Jason’s Stage 3B Colon Cancer Story
Interviewed by: Alexis Moberger
Edited by: Katrina Villareal

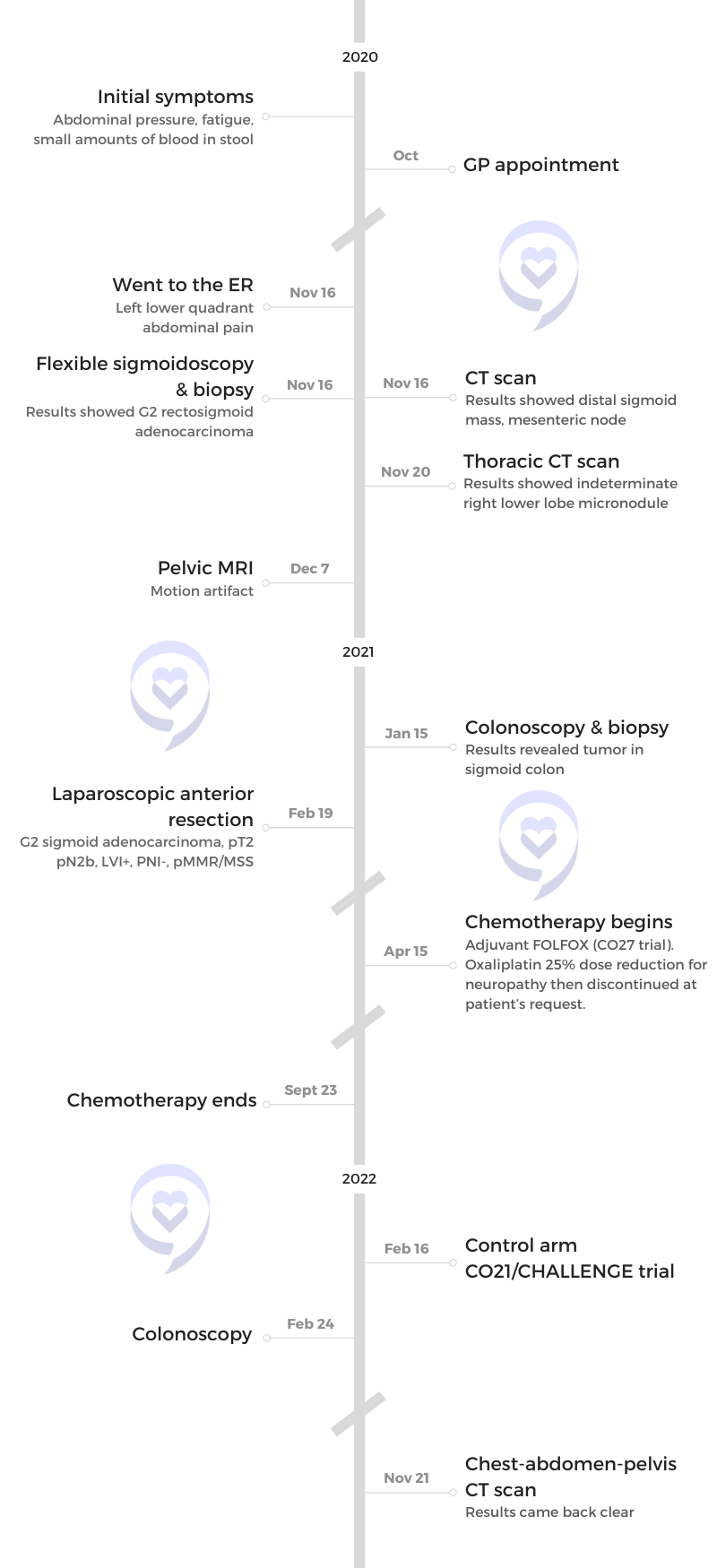
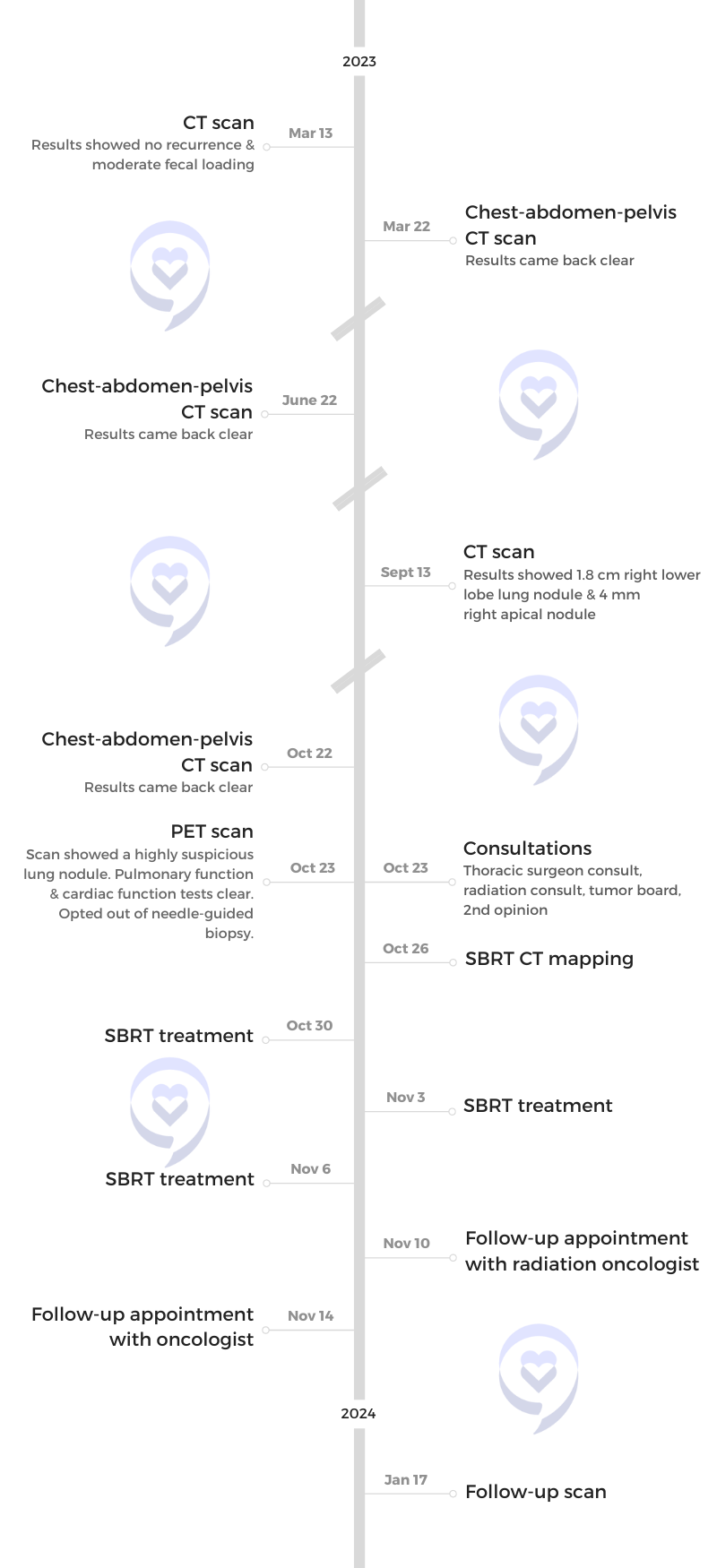
Jason was diagnosed with stage 3B colon cancer at 36. He first experienced minor abdominal pain and blood in his stool. His concern grew after repeatedly encountering colon cancer in online searches.
No abnormalities were detected after a visit with his general physician. Despite reassurances that colon cancer is unlikely in a healthy 36-year-old, he pushes for a colonoscopy referral.
Because of pandemic delays, his anxiety grew, leading him to seek emergency room evaluation. A CT scan revealed a mass in his colon and enlarged lymph nodes while a subsequent colonoscopy confirmed the presence of a tumor. Pathology results indicated the presence of cancer cells in some lymph nodes.
Jason reflects on the shock of the diagnosis, the emotional impact, and the difficulty in breaking the news to family and friends. Throughout his journey, he learned the importance of actively participating in one’s health care, advocating for oneself, and seeking support from organizations and communities. He also highlights the impact of a cancer diagnosis on caregivers and the need for a strong support system.
In addition to Jason’s narrative, The Patient Story offers a diverse collection of colorectal cancer stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
- Name: Jason A.
- Diagnosis:
- Colon cancer
- Staging:
- 3B
- Symptoms:
- Abdominal pressure
- Fatigue
- Small amounts of blood in stool
- Treatments:
- Surgery: colon resection
- Chemotherapy: FOLFOX (folinic acid, fluorouracil, and oxaliplatin)

This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
Introduction
I live in Ottawa, Canada, with my wife Leslie, our three-year-old daughter Kira, and our dog Sage.
I love the outdoors. I’m a big runner. Over the last few years, a big passion of mine has been doing a lot of advocacy work and peer support in the cancer world.

It was the blood in the stool that got me thinking there was something more going on.

Pre-diagnosis
Initial Symptoms
My story started when I was 36. I was a healthy, active, very typical 36-year-old adult. I was in the prime of my life. I was happily married and work was going well.
I started getting very minor abdominal cramps and pains that I’d never really felt before. I thought it was stress, something I ate, or a pulled muscle. I didn’t think anything of it.
Then I started to have a little bit of blood in my stool. It was very, very minor. It could have very easily been passed off for hemorrhoids, an inflammation in the intestine, or an infection in my GI tract.
But when I was searching “abdominal cramps, blood in the stool” on Google, colon cancer kept coming up. It wasn’t on my radar, to be honest, but the fact that it was there got me thinking about it. I got concerned when that started popping up over and over again.
Seeing a General Physician
In September 2020, I went to see my GP. I don’t think my early symptoms were what you often hear. I wasn’t in debilitating pain or needed emergency surgery.
My doctors even said they didn’t necessarily know if that had anything to do with the colon cancer because it was so mild. It was more like a nuisance. It was a little bit of pressure here and there, the odd spasm-like sensation. It came and went. There was nothing persistent. There was nothing that affected me dramatically. It wasn’t something that concerned me. It was the blood in the stool that got me thinking there was something more going on.


My tumor was quite small. It was only about 2 x 3.5 cm. Because of the size and where it was, which was in my sigmoid colon, my doctors don’t believe that a lot of that pain even had anything to do with that. At the time of my diagnosis, I had a very physical job. I was running and working out all the time so it could have been anything.
My GP is awesome. We have a great rapport. She has my back and has always taken good care of me. The day I went in, it was clinic day and they had residents working with the doctors. I got to meet one of her residents who was probably around the same age as I was.
He did everything I was expecting. He asked all the questions. “How long have you had the symptoms?” “Are they impacting bowel movements?” “Are you eating?”
Because of the blood, he did a digital rectal exam, but he didn’t feel anything nor was there anything odd so he left it as potentially an infection. It could be an inflammation from a hundred different things. Hemorrhoids and stress came up, the typical stuff you hear when you have things going on in your stomach. But I pushed back a little bit because I was concerned that I kept seeing colon cancer come up every time I searched on Google.
Part of the visit I always try to highlight was him looking right at me and saying, “Mr. Abramovich, you’re 36. You’re healthy. This is not cancer.” At the time, that was reassuring. When he said that, it was a huge weight off.
I still saw my actual GP afterward and she was honest. She did say that it’s very unlikely. She didn’t dismiss my concerns, but it was unlikely that a healthy 36-year-old adult had colon cancer and that was a fair assessment.
However, she’s quite diligent. She asked if I wanted to have a referral for a colonoscopy and I said, “Absolutely. That’s what I was hoping to get out of the appointment.” I hope the resident that I saw found out what happened. It happened right in front of him. He sat with a healthy, 36-year-old male and said, “It doesn’t happen to young adults.”
The scary thing was how many other patients he could’ve said something like that to. This was a brand new doctor who still thought that young adults couldn’t get this disease. It’s disheartening that it hasn’t hit home yet in medical school that it could happen to anybody.

My anxiety was getting quite high and I was getting worried… There was too much waiting and I wasn’t doing well with it.

Diagnosis
Going to the Emergency Room
My situation unfolded a little bit differently in the sense that this was all during the pandemic so everything was a little bit delayed. I had a little bit of a wait to get a colonoscopy because I wasn’t presenting urgent symptoms. It was more exploratory.
I was on a two- to four-month wait to get that colonoscopy done. However, my GP is an ER physician as well in the hospital and said, “If it’s getting worse or you want to get this solved quicker, go to the ER so you’ll have access to this a lot quicker.”
After a couple of weeks, my anxiety was getting quite high and I was getting worried. My wife had very gently encouraged me to go to the hospital and get it looked at for the good of my mental health. There was too much waiting and I wasn’t doing well with it.
I ended up in the ER because some of the symptoms were getting a bit worse. Again, I was looked at as a healthy 36-year-old adult. They did a physical exam. My blood work came back perfectly. My CEA was 1.8. It’s never changed. It’s always stayed at that so they were leaning towards diverticulitis, stress, inflammation, and everything they consider before cancer because of my age and my health.
Getting a CT Scan
The ER physician decided to do imaging. He wanted to do a CT scan to confirm what his thoughts were because he didn’t want to give me antibiotics unnecessarily.
I came back the next day and did the CT. About an hour later, he called me. I knew right away that something was wrong. From working in emergency services, I know people’s demeanors and the whole process of giving someone some bad news so I knew right away that something was up when he called me back.
He took me back to a private room, sat down on the bed right next to me, showed me my CT report, and said they found a mass in my colon. They also saw some lymph nodes that were enlarged regionally in that area.
Colonoscopies are not scary at all. They’re pretty smooth and painless.
Getting a Colonoscopy
I didn’t have a colonoscopy until after they found the tumor on a CT scan.
Colonoscopies are not scary at all. They’re pretty smooth and painless. To be honest, the most uncomfortable part is the prep to clean out your bowels but, at the same time, it’s not that bad. You have to drink a whole bunch of liquid that doesn’t taste very good.
Would I rather not have to do them? Absolutely. But at this point in my journey, I’ve had about 3 or 4 of them.
When you get the procedure done, you’re comfortable. I didn’t feel a thing. The staff was great. They gave me the choice to be awake or be totally out based on my comfort level.
The whole procedure lasted about 25 minutes. In my situation, I found it neat and a little empowering because I stayed awake. My surgeon did my colonoscopy and showed me my tumor. She explained where it was exactly and gave me an idea of what was going on, which I thought was cool because you never really get that perspective.
A procedure that could save someone’s life or make a drastic difference in an outcome is a no-brainer. I talk a lot about colonoscopies because a lot of people are scared of them or don’t want to do them. There are so many myths about them, but they’re quite simple, pretty comfortable, and quick procedures to get done.
Reaction to the CT Scan Results
I was in complete shock. This was the complete opposite of what anybody thought that was going on.
Unfortunately, given the pandemic, I was alone. It was not a pleasant situation. I know the staff felt quite bad as well. They were doing their best to comfort me and do what they could.
I was able to call my wife to let her know what was going on, but she wasn’t allowed in the hospital. She drove down and waited in the parking lot in case I needed anything.
I had an amazing medical professional. The nurse I had that day was phenomenal. She was a blessing in disguise in a difficult time. We were very similar in age so I think what was happening hit home to her.
The rest of that day was a blur. I was fortunate that my GP had a lot of connections at that hospital. I got a quick emergency procedure done to do a sigmoidoscopy and get a biopsy done.


Getting a Sigmoidoscopy & Biopsy
When I woke up, the general surgeon was very open with me. He said that he was 99% sure that we were looking at cancer. I was coming out of sedation so it didn’t hit me how it necessarily would if I wasn’t. Luckily, my wife was there.
Waiting and not knowing what was ahead, those few days after finding out were tough in many different ways.
Reaction to the Diagnosis
We went home in shock. We didn’t know what to say or what to do. We had a five-day wait to get the biopsy results back.
We both decided to keep working to keep things as normal as possible throughout the week. We tried not to sit around, thinking and waiting, because it wasn’t going to make anything easier.
That Friday, I got a call in the parking lot as I was leaving work and it was the general surgeon with the biopsy results. He confirmed that it was cancer, that he was sending all of my files immediately over to The Ottawa Hospital Cancer Centre, and that I’d be hearing from them at some point early the following week.
At that point, everything came crumbling down. I remember driving home and having to pull over on the side of the highway. My wife had to meet me because I couldn’t. I wasn’t there. When she pulled up, I was walking up and down the side of the road, in shock. I didn’t know what to think at that point.
We cried a bit. We drove home and were in shock for a few days. Waiting and not knowing what was ahead, those few days after finding out were tough in many different ways.


Breaking the News to Family and Friends
The toughest part was having to tell people because there’s very little cancer history in my family. I didn’t have any predispositions to anything that made sense.
Having to tell my family and friends was quite the thing. My wife played a huge role. She told a lot of people because I didn’t know what to say. I couldn’t have those conversations at that time.
The tumor was small and in a place they could reach very easily. They can take a few inches of my large intestines out and reconnect everything.
Treatment
Getting a Sigmoidoscopy
The initial procedure was a sigmoidoscopy. If I recall, it was 30 minutes between getting sedated and waking up again. There was no recovery, to be honest. I had a bit of a little discomfort in my rectum area, but beyond that, it was a quick, painless procedure.
I was very naive to the cancer world. You always hear of stages because of how cancer is portrayed in the media and on social media, I guess.
All my stuff got sent to The Ottawa Hospital. The following week after the biopsy confirmation, I heard from the colorectal surgeon’s office and they reviewed everything. Because the tumor was quite small, they decided to do surgery upfront.


Colon Resection
They weren’t sure if the lymph nodes they were seeing were involved. They couldn’t confirm that at that point. But what they did know was the tumor was small and in a place they could reach very easily. They can take a few inches of my large intestines out and reconnect everything.
Between the first week of December and about mid-January, I was doing pre-surgery workups, like blood work and pulmonary tests. They checked my heart and my lungs. I met with the anesthesiologist and the prep nurse. I had two MRIs because my stomach was not behaving and there were motion artifacts so they had to redo it.
Following that, I had a colonoscopy so they could go in, take a look, and mark the tumors because that’s how they locate them when they do the surgery laparoscopically. They also wanted to check the rest of my colon. Everything was clear. There were no other areas of concern.
I had my surgery on February 19th and it went smoothly. There were no issues. The surgery was about 3 1/2 hours. They were able to do it laparoscopically so it was minimally invasive, which was great. They ended up taking out about 6 or 7 inches of my large intestines and were able to reconnect the plumbing, as my surgeon called it.
I had a lot of support. My family was great. During that time, I found great social and emotional support groups that helped me during that time.
Recovering from Surgery
One of the things I was worried about was whether I was going to wake up with an ostomy bag. That was a big relief. I know it’s silly but out of everything, that was the big stressor for me. In retrospect, it’s probably the least that can go wrong.
Hospital stays are normally 4 to 7 days, depending on what happens. I was lucky I got out in three. The surgeons were happy. I went in strong and healthy. I was up and walking the next day.
The pain wasn’t too bad. I was off pain meds the next day. I was switched to Tylenol 3s. They sent me home with a bit of codeine. I used it once and beyond that was regular Tylenol.
I was in good shape. I worked out going into the surgery and prepped myself for it so that helped with the recovery as well.
In my mind, everything was great. The surgery was successful. Recovery was going well. There was the stress of all of this happening during COVID and being in the hospital was not fun.


After I got home, they called me because a nurse that I had tested positive. Luckily, I was negative, but it was a pretty stressful situation because I’d been home for a week already and my family was around me. Everything was great, but that was a stressful little situation after a pretty stressful situation of major surgery.
I was active during my recovery. Some days were more difficult and there was a little more pain. The first couple of weeks especially were frustrating. I’m active and independent. I work out, run, and lift weights, but for six weeks, I couldn’t even lift the laundry basket. I took handfuls of laundry in little scoops at a time. We went to buy groceries and I was able to carry in one item at a time.
That was quite challenging mentally. Going from being strong, healthy, and independent to suddenly being unable to do anything for yourself. That was tough, but I got through it.
I had a lot of support. My family was great. During that time, I found great social and emotional support groups that helped me during that time. Getting onto some Zoom calls, talking to other patients, and making those peer connections definitely made recovery a lot easier.
There were cancer cells in 7 out of the 25 lymph nodes that they removed so that took me from what they thought was stage 1 or 2 to stage 3B.
Getting the Pathology Results
We had to wait for the pathology results. They took out the tumor, but they also took out about 25 lymph nodes that had to get sent to pathology so there was about a four-week wait for all that to come back.
When we got the pathology results, unfortunately, it showed that there were cancer cells in 7 out of the 25 lymph nodes that they removed so that took me from what they thought was stage 1 or 2 to stage 3B, which was a pretty big jump. I was not expecting that.
In retrospect, my stage still had great odds and was a very manageable stage, but it was still a shock to hear. It was more of a shock because I knew that meant chemo. It made the difference between everything being over after surgery and having a whole other adventure in this situation.

FOLFOX Chemotherapy Regimen
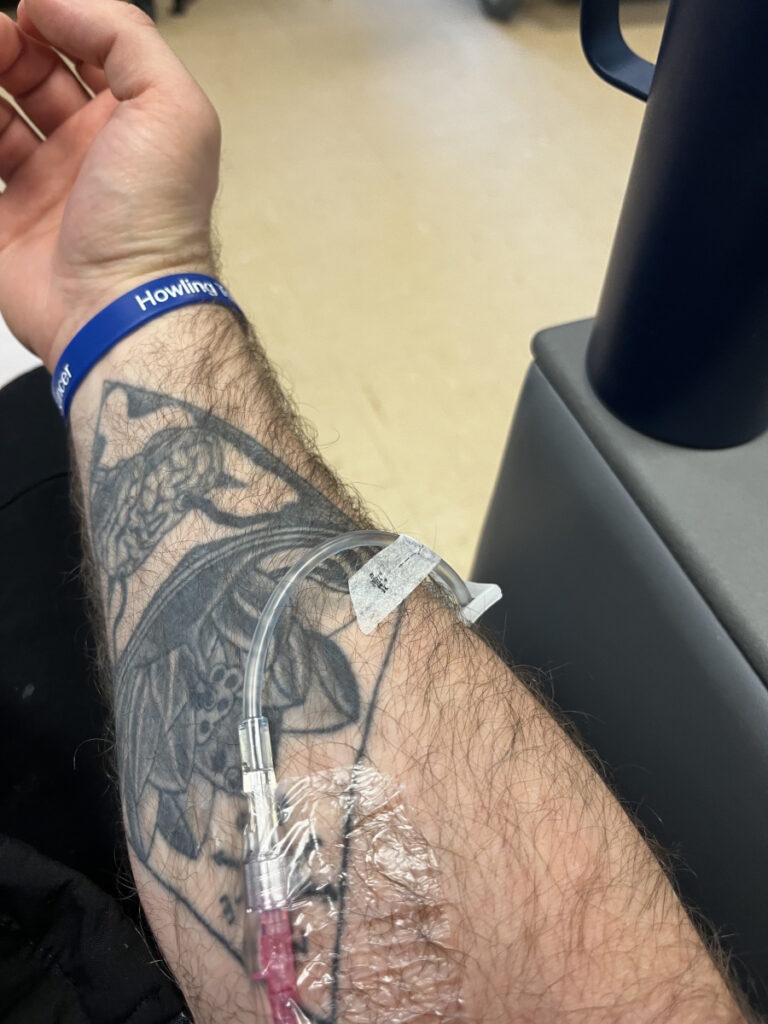
My diagnosis was stage 3B colon cancer. After recovery, I was lined up for six months of FOLFOX (folinic acid, fluorouracil, and oxaliplatin).
A couple of days before my first treatment, I went to the cancer center to do my chemo education. The first time I walked in, everything hit home. Up until that point, it was scary and traumatic. Hearing I had cancer was huge, but the surgery was like any other surgery. There was nothing different just because it was cancer surgery. The recovery was very smooth.
Walking into that cancer center and being a patient, not going there to visit someone or cut through to go to another part of the hospital, was quite the gut punch. That was a very big moment.
The beginning was a very interesting experience. The staff was amazing. They took great care of me. They took me on a tour. They educated me about my chemo and helped me choose if I wanted a PICC line or a port.
But one thing that stood out was every time I go to the cancer center, people look at me and wonder why I’m there. They don’t realize that I’m a patient. I’ve been asked several times, “Who are you picking up? Who are you visiting?” And when I say I’m here to get chemo, they give you the big deer-in-the-headlight look like it doesn’t make sense.
Waiting rooms are strange because I’m young and I look healthy and great. I would say 99% of the people are 50- to 60-plus. Most of them look pretty rough. The whole experience is very different. It’s really sad to say that I’ve gotten used to it. I put my blinders on, do my thing, and leave.
Those first couple of months were tough because they magnified and amplified the why me. Why am I the only 36-year-old sitting in this place? I treat myself well. I’m young and healthy beyond this, but I’m sitting in this room with all these people. That was quite a challenge as well.

The friends I made in Man Up to Cancer helped a lot because I was able to talk to them about that stuff. I quickly realized that it’s a widespread experience for a lot of people, especially younger adults. When you realize you’re not necessarily alone, it makes it a little bit easier to deal with.
Any colorectal cancer person is very familiar with the chemo regimen I did. I did six months of FOLFOX. I did 12 treatments.
I did a lot of things to help myself, which I do think made my experience with chemotherapy a little bit different.
Side Effects of FOLFOX
I tolerated it quite well. I was lucky in that regard. I worked while I was getting my treatments. I was quite active. They took great care of me.
I’m not going to sugarcoat it. There were days I felt like crap, but I also took control of a situation that I had very little control of. I did a lot of things to help myself, which I do think made my experience with chemotherapy a little bit different.
I got through the 12 cycles with no incidents. I did chemo from April until September 2021. My last session was on September 23rd. After that, I was NED (no evidence of disease) essentially. I was graduated to surveillance and that was supposed to be the end of it.


I know I did a lot, but I got very lucky. My body took to it very well, fortunately. The major side effect that I had was fatigue. I had quite a bit of fatigue.
My skin was not happy. I have sensitive skin as it is, but it did a number on my skin with rashes, dryness, and cracking. I had a pretty rough time with that at some points.
The neuropathy was not fun. Anyone who’s done FOLFOX knows that neuropathy from oxaliplatin can get pretty nasty, but I did a lot to counter it. It wasn’t too bad.
My oncologist and I have a great relationship… He’s very open to things as long as he has good data to make an educated decision.
Managing Neuropathy
To combat neuropathy, I worked with a naturopath. I took a lot of supplements. I did acupuncture, reflexology, and massage. I was doing all kinds of alternative stuff.
In my cancer center, I was one of the first people to do icing. I iced my hands and feet during every infusion of FOLFOX. I know in the States, in some of the larger cancer centers, it’s been a bit more common in the last few years, but in my cancer center, at that point, no one ever did that before. Everybody was dumbfounded by that because why would you ice your hands and feet with a chemotherapy agent that has extreme cold sensitivity?
I was fortunate to be hooked up with COLONTOWN. I was able to present my oncologist with studies, actual data, and factual information as to why it’s used.
My oncologist and I have a great relationship. We have a lot of respect for each other. He’s very open to things as long as he has good data to make an educated decision. I was the first person to do icing at my cancer center on FOLFOX and now he recommends that to a lot of his patients. He gives that as an option to anybody moving forward with that regimen so that’s cool.


I don’t know the detailed science behind it, but essentially what it’s supposed to do is help with the cold sensitivity because it restricts blood flow to your extremities. It shrinks your veins and arteries down so you don’t get as much blood flow in that area. I guess the theory is not as much chemo gets to your hands and feet so it lessens the cold sensitivity effects.
I’d put my hands in the freezer, pick up frozen food, and be okay. Patients who didn’t do that couldn’t even touch a cold cup. You’d get shocks and it would be extremely painful. I would take all these videos to show to my oncologist and he loved them because it’s not something that he was familiar with at that point.
There’s so much stuff out there and it’s not his fault. It seems a lot of stuff from the States comes to Canada 3 to 5 years later. It hasn’t gotten here yet, but it’s becoming more common. I’m happy that I got to try it and it benefited me so it’s going to benefit a lot of other people that come after me, too, which is cool.
Celebrating the End of Treatment
After I had my last chemo on September 23rd, I rang the bell. I had a nice big celebration. I hugged all the nurses there.
After six months of going in by myself, my wife was allowed to come in for my last treatment, which was cool because she’d never seen the cancer center because of the restrictions. She didn’t know what happened to me for three hours when she dropped me off at the front door. It was really neat for her to see what the process was and what I’d been doing for six months.
The plan was a couple of months after, I was going to get a follow-up scan to get a post-chemo baseline. That scan came back clean. At that point, I was under surveillance. I was declared NED and it stayed that way for about 16 months.

I realized how tired and burnt out I was… I didn’t process anything that happened to me that year and a half until chemo was over.

Taking Time Off Work
After that scan, I took time off work to recover because I’d been working through everything. Once that scan came back clear, it was like the weight of the world was lifted.
I realized how tired and burnt out I was from the year and a half of appointments, treatments, procedures, and operations so I decided to take a couple of months off work.
During that time, we adopted a little girl. She was one. That was something we put on hold when I got this diagnosis. We were in the process of becoming adoptive parents when we found out so we had to put that on pause.
Two weeks after my last treatment, we got a call that we were matched with this one-year-old adorable little girl. Two weeks after that, she was living with us. I went from a year and a half of being a patient to a dad in two weeks. There was no time to process anything.
It was this amazing, life-changing thing after a year and a half of this difficult, life-changing thing. It was exactly what my wife and I, and our family needed to have something great happen and get back to living.
Taking Time to Process Everything
It was a new normal. The next six months were hard. It was tough emotionally because I was finally able to stop. I wasn’t in survival mode anymore. I knew I was okay. All my systems started to slow down. Then you realize what you’ve been through. I didn’t process anything that happened to me that year and a half until chemo was over.
Everything surfaced and hit me like a freight train. I spent a lot of time working with a social worker and my psychologist. I did a lot of peer groups within the cancer support community to work through everything and figure out what my new normal is and who I am now.


Everything changed. I was a first responder before and I was always a big risk taker and helper. After this, I realized, all my priorities had changed. Your outlook on everything is different.
I had to give myself time to heal both physically and mentally but also to figure out who I was, what I was going to do, what I wanted my life to look like now, and what was the healthiest thing for me moving forward. Working through all of that and trying to navigate some of the chemo side effects took a good chunk of the next year.
I was getting scans every three months for the first year. Then I moved up to every six months. I had one six-month scan that was clean.
How could a reoccurrence happen when you’re feeling great?
Finding a Lung Nodule
In September 2023, on one of my surveillance scans, a lung nodule popped up. We went back and saw that it was on a scan a year ago. It was tiny and a lot of the time, stuff in the lung isn’t noted until it changes because a lot of us have stuff on our lungs that are absolutely nothing. It changed gradually over the past year.
It was a bit of a shock. I’ve been completely asymptomatic. I’ve been feeling pretty good. I think I’m in better shape and feeling better than I was before my diagnosis, which is awesome but also a little confusing. How could a reoccurrence happen when you’re feeling great?
I didn’t feel any different. I was feeling great. If it wasn’t for that scan, I wouldn’t have a clue anything was there. That thrust me back into patient mode quickly, which was challenging because I’ve spent the last almost two years trying to figure out how not to be a patient anymore and I was in a really good spot.

Discussing Treatment Options
Luckily, I had a lot of options. I had a whole bunch of tests done. It was an isolated incident and there was no spread anywhere else. Everything else is still great.
After meeting with a thoracic surgeon, the first go-to will be surgery to take it out. I did a PET scan, which came back great. I had a brain MRI, which was clear. I did a CT scan, a cardiopulmonary test, EKG, and all the pre-surgery stuff.
Because of the location, even though it was a small 18 mm tumor, they were going to have to remove my whole lower lobe because it was quite central. They couldn’t do a wedge resection. They would have had to take too much out so it was safer to take the whole lobe.
From the time that lung nodule popped up on the scan, within a week, I had four procedures booked and done. I had a consult with a surgeon the following week.
Seeking a Second Opinion
Because of my age, my health, and because there was a low disease burden, I asked for a second opinion. I knew that there had to be a less invasive but as effective approach. I thought I was being pretty logical.
I talked to a couple of great people who are quite educated in the advocacy world and they guided me in the right direction about how to do that, what to do, and who to contact.
I ended up getting a second opinion from a highly regarded surgeon in Toronto out of Sunnybrook and he ended up being my thoracic surgeon’s mentor when he was in med school. Small world.
I pushed. If I need something, my doctors make it happen because if not, their phones are going to be ringing and I’m going to annoy everybody.

From the time that lung nodule popped up on the scan, within a week, I had four procedures booked and done. I had a consult with a surgeon the following week.
My oncologist is great. He goes to bat for me, which helped as well, but I was on the phone daily, calling the offices. “Do you have my file? Has it arrived yet? When’s my appointment? Book me in.”
My oncologist called me that week, saying, “Who are you calling? I’ve been getting messages about you all day and I don’t understand where these are coming from.” We had a good little chuckle.
What that ended up doing was getting my second opinion quickly and getting it moved to the tumor board the very next day.
Stereotactic Body Radiation Therapy
We ended up deciding to do SBRT as opposed to surgery. I had three 15-minute sessions in that area, which was done in November.
It’s a very specialized and precise radiation. As opposed to traditional radiation, which targets an area of the body and a whole bunch of tissue gets affected, they map out almost to the millimeter. The radiation impacts only the tumor and very minimal surrounding tissue around it.


Side Effects of SBRT
I had very little side effects. I had a little bit of fatigue immediately after each session, a little bit lethargic, but that’s it.
It’s quite amazing that 45 minutes of treatment could replace losing a whole lobe of your lung. They’re as effective but on opposite ends of the spectrum with invasiveness so I’m fortunate for that second opinion.
My surgical oncologist would have come to that anyway, but that second opinion sped the whole thing up.
My situation is very good. I know I’m fortunate. I’m right on the brink of being NED again and staying there for a long time.
Follow-up Protocol
Technically speaking, if the SBRT did what it was supposed to do, I am back at NED. There was another tiny nodule that popped up that they were watching, but it did not light up on my PET scan so they’re not sold that it’s anything at all.
They’re going to keep a close eye on it in the next set of scans to see if anything changes. If it does, my radiation oncologist has already told me that he will treat it with SBRT right away. If it does turn into something at some point, I have a plan. I’m good. I know that SBRT is highly effective and minimally invasive so I’m happy about that.


My next scans are in January 2024. Those are going to be big ones. Everybody gave me the holidays off. They said, “SBRT takes some time to work so let’s push the scans back a couple of weeks. Enjoy the holidays with your family. You don’t need test results hanging over your head. We’re going to scan in the second week of January and ensure that the SBRT did what it was supposed to do.”
Knock on wood, it’s shrunk, it’s dead, it’s stable, whatever they need to see. If it did grow at all, I do have the option of doing another round of SBRT on it.
My situation is very good. I know I’m fortunate. I’m right on the brink of being NED again and staying there for a long time, if not forever this time. I’m a little bit nervous about that appointment because I don’t know if my oncologist is going to suggest clean-up chemo to be sure.
My situation is fairly unique because it was one isolated met. We didn’t do a biopsy on it because I felt that the risks of that lung biopsy were not necessarily worth it, especially given that it lit up on the PET scan. The fact that it lit up on the PET scan was enough for me. I didn’t feel that the potential side effects and risk factors were worth it. My oncologist and my team agreed.


Technically speaking, they don’t know 100% if it’s a CRC met or if it was potentially a second primary cancer in the lung. My staging is not necessarily changing. They’re not rushing to jump on anything. It’s essentially a stage 3B with an unconfirmed met in the lung essentially. I’m in a weird gray zone, I guess you could say.
The way I see it is I can still be NED from my stage 3 colon cancer and have a stage 1 lung something and they blast it out with SBRT. Both of those have extremely high cure rates and success rates. The worst case is that it was a met. It was isolated, the rest of me is clear, they blasted that away.
Do your research. Talk to organizations. There are great organizations out there. Get a network built around you.
Words of Advice
Our systems are very different in the US and Canada. Second opinions and all that work very differently, but at the core of it, advocacy is advocacy.
The biggest lesson I’ve learned is you have to trust your doctors. They’re the pros. But you also have the right to question them in a polite, professional, appropriate way.
You’re allowed to ask questions. You’re allowed to ask them why they’re making the decisions they’re making and why not. You’re allowed to give them ideas.


Do your research. Talk to organizations. There are great organizations out there. Get a network built around you.
Don’t hesitate and don’t be scared to say you don’t understand something, don’t agree with something, you got an idea from somebody, or you heard of a study, new treatment, or what have you. Don’t think that bringing that to your team is going to hurt their feelings or insult anybody.
At the end of the day, it’s your body and it’s your outcome. Doctors are amazing, absolutely. I love my team. There’s a very mixed bag of oncologists and doctors. People have very different experiences. But at the end of the day, they are not the be-all and end-all.
They help you and quarterback you, but their word is not the final say and it’s not always the right one. I’ve learned that when you bring things to their attention, when you learn how to work with them and be part of your care, they take your opinions and some of your ideas and make things happen.
Be part of your care. When there are meetings and decisions to be made, be part of that. Be actively engaged and make your voice heard.
If they know you’re going to cause a ruckus, speak up, and stir up the pot essentially to get things done, they will work that much harder for you because they know you’re invested and that you’re not going to wait. If they lag or say no, you’re going to find a way. Don’t take no for an answer. Don’t be scared to question and ask why.


We cannot do this alone. Supporters and caregivers are often not talked about enough. They get as affected as we do. Maybe not in the same ways, but they experience this with us. When one of us has cancer, the whole family does. Don’t forget about those people. Everybody’s trying to help. Surround yourself with good.
There are a lot of amazing organizations out there. I used Young Adult Cancer Canada, Colorectal Cancer Canada, Man Up to Cancer, and CCRAN.
Surround yourself, educate yourself, and be knowledgeable. Don’t put your head in the sand and isolate because that’s not going to go well. Find your people and latch on to what helps. That community will help you get through this.
Be part of your care… Be actively engaged and make your voice heard.

Inspired by Jason's story?
Share your story, too!
More Colon Cancer Stories
Kristie C., Colon Cancer, Stage 4 (Metastatic)
Symptoms: None per se that she noticed; she experienced constipation and passed narrow stool, but had been experiencing constipation most of her life, and thought that these digestive issues could also have resulted from perimenopause
Treatments: Chemotherapy (including adjuvant chemotherapy), radiation therapy, ablation therapy (liver ablation), surgeries (colectomy, temporary ileostomy, ileostomy reversal, scheduled liver resection)
Briana H., Colorectal Cancer, Stage 3
Symptoms: Periods of constipation initially lasting one week and then extending to two weeks, nausea, pain in lower left abdomen, lack of appetite, vomiting and inability to keep fluids down
Treatments: Surgeries (colon resection, tumor removal, colostomy placement, colostomy reversal), chemotherapy
Kailee O., Colorectal Cancer, Stage 4 (Metastatic)
Symptoms: Sensitive stomach sometimes leading to vomiting after eating, bleeding during bowel movements, persistent fatigue, back pain, abdominal pain, anemia, significant symptom flare-up during second pregnancy
Treatments: Surgery (colectomy), chemotherapy, targeted therapy
Starr S., Colon Cancer, Stage 4 (Metastatic)
Symptom: Abdominal pain
Treatments: Chemotherapy, surgeries (colectomy, hepatectomy, lymphadenectomy), targeted therapy
Jackson L., BRAF Mutation Colon Cancer, Stage 4
Symptoms: Severe stomach pain, fatigue, lack of motivation, anemia, blood in stool, thinning stool
Treatments: Surgeries (emergency bowel obstruction surgery with temporary colostomy, possibility of HIPEC in 2026), chemotherapy, immunotherapy
Heather C., Colon Cancer, Stage 4 (Metastatic)
Symptoms: Severe bloating, indigestion, vomiting, rectal bleeding
Treatments: Chemotherapy, surgery (liver transplant, upcoming)