Gwendolyn Jackson’s Metastatic Cervical Cancer Story
Interviewed by: Alexis Moberger
Edited by: Katrina Villareal

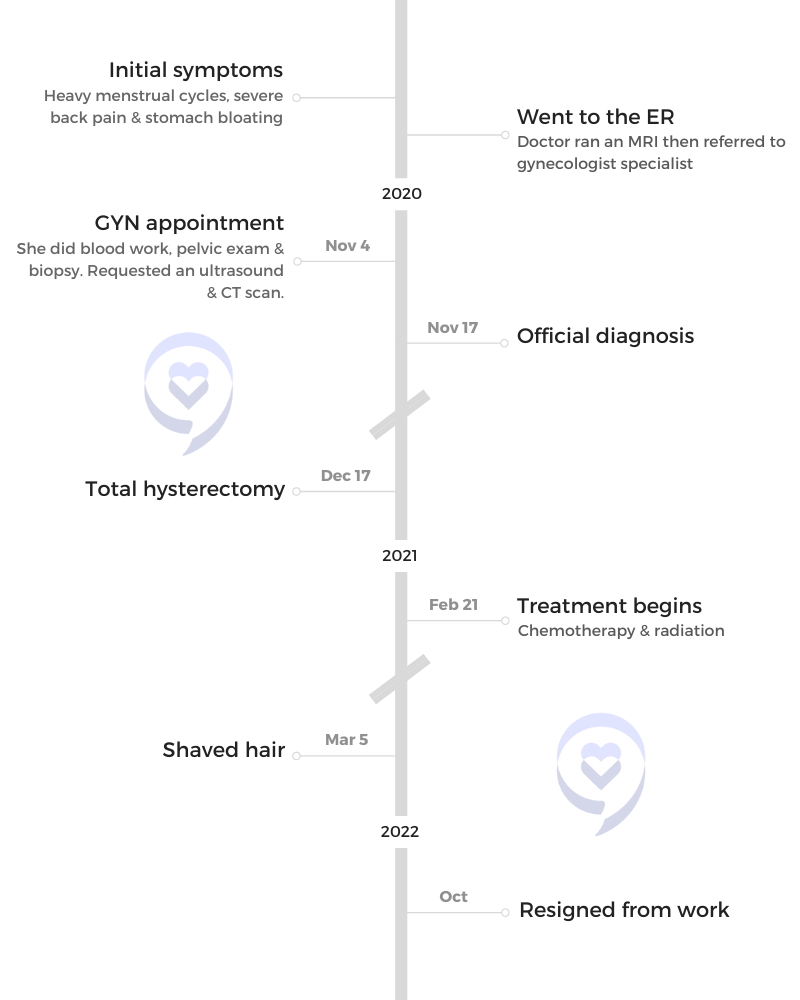
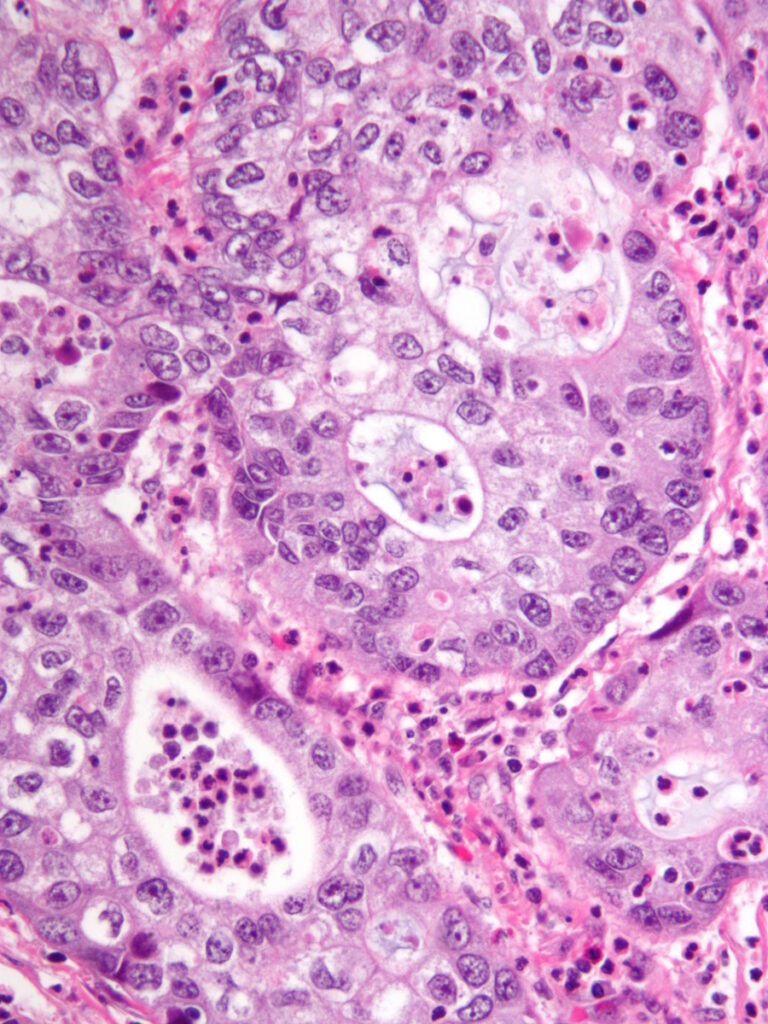
Gwendolyn Jackson initially experienced heavy menstrual cycles, back pain, and bloating, which her doctor suspected to be fibroids. Despite regular tests, including an HPV test and ultrasound, her symptoms persisted. Later, clear fluid leakage led to an ER visit where an MRI and biopsy confirmed cervical cancer.
She underwent a hysterectomy, followed by chemotherapy and radiation, but further tests revealed the cancer had spread, drastically changing her prognosis. Severe side effects from treatment, including weakness, nausea, multiple strokes, and heart attacks due to dehydration, required intensive therapy. Despite initial hesitation, she joined a clinical trial at MD Anderson, which has helped manage her condition more effectively than traditional chemotherapy.
Throughout her journey, Gwendolyn faced misconceptions about clinical trials and the stigma of cervical cancer within the African-American community. Financial challenges resulted in losing her job, insurance, and assets. She found crucial support through Cervivor, an online community for women with cervical cancer.
Gwendolyn’s experience highlights the importance of self-advocacy in healthcare, the life-saving potential of clinical trials, and the need for greater awareness and support for cancer patients.
- Name: Gwendolyn J.
- Diagnosis:
- Cervical Cancer
- Staging:
- Stage 4
- Initial Symptoms:
- Heavy menstrual cycles
- Severe back pain
- Stomach bloating
- Treatments:
- Chemotherapy
- Radiation
- Tisotumab vedotin (innovaTV 301 clinical trial)
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
I knew I wasn’t pregnant, but it felt like my water bag had burst. I said, ‘Okay, this is not good.’
Introduction
I’m from Houston, Texas. I used to be a case manager who helped house homeless individuals, which I loved to do so dearly.
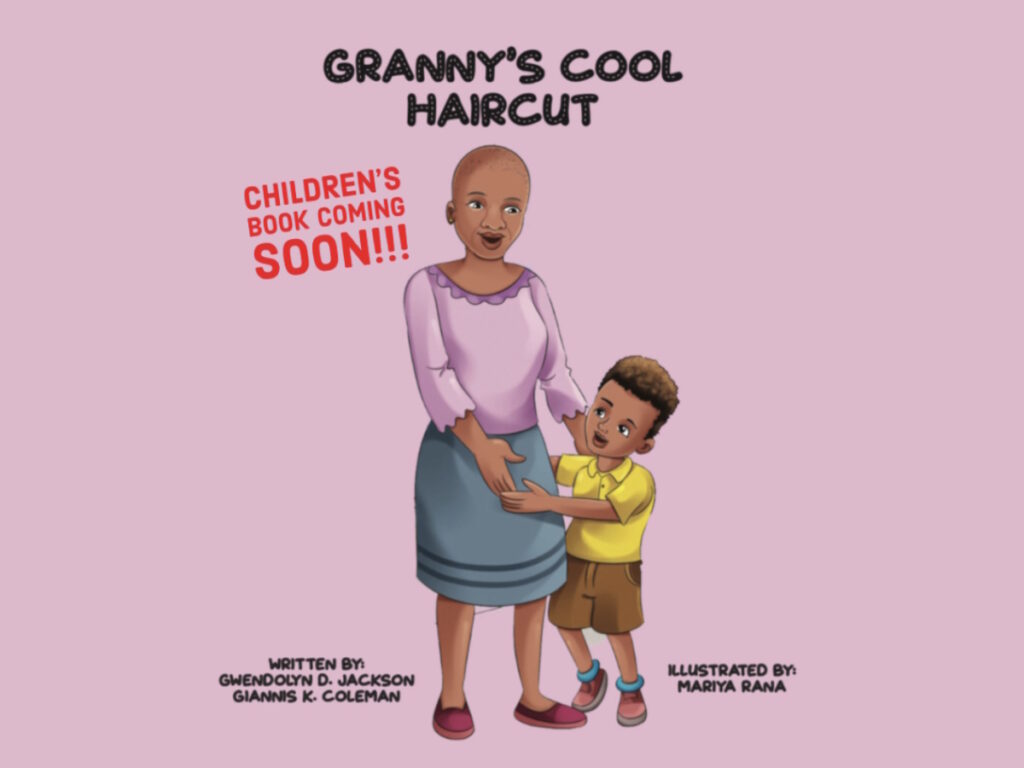
I’m a mother of two. I have a 31-year-old daughter and a 28-year-old son. I’m a grandmother of two granddaughters and one grandson.
I’m the founder and CEO of a non-profit organization called the Roy L. Jackson Community Outreach Center. I’m also part of an organization called Cervivor.
Pre-diagnosis
Initial Symptoms
I started having heavy cycles, severe back pain, and bloating in the stomach.
I went to the doctor regularly. When I went for my well-woman exam, I told my doctor. He said, “I think you have fibroids. It’s very common in the African-American community.” That’s what it sounded like to me. “We’ll run some more tests.”
My symptoms persisted, so I went to my mother because I’m that girl who thinks mom can fix everything. I told her, “I’m having very heavy cycles. I don’t know what’s going on. The doctor said he was going to run some tests. They haven’t called me back yet.” She said, “You’re going through pre-menopause. I went through the same thing at the same age. It’s just pre-menopause.”
My cycle wasn’t getting any better. I finally went back to my doctor and he ran some tests. He did the HPV test and it came back negative. I was still having symptoms, so he said, “I’m going to do an ultrasound.” He did and said, “I see fibroids, so we might have to do a hysterectomy.”
In October 2020, while I was at work, I started leaking clear fluid from my vagina. I knew I wasn’t pregnant, but it felt like my water bag had burst. I said, “Okay, this is not good.”
When I saw cervical cancer written on that paper, I lost it. He wrote it down before they even found out I had it.
Going to the ER
I wish I could remember the name of the doctor who saved my life. I don’t know what would’ve happened if it wasn’t for him and that MRI.
When I went to the emergency room, a younger doctor who looked like he had just become a doctor said, “I want to run some more tests on you. I don’t feel comfortable with everything you told me. What can we lose? Let’s do an MRI.”
After the MRI, he came back and said, “I see fibroids, but I see something under the fibroid, so I’m going to send you to a gynecologist specialist, so they can run more tests because I’m not sure,” but he put “cervical cancer” on my paperwork.
I went home and did the worst thing I could do. I went online and searched “cervical cancer.” My father passed away from cancer, so when I saw cervical cancer written on that paper, I lost it. He wrote it down before they even found out I had it.
Diagnosis
Seeing a Specialist
I went to the specialist who said, “We have to run a biopsy. Calm down. Don’t worry. You’re pretty healthy. I see all the tests they’ve done. I don’t think you have cervical cancer. It might just be fibroids.”
Getting the Official Diagnosis
I was diagnosed during the COVID pandemic, so I had to go by myself. On the way, I talked to my mother and my sisters. Everybody said it was just fibroids. My sister said, “We have fibroids. We had to have a hysterectomy too.” They were reassuring me, so that’s what I thought.
I went in thinking I had fibroids and left finding out I had cancer. You will never forget the day. I was diagnosed on November 17, 2020.
I started treatment right after I recovered from the hysterectomy. I thought it was just a preventative measure to make sure I was okay.
Reaction to the Diagnosis
When you first hear, “You have cancer,” it doesn’t register. For some reason, I thought I was exempt because I was helping people with cancer. I started my nonprofit in memory of my father who died from lung cancer. I thought, I eat right. I run five miles every morning. I don’t smoke. I don’t drink. What did I miss?
Cervical cancer has this stigma that people who get it are either prostitutes, have a high sexual drive, or don’t go for their well-woman exam. That’s not me. On the way home, I thought it was something I did wrong.
I wanted to find out for sure first. The doctor put it on the chart and then gave me paperwork for the referral. I was left alone not knowing if this really was true. That two-week wait was difficult mentally.


Treatment
Hysterectomy
They said, “We’re going to go in and remove the whole tumor. After, you’ll do radiation and that’s it. Your life will be back to the way it was,” so that’s what I thought.
I had a full hysterectomy on December 17, 2020. The tumor was 9 centimeters. Before I went in, they were telling me, “You’ll be fine. After we remove the tumor, radiation will take care of everything else.”
After 6 to 8 weeks, I went for radiation. My doctor did some blood work and he was concerned with the results. He said, “The blood work didn’t change. Something isn’t right. I’m going to do an MRI and a PET scan. We have to see what’s going on.”
After I had the hysterectomy, they said, “We’re going to do radiation and you’ll take a chemo pill. That’s just protocol.” I started treatment right after I recovered from the hysterectomy. I thought it was just a preventative measure to make sure I was okay. They were thinking they got everything not knowing that it was spreading.
The chemo was so hard on me. Some days, you can’t get out of bed. Some days, you don’t have an appetite.
Cancer Spread
They found out that my cancer had spread to my hip bone, my legs, and my spine. Imagine going from everything is going to be okay to find out you have 16 months to live.
I said, “God, I don’t want to die. I just had grandchildren. I just turned 49. I haven’t hit 50 yet. I’ve been waiting to be 50 all my life. Please give me more time.”
When they realized it spread, my team had to come back together and treat me differently. They were going to try a bone marrow transplant, but they couldn’t do it because of how mine spread. My insurance would no longer approve it.
Knowing that was all they could do, I got scared. I have anxiety and depression, and I take medication for them now. I’ve never had depression before, but because of all of this, I take medication for it.
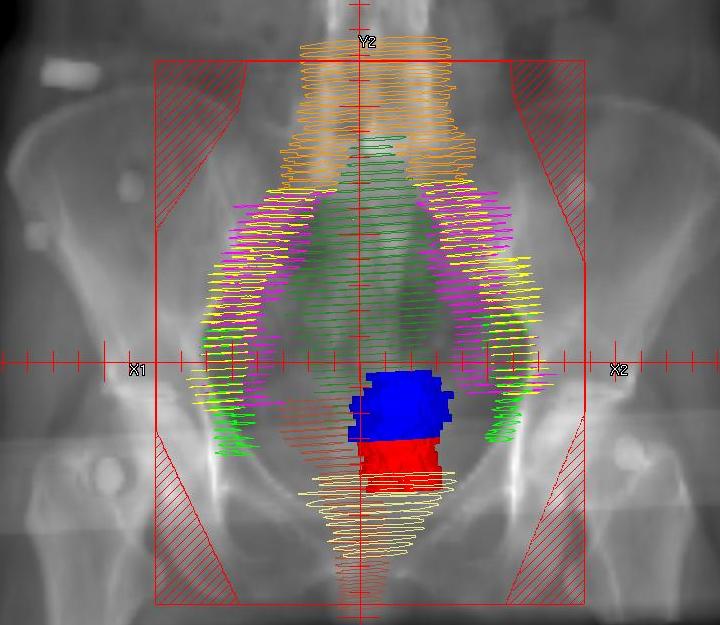
Chemotherapy & Radiation
I didn’t want a port. I asked, “Can we figure out something? Is there a way that I can take pills?” I took chemo pills and did radiation.
Side Effects of Chemotherapy & Radiation
The chemo was so hard on me. Some days, you can’t get out of bed. Some days, you don’t have an appetite. You don’t want to eat. You look at food and get nauseous. People don’t understand that. It’s not that we don’t want to. I’m trying. I’m showing up every day and doing the best I can. I used to tell my dad, “Come on, you can eat. Come on, you can get out of bed.” Now, I understand.
The radiation that targeted my cervical cancer was terrible. It burned the lining of my stomach and I kept getting infections.
I used to help my dad button and zip his clothes. I have the same issues now. I can’t button or zip. These are everyday things that we take for granted. I also felt numbness in my fingers and my feet.
I couldn’t keep anything in my stomach. I was vomiting and had diarrhea. They were giving me medication for everything, but nothing was working.
I feel so weak and cold all the time. I always have a heater with me, but I was so, so weak that I didn’t think I was going to make it. My daughter and the guy I was dating at the time were very helpful. They would bathe me and help me get up.
Because I lost so much weight and wasn’t strong, even my doctor was saying, “You’re getting weaker and weaker.” He kept prescribing me medication for nausea. They finally found a prescription that worked for me and that I love.
Radiation burned my face. It was burning and itching at the same time. My face swelled up and blistered. My doctor told me about a cream I could use, which cleared up my face.
The radiation that targeted my cervical cancer was terrible. It burned the lining of my stomach and I kept getting infections. I never want to do that again ever.

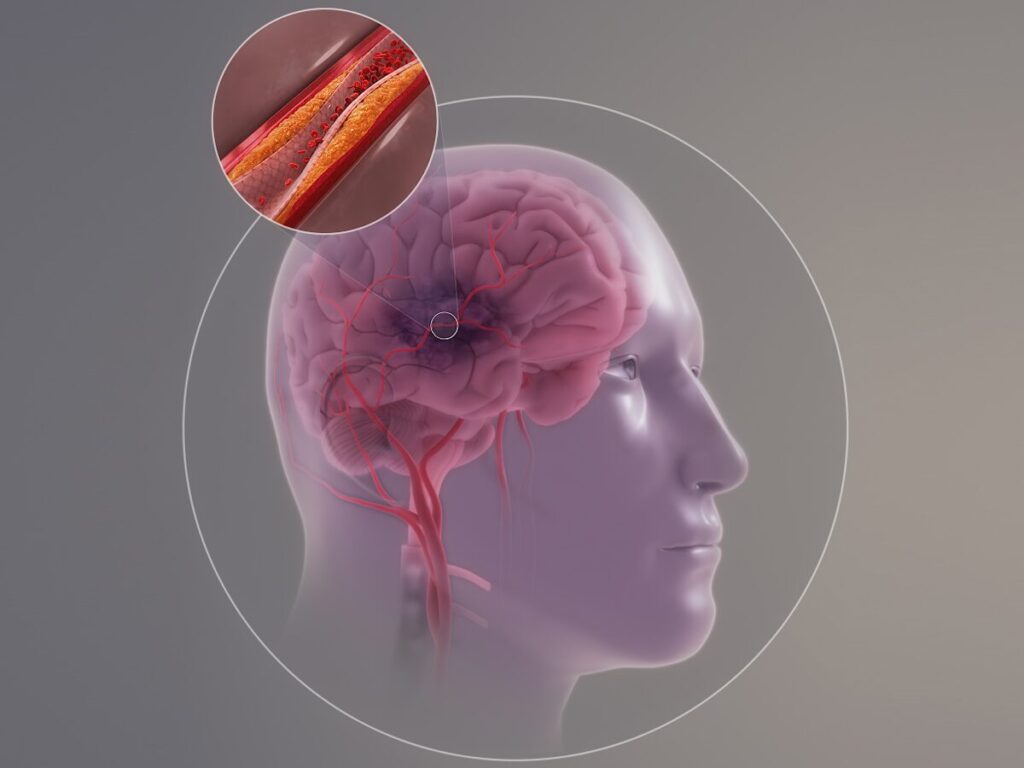
Strokes & Heart Attacks
When I went to the hospital, the ER doctor said, “She has high blood pressure.” I said, “No, I don’t have high blood pressure.” When he checked, my blood pressure was very low. When they ran tests, he said, “You’re having a stroke and a heart attack, and it’s because you are severely dehydrated. You need fluids in the body to make all the organs work.” I didn’t even know you could have a stroke or a heart attack from being severely dehydrated.
I had to stop treatment temporarily because I was in inpatient therapy for 14 days.
Recovering from the Strokes & Heart Attacks
I couldn’t walk, so I was in a wheelchair. I had to stop treatment temporarily because I was in inpatient therapy for 14 days and then I went to the Centre for Neuro Skills in Webster, Texas. I always speak so highly of them because they gave me my life back.
When I came in, I felt so helpless. I wouldn’t use the restroom, even though I was there from 9 to 2 o’clock. I didn’t want anyone to take me. I ended up getting a UTI and people there had to tell me, “We’re here to help. We want to make you better. You have to allow us to help you. You’re still the same person.”
I had three mild strokes. They didn’t understand the last one I had. They said, “Usually when you have a transient ischemic attack, you bounce right back.” I didn’t, so he said the last one wasn’t a TIA. It was a regular stroke because I had all the symptoms. I had to go from a wheelchair to a walker to a cane.
Because of the strokes, I can’t remember exactly what chemo I was on.


Joining a Clinical Trial
I met a doctor at one of Cervivor’s retreats. She was different if that makes sense. I knew that she cared about people. She said, “When you get back to Houston, let’s stay in touch,” because she worked at MD Anderson. I said, “My treatments are not at MD Anderson.” She said, “Let’s just stay in touch.”
My doctor never brought up clinical trials. I was doing some research. I kept hearing other patients talk about clinical trials when I went to the doctor. I decided I was going to ask my doctor, but I want to have information before I go in. I wanted to educate myself.
My doctor said, ‘This is great, but these clinical trials are at MD Anderson. If you can get in, go there. I’ll send your medical records over.’
I reached out to the doctor at MD Anderson and asked about clinical trials. She gave me all the information, told me which ones she recommended, and sent an email right away. It was after hours and she was volunteering her hours to help me. She’s still a big supporter of mine. She still checks on me and asks how I’m doing.
I took the information to my doctor and my doctor said, “This is great, but these clinical trials are at MD Anderson. If you can get in, go there. I’ll send your medical records over.”
My dad enrolled in clinical trials at the end and I said, “Y’all not helping him. This is not helping him.” My dad was such a great guy. He said, “This is how they’ll find out if it works for someone else. If it doesn’t work for me, they know it doesn’t work. If I can help someone, that’s what I want to do. I want to help someone.”

I didn’t understand at that time because I wasn’t a patient. But when you become a patient, you feel that way. If it doesn’t work for me, we know we have to try something else. If it works for me, that means this could be it. If I have to go through all of this to make sure it can save me and someone else, it’s so worth it.
When I went to MD Anderson, they had to do all the scans themselves. Their team comes in and speaks with you, and they have a team for everything. Even though I had cervical cancer, they also had a bone cancer specialist.
They redid all the tests I already had to make sure what they had in the file matched. Once they did everything over and made sure I was good to go, they started talking about treatment.
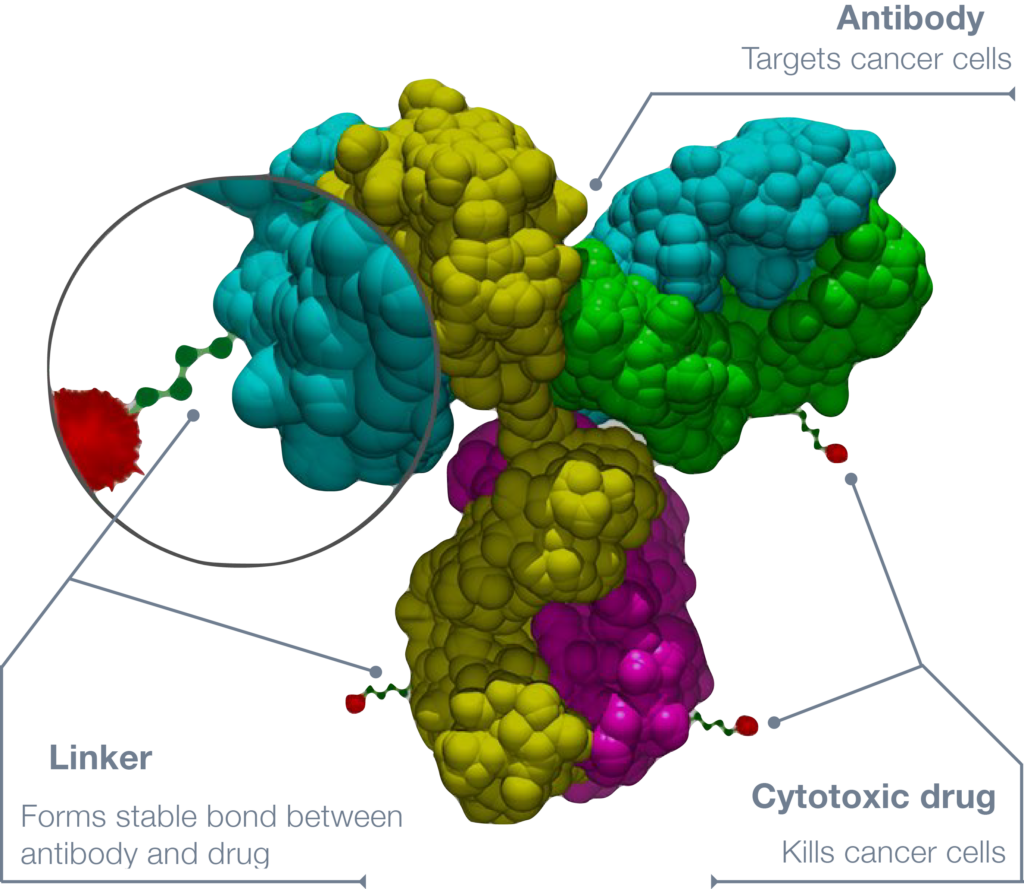
The clinical trial I’m on is called innovaTV 301. It’s a phase 3 study of tisotumab vedotin.
I like tisotumab vedotin better than traditional chemotherapy. It’s not so hard on my body.
Side Effects of Tisotumab Vedotin
They gave me medication for nausea and vitamin B12. So far, so good. The steroids are putting weight on me. I was a little nauseous at first, but the pill helped with that.
I lost my hair. I went bald when I first started and then it started growing back.
With bone cancer, being cold is a no-no for me. It’s very painful, so I wear a lot of warm-ups or layers to try and stay warm. Even in the summer, when I feel cold, I’ll be in warm-ups. I tell people all the time to be nice to people in warm-ups because you never know why they’re wearing them even when it’s warm out.
I noticed my appetite was not the same. I’ll crave something because of the steroids, but when I get it in front of me, I might take one or two bites and then I don’t want it anymore.
I like tisotumab vedotin better than traditional chemotherapy. It’s not so hard on my body. Do we know if it’s working? I don’t know if they think it’ll work. They’re buying me more time, so if that’s what it can do, I’m okay with that.

In the African-American community, clinical trials are frowned upon…In our mind, we still think we are being experimented on.

Misconceptions
In the African-American community, clinical trials are frowned upon. I think it goes back to when they were using African Americans for experiments and being the guinea pigs. In our mind, we still think we are being experimented on. If you tell anybody you’re doing clinical trials, they think you’re being a guinea pig.
I didn’t have the support. Everybody supports you when you’re going through chemo, but when it comes to clinical trials, they think you’re letting them experiment on you. They don’t care. I have to keep it to myself. I’ll tell people who are battling cancer that I’m in clinical trials, but other people, I don’t.
When it comes to the medical team, sometimes we feel like we’re not being heard. At first, I felt like my doctor wasn’t hearing me when I said it wasn’t fibroids and that something was going on, but they kept brushing me off.
I thought it was just Black women who go through that. Being in the teal and white community and the Cervivor community, I found out that it’s women as a whole. They are not listening to us.
Insurance Coverage
People think that if you want to be a patient at MD Anderson, you can just show up. It doesn’t work like that. When I first found out I had cancer, I wanted to go to MD Anderson because they’re number one. My insurance wasn’t in their network so they couldn’t take me.
While I was going through all of this, I still had insurance because I was still employed. They took excellent care of me during that time, but they could only take me so far. I was getting temporary disability, but my doctor put “permanently disabled” on my paperwork, so I had to resign from my job. They knew I wasn’t coming back, so they said, “You’re going to have to figure out your insurance yourself.”
Even with insurance, I was paying $2,000 to $3,000 for treatment. I lost everything. I lost my cars and my townhouse. The clinical trial was free for me, so that was good. They just had to make sure everything lined up.

I needed people who understood what I was going through, the stigma that comes with it, and that we have a voice. We didn’t do anything wrong.

Finding Support Online
I felt like nobody understood what I was feeling or going through. My mother kept saying, “It’s going to be okay,” but I told her, “What if it’s not? What if I die? What if this is my story?” But, of course, she didn’t want to hear that. “No, you’re going to be okay.”
My sisters were supportive, but nobody knew what I was going through. The only person that I felt I could talk to was deceased. My father would be the only one that would know what I was going through.
I went online and found Cervivor. I needed them more than they probably knew. I needed people who understood what I was going through, the stigma that comes with it, and that we have a voice. We didn’t do anything wrong.
I went to a retreat because I needed to be around these women. I needed them to love on me and I needed to love on them. They gave me hope. They said, “You can do this. You can fight this. Don’t give up. We support you.” They have a group chat where they talk about whatever they’re going through. If somebody doesn’t respond, they all get nervous.
Words of Advice
Cancer taught me to slow down because I was always on the go. I never slowed down to notice anything. Now I would stop and notice things. “Did you know mom has roses in front of her house?” And then I would stop and smell them.
Everything matters to me now because I don’t know how long I have. When I had my stroke, I couldn’t walk and we take that for granted. Even going to the restroom, I needed someone to help me and I appreciate that so much now.
Clinical trials can save us. I’m doing pretty well. It’s working for me. I’m still alive because of the clinical trial. My brother, who has cancer, is on a clinical trial and doing well too.
A doctor told me, “When you go into the doctor’s office, they are working for you. You are not working for them.” When you have that in mind as you’re going in, it’s different.
If you feel like something is not right, speak up. If there’s a treatment that you don’t want to do, say it. We get so nervous when we go in that we freeze up. Use your voice.

Cancer taught me to slow down because I was always on the go… Everything matters to me now.
In addition to Gwendolyn’s narrative, The Patient Story offers a diverse collection of cervical cancer stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.

Inspired by Gwendolyn's story?
Share your story, too!
More Cervical Cancer Stories
Willow B., Pelvic Cancer, Grade 1, Stage 2.5
Symptoms: Persistent fever-like chills, scratchy throat, fatigue, post-orgasm pain, heavy bleeding, severe cramping
Treatments: Surgery (radical hysterectomy), radiation, chemotherapy, hormone replacement therapy (HRT)
...
Samantha R., Adenocarcinoma Cervical Cancer, Early Stage
Symptoms: Irregular bleeding, pain
Treatments: Surgery (radical hysterectomy, pelvic exenteration), chemotherapy, immunotherapy, radiation therapy, hormone replacement therapy, hyperbaric oxygen therapy
...
Amanda L., Cervical Cancer, Stage 3
Symptoms: Heavy periods, abnormal bleeding, large blood clots, severe cramping, severe abdominal pain, pain radiating down the left leg, loss of mobility in the left leg, loss of appetite, fatigue
Treatments: Chemotherapy, radiation therapy (external beam radiation therapy & brachytherapy)
...
Mila L., Squamous Cell Cervical Cancer, Stage 1B1
Symptoms: Abnormal lump in cervix area, bleeding after sex
Treatments: Chemotherapy (cisplatin), radiation, adjuvant chemotherapy (carboplatin & paclitaxel
...
McKenzie E., Cervical Cancer, Stage 3C2
Symptoms: Severe abdominal & back cramping, persistent & extreme pain, heavy discharge & bleeding
Treatments: Radiation, chemotherapy (cisplatin), brachytherapy, immunotherapy (Keytruda)
...
Marissa N., Squamous Cell Cervical Cancer, Stage 3B
Symptom: Excessive and prolonged vaginal bleeding
Treatments: Chemotherapy (cisplatin), radiation, brachytherapy
...
Alicia P., Bile Duct Cancer (Cholangiocarcinoma), Stage 4 (Metastatic)
Symptoms: Bleeding for a month, passing large clots of blood, severe pain in lower back
Treatments: Chemotherapy, radiation therapy
...
Leanne B., Cervical Cancer, Stage 4
Symptoms: Fatigue, irregular periods, pain after sex
Treatments: Radiotherapy, brachytherapy, chemotherapy (carboplatin & paclitaxel)/p>
...
Kristine M., Adenocarcinoma Cervical Cancer, Stage 2B
Symptom: Tumor found during postpartum pap smear
Treatments: Colposcopy with endocervical curettage, cone biopsy, total abdominal radical open hysterectomy with lymph node removal
...








