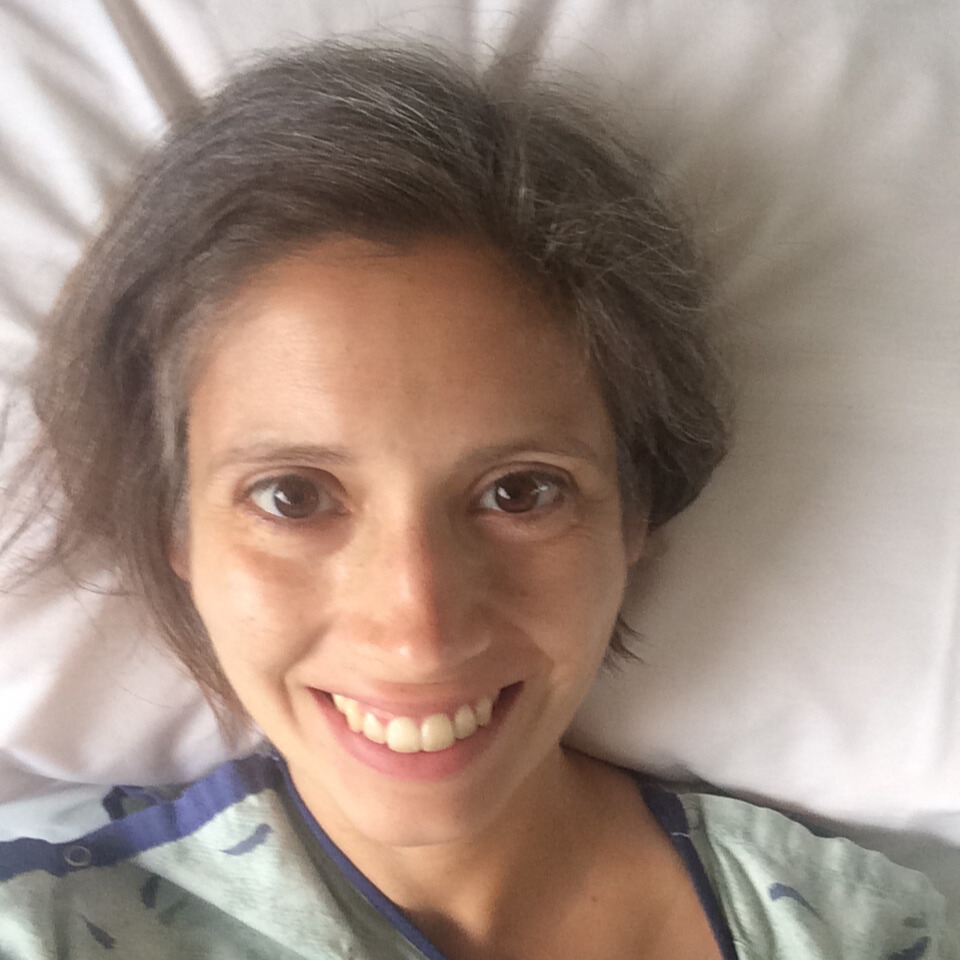
Jelena’s Stage 3 Rectal Cancer Story
Jelena, a mother and avid runner, shares her journey with stage 3 rectal cancer. Initially experiencing changes in her gas, she attributed it to dietary issues. When bleeding occurred, she consulted a nurse practitioner who suggested monitoring the symptoms. After three months, the bleeding intensified, prompting tests and a colonoscopy. Despite being healthy and in her 30s, Jelena received an unexpected diagnosis – rectal cancer.
The following weeks involved diagnostic testing, revealing the cancer’s stage 3 status. Jelena faced decisions on treatment options, considering seeking second opinions from larger cancer centers. Ultimately, she opted to undergo 28 days of radiation and oral chemotherapy followed by surgery to remove the tumor.
Her journey continued with additional chemotherapy sessions, challenging moments, and a supportive online community. Regular follow-ups and surveillance became part of her life, offering reassurance as she embraced the role of a cancer survivor. Jelena emphasizes the importance of online support groups and encourages others facing similar challenges to connect, share experiences, and find strength in solidarity.

- Name: Jelena T.
- Diagnosis (DX):
- Staging:
- Stage 3
- Symptoms:
- Change in gas
- Bleeding and spotting
- Age at DX: 34
- Treatment:
- Radiation
- Chemotherapy
- XELODA
- FOLFOX
- Surgery
- Tumor removal
- Ileostomy reversal
Social media can get a bad rap a lot of times, but it can be great in situations like this, to connect with others that are in your situation that may not be in your town or even in your country where you live.
Jelena T.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Symptoms
Tell us about yourself
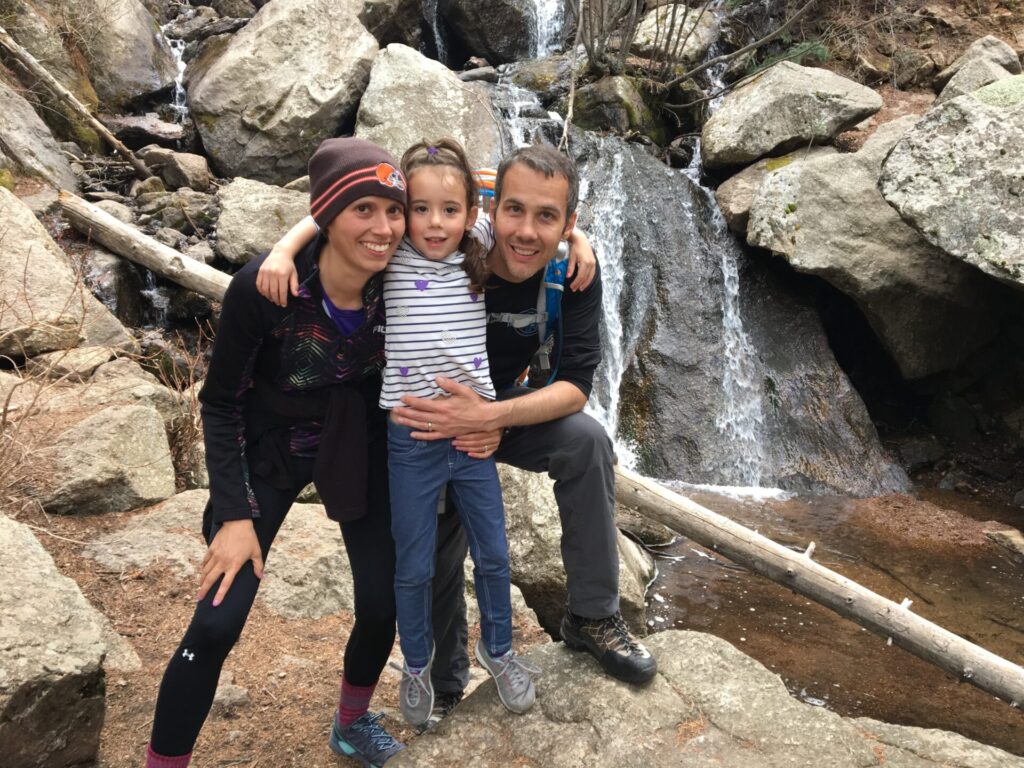
My name is Jelena. I am a mom to a now 12 year old daughter. Some of my activities that I like to do, I love to run. I’ve been running ever since high school. I enjoy sewing. I’ve been sewing figure skating costumes for my daughter, who is a skater.


Other hobbies that I have, I’ve got a YouTube channel that I started after my cancer diagnosis called Life As A Cancer Survivor, which keeps me very busy. I enjoy hanging out with my family and spending time with them and traveling when we can.
What were your first symptoms?
I didn’t necessarily know anything was super wrong at first when my first symptoms popped up. My first symptom was actually a change in my gas. It smelled different and was more potent than it used to be. I thought maybe it was just something I was eating so I tried taking some probiotics, thinking that would help. Then I started experiencing bleeding when I would go to the bathroom after taking those probiotics, so I stopped. I let the bleeding stop and let the probiotics work their way out of me.
My first symptom was actually a change in my gas. It smelled different and was more potent than it used to be.


I tried them again, got the same result, so I thought that I was stuck with stinky farts for the rest of my life. When I went in for my physical a few months later, I mentioned that experience with the nurse practitioner, and she asked if I was still experiencing the bleeding, and I said no. She suspected maybe it was just a change in my diet, although my diet really hadn’t changed, so it could have just been changes in my body as I aged. She did say that if the bleeding started again to call the office and let them know and they’d investigate further.
»MORE: Colon & Rectal Cancer Symptoms
Running tests and scans to investigate the symptoms
Three months later, the bleeding did pick up again and I hadn’t been taking the probiotics. I called the office and they brought me in for tests. They ran blood work to check me for all kinds of food allergies, to see if something was just upsetting my digestive system and causing the bleeding. Everything came back negative, so she sent me in for a colonoscopy so they could investigate firsthand what was going on inside. I was 34 at the time back in 2016.
Tests & Scans
Was it easy to get a colonoscopy?

If they refuse a colonoscopy, tell them that they need to put in your file that you came to them with symptoms and that they refused to give you a colonoscopy. That may also make them think twice about denying it.
My doctor, I didn’t have to really fight with her about it, but I know many others do have troubles going in. My advice would be to try and keep track of all of those symptoms. Mark in a calendar or some kind of symptom tracker, how many times you’re using the bathroom and how your stool has changed, or when you’re experiencing blood and all of those things. So you’ve got hard evidence to take in to the doctor’s office when you see them.
If they refuse a colonoscopy, tell them that they need to put in your file that you came to them with symptoms and that they refused to give you a colonoscopy. That may also make them think twice about denying it. They might say, “Well, I don’t want to look bad. Okay, we’ll let you go in for one.” Or if they are still adamant about it, get a second opinion from another doctor. I know that’s not always the easiest thing to do, but if these symptoms are ongoing and aren’t getting better with diet changes or other recommendations from a doctor, then it needs to be checked out.
Did you suspect you had cancer?

I was not thinking cancer at all. Cancer doesn’t run in my family, especially not colorectal cancer. I was 34, I was healthy, as I mentioned, I was a runner. I had just run a half marathon up and down Pikes Peak, which is a 14,000 foot mountain here in town. I was in some of the best shape of my life. I ate healthy and didn’t ever think that cancer would strike me at such a young age.
I was going in thinking I had some kind of digestive disorder that was causing this. I might have to be gluten free for the rest of my life, or maybe take some kind of medication to keep things from progressing or to keep the gas and bleeding under control. I did not suspect cancer at all.
Describe your experience prepping for a colonoscopy
I actually just went in for my most recent colonoscopy last week, so it’s been a week since my most recent one. But for that first one, they did tell me not to eat fruits and vegetables for the two days leading up to the colonoscopy. No fresh fruit or vegetables. Canned stuff, you can digest easily, you can eat. They want your colon to be nice and clean. A lot of those fibrous things that we eat, they can linger or leave residue behind. That makes it difficult to really see the entire colon wall.
The day before the procedure, the prep they had me do, I drank magnesium citrate. It’s like a 16 ounce weird tasting sprite, bubbly beverage. I drank that. I took some stool softeners, and then I mixed up the Miralax and Gatorade and had two different doses of that to clean me out.

Diagnosis
She said that they found a mass in my rectum when they were doing the colonoscopy…she was 99% sure that it was rectal cancer.
Grappling with possibly having cancer while awaiting results
I had the procedure the next morning and went in. It was late in the morning. It was at 11:30 because my daughter was in preschool at the time. My husband had to drop me off at the colonoscopy, go pick her up from preschool, and bring her back to pick me up. When I was waking up from the procedure, he was in the room, but my daughter was not. I was like, “Where’s Maelle?” They said, “The nurse wanted her out while they come in and talk to you.” That was when my stomach dropped and I suspected that there was bad news coming if they didn’t want my daughter in there. She said that they found a mass in my rectum when they were doing the colonoscopy. They took biopsies of it to see what exactly it was, but she was 99% sure that it was rectal cancer.
She said they put a rush on the biopsy so they would get the results as soon as possible, but she didn’t discuss anything further. She said we’d talk more once those results came in, which only took two days. The colonoscopy was on a Monday, and by Wednesday afternoon we were in her office to get the results. It was heart wrenching finding out that I could have cancer, that it was bad enough that they couldn’t just scoop it out during the colonoscopy. I knew it wasn’t just stage 1 or 2. It was probably more advanced, but had no idea how advanced it was.
My daughter was finishing preschool. We were in the process of building a house in a nearby neighborhood, but I had no idea if I was going to live to see that house completed. I was like, do we even continue with this or just pull out? Because I’m not going to be here. We’re not going to need this house.

You try your hardest to not let your mind go to the worst case scenario, but it’s really difficult when you hear the word cancer, and you have no idea how bad it is to not let your mind wander there occasionally. So then it’s just planning. Okay, well, what happens if it is this or if it is that? You’re trying to not let that get too out of control because you can spiral quickly and think the worst when it may not necessarily be the worst case scenario.
»MORE: Reacting to a Cancer Diagnosis
Receiving a cancer diagnosis
As I mentioned, two days later, we were getting the results at the doctor’s office and she confirmed. When she was walking us back, she seemed cheery and upbeat so I thought, oh well, maybe it’s not cancer or it’s not bad. Then she sat us down and she said it was cancer. My husband was there with me and we cried. The doctor held my hand and cried with us, and she said, we don’t know how bad it is, but the next week or so is going to be full of diagnostic testing to find out the staging of the cancer so that we can begin treatment.

It was heart wrenching finding out that I could have cancer.
Receiving further tests and diagnostics
She referred me to multiple offices to get the CT scan. She referred me to an oncologist, which I’m glad because I had no idea who I would go and see for this. Her office took care of getting in touch with all of those offices, and they reached out to me to get everything scheduled. The next couple of days was just a flood of getting phone calls, scheduling appointments, figuring out preps for this because some of them, you can’t eat for a few hours before or you need to do this, you need to do that.

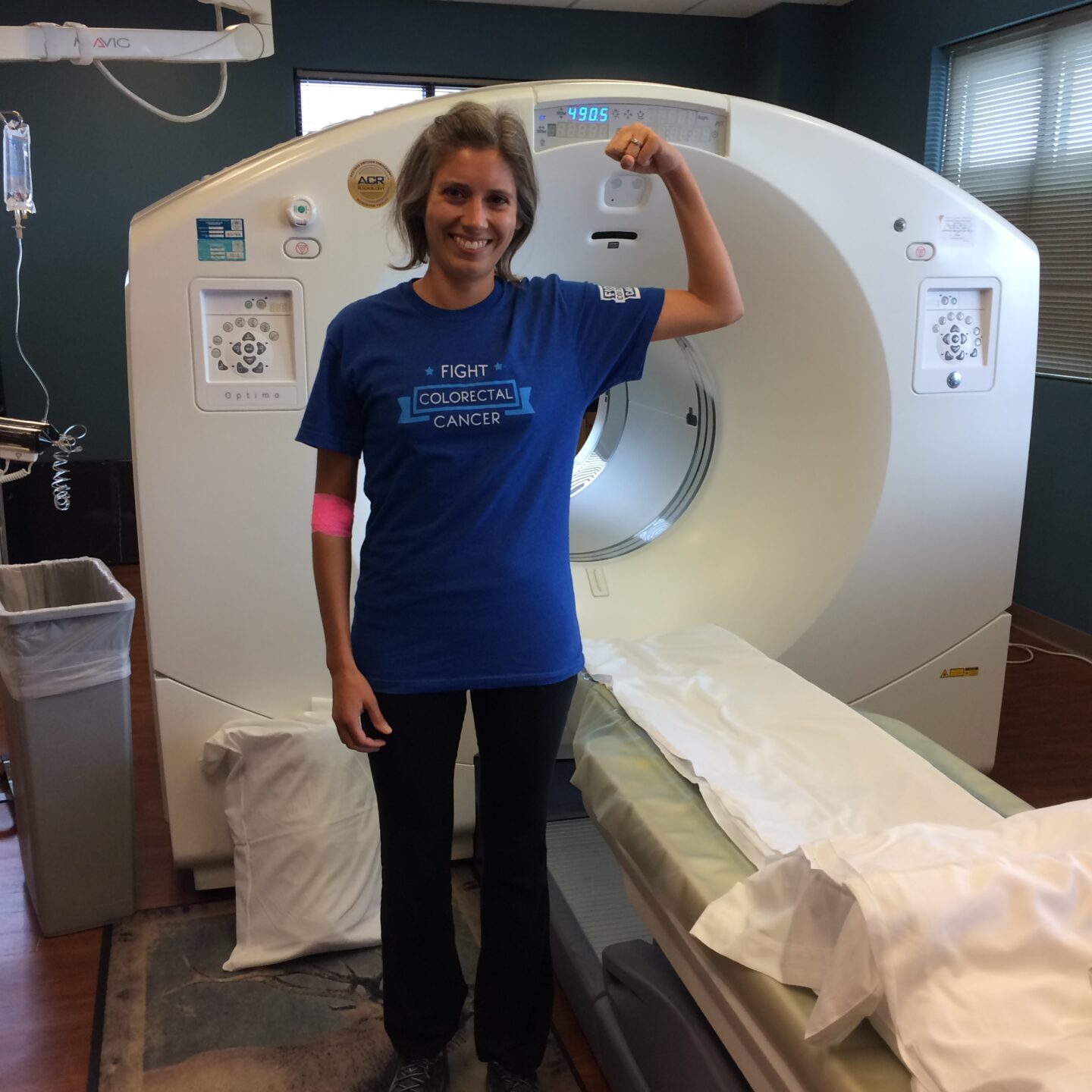

Over the next week, I did an a CT scan, I had an MRI, I had a rectal ultrasound so that they could see if lymph nodes were involved because it was difficult to see in the CT scan whether or not multiple lymph nodes were involved. In the CT scan, a lymph node lit up in my chest and they weren’t sure if it was cancer or not. They said typically if it had spread up into the chest, there would be a trail leading from the cancer up to there. To be sure, they sent me in for a PET scan, so there was another scan that I had to do.
Stage 3 Rectal Cancer Treatment
Considering traveling to receive the best medical care

Meeting with the oncologist, we hadn’t gotten the PET scan results yet but we had gotten CT scan and ultrasound results, so they knew it was at least stage 3 rectal cancer when I met with him. He explained what the standard of care was, what order treatment was going to go in, and what the next steps would be. Then from there, we went home, and researched is what he’s saying in line with what other people have done with what the standard of care is. Do we need to get second or third opinions?
We’re in Colorado Springs, so it’s a decent sized city, but we don’t have a huge medical center here. I have family in other states near big cancer centers. If this isn’t where I can get the best treatment and other places could, I want to know if I should be going out to Washington, to Ohio, or to North Carolina to seek options that may not be available to me here. After doing our research, everything that we saw lined up with what the oncologist was telling us.

I was comfortable with getting treatment here when we met with the radiation oncologist as well. I asked him if he thought we should seek out other opinions. He said, “I would put my ego aside if I thought you could get better treatment elsewhere. I would totally recommend you other places, but I feel like with your situation, you can get perfectly great treatment and we can handle your situation here.” That comforted me as well that we were making the right decision to stay in town for treatment.
What cancer treatments were you on?

I started out with 28 days of radiation and the oral chemotherapy Xeloda. For radiation, I went in 5 days a week Monday through Friday. On those days I took the chemotherapy pills. Saturday and Sunday were break days so I didn’t take anything on those days. I had 5 and a half weeks of that. The 4th of July and my sister’s wedding happened right in the middle of treatment so I had a couple of days off in the middle there. He cleared me to go fly to my sister’s wedding while I was going through treatment. Then I came back home and finished it up.

I rested for 2 months, which is what my surgeon wanted to give the radiation a chance to do its job as much as possible, because the tumor continues to shrink even after you’re done with radiation. My tumor was located low enough in the rectum that when we started treatment, if it didn’t shrink at all during radiation, then I most likely would have had a permanent colostomy when I had surgery. But the tumor shrank and it shrank in the correct direction, so my surgeon was able to remove the tumor and leave enough rectum so that I just needed a temporary ileostomy while the resected site had a chance to heal.
They took out about 12 inches of where the colon and rectum joined together, and they took out 17 lymph nodes during that surgery. Five of them were still positive for cancer. That meant I would do 8 rounds of the IV chemotherapy FOLFOX. I waited about 6 weeks after my surgery. I had the opportunity to heal and get strong again. They put in a port about 2 weeks before I started my first round of chemotherapy then every 2 weeks I would go in for FOLFOX. I finished that at the end of March in 2017 and rested a couple of months.
I really wanted to run a race at the end of May with some friends that we had done multiple years, and so my reversal surgery would have landed, if he waited 6 weeks, it would have been 2 weeks before that race. I would not have been able to have run it. I was like, can I wait a little bit? So I waited a week after. It was really 2 months after my final round of chemo when I had my ileostomy reversed.

What is an ileostomy?
The ileostomy is where they take a portion of your small intestine and route it out your abdominal wall. For mine, it was a loop ileostomy. If this was the abdominal wall and my little knuckle here is my small intestine, they just pull a little bit of it out. Then they cut a slit in it and peel it back so it’s still connected. It’s not fully severed and your waste goes out into a bag that you wear over it.


There’s different types of bags. There’s ones that you can change the whole thing or change part of it. The ileostomy, the output is a little more liquidy than usual because it’s your small intestine, so it hasn’t had time for the large intestine to take out some of that liquid.
»MORE: Navigating Life with an Ostomy
It was a little trickier for me doing changes of the bag because the output wasn’t as predictable as if you have a colostomy. It looks more like what you would normally pass when you go to the bathroom and it’s about that frequent a lot of times. Versus the ileostomy, you don’t have control. You don’t feel anything coming out. Sometimes you can hear it, but it was more difficult to change the bag because of that output constantly happening.
Reflections
What advice do you have for someone with an ostomy?
I would just make sure you have all the supplies, have things ready to clean yourself up, clean up any messes afterwards, and again, reach out to others for help. Also, on YouTube there’s quite a few people that have ostomies that have explained what works for them for bag changes and if things get irritated, what they do. So don’t ever feel like you’re alone. Look around. The internet is a great place for finding help through all of these things. So many other people have been through this, you just have to find them.

Are you receiving follow-up scans and tests?
It’s been maintenance and surveillance. I went in, at first, every 3 months for CT scans and checking my CEA and my bloodwork to make sure all my blood counts were bouncing back. Eventually, it got strung out to every 6 months, every year, and now I am just going in once a year for follow-up blood work and to check in with my oncologist.
The colonoscopy I did one follow-up one year after my surgery. I went in after 3 years, another 3 years, and after this past one that I went in this past week, everything looked good. There were no polyps, nothing suspicious. Now I get to wait 5 years until my next colonoscopy. I will be of a normal age of getting a colonoscopy for my fifth one.



The importance of finding a cancer community
I think one of the things that really helped me along the way, because I didn’t have any family members that had any history of cancer, so I didn’t have anyone nearby that I could reach out to. I looked online on social media. Social media can get a bad rap a lot of times, but it can be great in situations like this, to connect with others that are in your situation that may not be in your town or even in your country where you live.
I connected with so many others that had either finished treatment or were going through treatment at the same time as myself to just have that support group and know I wasn’t the only young woman that was going through this. There were other women across the country, in Canada, elsewhere, that were going through that same thing.
Social media can get a bad rap a lot of times, but it can be great in situations like this, to connect with others that are in your situation that may not be in your town or even in your country where you live.
We could vent to each other when we were really tired or ask, “Hey, is this bothering your system?” Or, “Oh my gosh, is your ileostomy going crazy too? What can you do to slow this down? What do you drink when you’re going through FOLFOX and you’ve got that cold sensitivity and everything has to be hot? I can only drink so much hot tea before I’m tired of it. Like, what else are you drinking?” Those are some of the things you don’t necessarily bother your oncologist about, but having a friend there to support you through can help bounce ideas off of you and help you feel like you’ve got a support group that’s there for you and that you can reach out to if you’re having a bad day.
»MORE: Read More About Cancer Support
More Colorectal Cancer Stories
Kristie C., Colon Cancer, Stage 4 (Metastatic)
Symptoms: None per se that she noticed; she experienced constipation and passed narrow stool, but had been experiencing constipation most of her life, and thought that these digestive issues could also have resulted from perimenopause
Treatments: Chemotherapy (including adjuvant chemotherapy), radiation therapy, ablation therapy (liver ablation), surgeries (colectomy, temporary ileostomy, ileostomy reversal, scheduled liver resection)
Briana H., Colorectal Cancer, Stage 3
Symptoms: Periods of constipation initially lasting one week and then extending to two weeks, nausea, pain in lower left abdomen, lack of appetite, vomiting and inability to keep fluids down
Treatments: Surgeries (colon resection, tumor removal, colostomy placement, colostomy reversal), chemotherapy
Kailee O., Colorectal Cancer, Stage 4 (Metastatic)
Symptoms: Sensitive stomach sometimes leading to vomiting after eating, bleeding during bowel movements, persistent fatigue, back pain, abdominal pain, anemia, significant symptom flare-up during second pregnancy
Treatments: Surgery (colectomy), chemotherapy, targeted therapy
Starr S., Colon Cancer, Stage 4 (Metastatic)
Symptom: Abdominal pain
Treatments: Chemotherapy, surgeries (colectomy, hepatectomy, lymphadenectomy), targeted therapy
Jackson L., BRAF Mutation Colon Cancer, Stage 4
Symptoms: Severe stomach pain, fatigue, lack of motivation, anemia, blood in stool, thinning stool
Treatments: Surgeries (emergency bowel obstruction surgery with temporary colostomy, possibility of HIPEC in 2026), chemotherapy, immunotherapy
Heather C., Colon Cancer, Stage 4 (Metastatic)
Symptoms: Severe bloating, indigestion, vomiting, rectal bleeding
Treatments: Chemotherapy, surgery (liver transplant, upcoming)