Ananda’s Stage 3B Rectal Cancer Story
Interviewed by: Alexis Moberger
Edited by: Katrina Villareal

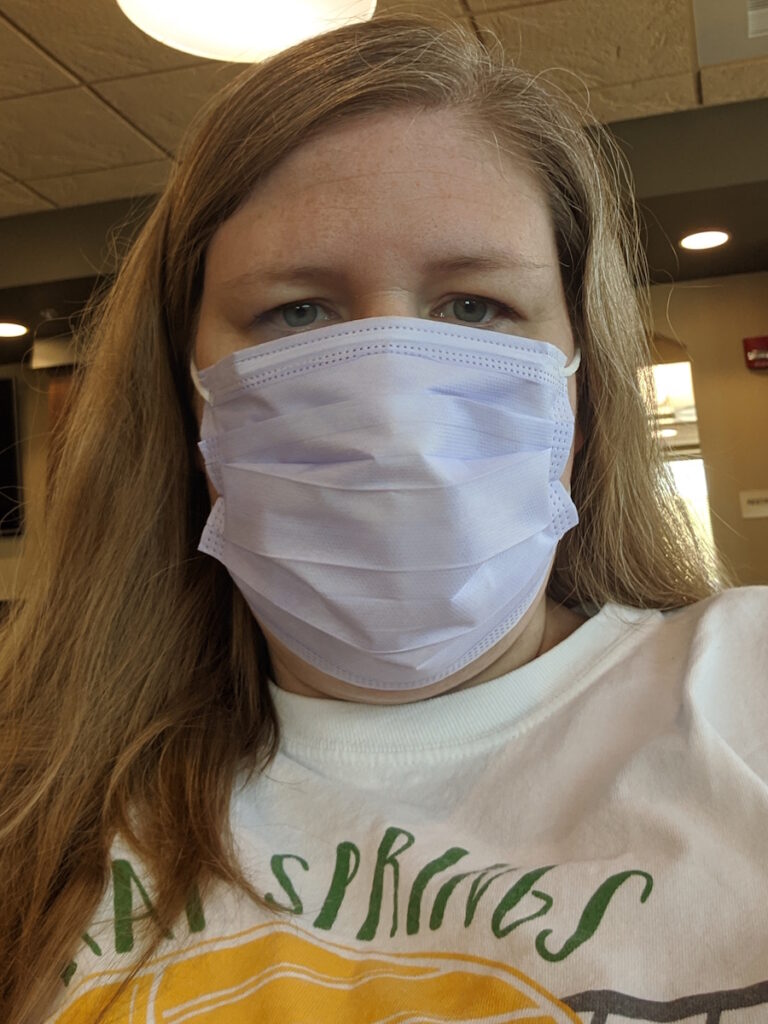
Ananda was diagnosed with stage 3B rectal cancer at 44.
Ananda knew something wasn’t right when she experienced rectal bleeding after the birth of her son in 2014. Even though her symptoms got worse, doctors dismissed her concerns as hemorrhoids for years.
It wasn’t until 2020, after the birth of another child, that Ananda was finally able to get a colonoscopy which revealed a large rectal tumor. She was then diagnosed with stage 3B rectal cancer at 44.
Knowing that she needed to see a specialist, she made the 10-hour drive to the Mayo Clinic where she subsequently had her surgery.
She shares the importance of being your own advocate and listening to your body. Leaning on her faith helped her through the most traumatic thing she had to go through.
In addition to Ananda’s narrative, The Patient Story offers a diverse collection of colorectal cancer stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- Name: Ananda P.
- Diagnosis:
- Rectal cancer
- Staging:
- 3B
- Initial Symptoms:
- Intermittent rectal bleeding
- Treatment:
- Surgery
- Chemotherapy: FOLFOX (folinic acid, fluorouracil, and oxaliplatin)

Introduction
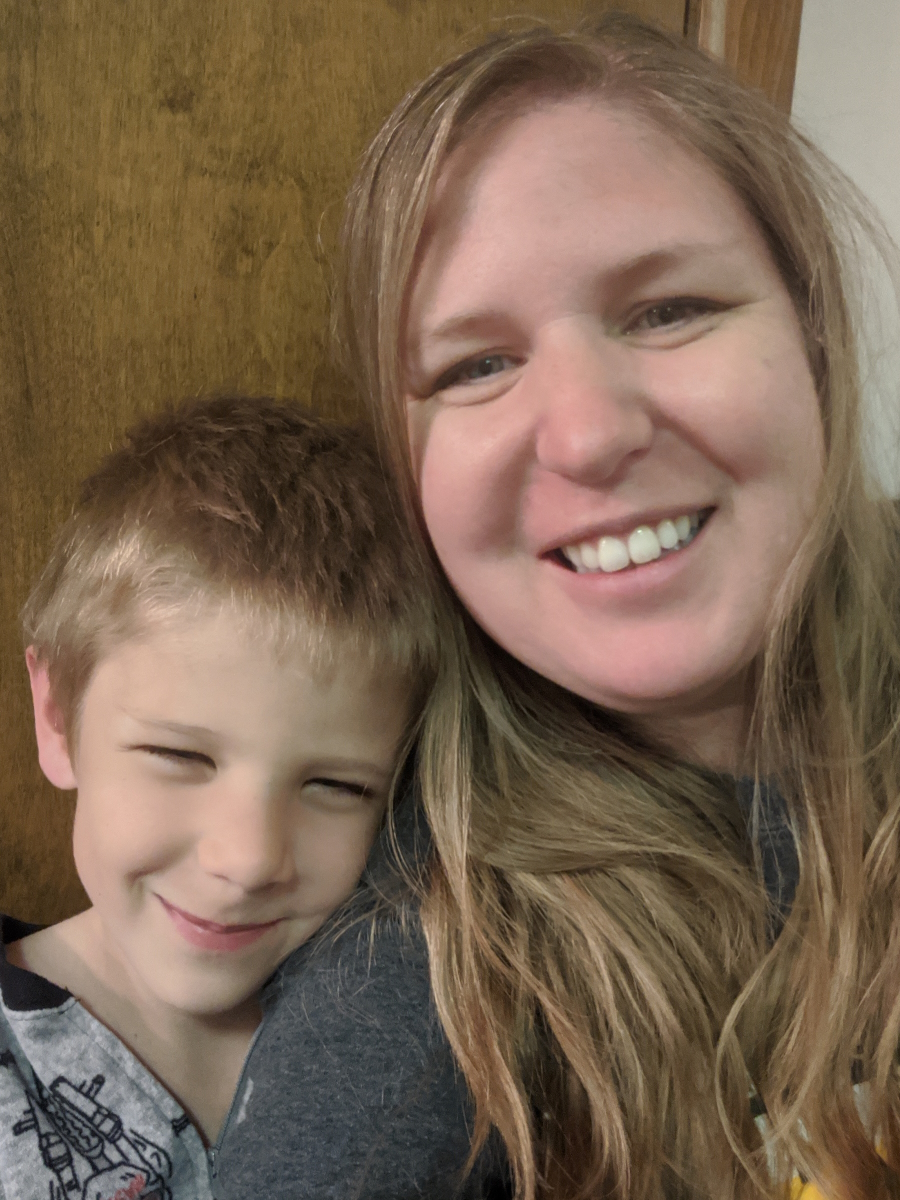
I’m originally from Canada. I live in Rapid City, South Dakota. My husband, Joe, and I have eight kids from ages 3 to 20.
My background is in journalism. Writing and reading are my two big hobbies. I love people, ice skating, and a lot of different things.





Pre-diagnosis
Initial symptoms
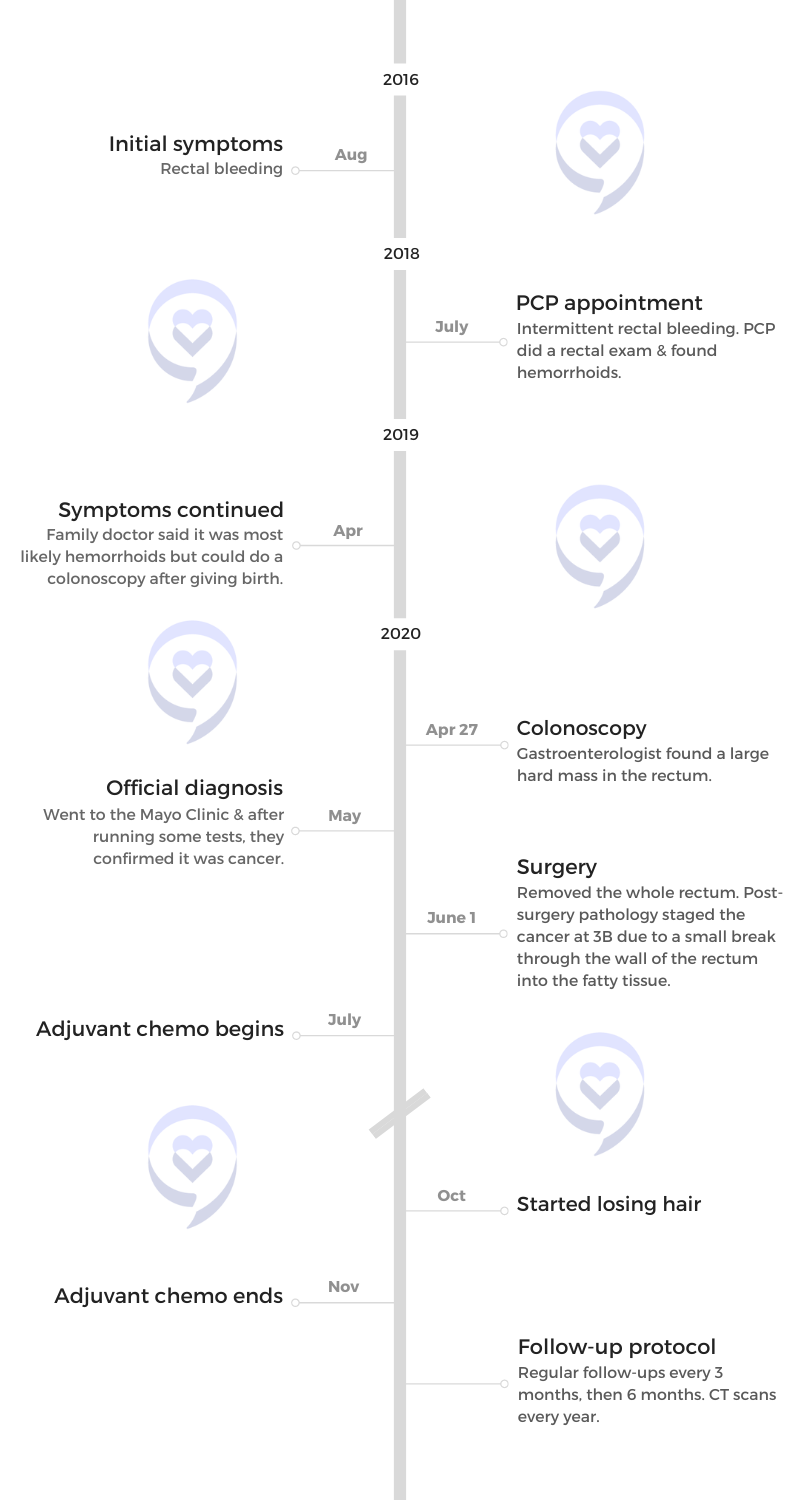
My son, Reeve, who’s number six, was born in 2014. I had some rectal bleeding after he was born and it was really painful.
I went to the doctor. She did an exam and said, “You have a fissure so increase your fiber and drink lots of water to clear it up,” so I did. Magnesium was amazing; that really helped. It cleared up and went away.
Fast forward two years later, my son Avram was born in August 2016. I had some more bleeding so I started taking more magnesium, fiber, and lots of water, but it wasn’t clearing up.
The bleeding didn’t happen every time. It was just sporadic. I would take two magnesium, which was more than enough but I was still having this blood on and off.
In January 2017, five months after he was born, my uncle was diagnosed with stage 4 colon cancer and he died a month later. I thought, I really need to get on my issue.



I got pregnant again and had a late miscarriage so going to the doctor or having a colonoscopy was on the back burner.
In July 2018, I finally went and said, “My uncle died last year.” My primary care doctor asked, “Are you having any pain in your stomach or any other symptoms?” I said, “No, just blood every once in a while.” She said, “With your history of having all these babies, I’m so sure it’s hemorrhoids. Your risk of getting cancer at this age is so slim.” I was 42 at that point.
She did an exam and said, “Yep, I can feel the hemorrhoids,” so she gave me hemorrhoid medicine. Then she said, “If it doesn’t clear up, come back and see me.” We were in the middle of an interstate move so I thought that since it was hemorrhoids, I checked that off the list.
Symptoms worsen
It didn’t go away and it became more mucousy. There was one point where I passed a hard thing the size of a grape and it wasn’t poop.
Now I was pregnant again. I talked to a different doctor than I’d gone to before and she said, “After this baby’s born, we’ll get you in for a colonoscopy.”





Finally getting a colonoscopy
My son was born in January 2020, on the day the world announced COVID. I had trouble nursing him. As a mom, you always feel so guilty when you can’t nurse. A lot of moms feel that way and I felt since this is my 8th, I should be able to.
Because I had all these other kids, I couldn’t get in the right frame of mind to devote as much as I needed to nurse him. I put him on the bottle, which I felt guilty about but was a huge blessing because if I was nursing, I would have put the colonoscopy off for another year.
In April, I went in for a colonoscopy. The gastroenterologist said, “I’m so sure it’s hemorrhoids.”
I had a close friend diagnosed with colorectal cancer a year before me. She was exactly my age. When I told her my symptoms, she said, “Get in for that colonoscopy.”
Even though it was dismissed, I said, “I really want this.” I was 44 at that point and the gastroenterologist said, “I’m sure that it’s hemorrhoids. We’ll talk about it when you come out. We can do a banding procedure. It’s real simple.”



Diagnosis
Getting the official diagnosis
I went to sleep and when I woke up, the doctor was looking at me and she said, “I am so sorry. I did not expect to be telling you this, but there is a large mass in your rectum and I’m quite sure it’s cancer. It’s very hard and that’s generally a sign of malignancy.”
Reaction to the diagnosis
That was a huge shock. You’re never ready for that; that’s what everybody always says. I called my husband. He wasn’t there with me because he was watching the little ones.
I’m a pretty organized person, but when you get news like that, where do you go from there? They got a small enough sample for a biopsy because she was sending it to pathology.
She called, but it was not immediate. Although she did believe it was cancer, we didn’t know for sure.




Genetics
They’re seeing more and more younger patients. The doctor at Mayo said they were studying this pretty intensely. One particular doctor who’s studying it said, “I believe there is something that’s causing it. We just haven’t figured out what that thing is yet.”
I was told that a lot of times, at least with colon cancer, you don’t see blood. With rectal cancer, it’s more common because you’re closer to the opening.
They did genetic testing and there were no genetic markers, but I don’t know. My uncle died from it so maybe there’s some predisposition. My dad had polyps removed when he was young and forgot all about it.
My family got their colonoscopies and nobody had any issues. They were all good. There were a couple of polyps.
This doesn’t have to be a hopeless situation. There is hope in the midst of it.
Ananda P.



Treatment
Finding a cancer treatment center
My friend who had colorectal cancer went to the Cancer Treatment Centers of America in Tulsa and she had such a good experience so I called them.
We don’t have traditional insurance. We’re part of a healthcare sharing network so we’re handled as self-pay. We get it all reimbursed, but it’s not traditional. When I told CTCA that, they were really slow to call me back.
In Rapid City where I had gone for the colonoscopy, they referred me to a general surgeon. I immediately went online and found out that rectal surgery is very complicated and you really want a specialist doing it.
I called the Mayo Clinic and they were just starting to open up after going on restrictions with COVID. It was 4 o’clock in the afternoon and they said, “Can you be here at 8:30 tomorrow morning?” I said yes.



Honestly, I didn’t even know where Rochester, Minnesota, was. Being from Canada, my US geography is not wonderful. I told them I would come and found out it’s a 10-hour drive.
I called my husband and we figured out who would stay and who would go. I brought my 15-year-old daughter who had a learner’s permit so she could help drive and my three-month-old baby because he would be the most work.
Going to the Mayo Clinic
We drove through the night. She drove through the night to Minnesota on her learner’s permit. We got in at six or seven in the morning and I showered and went to this appointment.
They are so efficient at Mayo. I got in for the appointment with the gastroenterologist. They did a CT scan and an MRI. I don’t remember if they did the lower ultrasound at that point or if that was later; I think they did. By the end of the day, they know what you have.
I’m not sure exactly if everything happened all in one day or over the course of a couple of days. I know the results came in very quickly. We knew this was cancer.



Meeting with the rectal surgeon
I met with the surgeon first. He does rectal surgeries all day, every day and he teaches other people to do rectal surgeries. I remember him coming in wearing a suit and sitting on the bed. He was very professional but casual. He knew what he was doing.
He said, “Here’s what’s going on. We’re going to do the surgery a month from now,” so they scheduled it for June 1st. I said, “A month? What if the cancer spreads through my body?”
He explained that the kind of colorectal cancer I had was very slow-progressing. He said, “You’ve probably had this 6 to 8 years.” Back when I had that fissure those years ago, there was probably some rectal cancer already going on.




Surgery
We went back home and I came back on June 1st to have the surgery. It was quite a long surgery. They got the tumor out with clear margins.
When I went in, they thought it was stage 1 and that they caught it early. When they did the pathology post-surgery, they realized that there had been a small breakthrough through the rectal wall into the fatty tissue, which made it stage 3B.
Because of that, they recommended adjuvant chemo for four months to make sure it doesn’t come back. I would start in July 2020.
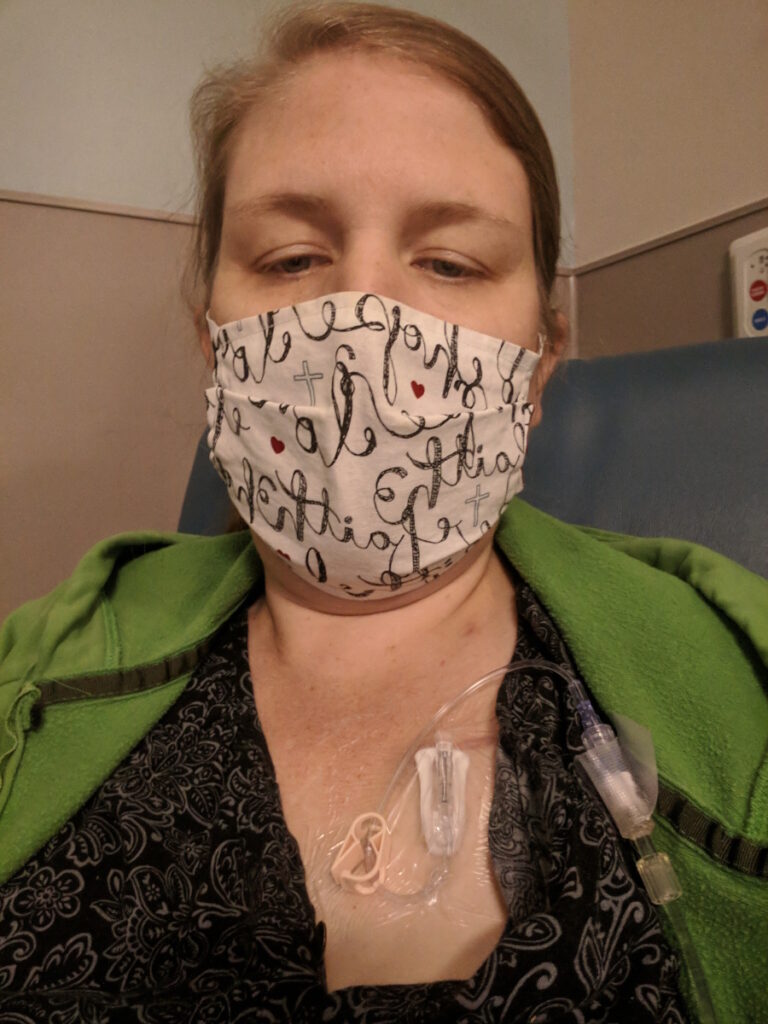
Adjuvant chemotherapy
That was the most traumatic thing that I had to go through. It’s the mental difficulty of knowing that you’re putting poison in your body and knowing I didn’t have cancer anymore.



They come into that chemo room in a hazmat suit because they can’t touch the chemo. The nurses are head-to-toe garbed up yet they put the needle into your body. It’s such poison and yet I’m willingly letting it be injected into my veins.
I really struggled with it. I wanted to quit. I did quit. I called my oncologist and said, “I’m done.” I was doing it in Rapid City. They basically explained chemo is chemo wherever you have it done so I decided to do it at home. But when I called her, she talked me back into it and explained the statistics.
Side effects of chemotherapy
I was doing oral chemo, which made me very sick and my stomach hurt really bad. Then they switched me to FOLXFOX. It’s a pack that you wear for two days then they take it out.
I didn’t get sick with that, which was amazing. That was an answered prayer because oral chemo was awful. I’ve heard other people say they liked oral chemo, but it was awful for me.
I remember one pharmacist said managing anxiety is an important part of your care plan. Up to that point, I felt guilty feeling so fearful.
Ananda P.




Managing anxiety
That time was really, really, really difficult. I felt like I should have been stronger, but I wasn’t. I would go outside, sit there, and breathe. It was hard to slow down my body to breathe.
They gave me Ativan for anxiety, which helped me sleep at night. I didn’t take it too much because I liked it and thought I would get addicted to it, but it did help me for a short time.
I’m very task-oriented so I go into the mode of what needs to be done. It was absolutely terrifying thinking I was two steps away, two stages away from terminal cancer. In between me and stage 4, there’s only 3C and I have a little baby and a lot of little kids at that point.
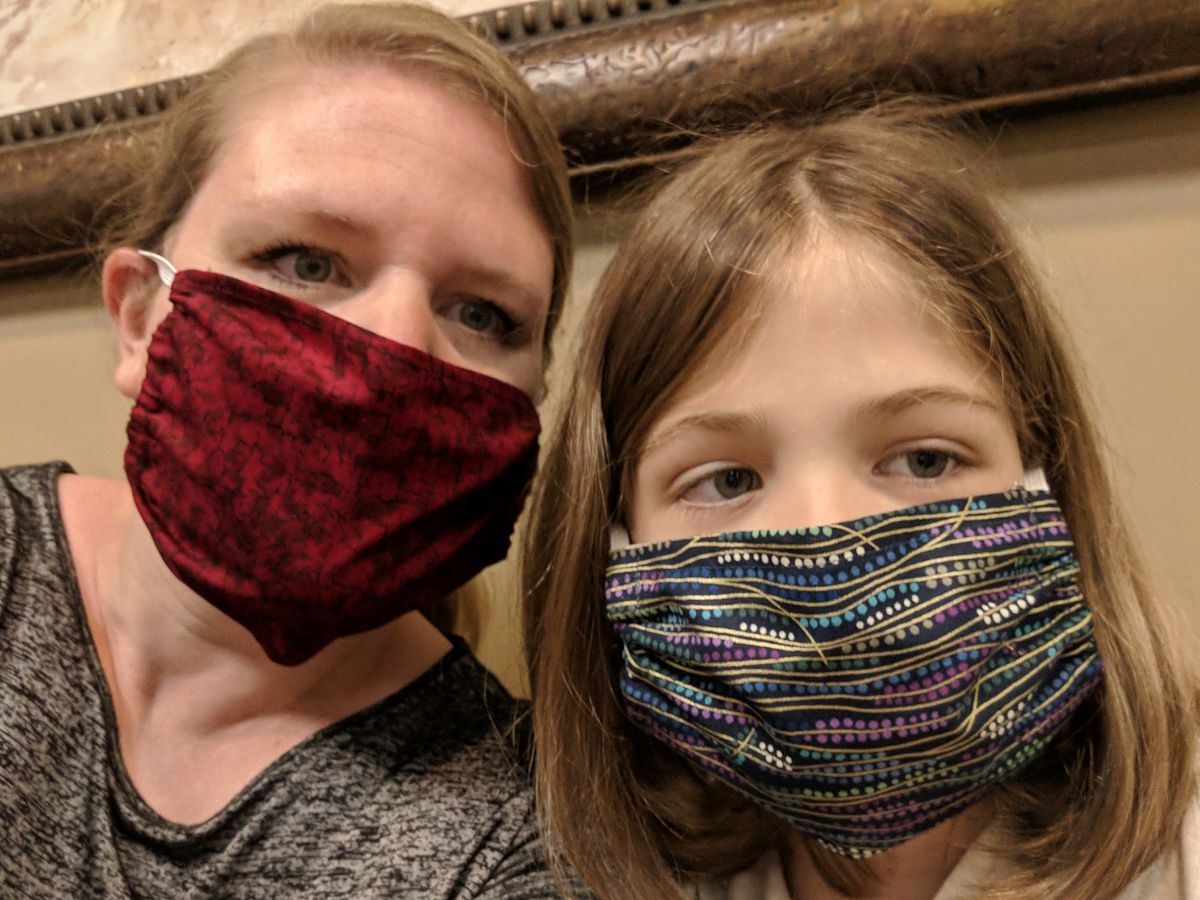
My teenage daughter was going through a really hard time. I couldn’t be there for her and that was so difficult. My son graduated from high school. He was homeschooling and he just finished his work. It was October and I was in the middle of chemo. I wanted to celebrate that, but I was in survival mode.


All these big things are happening and it was so difficult to function. It’s really good to talk about it right now because it was pretty traumatic. Processing the trauma takes a long time. You think you’re over it and then something will come up.
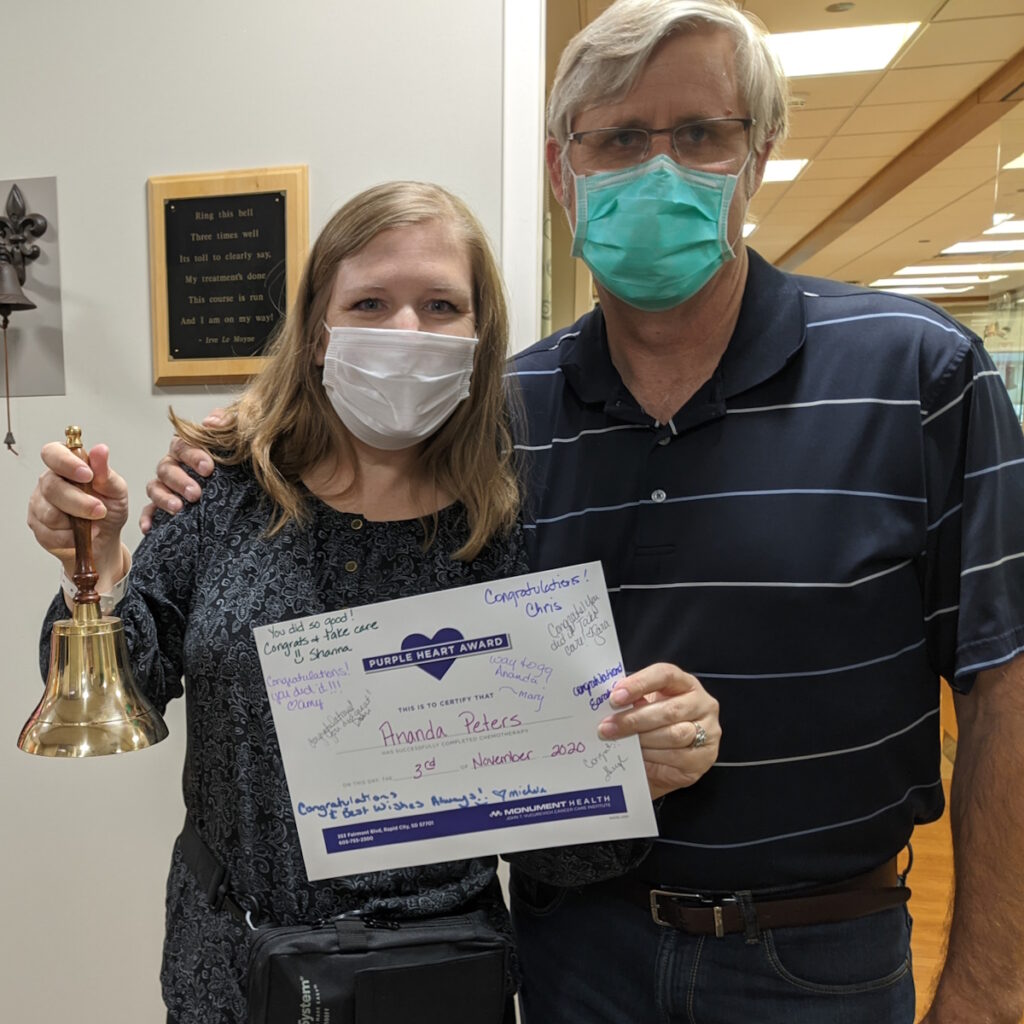
I rang the bell in November 2020 and the cancer has never returned. At the Mayo Clinic, they told me they had a very low recurrence rate with rectal cancer, which was the opposite of what I read online so that was really good.
Follow-up protocol
I regularly go for CT scans. It started with every six months and now it’s once a year. Once I get to five years, the chance of getting rectal cancer would be the same as anyone else getting it.



Words of advice
I think God gives us an instinct about our bodies. You don’t know what it is and you can’t pinpoint it, but something is wrong and that’s a real thing. That’s a real voice to listen to.
Be your own advocate. I know doctors don’t like it when you go online and do all this Dr. Google research, but I learned so much. My sister came down from Canada for five weeks and the two of us were reading all these medical journals nonstop.
We would call the doctors at Mayo and ask, “What about this?” We were pretty impressed with our own knowledge. I don’t say that boastfully, but my point is that you can learn about what’s going on with your body.
Not that doctors aren’t trustworthy; they are, but they’re not inside your body so they don’t feel that feeling of something is off. Only the patient feels that and that’s a real thing so listen to that.



What really threw me off, and I wish I had known, is all of the anxiety and fear. It’s not that you’re not strong enough to handle this. This is part of the process. My medical team was really good about explaining that to me, but I didn’t know it until I was far into the process.
I remember one pharmacist said managing anxiety is an important part of your care plan. Up to that point, I felt guilty feeling so fearful. I was so terrified and I thought, This could be it. This is what happens. People just all of a sudden get a diagnosis and then they die.
I was so scared for my kids. I had a friend who had never had kids and had never been married so she didn’t understand. She’s very kind, but she said, “You need to focus on yourself and not just be thinking about the kids,” and I couldn’t. I’m a mom. It’s instinctual to constantly be thinking about your kids.
That’s what I wish I had known. The anxiety is going to be crippling and it’s not your fault. It’s part of this journey.





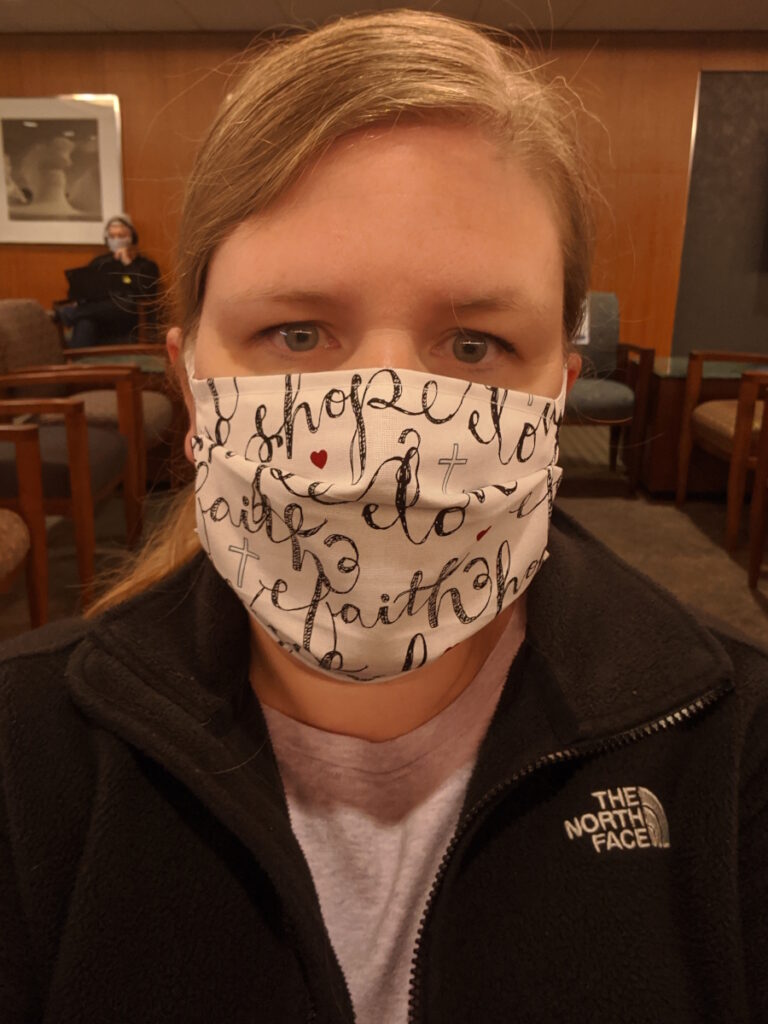
Leaning on faith in God
The other thing I learned was to lean on my faith. I didn’t have the frame of mind to pray. I would put scriptures on my phone and read them in my desperation. Things like, “God is a refuge and strength, an ever-present help in times of trouble.”
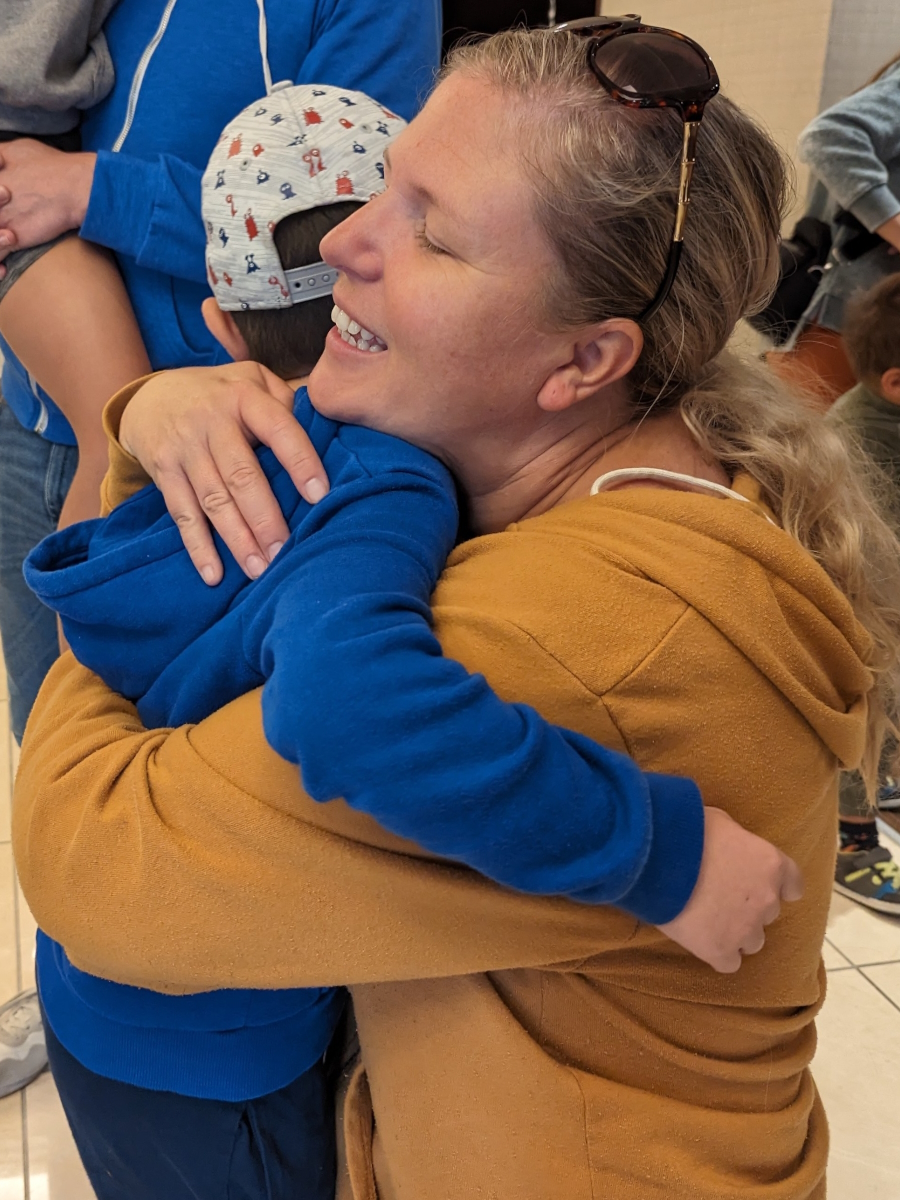
I’m not in this alone. I have my sister, my sister-in-law, and my husband. I had friends. My friend Amy drove me to all my chemo appointments. She was amazing. I had a good human team and I had God who I relied on and we got through it.
There is an end, even for those who are diagnosed with stage 4, like my friend Julie was. It’s a day-to-day journey but there is strength and there is hope. This doesn’t have to be a hopeless situation. There is hope in the midst of it.
Thank you to The Patient Story for all you do. I watched so many videos and was on the website. It was really, really helpful to hear other people’s stories of what they’d gone through. You are doing a great thing and I’m really thankful for what you do.




Inspired by Ananda's story?
Share your story, too!
More Rectal Cancer Stories
Sarah G., Rectal Cancer, Stage 2A
Symptom: Minor and inconsistent rectal bleeding
Treatments: Surgery (low anterior resection or LAR), chemotherapy (FOLFOX)
Kalei M., Rectal Cancer, Stage 4 (Metastatic)
Symptoms: Presence of mucus and tissue-like substance and blood in stool, stomach cramping
Treatment: Radiation therapy, chemotherapy, surgeries (two lung resections)
Jessica A., Rectal Cancer, Stage 4 (Metastatic)
Symptoms: Changes in bowel movements, blood in stool, abdominal pain, back pain, difficulty sitting comfortably, constipation, feeling of incomplete evacuation (as if some stool remained after bowel movements), mucus-like stool consistency, bloating
Treatment: Immunotherapy under a clinical trial
Shiva S., Rectal Cancer, T2, and Renal Cancer, T3
Symptoms: Pressure and urgency of bowels, back pain
Treatments: Chemoradiation (for rectal cancer), surgery (ileostomy, combined bowel and kidney surgery), immunotherapy (for kidney cancer)
Jeanine B., Rectal Cancer, Stage 3 (T3bN0M0)
Symptoms: Long history of bleeding that was blamed on hemorrhoids, pain in the tailbone, urgent need to use the restroom, unusually narrow stools, presence of mucus in stools, fatigue
Treatments: Chemotherapy, radiation therapy
Devon B., Rectal Cancer, Stage 4
Symptoms: Pain when trying to move bowels, increased frequency of bowel movements alternating with periods of constipation, passing mucus instead of feces, narrow stools
Treatments: Surgery (ostomy surgery), radiation therapy, chemotherapy





