Lee’s Stage 4 Metastatic Relapsed Colon Cancer Story
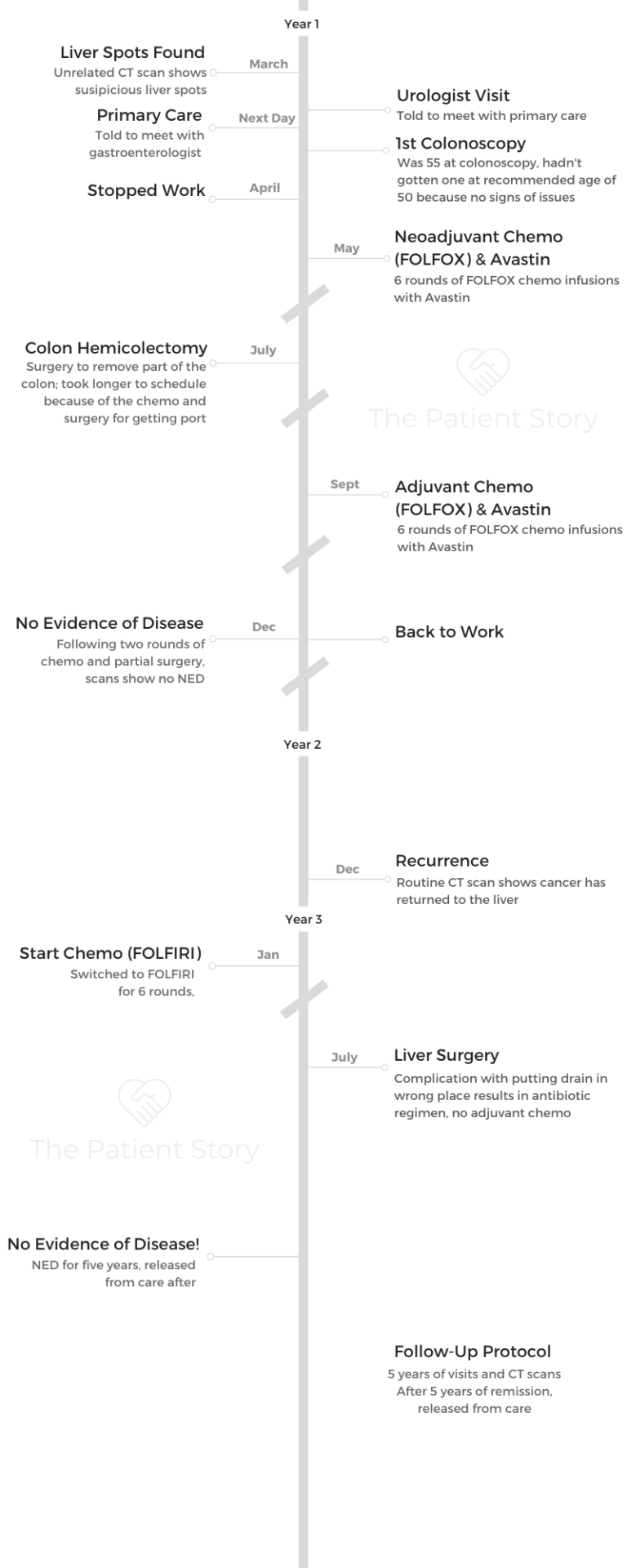
Lee shares his stage 4 metastatic colon cancer story, which included a relapse. He details his treatment, first-line chemotherapy, hemicolectomy (surgery), and chemo and liver surgery for the metastasis after the relapse.
In his story, Lee also talks about his shift to patient advocacy and navigating life after the colon cancer diagnosis, including managing the shift in work life and identity, the importance of having a caregiver during treatment, and the impact on his marriage.
- Name: Lee J.
- Diagnosis: Colon cancer
- Staging: 4, Recurrence
- 1st Symptoms:
- No first symptoms, unrelated exam showed spots on liver (metastais)
- Treatment:
- Neoadjuvant chemotherapy
- FOLFOX (infusion) + Avastin
- 6 rounds
- Hemicolectomy (surgical removal of part of the colon)
- Adjuvant chemotherapy
- FOLFOX (infusion) + Avastin
- 6 rounds
- Chemo after recurrence
- FOLFIRI
- Liver surgery (for metastasis)
- Neoadjuvant chemotherapy
- Topics of interest:
- How to be a self-advocate as a patient
- Patient advocacy
- Diagnosis
- Treatment Plan
- First-Line Treatment
- Describe the chemo regimen
- Describe the first treatment schedule
- Did you like your port?
- What was the neoadjuvant + adjuvant chemo regimen?
- How was it with the chemo pump?
- What were the FOLFOX chemotherapy side effects?
- What were the Avastin side effects?
- What have been the longer term side effects?
- Learning more info from your medical team
- Advocate for yourself by asking for what you need
- How was the colon surgery (hemicolectomy) after neoadjuvant chemo?
- Recurrence & Second-Line Treatment
- Second chemo after the recurrence
- There was some guessing involved with where cancer might be
- How did you decide whom to trust?
- Describe the plan and prep with the liver surgery
- What were the complications during the surgery?
- Describe the reaction to the anesthesia
- Describe the physical recovery from the liver surgery
- How long did it take to feel “normal” post-surgery?
- What was the follow-up protocol?
- Reflections
- Was there ever a moment where you felt a sense of relief?
- Any guidance on whether to work during treatment?
- Reconciling your work identity after cancer can be challenging
- Guidance to others on the work front
- How was your wife most supportive in the caregiver role?
- How did cancer impact your relationship with your wife?
- More access to latest treatments at big teaching institutions
- Why did you decide to keep your port implanted?
- As a patient advocate, what are the top takeaways for our readers?
- How are you doing now?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

No matter how bad your prognosis or diagnosis is, nobody knows. There’s some thinking that if I can just live another 6 months, they might find the cure to my type of cancer in the next 6 months, so let’s go for the extra time.
Sometimes people say, ‘I’ve had enough. I don’t want to do this anymore.’ That’s fine. People want care and to do hospice. Those are things that are there if they feel they need that.
Lee J.
Diagnosis
How did you know something was wrong?
It was totally unrelated to what was wrong. I was 55. Let me start off by saying I did not have a colonoscopy. I had no risk factors. I never smoked. I was not particularly overweight, though I’ve lost 40 pounds since then.
I exercised fairly regularly, hadn’t eaten red meat in 30 years, and no family history of cancer. I was busy. I had 2 teenage kids and a senior executive job in the government. I didn’t bother with a colonoscopy.
It turned out that I had a prostate infection. I went to a urologist. I had gone to him before. He gave me an antibiotic. It didn’t take care of the issue, so he had me get a CT scan to see what else might be going on.
They found 5 spots on my liver. I just happened to be back at the same hospital I had been to 6 months earlier where I had pneumonia and pleurisy. They thought it might be appendicitis because the pain was really low in my abdomen.
The same radiologist said, “These spots weren’t here 5 months earlier. You shouldn’t have spots on your liver growing in 5 months.”
That’s when they recognized something was wrong. I went back to the urologist, and he said, ‘You need to see your doctor.’ I saw my doctor, and he asked for a gastroenterologist that same week.
I went in for a colonoscopy, and they found the primary tumor in my colon.
Were you able to process the news of the tumor?
Totally unexpected. I had no clue that was going to happen. It was, “Okay, this is what I need to do.” I am an active cancer patient research and advocate now.
Back then, I don’t know if advocates really existed to this same extent. Maybe breast cancer? So it was, “I don’t know what to do. Tell me what to do.”
»MORE: Patients share how they processed a cancer diagnosis
What happened during the colonoscopy?
A tumor is bigger than a polyp. Polyp they can remove, but tumors they can’t remove during a colonoscopy. They can take a bite out of the tumor and get that biopsied, but the gastroenterologist could tell from looking at it that it was highly suspicious and (likely) cancerous.
Describe the colonoscopy process
For most people and myself, it’s the prep that’s the hard part. The food prep is having to eat bland, non-fibrous food for a couple days beforehand. You have to drink this stuff to purge your system. That’s pretty uncomfortable. You’re up in the middle of the night.
I just had another colonoscopy. I have one every 3 years now. I remember I had to take my last dose at 4 in the morning and be up until 6, then go in at 9 for the colonoscopy.
The procedure itself is nothing.
In fact, the first time, I remember I said, “When are you going to start?” They said, “Oh, we’re already done.” They give you this conscious sedative, and it’s really easy. It’s not pleasant, but it’s not unpleasant. It’s like good sleep. Then you’re done!
This last time, just a few weeks ago, the same gastroenterologist I had (in 2004) who diagnosed me said, “We found 2 polyps. We cut them out. They were biopsied, and there was no problem.” That’s how it goes.
It’s leading up to it that’s difficult. Of course, you hope the results are that they don’t find anything significant. I would recommend everyone get a colonoscopy at age 50. Now there’s recommendations to get one at age 45 because younger people are getting colorectal cancer.
Treatment Plan
What were the next steps?
I first saw a surgeon who said, “We don’t normally do surgery first at Georgetown University Hospital. You should get chemotherapy first.” I didn’t even know how to go about doing that.
It was a matter of, ‘I’ll do whatever.’ I didn’t know any better.
What held things up was trying to figure out what to do next. My wife called the National Cancer Institute helpline to ask what to do. She talked to her doctor, who had a relationship with Georgetown University. We’re in the Northern Virginia area. She knew some people at Georgetown, so that’s why we ended up going there. That’s how things happened.
They got started fairly quickly, but everything takes much longer than it’s going to take. There’s a lot of waiting.
Describe the various points of waiting time
A lot depends on the type of cancer you have and how they’re going to go about treating it.
One of the drugs I was going to be getting, something called 5FU, required an infusion over time, so I had to get a mediport put in, which is outpatient surgery but is still a surgery. They make a cut, and they put it into your jugular because it’s a central line.
Also, one of the drugs they were going to give me before my colon surgery was something called Avastin, which has effects on the blood system. It can cause bleeding, so they have to wait. Even after the mediport was put in, they had to wait a certain amount of time before I could start getting the chemo.
How did you process the stage 4 diagnosis?
I knew from the beginning, since they found the spots in my liver, that when they found the primary tumor, it was stage 4. It had already spread to my liver. I don’t know if that’s good, at least knowing that first step and how bad it’s going to be.
I remember going home after the colonoscopy and going on Dr. Google, of course, looking at stage 4 colon cancer. The 5-year survival rate was 7%, people who survive 5 years.
I guess I was stunned and didn’t think about it. I was really able to compartmentalize my thinking, and I was thinking, “There’s nothing I can do about that.”
»MORE: Patients share how they processed a cancer diagnosis

How did you break the news to your loved ones?
The gastroenterologist comes in after the colonoscopy and says, “Here are the results.” I remember he gave me a picture from the scope that showed the tumor. I still have that. My wife had taken me because you have to have a driver come in with you.
I had 2 teenage sons at the time. We told them what the situation was. In a way, it’s fortunate they were teenagers because they had their own issues they were dealing with.
In fact, only recently, my younger son, who is 30, said, “Dad, I never realized how seriously sick you were.”
For one thing, I didn’t look like I was sick. I didn’t act normally like I was sick, but I would sit in my chair all day recovering from chemo. They’d be off at school and doing things with their friends, so that was good. There was no reason for them to suffer any more than they had to.
I have realized that the caregiver really, in some ways, suffers more than the patient. The patient, all you have to do is everything you have to do. Give me this; give me that. I’ll do the best I can.
The caregiver has to do everything else — everything they had done before, everything that you were doing before, and then taking care of you. That’s really a tough role. Tougher than the patient role, I think.
»MORE: Breaking the news of a diagnosis to loved ones
How did your wife process the news?
I think like most of us, she hid her feelings. There’s only one time through the whole process that I recall fearing that I might not live. We never talked about that. She never broke down and cried. It was always she was supportive.
One thing she really was good at doing was, “You’re supposed to be taking this medication at this time. Be at this place at this time.” It was more staying on schedule, doing what needs to be done, and keep the process moving than tears and whatnot. That was good.
Even my oncologist was much more of a scientist. There was not a lot of touchy-feely stuff, which was fine for me. It’s what I needed. I didn’t miss anything else.
»MORE: Read different experiences of a cancer diagnosis and treatment
Changing your diet pre-surgery
One interesting thing is I hadn’t eaten red meat for 30 years. I had a great high-fiber diet. Because I had a tumor in my colon, they were concerned that if it got blocked, I would need to have emergency surgery. I had to go on a low-fiber diet, eating all those things I had never eaten for so many years.
I couldn’t eat the things that I loved to eat. I had to eat white bread and couldn’t even have whole wheat bread. This just made it seem longer, but during this time, I had no idea what was going on.
They couldn’t tell me how I might respond to the chemo [or] what the course of the whole process would be. All I knew was I’d be going in for colon surgery.
First-Line Treatment
Describe the chemo regimen
There’s an infusion center, and it had a whole a bunch of recliners all around the room with curtains around them. They have the infusion nurses who come in. For the 5FU, they give you bolus infusions at the center.
I had the rest of the chemo with something called FOLFOX, 5FU, oxaliplatin, leucovorin, and then they added the Avastin to it. Coincidentally, and I think very fortunately for me, Avastin had just been approved the month before I got diagnosed. I was diagnosed in March, and it was approved in February.
So I was one of the first people that used it as treatment for stage 4 colon cancer.
Describe the first treatment schedule
Summary: 6 rounds neoadjuvant chemo, colon surgery, 3 months scans, 6 rounds adjuvant chemo
There’s neoadjuvant chemo, which means getting chemo before the surgery. Even now, for most institutions, people who are treated for colon cancer get their chemotherapy after surgery. In my case, what they wanted to do was control the growth of the tumors in my liver.
As my oncologist said, no one’s going to die from a tumor in their colon, but they will die from tumors in their liver. There’s neoadjuvant, and then there’s adjuvant chemo, which is chemo you get after the surgery.
Did you like your port?
That was my first thought: “Oh my gosh, I have a foreign object inside my body now.” First time ever. I had never been in a hospital, never that sort of thing.
The only time it got plugged up was when I was in the hospital having it accessed regularly. They had to give me TPAs to go in and open it up. Otherwise, I have great blood flow. I never had a problem with it.
What was the neoadjuvant + adjuvant chemo regimen?
It was every 2 weeks, about 3 or 4 hours (each time). When they were done with the infusion, they hooked up the pump, so I had a fanny pack with a pump. It was 32 hours that I had to have that (pump) infusion. Then I’d have to go back in after.
I had 12 infusions, neoadjuvant and adjuvant, both 6 each time.
How was it with the chemo pump?
It was really hard to sleep with that thing on. Sometimes in the middle of the night, the pump would clog up and start beeping. It was a nightmare.
I just found part of the problem was being able to roll over at night because you hit the pump, you can’t roll over, and I just never got a good night’s sleep.
But the pumps today are better than when I had one. Just do what you have to do. If that’s what it takes to get through the process, it’s not fun, but it’s necessary.
What were the FOLFOX chemotherapy side effects?
One of the side effects from all the platinum-based drugs (like oxaliplatin, which is in FOLFOX) is peripheral neuropathy. For me, it was miserable at the time.
Any time going to the refrigerator or freezer — and I had always done all the cooking at home, so I would go into those a lot — it would feel like burning. Even going outside in the winter, any exposed skin would feel like it was burning.
I know people who had oxaliplatin and who’ve had neuropathy for years afterwards. Fortunately, for me, it went away fairly quickly, even to the point where I was able to play guitar in a band 2 years after my treatments ended. My fingers were still nimble, but for other people, there’s pain and tingling for years afterward.
What were the Avastin side effects?
There are a lot of things they don’t tell you about. It turned out after 12 rounds, I started getting allergic reactions. They said, “Don’t worry, we found after 12 rounds with Avastin, people get allergic reactions.” They just gave me Benadryl through my IV, and it went away.
But they didn’t tell me that in advance. You learn that after it happens. It was like, ‘Why didn’t you say something about that? I could have been prepared.’
»MORE: Read more patient experiences with Avastin
What have been the longer term side effects?
There’s another thing I’ve learned as an advocate. Both Avastin and 5FU have potential cardiac issues that are late effects. They don’t happen till years afterwards.
There’s also one for breast cancer (trastuzumab) that they know about, so for someone treated with that drug, they will usually do a cardiac workup at the time.
We found there are these late effects they don’t tell you about, that primary caregiver doctors don’t know about.
I was actually at a patient group talking about this. They had no idea this would happen until they got to the point where they couldn’t walk up the stairs at home because of their cardiac issues. It was, “Why didn’t you tell them?”
A lot of it is because they got treated when they were in their teens for non-Hodgkin lymphoma, and the drug they got and radiation near the heart would have that effect as well.
They didn’t know, their primary doctors didn’t know, so it was only when they were at the point where they could not carry on a normal life that they found out they had a problem.
Learning more info from your medical team
It’s just full disclosure and honesty. It’s a trust relationship. We trust our oncologists because we have to, but why did you hide that from me? Why didn’t you just tell me about that?
Most of the time, they do disclose what the side effects of the drugs you take might be. I know Avastin had a lot of potentially very harmful, potentially deadly side effects.
I knew it was a possibility, but what do we do? We have to assume that it will work out for the best. Otherwise, we’d never do any of this stuff.
There are a lot more resources for patients now. The whole industry from the Food and Drug Administration, which does patient-centered research, there are a number of things I’m involved with as a patient advocate that I don’t think existed before. There was Komen years ago. They had patients involved for a long time, but I don’t think other cancers had that input from patients.
Advocate for yourself by asking for what you need
One of the things I believe in is if you need pharmaceuticals, you should get them. I told my doctor I had trouble sleeping, so he gave me sleeping drugs.
At one point, I said I was feeling pretty depressed, so he gave me Paxil for depression. It was up to me, [what] I was feeling with everything, to say, “I don’t really need this anymore. I shouldn’t have any trouble sleeping; I’ll stop this. I have no reason to be depressed.” I woke up one day and said, “I’m fine. I don’t need this.” I worked with my primary care doctor to wean off the Paxil.
If you have issues, don’t think, “I have to be strong, and I can’t weaken to that.”
If you have pain, deal with the pain. If you have depression, deal with the depression. If you have constipation, diarrhea, or vomiting, deal with it. Don’t just feel you have to suffer through everything, because there’s enough suffering to go around.
»MORE: How to be a self-advocate as a patient
How was the colon surgery (hemicolectomy) after neoadjuvant chemo?
It was a right hemicolectomy, so they took out 20 inches or so of my colon to make sure they got the margins. I had no problem with that surgery at all. I thought, “Oh, this is pretty easy.”
When I was finished with that, I had to have CT scans every 3 months to see what the status was. After I finished that, I had the other 6 rounds over what would have been 12 weeks post-surgery.
I had no evidence of disease. I thought that I was cured. I had my colon surgery. No evidence of tumors or spots in my liver anymore; I’m cured.
They never told me that chemotherapy typically does not cure colorectal cancer. Surgery cures it. I found out about a year later when the cancer recurred or showed up again in my liver that no, it hadn’t cured it. I was just “NED” (no evidence of disease), and now I had to go through liver resection.
Recurrence & Second-Line Treatment
Second chemo after the recurrence
After the recurrence back in the liver, my oncologist said, “Just in case your tumor’s gotten used to the oxaliplatin, they went with irinotecan.” It became FOLFIRI rather than FOLFOX. Otherwise, it was the same, except for the irinotecan.
The difference is irinotecan tends to have more gastrointestinal issues and not the peripheral neuropathy. It was to mix it up for the cancer, because cancer cells get resistant to the chemotherapy drugs and they’re still trying to find out why that is and overcome it.
One way to overcome it is to change the drug so even the cells that had resistance to it, then the other drug might come through and kill it. That’s indeed what happened.
There was some guessing involved with where cancer might be
Interestingly, after it recurred, the liver transplant unit that was going to do my surgery looked at my CT scans and said, “I don’t really think there are live cancer cells in this gray mass in the scan. We don’t really know enough about how Avastin affects those things, so I don’t think we really need to do the surgery.”
But my oncologist said, “We need to do that. The fact that we don’t know is not a reason we shouldn’t do it. Let’s go ahead and do it.”
After the surgery, they did the biopsy of the tissues they took out, and there were live cancer cells in there. The oncologist was right; the liver surgeon was wrong.
How did you decide whom to trust?
I had a relationship with my oncologist. I’d been seeing him for a year and a half at that time. The surgeon was late to the game, so I figured I’d rather be safe than sorry.
I’d gone through the colon surgery so well that I thought the liver surgery would be another piece of cake, which it wasn’t. It just made sense to go forward with the liver surgery.
Describe the plan and prep with the liver surgery
There really was no prep. The only thing was I had to wait 3 to 6 weeks from the last Avastin I had to going into the surgery. Otherwise, you could have bleeding effects.

What were the complications during the surgery?
They say don’t have major surgery in July because July is when the new bunch of residents come in.
I had my surgery on July 3rd. My wife still reminds me there was a conference I wanted to go to that was being held earlier. I could have had my surgery scheduled then, but I wanted to go to that conference, so I did. July 3rd was the next time I could have it done.
It turned out that somebody, whether it was a new resident, put the drain in the wrong place. The colon surgery took out my appendix, which I didn’t need anyway.
In the liver surgery, they took my gallbladder as well, but you end up getting bile. Because it has to go somewhere, they put a drain in to drain that bile.
They put the drain in the wrong place, and the bile was accumulating in my abdomen and getting infected. From July through September, I was going in and out of the hospital, in and out of the emergency room.
I’d be at home taking my temperature all the time. If it was over a certain temperature, I needed to come in. It was just a horrible period of time getting the antibiotics all the time.
They ended up putting a PICC line in my arm and giving me IV antibiotics at home for a month, so my wife was doing that. Then she had to take our older son to college, so we had to teach the younger son how to disconnect the PICC line because I couldn’t even think about doing it.
I would just get sick. That’s when I got the sickest and lost the most weight. It was from those antibiotics for a month. IV twice a day, serious antibiotics to try and get rid of this infection.
I had to go back into the group called Interventional Radiology, which is not standard radiology. It uses technology to do other procedures. They had to thread a tube in through my back and missed my lung to put the drain in a different place, so it would start draining that bile. Over time, that worked. It took a while. I kept watching the stuff filling or not filling the pack that I had for the drain.
Describe the reaction to the anesthesia
I had a real hard time [with] the liver surgery. I was hallucinating after I came out from that anesthesia. When I shut my eyes, I could see — for some reason, it was documents. I wasn’t sure whether I was really seeing documents from somewhere or whether I was making all this stuff up. It was in a way disappointing when I closed my eyes and stopped seeing that stuff, because I had gotten so used to it.
General anesthesia can itself have that effect. I don’t recall that at all from the colon surgery, but I think the liver surgery was a longer period of time of being out of it.
It was much tougher coming back to real life than the colon surgery had been.
Describe the physical recovery from the liver surgery
There’s the lung capacity after the general anesthesia. I remember blowing on this thing and having the toughest time. My wife was in there, and she was making me walk, just get my pole and walk around. I thought, “I’m sick. I can’t do this.” But you do it, and after a while, it works fine.
Actually, the thing I think was the worst was when you have a catheter in, and they want you to be able to urinate on your own.
If you can’t in a certain amount of time, they threaten to put the catheter back in, which means it’s a very painful process you don’t want to go through, so you’d better work even harder at it than you had been.
The other thing I remember is when I was in the room for recovery, the attending physician wanted to bring some new students in to talk to me, because a lot of these people have never met a patient.
You can go all the way through med school without probably meeting a patient or at least talking with a patient, other than doing a workup on them.
- How do you feel?
- What was this like?
- Is there anything that could have been done differently?
- Any advice for us?
The attending asked if I would do that, and I said, “Sure, I’d be happy to help out.” It was one of my first advocacy roles in trying to help out other people. They could learn from me and be able to better treat their patients.
How long did it take to feel “normal” post-surgery?
It was probably Halloween, so from July 1st to October 31st. That’s when the infection was gone.
What was the follow-up protocol?
After the July surgery, for colorectal cancer there’s a 5-year surveillance process, where you can get CT scans every 3 months, then every 6 months, then once a year.
My regular oncologist was gone. I talked to a new guy, who said, “Well, nothing more we can do for you. Nice to meet you; have a good life.”
The health care establishment doesn’t like to use the word ‘cured’ because there is no cure for metastatic cancer. But I’m not a medical doctor. I can say whatever I want.
I want to say I’m cured because I haven’t had any evidence of disease since 2011. If I have it now, it’ll probably be a second cancer.
Reflections
Was there ever a moment where you felt a sense of relief?
After that one year of no evidence of disease and then they found it again, I was not going to trust anything, even after 5 years. There’s always that fear of recurrence.
During those 5 years, I worked out a process where I’d go to the radiology lab after my CT scan, give them my fax number at home, and have them fax me the radiologist’s results so I did not have to wait for my oncologist to let me know.
I learned a lot through this whole process, so I didn’t want to wait. I wanted to know if there was going to be a problem. If there was a problem, I was just going to deal with it. Let’s go through it again. That’s fine.
There’s always that fear of recurrence, no matter how far out you might be from your cancer, particularly if it’s metastatic. You know if there’s one cell in there they didn’t get and your immune system didn’t catch it, it could be growing somewhere.
Any guidance on whether to work during treatment?
Whatever that takes to get through. For some people, it’s work. We want to talk about work — my attitude was my primary job is to stay alive and get better.
I was a senior executive in the federal government at the time. I had a $20-million budget and 100 people in contract who were working for me through the first time (of cancer).
There was someone going through lung cancer. He was at work every day — it was amazing — and then he [passed away]. I guess I was willing to not be applauded for being at work every day and being an amazing worker.
I took a year, essentially, going through my first round of cancer and lost 3 jobs as a result of the cancer for various reasons. At a senior executive level, they expect you to perform 80 hours a week, and you’re not always able to do that, particularly after going through the liver surgery.

Reconciling your work identity after cancer can be challenging
I felt that I was treated very unfairly. It turned out that the deputy I had put in that position, who had thought she should have gotten my job to begin with before I came in, ended up convincing a temporary political appointee at that organization that I was not competent and that she should have my job.
When I came back, they were really quick to shuffle me off into nowhere, into essentially a do-nothing job in an entirely different office that happened to have a slot that I could fit into. I spent most of my time trying to find another job.
I did and liked the job that I had, but 3 months later I got diagnosed with a recurrence. When I was off of that job, they laid me off. They had a long-term disability program, which I was on, and I was on social security disability as well.
After they laid me off and I got better, I happened to run into a guy at a conference, who hired me as deputy chief financial officer at a different agency. I only lasted there a year because that was when I couldn’t work 60 to 80 hours a week. Then I went back to that on a part-time basis for another year before I started working on a more full-time basis.
Guidance to others on the work front
It’s a matter of setting your priorities.
Fortunately, my wife was always one to say, “I’d rather you have more time with your family than make more money. We have enough money.” She was a lawyer for the government; she had a good job. I didn’t have to be out there working.
I had one opportunity between going with a big-name consulting company doing work on the West Coast — and I live in Virginia — versus being a vice president for a bank based in Pittsburgh. She said, “I don’t want you on the West Coast every week. We don’t need that.”
It is good to have a spouse or caregiver or significant other who agrees with your priorities and helps you set priorities that are more reasonable than, “I have to get out there and be the big shot again.”
It was tough to go through that whole devolution process after working so hard to get up to the top, but ultimately, being alive is much better.
I enjoy being a cancer research advocate a lot more than I ever enjoyed my senior executive job in the federal government or my job as a bank vice president, my job running my own consulting company, or any of those kinds of jobs. It’s nice.
How was your wife most supportive in the caregiver role?
She was really great at keeping me organized and keeping us organized. “You’ve got to be here at this time. You have to be doing this or that.”
I know when I was recovering, I sometimes felt like when she was getting me back to normal, I wanted to be the sick guy. “Don’t bug me. I’m sick. I don’t want to do that. I don’t want to take the garbage out this week.”
Sometimes that tough love is what you need, because the goal is to get back to some semblance of normalcy. The closer to that previous normal, the happier you’re going to be and the happier everyone else is going to be.
It’s easy to play the sick patient role, and I know there were lots of times I just didn’t want to do anything. No, I don’t want to go for a walk or do this. Ultimately, it turned out to be all for the best.
That’s as much as I could ask for.
How did cancer impact your relationship with your wife?
Probably like a lot of men, I’m not as demonstrative as women tend to be. I think my wife being a lawyer, she’s not as demonstrative as someone else might be or as emotional as someone else might be. We are well matched in that area, so we dealt with things we had to deal with.
Now, we’re both retired, and literally we can be sitting 6 feet away from each other all day long and not say a word or 2 words. I’m doing my thing, she’s doing her thing, and there’s nothing we need to deal with.
I think a lot depends on the nature of that relationship and how you communicate to begin with. I can’t say I found spiritualism or anything else. I certainly did find that there were things more important in life than a job, even a high-level or high-esteem kind of job.
»MORE: 3 Things To Remember If Your Spouse/Partner Is Diagnosed With Cancer
More access to latest treatments at big teaching institutions
You do have opportunities to get the latest in treatments. There needs to be some way we can get these things to community hospitals, where the majority of patients are treated. It’s not right that they don’t get access to these things, especially some of the clinical trials they have at teaching hospitals.
People recognize this as a problem, and I think they’re trying to work on it. I’m an advocate on a group, and we do a lot of work, especially non-drug trials. I’m on the survivor committee, so we do a lot of trials to these NCORP community-based centers.
Why did you decide to keep your port implanted?
I still have my port in. Most people don’t, but I wanted to remember what I went through. A lot of people want to forget about the process, but especially as an advocate, I want to remember because I’m talking to people who are having the issue.
I’m talking to doctors and researchers who are doing research on this. It helps me remember what it was like to be a patient and on the other side of this whole process, not the side I’m on now.
I do have to go into the infusion center every 2 months (for maintenance), so I get to talk to the patients in there for their chemotherapy. I get to talk to the oncology nurses. It helps me stay connected.
As a patient advocate, what are the top takeaways for our readers?
Most people I work with all day long are researchers and doctors these days. Many times I’m the only non-PhD in the room, which can be very intimidating. They generally try to be nice, even when they don’t pay attention to what I say.
What I’d say is there are things you can do to improve your health outcomes. To the extent you can do those things and the younger you start doing those things, that’s good, because it may pay off when you’re older.
Number 2, no matter how bad your prognosis or diagnosis is, nobody knows. There’s some thinking that if I can just live another 6 months, they might find the cure to my type of cancer in the next six months, so let’s go for the extra time.
Sometimes people say, “I’ve had enough. I don’t want to do this anymore.” That’s fine. People want care and to do hospice. Those are things that are there. People need that if they feel they need that.
The same is with medications [and] stuff you get to make yourself feel better to get through the process better. That helps.
The third thing is whether you’re in treatment or out of treatment, being an advocate and helping other people is always going to be a plus for you. It’ll make you feel a whole lot better than anything else you’ve ever done in your life probably. It’s so needed. Patients need it. The research community needs it. Hospitals need it. Doctors need it.
There are lots of different things you can do, like going in and helping people navigate through the process in the hospital or giving talks at your local Lions club on colonoscopies or whatever.
Every state has a Cancer Action Plan. I got involved with my state, Virginia’s Cancer Action Plan and on the board of directors for the Cancer Action Coalition of Virginia. I’m trying to help my community deal with cancer better.
There are lots of things you can do, so those are the 3 big things I found to be most helpful for me and help me get through this better than when I started.
How are you doing now?
I’m really lucky. I have no real health issues and have recently been able to get to the 150 minutes of exercise that the American Cancer Society recommends for cancer survivors. I’m exercising more than I was before the coronavirus!
Inspired by Lee's story?
Share your story, too!
Colon Cancer Stories
Kailee O., Colorectal Cancer, Stage 4 (Metastatic)
Symptoms: Sensitive stomach sometimes leading to vomiting after eating, bleeding during bowel movements, persistent fatigue, back pain, abdominal pain, anemia, significant symptom flare-up during second pregnancy
Treatments: Surgery (colectomy), chemotherapy, targeted therapy
Starr S., Colon Cancer, Stage 4 (Metastatic)
Symptom: Abdominal pain
Treatments: Chemotherapy, surgeries (colectomy, hepatectomy, lymphadenectomy), targeted therapy
Jackson L., BRAF Mutation Colon Cancer, Stage 4
Symptoms: Severe stomach pain, fatigue, lack of motivation, anemia, blood in stool, thinning stool
Treatments: Surgeries (emergency bowel obstruction surgery with temporary colostomy, possibility of HIPEC in 2026), chemotherapy, immunotherapy
Heather C., Colon Cancer, Stage 4 (Metastatic)
Symptoms: Severe bloating, indigestion, vomiting, rectal bleeding
Treatments: Chemotherapy, surgery (liver transplant, upcoming)
Nicole S., Colon Cancer, Stage 3
Symptoms: Dull lower abdominal pain that sharpened and was focused on the lower left side, appearance of dark blood in stool, difficulty retaining food due to near-complete blockage of sigmoid colon
Treatments: Surgery (colectomy), chemotherapy
Ian D., Colon Cancer, Stage 3C
Symptoms: Fatigue, unusual blood test results during annual physical, blood in stool
Treatments: Surgery (partial colectomy), chemotherapy, clinical trial





