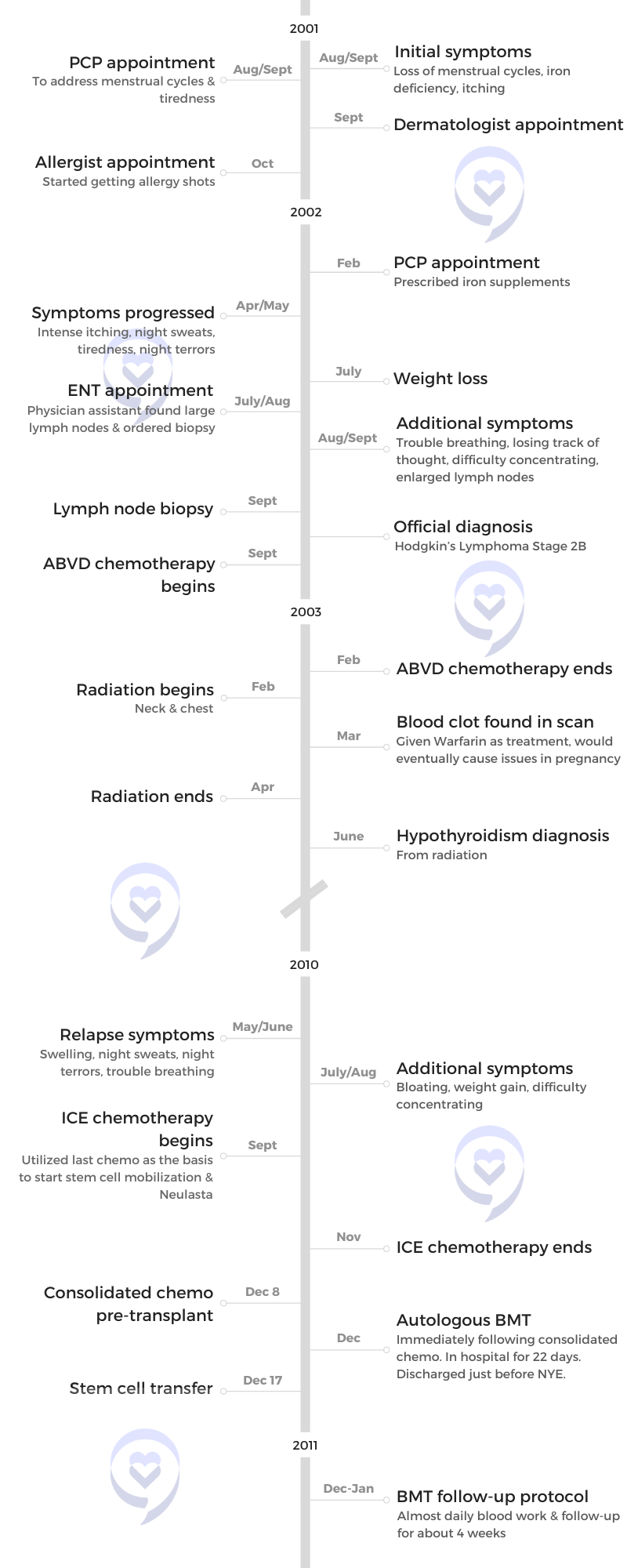
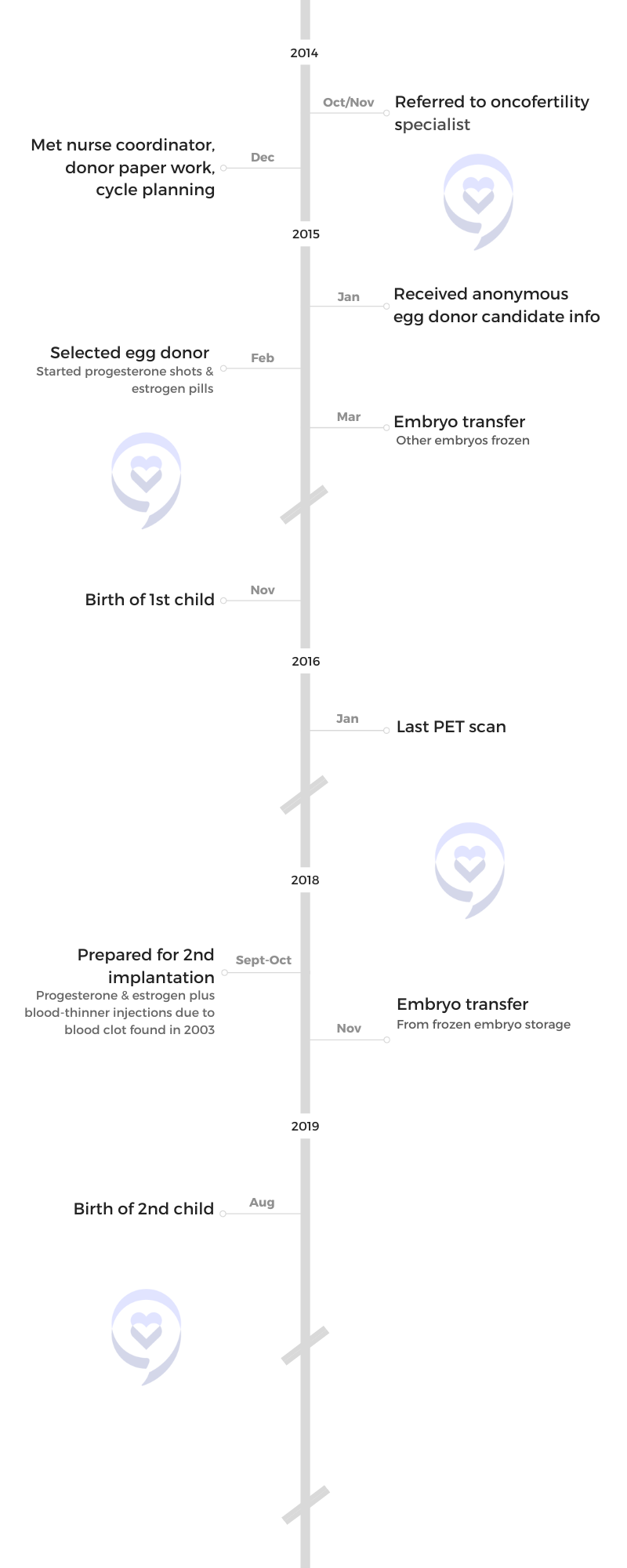
Manda was diagnosed with stage 2B Hodgkin’s Lymphoma at 19, which relapsed after eight years.
She shares what it was like being a young adult with cancer and the importance of knowing your fertility preservation options, no matter your age.
- Name: Manda M.
- Diagnosis:
- Hodgkin’s Lymphoma
- Staging: 2B
- Symptoms:
- Loss of menstrual cycles
- Iron deficiency
- Itching
- Night sweats
- Tiredness
- Night terrors
- Trouble breathing
- Difficulty concentrating
- Enlarged lymph nodes
- Treatment:
- ABVD chemotherapy
- Radiation
- Relapse Symptoms:
- Swelling
- Night sweats
- Night terrors
- Trouble breathing
- Bloating
- Weight gain
- Difficulty concentrating
- Treatment:
- ICE chemotherapy
- Autologous bone marrow transplant
“I wish I would have asked about fertility, honestly… I could have frozen my eggs or I could have prepared for what’s next.”
Thank you to Seagen for its support of our patient story series! The Patient Story retains full editorial control of our content. The interview has been edited only for clarity.
- Pre-diagnosis
- Initial symptoms
- What was going through your head?
- Diagnosis
- Treatment
- Getting diagnosed with hypothyroidism after radiation
- Being a young adult with cancer
- What was that like being 19 & having to reconfigure your college life to this?
- How did you cope with seeing your peers live normal lives?
- How did you open up about your diagnosis?
- Was there any talk of fertility preservation or family planning options?
- Is there anything that you would have done differently?
- Importance of knowing your fertility preservation options
- Relapse
- Treatment
- No evidence of disease
- Fertility preservation & family planning
- What was the big difference between being diagnosed at 19 & again at 27?
- Did you bring up fertility or did somebody else?
- How did you process the news?
- Meeting with an oncofertility specialist
- Deciding to have children after cancer
- Process of choosing an egg donor
- Fertilization & preparing for embryo transfer
- Financial impact of IVF
- Importance of fertility preservation options
- Words of advice
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Pre-diagnosis
Tell us about yourself
I am 39 years old. I currently work in strategy and business development. I have two children and a husband.
I grew up in western North Carolina. I stayed in North Carolina [and] live here still. As far as hobbies go, I like to be outdoors. I play with my kids and just generally like to hang out with my family.
My son, he’s six. He’s very empathetic. He understands emotions so he can tell when I’m not happy and he likes to give me a hug when he sees that.
My daughter, she’s just goofy. She does goofy things and she tries to make everybody laugh.
Both of my kids are very independent. They like to do things themselves and they get upset when they can’t do [them]. They’re just really good kids. I think they’re just exactly like they should be. When they get on my nerves, I’m like, You’re my miracle children. I remind myself, You willingly had these children.

“I knew something was wrong because I just didn’t feel quite right.”
Initial symptoms
It started back when I was ending high school and the summer after that. I was having a lot of interesting symptoms in terms of itching and my menstrual cycles. I told my mom and she started to look into different doctors that I could go see.
That progressed into a little bit more intense itching. Then I started to have trouble sleeping. I had already started college, into my sophomore year. That’s when the intense symptoms started to happen.
I went to the dermatologist first because it was itching and it seemed like a logical thing to do. Then I started to feel like, “Maybe I’m allergic to something,” and so my PCP sent me to an allergist. They tested me for a lot of things and decided that I was allergic to a couple of different things so [they] started giving me allergy shots. Then I just kept seeing individual specialists for individual things.
“My mom kept taking me to doctors to try to figure it out because she saw that I was not myself during that whole year that we were seeing specialists.”
What was going through your head?
I knew something was wrong because I just didn’t feel quite right, but I had started college and so things had changed from a lifestyle perspective. Maybe I wasn’t eating as well, I wasn’t exercising as much, and maybe I was stressed out. I just thought, Maybe it’s just the new normal.
But then I would go to the doctor and just be like, “It’s still not fixed.” My mom kept taking me to doctors to try to figure it out because she saw that I was not myself during that whole year that we were seeing specialists.

Finding swollen lymph nodes
I came home from school one break during my freshman year and my dad was like, “Why is your neck so big?”
I don’t think anybody thought lymph nodes because he was just like, “What are you doing?” I think you just think college. She must be getting into stuff she’s not supposed to be getting into and so that’s where it left off. I didn’t think of it then. It’s all hindsight.
Biopsy scheduled
I went to the ENT in Claremont, North Carolina, where I grew up and my parents specifically said, “Can we get a surgeon in Chapel Hill?” Because that’s where I was going to school. It took a little bit to make that all happen.
Did you think that cancer was a possibility?
No, that hadn’t even crossed my mind, actually. I thought maybe I just had mono or some infection that just had gone crazy.
Lymph node biopsy
I can’t remember exactly, but I know it was outpatient. It was just at the surgeon’s office. I didn’t go to the hospital or anything. I don’t think there was a complete incision. I think he just inserted something in there.
‘He’s in with a patient, but I can get ahold of them for you. You just stay on the line.’ That would have been a red flag because usually, they don’t drop everything.
Diagnosis
How did you learn that there was something serious going on?
A week had gone by and I haven’t heard from the doctor. My parents were constantly asking me. Finally, my dad was like, “We’re coming up and we’re going to figure out what the answer is.” They came up to Chapel Hill and called the surgeon’s office.
My dad was on the phone. My mom and I were sitting with him. The receptionist was like, “He’s in with a patient, but I can get ahold of them for you. You just stay on the line.” That would have been a red flag because usually, they don’t drop everything.
The surgeon came on the line and then my dad, I just saw his face drop, and that was when they were like, “Your daughter has Hodgkin’s lymphoma.” I looked at my dad and was like, “What’s happening?” He was like, “You have cancer.”
My dad, I just saw his face drop… I looked at my dad and I was like, ‘What’s happening?’ He was like, ‘You have cancer.’
What was it like hearing from your dad that you have cancer?
It was just weird because I didn’t actually get it from the surgeon. It was relayed from my dad, which, now that I think about it, probably was good because both my parents were there at the same time.
He’s stoic. It’s almost as if it was a relief because finally, I know what’s going on. But also scared, obviously, because I didn’t quite understand what it meant. A little uncertain and nervous about it.
Reacting to a cancer diagnosis: how cancer patients feel in the moment »
Treatment
Starting treatment & deciding where to go
Choosing where to go was pretty easy because I was on campus already at UNC and they have a UNC Cancer Hospital there. That process went pretty quickly. I got in to see them within a week or two.
At that point, it was just talking about what the next few months were going to entail. I decided to stay there because they’re on campus so I could walk to treatment. It made it easier because I had everything I needed to reduce my course load.
I had ABVD every other Friday. My parents would come up and I would meet them at my class. They would pick me up, take me to outpatient chemotherapy, and then take me home for the weekend.
Side effects from ABVD chemotherapy
My major [side effect] was nausea and vomiting. I would actually start vomiting before I even got treatment because I was just so nervous. I think they called it anticipatory nausea. I would sit in my biology class and start getting sick without any treatment.
I did have some hair loss. I got my hair cut really, really short so it looked like I just had a really short haircut. It was falling out. But, at any given point, I don’t think I went entirely bald. Ultimately, nausea, vomiting, and the general overall ickiness that I felt [were] my main [side effects].
Managing nausea and vomiting from chemotherapy »
Side effects from radiation therapy
I just had a really, really sore throat. I actually ended radiation about a week before the last day of classes. I thought it would be cool to take a shot of something to commemorate the end. That was the worst thing I could have ever done because it just burned my throat down.
I went to my radiation oncologist. “I am sorry. I can’t do that,” and he was just laughing. He was like, “I’ve seen it before. There [are] a lot of college students that have come through here who’ve had cancer and radiation. I understand. Here’s the stuff.” He gave me this liquid and then he was like, “Take it like a shot.” I was like, “Okay, fine, whatever. I deserve it. I’m never doing that again.”
A month later, I had no problems. I would say after that, my radiation oncologist was really adamant about testing me for hypothyroidism. He was constantly checking my thyroid. That ended up being a long-term side effect of the radiation treatment.
Learn how other cancer patients got through the different side effects from cancer treatment »
Getting diagnosed with hypothyroidism after radiation
It wasn’t too bad. It was just understanding that for the rest of my life, I have to be tested for this and make sure my blood work is okay. But other than that, it was just trying to find the right dosage and sticking with a plan [to] make sure that you’re getting the right dosage over time. They walked me through that and then my primary care physician was brought on board. He understood what was going on.
Now it’s just routine where every couple times a year, I go and make sure my thyroid levels are correct. Then they [adjust] the medication [as necessary] to keep it stable.
It helped to be on campus and have that normal life because I didn’t really want to stop everything all at once.
Being a young adult with cancer
What was that like being 19 & having to reconfigure your college life to this?
Looking back, it was probably the best thing I could have done because it gave me normalcy. I think if I moved back home and just stopped everything, I would have been unhappy. Having my friends around and a normal college life was actually helpful. Now, my GPA probably wouldn’t say the same thing, but as a person, it helped to be on campus and have that normal life because I didn’t really want to stop everything all at once.
I actually met someone who had Hodgkin’s, an undergrad who was in law school at the time. The doctors put me in contact with him. He was like, “It seems daunting, but I think with the reduced course, you might be okay,” because he had done the same thing.
I was able to take my course slowed down to less than half and still be considered a full-time student. I took his advice. He was really helpful during that whole time.
I don’t know if I took it in stride. I felt like I didn’t really have a choice so I had to do it. It was probably the best-case scenario for me that I was at a campus that had a really great cancer hospital. It almost felt like it fell into place a little bit so it helped drive my decision-making.

How did you cope with seeing your peers live normal lives?
I found my people. I had some really great friends who were willing to change their lifestyles for me. They knew that I couldn’t go out and have fun on most nights after treatments or when I got back.
My parents would drop me off after treatment. I would go home with them on Friday and then they would drop me back off Monday morning. Monday evening, my friends would come over with takeout and they would just watch a movie with me. It was just really having a support system that helped and allowing my friends to just be.
Sometimes they would come and sit with me during treatments. My parents were there but just knowing that they’re there was nice.
I found my people. I had some really great friends who were willing to change their lifestyles for me.
[Don’t] try to push people away. I felt like I can’t really make friends now because I’ve got all this stuff going on but [don’t] let your mind go there. Your friends want to help you and they want to be with you. It may not be ideal, but they’re willing to put the effort into helping you, too.
It was cool because UNC is a really big sports school. But if [my] platelets were low or [my] white blood cells were low, I can’t go. They were like, “Let’s just do something else.” They were really good about including me in things that they knew that I could go to and I wasn’t going to get sick.
Your friends want to help you and they want to be with you. It may not be ideal, but they’re willing to put the effort into helping you, too.
How did you open up about your diagnosis?
After the first diagnosis, I was pretty open to people about it because it was a huge part of me. I felt anybody that I was romantically involved with should know and just could tell if it was going to be a problem or not
A lot of my friends already knew because I was still talking with the same friends. The new friends that I had made maybe weren’t really privy to it, but I felt like they were really just supportive, good people so I didn’t worry too much.
I honestly don’t know how you would bring it up to people who don’t know. There’s a certain part of your life where you just think you’re never going to get it again so why bother telling people about it.
It’s just a select few where you’re like, Maybe this person should know. I just felt that way, at least with my boyfriend, because we had been dating for a long time and there was something there. I should probably make sure that he knew a lot about my health history.
How to tell your family and friends you have cancer »
Was there any talk of fertility preservation or family planning options?
No, not at that time. Doctors never really mentioned it and I never really said anything because I just wasn’t thinking about it. I wasn’t really prepared to ask questions.
Is there anything that you would have done differently?
I wish I would have asked about fertility, honestly. I had just read everything about Hodgkin’s lymphoma, how usually it’s cured, and you never really have to deal with it again.
There was a span of eight years between my first diagnosis and then it coming back. I could have done something. I could have frozen my eggs or I could have prepared for what’s next. Even if I wouldn’t have needed it, it would have been nice to have had that opportunity to know that there is a chance that this could happen.
It’s not really part of the treatment plan going forward and so I just never really thought about it. I wish I would have.
Now, when I talk to other 19, 20-year-olds that are going through this, I’m always like, “You think you don’t need it and you may never need it, but just be sure that you ask about infertility and if there [are] options for freezing your eggs.”
Learn about fertility options before and after cancer treatment »

I’m a cancer survivor, but I’m still dealing with a lot of other things because of that.
Importance of knowing your fertility preservation options
At that time, I feel like [the] doctors did what they were supposed to do. They cured my cancer, but they didn’t really tell me what’s life after that. What are the things you might have to deal with later? And it’s not just infertility.
I had hypothyroidism, which they told me a little bit about. But then you have the potential for heart problems, lung problems… There was a blood clot I had that ended up showing its head 20 years later, in terms of things that I had to go through during my pregnancies.
The cancer’s gone but then [there’s] all this other damage in the process that I wasn’t really privy to. You go through your health history and doctors are like, “Oh, okay. Well, that could be a problem,” then you have to deal with it over and over again.
I’m a cancer survivor, but I’m still dealing with a lot of other things because of that.
I didn’t even bother going to my primary care physician. I just knew.
Relapse
What made you think something was wrong again?
I just didn’t feel right. I didn’t even bother going to my primary care physician. I just knew.
I tried to shove a lot of things into a couple of months that I know I really wanted to do. Then I was like, “Okay, now I’m ready to go tell somebody that this is back.” And that’s how that started in 2010.
‘I think I’m going to go to the doctor because I think something’s up.’

Why did you decide to do a last hurrah before seeing your doctor?
I met my boyfriend, who’s now my husband, back in 2006. I had given him an overview of what I had gone through in 2002 and 2003 so he understood what was going on because he knew that I was getting scans and stuff still for that.
Then in 2009, I started grad school. In the back of my head, thinking, I really want to get through grad school. I want to marry this guy and start my life. When 2010 rolled around and I started feeling a little off, I was like, Uh-oh. Maybe this isn’t the plan anymore.
I scheduled a vacation for the summer between my 2009-2010 grad school year. There were a couple of steakhouses I wanted to eat at because once you’re on chemo, you don’t like to eat so I went and ate at some of my favorite places.
Then finally, I was telling my parents and my boyfriend, “I think I’m going to go to the doctor because I think something’s up.” They knew that if I were saying something, I probably felt it.
I knew that it was going to take over my life for a while and I just wanted to make sure that I had some nice memories to fall back on once it started doing that.
Why did you decide to wait?
How much worse can it get in two months? I went a whole year without treating it last time so if I spend the next two months just trying to get things settled, then I felt like I could do it.
I knew that it was going to take over my life for a while and I just wanted to make sure that I had some nice memories to fall back on once it started doing that.
Was there a worry?
There was [a] worry I wouldn’t be able to enjoy, that my boyfriend would probably not want to stick around — which wasn’t the case, by the way, but it was in the back of my head. This is just going to wreck my life and so let’s just savor it for the last few months and then deal with it as it comes.
Official relapse diagnosis
I was like, “What stage is it?” They were like, “We don’t stage. We just say it’s recurrence.”
Treatment
ICE chemotherapy & autologous bone marrow transplant
They were pretty much adamant about [getting a bone marrow transplant] from the beginning. That was going to be the endgame
[With] ICE chemotherapy, I did a lot of my own research and I realized that it was pretty serious. They told me, “It’s intense. You would have to be in the hospital over three days in order to get the treatment.”
I don’t remember how many weeks I had in between, but it took a good chunk of that time to get healthy enough to even think about having the next one. There were a couple of times where we had to postpone, which didn’t happen with ABVD.
They had to postpone because my platelets had tanked or I [needed] blood transfusions and wasn’t healthy enough to get the next treatment. I had never had a blood transfusion before then. I can’t even keep track of how many blood transfusions I had over the span of those ICE treatments.
Then being really, really careful about not getting sick. During the pandemic, I was joking around with a friend, “This was my life in 2010 — always wearing a mask and never going anywhere,” because you just didn’t want to get sick. You wanted your next treatment because you didn’t want to postpone it again and again.

No evidence of disease
How is it thinking about that?
It seems like time has flown by. It doesn’t feel like it was 12 years ago because some things are still very vivid in my memory and other things are really fuzzy.
Thinking back on it, I’ve forgotten a lot of things as well. I don’t know if that was on purpose or my mind was just like, Maybe we should just shove this way far back because you don’t want to remember it.

Fertility preservation & family planning
What was the big difference between being diagnosed at 19 & again at 27?
At 19, it just wasn’t there at all. You spend a lot of your teenage years thinking, I can’t get pregnant. Don’t get pregnant. Then in [my] 20s, especially since I was in a committed relationship, I thought, Oh, I can see myself being a mom. It was pretty much at the forefront for me and the doctors as well.
The second time around, they actually mentioned about fertility and the impacts that my treatment would have on it. It went from being nothing to something that was talked about quite a bit when I was older.
Did you bring up fertility or did somebody else?
The doctors actually brought it up, but they brought it up in a really weird way. I couldn’t quite comprehend it at the time. I had to start treatment pretty quickly the second time around so there wasn’t really time to even think about freezing eggs or anything like that.
I was just laying in the hospital bed and a fertility specialist came in. I just received some of my ICE treatment and they were like, “Freezing your eggs is just not an option for you. This treatment, along with the bone marrow transplant, is underway and there’s just not going to be an option for you to have children.” It’s what I took from it. My mom, who was sitting there at the time, was just like, “Wait. She’s not really comprehending this,” because I was on medications.
They definitely had to explain it to me a couple of times. My BMT doctor also reiterated, “Let’s just get you better and we can talk about this later. But as of right now, there’s not going to be too many options for you.” I just took it as I guess I’m not going to have kids.
At that point, I was almost done. Let’s get this over with. Just get me better and then I’ll deal with it later.
How did you process the news?
It was just like mark this down. It’s another thing that’s just not happening. Okay, I guess grad school is on hold. Not happening. Maybe I’m not getting married. Why would this guy stay with me now that I can’t have kids? Let’s just keep marking things that aren’t going to happen.
At that point, I was almost done. Let’s get this over with. Just get me better and then I’ll deal with it later. You get a lot of bad news all at once and so it was a little bit disheartening. But the real thing that I really [wanted] was just to be done with the treatment. Let’s just get this over as fast as possible.
I talked to my parents quite a bit and my siblings. A couple of times, I called my dad crying, “All my hair’s falling out and all this is happening.” He would just be, “This is par for the course. Why are we crying about this?” And I was like, “Well, you know…” And he’s like, “You just have to keep pushing forward.”
I think it just all stemmed from because he had gone through a lot of stuff that I couldn’t even imagine. He was just like, “Sometimes, things just don’t go your way and you just have to go through it anyway. Just know that it can be better after it’s done. But it’s going to be worse before it gets better.”
There were just people like my dad who were like, “You can’t get down on yourself too much. Otherwise, you’re not going to get through this.” I think that was helpful to have that perspective of somebody who can just be like, “Pull up your big girl panties and just get it done.” That’s his mentality and that helped because otherwise, I would just sulk around and do nothing.
Feel bad for yourself, cry, and then get up and move on. Okay, fine. I’ll feel sorry for myself today and then I’ll move on. And so I tried. I tried waking up every day and like, “Okay, what’s the one good thing I’m going to do today that makes me feel good about myself?”
Find answers to the most popular fertility and cancer treatment questions »
Meeting with an oncofertility specialist
I went in for one of my scans, maybe my third-year scan. “Look. I got married and I’m thinking about having children and I just need to know my options. I don’t know what they are.” He’s like, “Oh, okay. Let me refer you to a fertility specialist that works with cancer patients.” I was like, “That would be wonderful.” Why do I have to ask for this?
He referred me to her and that got the ball rolling on understanding what my real options were. If I really wanted to have a kid, then let’s make this happen and this is how it’s going to happen.
It’s interesting because it’s still very much related to cancer. I wouldn’t be infertile if I hadn’t had cancer. It keeps coming up over and over again.
First, she wanted to see physically where I was from a fertility standpoint. She did ultrasounds, took bloodwork, and confirmed what we had suspected that physiologically, I was going to be able to have a child in the traditional way. She confirmed all of that.
Then she took me and my husband and [went] through the different possibilities. There was surrogacy, adoption, frozen embryos that can be donated, and IVF with an egg donor. She laid out all those things and was like, “I think you would be a perfect candidate for IVF with [an] egg donor.” Then we just talked through what that process would be and why she thought that that would be a good option for me.

I could carry a pregnancy and then my husband could actually be the father of the child. We could plan it so that we could use multiple embryos from the same donor and they would actually be full siblings to each other.
She said, “The good news is you have a cute uterus.” I was like, “Oh, okay. Good to know. I didn’t know they could be cute.” The silver lining is that [I] have things that are still functioning in [my] body so let’s go, let’s use them. I thought that was pretty, pretty nice.
The bad news is that I was fully in menopause. My ovaries were not working. She even showed me a picture. They’re supposed to look like chocolate chip cookies, I think, and mine didn’t.
She reiterated, “A lot more people have to use this route than we think,” and made it sound more like it’s a normal way of doing things. “It’s being done, people are using it, and it’s working so it’s going to work for you. We have a really high success rate with this.” She was just really confident and very hopeful that this was going to be the answer.
During the whole conversation with me and my husband, [there] was never a moment where she didn’t think there was an option. “We’re going to get you pregnant. You’re going to have a baby. This is the way to go.” She was just very confident.
The whole time, I was like, “Well, I don’t know if this is going to work or anything.” She was just like, “Yeah, it’s going to work. I know what I’m doing.” It was just refreshing to have someone who was just like, “This is done all the time and it’s going to happen for you, too.”
I also have a little bit of reservation. Will she be a little bit upset that I’m a cancer survivor and that maybe I shouldn’t be having kids? But none of that came up. “You’re fine. You’re five years out. Your doctor gave you the go-ahead. We’re doing this.”

Deciding to have children after cancer
Should I bring a child in this world that may have a mom that has cancer for [the] third time? A part of me was like, Maybe I shouldn’t have kids because I don’t want to put them through that process. But I thought, If I live that way, then I would never do anything.
I just thought through that a lot more because I wouldn’t want a child to have to see me suffer. But I quickly understood that I couldn’t live my life thinking that it would show up a third time.
It was just understanding that I got to point B in a really interesting way. And it was miraculous in some instances. When I think back about all that I went through and now that I look at my kids, I’m like, “They are truly unique and never would have existed had my story not existed.” When I think about that, it’s almost as if I would go back and do it all over again to get the same exact thing because it made it all worth it [in] the end.
It wasn’t the path I thought [I] would take, but I got what I had hoped for so why would I change that?
Before we could do the IVF, we had to go through counseling because it’s very important that your children understand where they come from and they were giving us pointers about how you talk to them about it. I just always tell them, “You are incredibly special because you came around in unfavorable circumstances. A lot of things had to happen for you to get here in a weird kind of way and so that kind of makes you extra special.”
It wasn’t the path I thought [I] would take, but I got what I had hoped for so why would I change that?
Process of choosing an egg donor
It was way easier than I ever thought it would be. They were really on top of it — the fertility doctor, all of her nurses. They walk you through the whole process and make it super easy.
They already had donors lined up that they thought met my expectations. I wanted someone who was Caucasian because I wanted them to look like me and my husband. I wanted someone who had a fairly good health history so they test them for a lot of different genetic diseases. As far as eye color [and] hair color, none of that really bothered me. I just wanted to make sure that they were healthy and kind of looked like me; that was my only thing. They were like, “Are you okay with having a first-time donor? We may not know if she’s going to be able to produce eggs or not.” I was like, “Yeah, that’s totally fine, too.”
I didn’t have too many requirements so they had quite a few donors that met the requirements and a little bit more. The donors can tell you about their ambition, their goals in life, what they do now, their personality, what they like to do, if they own pets, and the reason why they’re donating.
This particular donor said she was donating because she watched her aunt go through a lot of infertility issues. She felt because she was healthy and at an age that she could donate eggs that she wanted to do that in honor of seeing her family member go through this.
If this doctor is for real, this is happening… And it did. The first implantation worked.
Fertilization & preparing for embryo transfer
That process was lots of shots, lots of hormones, lots of things to make my body do things that I hadn’t done in years because I’ve gone through menopause at that point. That whole process was just injections and getting my uterus ready for implantation and then sustaining a baby after it was implanted.
There was a little bit of nervousness because if this doctor is for real, this is happening. At this point, I should probably start preparing to be a mom because this is going to happen.
And it did. The first implantation worked.
Financial impact of IVF
I know that they had financial help. You could pay over time or you could pay a set fee for three tries or something like that. I had opted out of the three-try one just because this is a lot of shots and I don’t know if I can do this for three rounds of IVF.
Because I had known that this was going to be the issue, we had prepared pretty well financially. When we met with the doctor, we knew it was either going to be adoption or something else. We knew that we would have to save up some money if we were going to do this and so we had been saving for quite some time.
The interesting thing is that [with] the first one, nothing was covered. It was a good sum of money.
Since then, I think some insurance companies do actually cover infertility because for my daughter, I was able to cover the implantation. Things have changed a little bit. I joke around with my kids that I need a return on investment because [they’re] expensive.

Importance of fertility preservation options
It’s just part of the cancer journey. It’s part of the treatment, really, and I don’t think people understand that. It just should be a part of how you treat it.
A lot of times, it ends after that last scan and you’re on your own. But it just really isn’t that way. There’s a ton of things that aren’t included in that treatment plan that should be. And I don’t really know how to fix it because I don’t know if that’s [an] oncologist issue. There’s just no guidance after or any help or understanding of what specialists [I] should have in place for the next 10 years in my life because I’ve gone to all kinds of specialists since then.
Just some understanding of what’s going to happen next and the things that you need to look out for because not every primary care physician is going to know what you need. You need to know yourself. It would be nice to have somebody guide you through how to advocate for yourself and where you need to go when you have these things happening to you.
I just tried to do a little bit every day. If I didn’t feel like doing any of it, I didn’t really get down on myself.

Words of advice
One of the things I really took to heart during that time… One of the PAs (physician assistant) who had had non-Hodgkin’s lymphoma and had worked with a lot of cancer patients came into my room. I was getting really down. He was like, “If you lose hope, then you lose everything. You just got to come in here and do your time. That’s all I’m asking you to do. Just come in here and do your time.” I was like, “It’s like prison here.” And he was like, “Yeah, like prison. Come in, do your time, but don’t lose hope.” And I was like, “Okay.”
I felt like I basically handed my body over and said, “I have no control over this thing anymore. You guys do your thing, get it better, and then hand it back to me when it’s done.” I just checked out mentally the whole time I was in my BMT. It was almost as if I was detached from what was going on because I had no control over it. It was just a really weird experience.
My advice would be that you just can’t lose hope and just do your time because there’s literally nothing else you can do. I think that was what he was getting across. Being here is all you can do right now. Just be here. That’s what I took to heart. Just sit here and do my time. There’s nothing else I can do.
I just tried to do a little bit every day. I didn’t try to make crazy goals for myself. I would say to myself, “Okay, you get up and you get a shower today and that’s a win.” And so I would just try to get up, shower, and then go back to my bed. But that was a win. I got up and showered. Just make small goals.
One day, I was like, “Okay, now you’re going to go for a walk around the neighborhood for five minutes and that’s it.” Tiny little steps day by day, trying to do something that maybe I didn’t do yesterday.
If I didn’t feel like doing any of it, I didn’t really get down on myself. I was just like, “Today’s not the day,” and tried to start over again the next day. Every day was like a new day, basically, where I had one small goal and that was it. I didn’t really get down on myself if I didn’t achieve that goal, but I tried really hard to see if I could.
‘If you lose hope, then you lose everything. You just got to come in here and do your time. That’s all I’m asking you to do. Just come in here and do your time.’

Inspired by Manda's story?
Share your story, too!
Hodgkin’s Lymphoma Stories
Jessica H., Hodgkin’s Lymphoma, Stage 2
Symptom: Recurring red lump on the leg (painful, swollen, hot to touch)
Treatment: Chemotherapy
Riley G., Hodgkin’s Lymphoma, Stage 4
Symptoms: • Severe back pain, night sweats, difficulty breathing after alcohol consumption, low energy, intense itching
Treatment: Chemotherapy (ABVD)
Amanda P., Hodgkin’s Lymphoma, Stage 4
Symptoms: Intense itching (no rash), bruising from scratching, fever, swollen lymph node near the hip, severe fatigue, back pain, pallor
Treatments: Chemotherapy (A+AVD), Neulasta
Brescia D., Hodgkin's Lymphoma
Symptom: Swelling in the side of her neck
Treatment: Chemotherapy: 6 rounds of ABVD





