Wade’s Stage 2A Hodgkin’s Lymphoma Story
Wade was only 18 years old when he was diagnosed with stage 2A Hodgkin’s lymphoma. Explore his story below, where he details his ABVD chemo experience and what it was like being an AYA (adolescent young adult) cancer patient.

- Name: Wade W.
- Age when diagnosed: 18
- Diagnosis:
- Hodgkin’s lymphoma
- Stage 2A
- Status:
- Remission after 1st-line treatment
- 1st Symptoms:
- Enlarged lymph node
- Found second enlarged lymph node
- Tests & Biopsies
- Ultrasound
- Excisional lymph node biopsy
- Bone marrow biopsy
- PET/CT scan
- Echocardiogram (transthoracic)
- Pulmonary function test (PFT)
- Treatment:
- ABVD chemotherapy regimen
- 6 cycles
- 2 cycles ABVD
- 4 cycles AVD (dropped the bleomycin to avoid lung damage)
- 6 cycles
- ABVD chemotherapy regimen
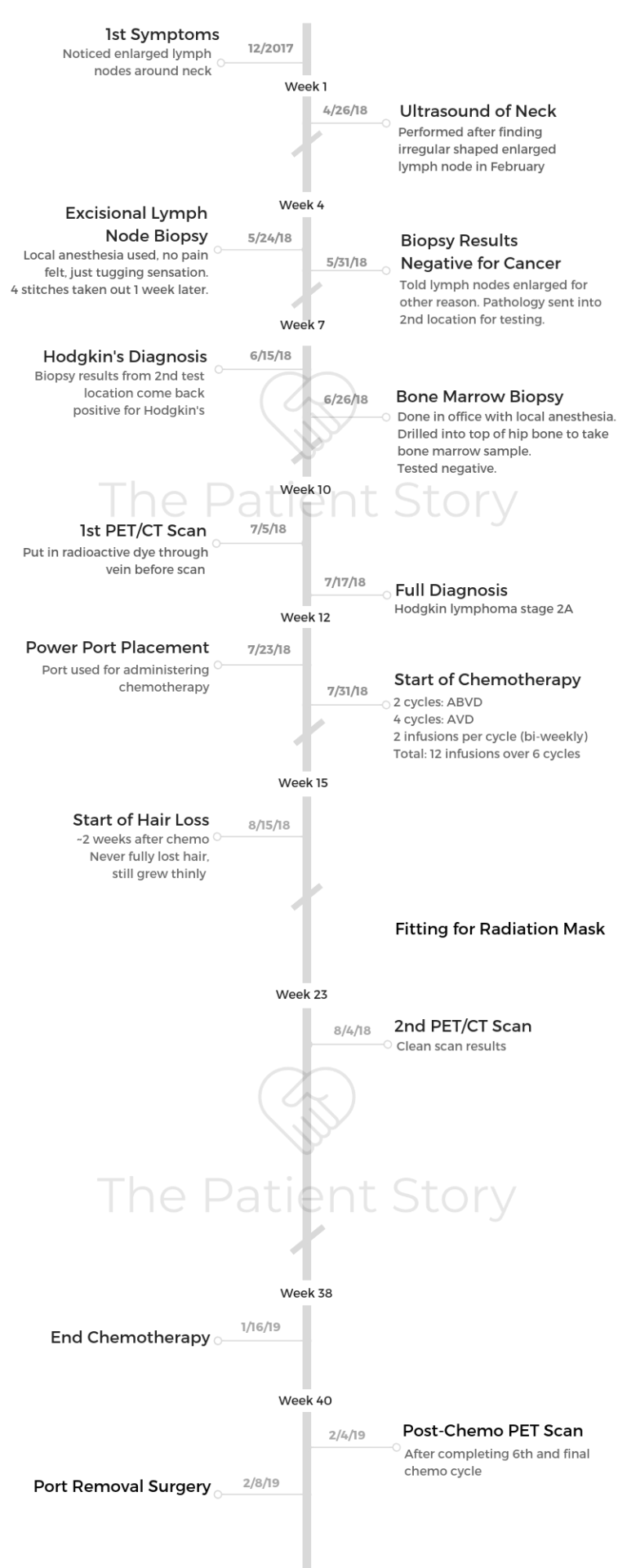
- Diagnosis
- Describe your 1st symptoms
- Getting the diagnosis
- How did you prepare yourself for the diagnosis?
- What tests, scans, biopsies did you undergo?
- Describe the excisional lymph node biopsy
- Describe the bone marrow biopsy
- So both biopsies were fairly easy for you
- Describe the PET-CT scan
- Describe the echocardiogram (transthoracic)
- Describe the pulmonary function test (PFT)
- Treatment Decisions
- Chemotherapy
- After Chemotherapy
- Quality of Life
- Care & Support
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

Watching other people go through it, even just digitally, helped.
Knowing that if I really did want to talk to any of them, they would’ve responded — which I didn’t need, but it was nice to know.
Wade W.
Diagnosis
Describe your 1st symptoms
In December, I noticed an enlarged lymph node. For whatever reason, I immediately was like, “It’s cancer.” I go to school in New York, but I live in Los Angeles.
I was about to leave New York, so I didn’t have time to go to the doctor here. I kind of forgot about it for winter break, so I didn’t end up talking to the doctors about it until February.
By then, there was another swollen lymph node. Then in spring, the doctor was monitoring them, and we did an ultrasound. I had a fine needle biopsy scheduled for the day I was moving out of the dorms, so I ended up not going to it.
A week later, I was talking to a different doctor in LA, who immediately said, “We need to do an excisional biopsy.”
In person, I was told that it wasn’t cancer, that it was some sort of infection that was causing the lymph nodes to be inflamed, but they sent it in to a different place for a second opinion.
That came back as Hodgkin’s.
Getting the diagnosis
It was actually a call because it was a week after they had told me in person. I go to art school, and I had just finished helping this guy move his studio. I was in the middle of nowhere, and I had to take the bus back home.
The doctor who did my biopsy called because I hadn’t talked to an oncologist yet. He called and said, “Yeah it’s cancer.” I was like, “Yeah, I figured.”
»MORE: Reacting to a Cancer Diagnosis
How did you prepare yourself for the diagnosis?
I really don’t know. I did some Googling, and it seemed really unlikely that there would be that many lymph nodes swollen for that long without any other symptoms.
I guess I was pretty fine with the diagnosis, the official diagnosis, because I had spent 6 months processing it beforehand.
What tests, scans, biopsies did you undergo?
- Ultrasound
- Excisional lymph node biopsy
- Bone marrow biopsy
- PET/CT scan
- Echocardiogram (transthoracic)
- Pulmonary function test (PFT)
Describe the excisional lymph node biopsy
They did local anesthesia, so you couldn’t feel pain or anything. This was in my neck, which is where all the lymph nodes were. You could feel a pulling, tugging sensation, which is weird.
You’re awake for it. The local anesthesia hurts when they put it in because they have to poke you a bunch of times to do it, but it stings.
It was unpleasant, but it wasn’t painful or anything like that.
Then I got 4 stitches, and it healed perfectly. Really quickly. I had to go back to get the stitches taken out a week later or something. Everything went fine.
I really like the doctor who did that for me. He joked around a lot, and it was a really fast procedure.
Describe the bone marrow biopsy
That one was done by my oncologist just in the office. It’s really an easy procedure. You’re also awake for it under local anesthetic. That one was worse because you can feel the drilling into the bone, which is a kind of unpleasant situation.
They drilled into the top of my hip bone from the back and took out an inch of bone marrow that was a millimeter wide. The doctor let me see it. It was pretty funny looking. It looked like a piece of string almost.
That one, you didn’t have to go back for anything. It was also fast. Just a tiny raised dot scar from that one.
So both biopsies were fairly easy for you
I think they were both 30 minutes each maximum. [Ranking pain from 1 to 10], I would put both of them as below 5 for sure.
I don’t remember exactly. I also have a pretty good pain tolerance, so I don’t know how that affects things.
Describe the PET-CT scan
I had to get it done through a vein. Maybe 5 minutes tops of them putting in the radioactive stuff. I had to sit in a dark room for 40 minutes.
Then they put me through the scan, which was short. I should know how long it takes since I’ve done it, but I guess I wasn’t looking at the time during it. Very short.
They put my knees up, and I had to put my arms above my head. There’s a rest for your neck, [the platform] moves slowly in and out, and there’s a spinning light.
It feels like a really slow amusement ride to me. I actually think that those are fun, when you’re just going back and forth on that platform.
They are kind of annoying for me because I have to take out my piercings in my ears with them. The place that I had it done had really bad transparent cloud things over the lights, so you’re just staring up at this repeating cloud pattern. It’s awful (laughs).
Describe the echocardiogram (transthoracic)
It was just an ultrasound of my heart. I don’t remember having to do anything. I just sat there, and they do the ultrasound.
Describe the pulmonary function test (PFT)
I had to do a lung test, where I had to breathe in and out. You have to drink some chemical beforehand.
That one was longer because they had to get your base lung functioning through this breathing test. Then they gave you something to open up your lungs more, and then they did that again.
They needed to gauge both my heart and lung functioning before starting the chemo.
Treatment Decisions
How did you decide where to get treatment?
That’s where we were referred. I was using my mom’s primary care doctor, so she knew the oncologist that she referred me to. I didn’t choose it or anything, but I didn’t have any unpleasant experiences there.
I didn’t try to change it at all. I think it’s a small system. There’s a specific film industry center. It’s just weird in and of itself. We ran into someone we knew there once; it’s just small.
I did all my treatment in LA because I was going back for the summer anyway. My parents work in the film industry, so our insurance is also through the film industry, specifically through UCLA. It’s easiest to get the treatments within that network.
Also in New York, I had to go to the doctor for other stuff here, and it’s all really jammed up in the scheduling. Takes forever. You have to take the subway everywhere, so I think trying to do it here was not feasible with the energy levels that I had.
Did you get a second opinion?
I didn’t because I had done research online of the different stages, and it was pretty standard treatments for those. What the doctor told me lined up with those, so I felt comfortable doing it.
The bone marrow biopsy was clean, I believe, but the first CT scan I did showed something in the bone marrow. They weren’t sure if it was a false alarm or not.
So there was some confusion about how long to assign the chemotherapy, because originally my impression was that it was going to be 4 months. It wasn’t until 2 cycles in that he definitively said 6 months.
Describe your hospital size and setting
Mine was really small. There were 3 doctors there. I got treated by one of them, and I talked to another when he was on vacation.
They were all really nice and pleasant. They were maybe 15 seats in the treatment center, tops. Very small.
What did you like about being at a smaller treatment center?
It felt less clinical, which was nice. The people there knew me. I met all the nurses there over the time that I did it.
I didn’t have very intensive chemo. I just sat there for 4 hours once every 2 weeks, so I think some people get a lot more of it. My understanding is it might affect someone more if they had that experience, as opposed to once every 2 weeks.
Once I had some scheduling issues, because I think there were fewer seats and then there was a holiday, so it threw everything off a little. But it was fine overall.
How was your medical team?
My oncologist was nice. I was thinking about the different demeanors of the people that I talked to. My technical primary care doctor, whom I’ve seen twice in my life, is a very nervous woman.
My mom got so freaked out after we went to talk to her, which was just annoying. She’s a nice woman, and I like her fine, but very kind of doom and gloom.
Then the doctor that I did the biopsy with was very joking. He was very LA. I don’t know how to describe it more than that. I think he also did plastic surgery, which I think is also why the scar is so clean.
My oncologist was generally pretty serious, just kind of matter of fact. But he did tell jokes. His favorite joke is that — he told it to me a couple times — he’s like, “So, time to start all over again, right?”
That was right when I ended it, which was funny. I don’t know that he knew how to relate to young people well, but he never did anything bad.
Describe the port placement
I was given the referral to the doctor who would do it, and I had to go into their office, which was fun because they have this golden retriever.
It’s the doctor and his wife who run the place, and Dr. Sharp also had lymphoma years ago, so he was able to relate to that. I didn’t talk to him for a long time, but he put it in and took it out.
I had to go, and then I had to get a blood test from the hospital. They hook you up to an IV and do anesthesia, so I was asleep for the procedure.
I know that it was really fast. I dealt with the full anesthesia well; I woke up pretty quickly after the procedure.
They make you prove you can eat and walk, so you have to eat jello or whatever. During healing at some point within a span of a month, my blood pressure and heart rate shot up.
There’s no discernible reason for that specifically. It probably has to do with the cancer, but I didn’t notice it until after they put in the port.
The night after they had it put in, I couldn’t fall asleep because my heartbeat was too strong. It was weird. I thought that the port had caused it, but they were like, “No.”
The nurse was like, “No, you’re just dehydrated.” Which I don’t think was true, because it’s starting to go back down again now.

They were originally going to put in a portacath, and instead they ended up putting in PowerPort which is slightly different looking. He originally wanted to use the portacath because I think it’s supposed to be easier, but something happened, and they had this one.
I also got it on my left side because I’m right-handed, and I know that different doctors do that different ways, I’ve heard. So for me, it didn’t interfere with a seatbelt or anything. It was on my less active arm, but the scar still stretched a lot.
Recovering from the port surgery
I don’t remember how quickly the anesthesia wore off the first time that they did it, and I don’t remember if they prescribed me pain killers for it at all.
I believe they probably do for the initial procedure. They didn’t when I had it taken out last week. I know last week the anesthesia wore off almost immediately. By the time I got home, it had started to hurt. It’s sore.
It’s right where a backpack strap goes, and you can’t really lift your arm above your head. Or you can lift it above your head a few days later, but you can’t really hold any weight. So it just made travel [harder].
Chemotherapy
ABVD chemotherapy regimen
I was on ABVD initially. That’s 4 drugs, and 2 of them were pushed, so that nurse has to sit there with a syringe and do it and alternate the drug with the IV solution.
I believe the Adriamycin was done that way. One of the other ones was also done that way.
Those are more annoying because you have to sit there. I think they gave me some steroid (dexamethasone) and some anti-nausea [drug]. They gave me pills of Tylenol, Benadryl and Ativan (anti-nausea). I slept through a lot of it. I was sick.
The longest drug I had was an hour long. I think I went in usually somewhere between 8 and 10, and I was out noon or 1.
What was each chemotherapy cycle like?
Each cycle was a month of 2 infusions. There are 2 infusions per cycle. It’s biweekly, so I had 6 cycles total. It was just over 6 months because the first time I did the chemo, my white blood cell count dropped crazy low.
They had to start giving me Neulasta, the white blood cell booster, but I had to wait a week to do it. That happened at least twice.
I would go in for the first week, and I got the 2 hours of chemo. Then I waited 2 weeks, I did the same thing again, and then 2 weeks, and then the next cycle started. So a month total.
I did 2 cycles with bleomycin. After that, it was dropped because of the side effects of damaging the lungs. The bleomycin can permanently cause lung damage.
Now, I’m not able to have pure oxygen, or it will scar my lungs. It’s not a widely publicized thing; it’s kind of weird.
Apparently there have been studies showing that it doesn’t have much of an effect after the second cycle. I believe that I was in total remission by the second cycle on the scan, so I responded very well to the treatment.
ABVD chemo side effects
- Nausea
- Fatigue
- Neuropathy
- Taste changes
- Hair loss
- Cramps
- Light sensitivity
Nausea, fatigue, neuropathy, taste goes away — I think it takes off your taste buds or something — hair loss. I had some things that I don’t know if they were from being more stationary. I got cramps way more easily in my legs. They’d tense up sometimes; it would go away pretty fast.
I also had increased light sensitivity. My second cycle, my eyes were doing this thing where I could only look up. It was getting increasingly worse, and I think it was mental as much as it was physical.
I was running around my house looking up, and I was on the ground trying to hold my head to face. It was stupid. I ended up with really bad neck cramps because I was also turning my head to the side.
It never got that bad again, but it would repeat after that. Every 2 weeks when I did it, a few days after, I got the increased light sensitivity. I think the busier I was, I could experience it a few days at a time.
If I was busy, I wouldn’t really experience it. If I was around people, I didn’t experience it. My dad wasn’t at work the first part of my chemo, and then he went back to some job. The first time I was completely alone again, it flared up really bad, and I had to call my mom to have her come home from work.
Then it got better. I think it was going away that evening. It was just a really weird side effect. I think it was me psyching myself out about it, too. I don’t know if that one would be helpful to anyone, but it was one of the more unpleasant ones.

Did the side effects get better as the cycles went on?
In some ways, I think the first one is the worst because you’re experiencing it for the first time.
I also had neuropathy in my fingers in the beginning. My dad’s side of the family has hereditary hand trembling, shaking, which I have sometimes.
I do art, so I’m usually using small things, really finicky, using wire and stuff like that. So that made it really not fun at all.
But after we lowered one of the drugs, it went away gradually. I don’t remember when it did.
I think the fatigue got worse over time because it’s building. The nausea was pretty much the same every time, like 3 to 5 days of it, taking the anti-nausea pills, which I had a couple of.
What helped most with the chemo side effects?
I got headaches from the Zofran, which I think happens to some people, but not others, so they prescribed it because they didn’t know.
Then I started having sleep issues, and they recommended melatonin, which didn’t really help at all. I ended up taking really low-dose edibles to help me fall asleep because I was not falling asleep for over an hour. Then I would wake up multiple times throughout the night, and still the same thing would happen.
At the beginning, because I was really tired during the day, I would nap. That would just make the night impossible to fall asleep.
After Chemotherapy
What was the hardest part of treatment?
I was physically isolated from all my friends because my friends from LA also go to college out of state, and my friends from college are in New York.
That was the rough part of it. It’s just long. I wasn’t working or anything, because I didn’t want to take a job and not be able to commit. I wasn’t really doing any school work, so I had a lot of free time.
You decided against radiation
I had a consult about it at the Walt Disney Cancer Center, but it was decided that it wasn’t worth it. Radiation was discussed but decided against because of the side effects and potential risks of doing it on young people specifically.
[Because of ] the risk of getting more cancer, different cancers later, it was decided that it wasn’t worth doing it. For someone much older, it might have been.
There was discussion, but there was never a point where I thought I should go get a second opinion about it. It all seemed like very standard treatment.
Describe the scanxiety
I didn’t really experience anxiety before the first scan because I hadn’t started anything at all. I think I was stage 2. I had lymph nodes in my neck, and I think I had some in my chest, too, so I found out from that.
I didn’t really have any anxiety before the second because I just started treatment and I wasn’t all the way through it anyway, so I figured it was probably going to be fine.
I had anxiety before the last one because it was scheduled that I was going to the scans, talk to the doctor, then get the port out. That gave me a lot of anxiety because I was starting the semester without knowing if I no longer had cancer and would be able to complete the semester.
Describe the moment you found out the scans were all clean
The doctor came in, and he was like, “Are you ready to do this all again?”
I knew he was joking because he had done it to me on the last day of treatment already. But [that got] my parents worried for a second. Apparently he does it to all his patients.
I found it very funny the second time. He was completely straight-faced and serious, but I was pretty sure he was joking. Even if it wasn’t, it would be kind of funny. Not in a good way, but it would be kind of funny if that’s the way he announced it.
It would have been very emotional if it was the other way around. But it was more of a confirmation than news, if that makes sense.
How long did your scan results take?
I got the scan [files] immediately afterwards. I got a CD of it, and it’s these weird files because they’re designed for Windows, and I only have a Mac computer. I just download this viewing software, but I had looked at those. I didn’t see anything on it.
There wasn’t anything that was stressing me out about it. I had both seen clean and the first scan, so I didn’t know anything about how to view them. But I could see the lymph nodes in one, and I didn’t see them in the other.
I got the scan on Monday, and I talked to the doctor on Wednesday. I don’t think it would be too bad either way, because there’s nothing I can do about it.
Quality of Life
Describe the hair loss
I’d already freaked out about hair loss before I had cancer. I think that was the only time I ever noticed I got really upset about it, and then I remembered that wigs existed.
I also had a couple rat tails that were 10 inches long that I had been growing out for a couple years. Then I was trying to grow out the rest of my hair. Right when I was starting to do that, that happened.
It was just really annoying to me and kind of upsetting. I buzzed my head before I started chemo because I didn’t want watch it fall out.
I also kept the hair. I had never buzzed it bald, and I never lost all the hair on my head. It looks bad because it’s really thin, but that started 2 weeks after the first treatment.
The little hairs are annoying. I had a bunch on my pillow that I didn’t have the energy to get rid of for a couple weeks.
I never lost all my hair. I lost most of my eyebrows, so I shaved off the rest of them. [I also] lost most of my body hair. There’s one line of hair on both my legs. It’s weird. My hair loss didn’t start till a few months in.
How did you deal with the hair loss?
It was annoying. I go to art school, and so I look like I go to art school. I think in some ways, it doesn’t affect me as much because my style is already alternative or whatever. So people are already like, “That kid looks weird.”
I also have an anime wig. It’s a green. It’s just fun. I would be fine with not having eyebrows if I had a full head of hair. I would be fine with not having hair if I had full eyebrows.
But having both of them gone at once is a little much for me because I don’t like walking around looking sick, especially when I’m not anymore. I’m waiting for it to grow back.
One is like a blonde wig. Short wigs don’t tend to look realistic, and I didn’t really want to pay for one the lace front ones where you can pull your hair back.
Those can look very realistic. They’re like 30 bucks each. They’re cheap. I got some extra hair from them and sewed on, so it matches and stuff.
What was the hardest to deal with mentally and emotionally?
Being physically isolated would’ve been the worst part because I was in digital contact with everyone. But it’s one of those things where there’s no real substitute for being around people. I just spent most of my time alone in my room.
What helped you through those tough times?
I watched a crazy amount of TV. I already watched a lot of TV, but then I started watching a lot more.
I got really into astrology because it’s one of those rabbit holes you can go down for a really long time. I don’t know how useful it is, but a lot of stuff like that.
Were you able to be active?
I don’t think I was really able to. I got out of breath way faster, and things tired me out more. I think physically, I could’ve done it, but the mental effort of doing it, I think, was not happening.
I had to do school, which places a huge value on productivity and constant work and not wasting any time. I had to unlearn that mindset.
Find out how to waste time, just do things slower, really dumb ways because the time passes way slower when you have way more of it free. Now I have to switch modes again, which is rough.
Did you experience “chemo brain“?
Yes. I already had a lot of focus issues before starting [treatment], and then I can’t focus on things.
I’ve also never talked to a mental health professional, so I’m looking into psychiatry and therapy right now. I didn’t feel like doing it. My parents aren’t huge on that stuff.
Care & Support
How important was it to have caregivers?
It was better in terms of being able to get places and not having to do grocery shopping myself and all that. But going from being on my own for a year, which was really nice because they’re very strict and overbearing a lot of the time, to being back in my house that I moved across the country to leave was rough. I have a brother who’s 17, so I’ve talked to him more, which was nice.
Advice on how to get support
Personally, it took me awhile. I know on a mental level, people not talking to you doesn’t mean they’re ignoring you, but it took a while for that to really sink in.
I was also able to do it all because I knew that it had an end, which I think is harder for people with stronger cancers. I knew logically stage 2 Hodgkin Lymphoma, it’s going to be over eventually. For some people, I don’t think they get that comfort.
You have to find a way to live your life like that indefinitely, where I had to find a way to live my life like that for a while, which is a very different thing.
Was there anything surprising about the support you got (or didn’t)?
I am a young person, so nobody my age is thinking about it. It’s not something that you expect to happen to 19-year-olds, so I think it might be different for older people, where they know more people where that has happened. It’s not something that people really know how to handle at my age.
Not that anybody’s bad about it. People don’t know what to say, and so they don’t always know if you want to talk about it or not talk about it.
Some people have expressed feeling bad about not contacting me, because they didn’t want to seem like they were making light of something or like that.
I personally was fine with joking. I’m fine with joking about it to some degree. I do take it seriously, but I think that if I had a conversation, a serious conversation about it with some people, it would tire out any support system that I have.
So I think smaller doses of it, because it’s a lot for other people to handle, too. It isn’t necessarily fair, but it’s just the way it is.
Also, I think people don’t like talking about cancer because if it happened to me for no reason, it could happen to them for no reason. I think stressing out about cancer all the time sucks. I don’t really want to inflict that upon other people to some degree.
Cancer as a young adult
I think younger communities tend to be — I don’t know if conscientious is the right word. They don’t know how to handle things. People deal with it in different ways, or some just don’t deal with it, and nobody has that intention [of being hurtful].
People are more forgetful, I think, and more distracted because they’re all going through something. They’re all doing school and work. They have busy lives, which I think is true at any age.
For me, I’m sitting around all day, so it feels like a lot longer, but when people are doing things all day, it’s a different experience. It’s like learning on two different time zones.
I felt like I was taken out of time a lot. I think generally people don’t have ill intentions. That’s just a good thing to remember.
Message to other patients
Just reiterating some of the things that I was saying right now, because I think it takes a little while to process.
Isolation and having an idea of what it’s like going in would’ve maybe been helpful. I didn’t really didn’t talk to anyone about it. I don’t really use Reddit, but I found that some Reddit for cancer. Trying to google random things. I didn’t post on there, but a couple times.
Watching other people go through it, even just digitally, I think helped and knowing that if I really did want to talk to any of them, they would’ve responded. Which I didn’t need, but it was nice to know.

Inspired by Wade's story?
Share your story, too!
Hodgkin’s Lymphoma stories
Jessica H., Hodgkin’s Lymphoma, Stage 2
Symptom: Recurring red lump on the leg (painful, swollen, hot to touch)
Treatment: Chemotherapy
Riley G., Hodgkin’s Lymphoma, Stage 4
Symptoms: • Severe back pain, night sweats, difficulty breathing after alcohol consumption, low energy, intense itching
Treatment: Chemotherapy (ABVD)
Amanda P., Hodgkin’s Lymphoma, Stage 4
Symptoms: Intense itching (no rash), bruising from scratching, fever, swollen lymph node near the hip, severe fatigue, back pain, pallor
Treatments: Chemotherapy (A+AVD), Neulasta
Brescia D., Hodgkin's Lymphoma
Symptom: Swelling in the side of her neck
Treatment: Chemotherapy: 6 rounds of ABVD





