Cara’s Stage 2C Cervical Cancer Story
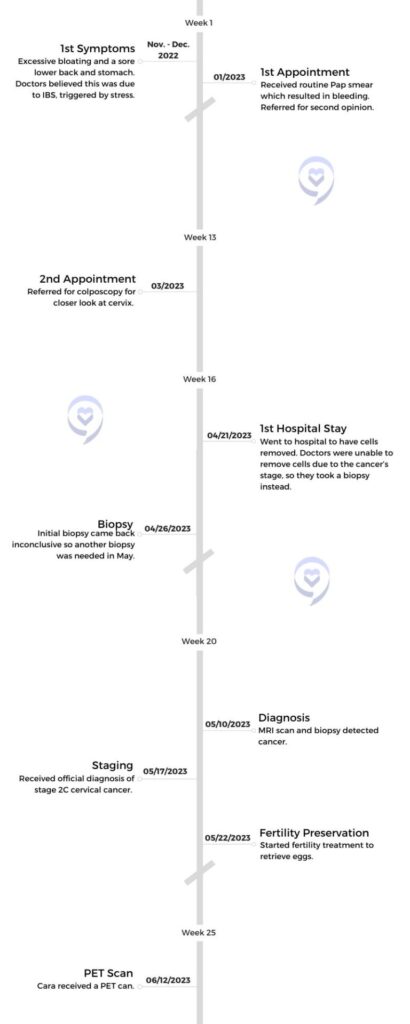
Cara, a 34-year-old primary school teacher from Inverness, Scotland, shares her journey with stage 2C cervical cancer. Despite experiencing symptoms like lower abdominal and back pain, along with bloating, she initially attributed them to irritable bowel syndrome (IBS). Due to a lack of awareness about cervical cancer symptoms, Cara’s diagnosis was delayed. She highlights the importance of recognizing potential signs early on.
Following a routine pap smear, abnormalities prompted further investigation, leading to a diagnosis of cervical cancer. Despite initial uncertainty, subsequent tests revealed the cancer’s extent, classified as stage 2C due to its spread beyond the cervix. Cara underwent cancer treatment, including chemotherapy, radiotherapy, and brachytherapy, alongside fertility preservation measures due to the impact on her reproductive health.
Cara emphasizes the need for increased awareness and education about cervical cancer symptoms, especially among younger women. By sharing her experience, Cara hopes to encourage others to prioritize their health, seek medical attention for concerning symptoms, and advocate for more comprehensive gynecological education.

- Name: Cara R.
- Diagnosis (DX):
- Cervical Cancer
- Staging:
- 2C
- Symptoms:
- Lower back pain
- Abdominal pain
- Excessive bloating
- Treatment:
- Chemotherapy
- 6 rounds
- Radiation
- 25 sessions
- Brachytherapy
- 3 days
- Hormone replacement therapy
- Chemotherapy
We need to be empowered by our knowledge and by our actions. Hopefully, bigger change will come government-wide and in education in schools, youth clubs, and anywhere else that we go.
Cara R.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Symptoms
Tell us about yourself

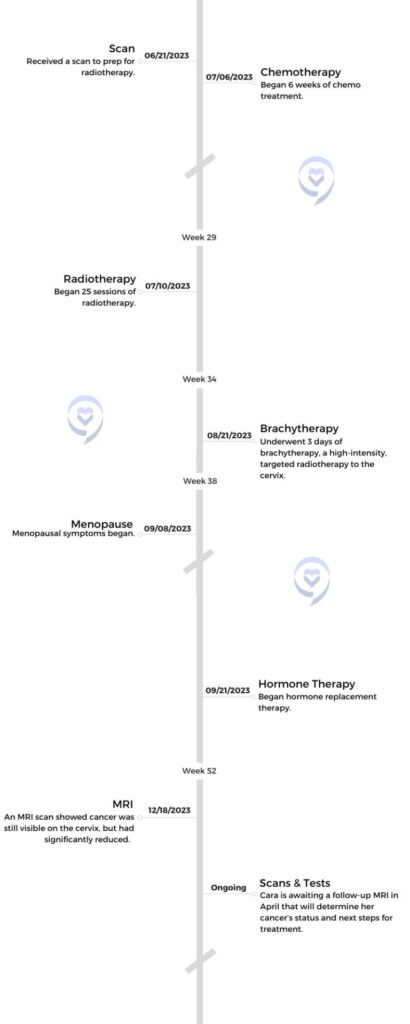
My name is Cara. I’m currently 34 and I’m a primary school teacher. I live in Inverness, in the Highlands of Scotland. In my free time, I like to go running, go to the gym, and socialize. I like to spend my spare time with family and just really love being around people.
What were your first symptoms?
It all started, I would say, in November or December of 2022. I was getting lots of lower abdominal pain, lower back pain, and excessive bloating. I had gone back and forth to the GP and they suggested that I had irritable bowel syndrome. They said that that’s something that could be triggered by stress. At the time, life was a little stressful and work was stressful, so it made sense. I didn’t question it.
Unfortunately, I didn’t know the symptoms of cervical cancer. That’s one of my regrets. I just had no awareness. I didn’t question the GP and I certainly didn’t challenge it. I just tried to reduce certain foods out of my diet that could be triggering. I did so much research about what that meant for my gut health. I went down the line of, I have IBS, how can I manage this?



The symptoms were getting progressively worse to the point that I was taking time off work, and I had a hot water bottle strapped to me. I spent an obscene amount of time in the bath just because it took the pressure and the pain away. Eventually, I had to take painkillers. Not strong painkillers, just paracetamols. I was unable to go on any car journey that was longer than 15 or 20 minutes because of the discomfort. It went from being a little sore to more severe and more frequent. It was almost every day.
At this point, I genuinely did not make the link. I should have. If I knew the symptoms and I was more aware, then I would have.
Receiving a routine pap smear left doctors wondering
It just so happened that I was due for my smear test in January of 2023. At that appointment, when the nurse did the scraping of my cervix, she said, “Oh, there was a little bit of a bleed there.” She asked me lots of questions and said, “I’m just a one-man band. It’s just myself that works here. For my peace of mind, I would like you to have a second opinion. I would like to book you back in for a GP that specializes in female health.” I said, “Yeah, no problem at all.”
About a month later, I went back to the GP and it was with this lady who was fantastic and she has a special interest in female health. She said, “I think I can see a little bit of a discoloring at the neck of your cervix. At the moment, I’m not overly concerned, but I think it would be a good idea to get you referred to the colposcopy clinic in the hospital. Have you had your smear results back yet?” I said, “No, funny you should say that. I did phone to chase them but there was a bit of a delay.”

The symptoms were getting progressively worse to the point that I was taking time off work.
I think usually in the UK it’s about a 6 to 8-week wait. Unfortunately, it was closer to about 16 weeks at the time. I’m not sure if that was because it was just a backlog or the time of year, but there was a delay. She decided to get the ball rolling anyway and have me referred to the hospital.
Did you suspect you had cancer at this time?
We started to think, okay, this could be more. At this point, I genuinely did not make the link. I should have. If I knew the symptoms and I was more aware, then I would have made the link. But I thought I had two parallel things going on here: an abnormal smear and IBS. Two completely different things.

We went to the colposcopy clinic. She had a little look at the health of my cervix and said, “I can see the discoloring that we’re talking about. I think they might just be high-risk cells. Fairly common. What we do is remove these cells, and depending on how severe they are, there are slightly different ways of doing that.” I was a bit nervous, naturally. It just so happened that afternoon when I got home, my smear results had come back to say, “There are high-risk cells being detected and we need to get them removed,” but I was already in the process.
Diagnosis
Receiving tests & scans to reach a diagnosis
I’m petrified of needles and anything related to the hospital. Until this point, I had only ever been to the doctor for eczema and just the usual things. Nothing serious. I opted to be put to sleep for the procedure. They give you lots of information about how it will be carried out, and the thought of them burning cells from the cervix, awake, didn’t fill me with joy. It filled me with stress.

I think if more women knew about their gyno health, if we knew symptoms for different gyno issues that happen, and we know the places to go for help, I think that would make all the difference to women.
It’s quite an undignified thing, sitting in the gyno chair. I’ve always been so private. I’m not one to flaunt my body or anything. To have someone there between your legs, it’s tricky. I understand I needed to do it, but I opted to be put to sleep, and I just thought, if I go to sleep, then I don’t know what they’re doing. They see this every day. I don’t need to be worried about anything other than just going in and getting it done. She could see I was very nervous at the appointment.
Due to my naivety at the time, I said, “I’ve been with my partner for 10, nearly 11 years. Is this a sexually transmitted disease? Should I be tested for other things?” I was hysterical because I didn’t know what HPV was and it was my first time learning about it. It was my first experience of having an abnormal smear or having to do anything about it. It was all foreign land for me.

»MORE: Reacting to a Cancer Diagnosis
To be honest, that in itself needs to change, because going to a colposcopy clinic and going to a gyno clinic is normal to a certain extent. This place is meant to make you better. They have such a specialized service, that actually, I think if more women knew about their gyno health, if we knew symptoms for different gyno issues that happen, and we know the places to go for help, I think that would make all the difference to women.
Overcoming the stigma of gynecological health
In this country, it’s embarrassing to talk about. There’s a stigma related to talking about your gyno health. People tend not to do it without a beetroot-red face and get embarrassed and want to skip the subject. I get it. I was that person. I probably didn’t go for my smear as quickly as I should have because I was so embarrassed. I was so ashamed of my body.

Looking back now in hindsight, that’s ridiculous. But that’s just truly how I felt. I think lots more can be done in schools and youth clubs and at home with your friends. If we talk about these things, it just normalizes them. Women have vaginas, that is what we’re built with. We have a cervix. These words are not swear words. We shouldn’t be embarrassed to say the word, because if we’re embarrassed to say the word, we’re going to be embarrassed to seek help when something down there goes wrong, whether it be discharge or something that changes.
I think we will empower ourselves if we talk about these things openly. Burn down all of the stigmas, because it’s so important that we look after our female health. The same goes for men, but we’re talking about cervical cancer. A lot needs to change. I don’t know if it’s the same in [America], but over here, a lot needs to change.
What were the initial results from your cell-removal procedure?
I was put to sleep for my procedure. I was then awoken from the procedure. I got myself dressed and had some water and something to eat. You have to tick those boxes before you’re allowed to leave the hospital. I thought I didn’t even feel sore down there or tender. The consultant came in. The lady that spoke to me before the appointment. She came in before to say hello and, “I’m going to be carrying out the procedure today. This is what we’re going to do. Do you have questions?” The same lady, came back in after the procedure and said, “Can we go somewhere more private?” I burst into tears.
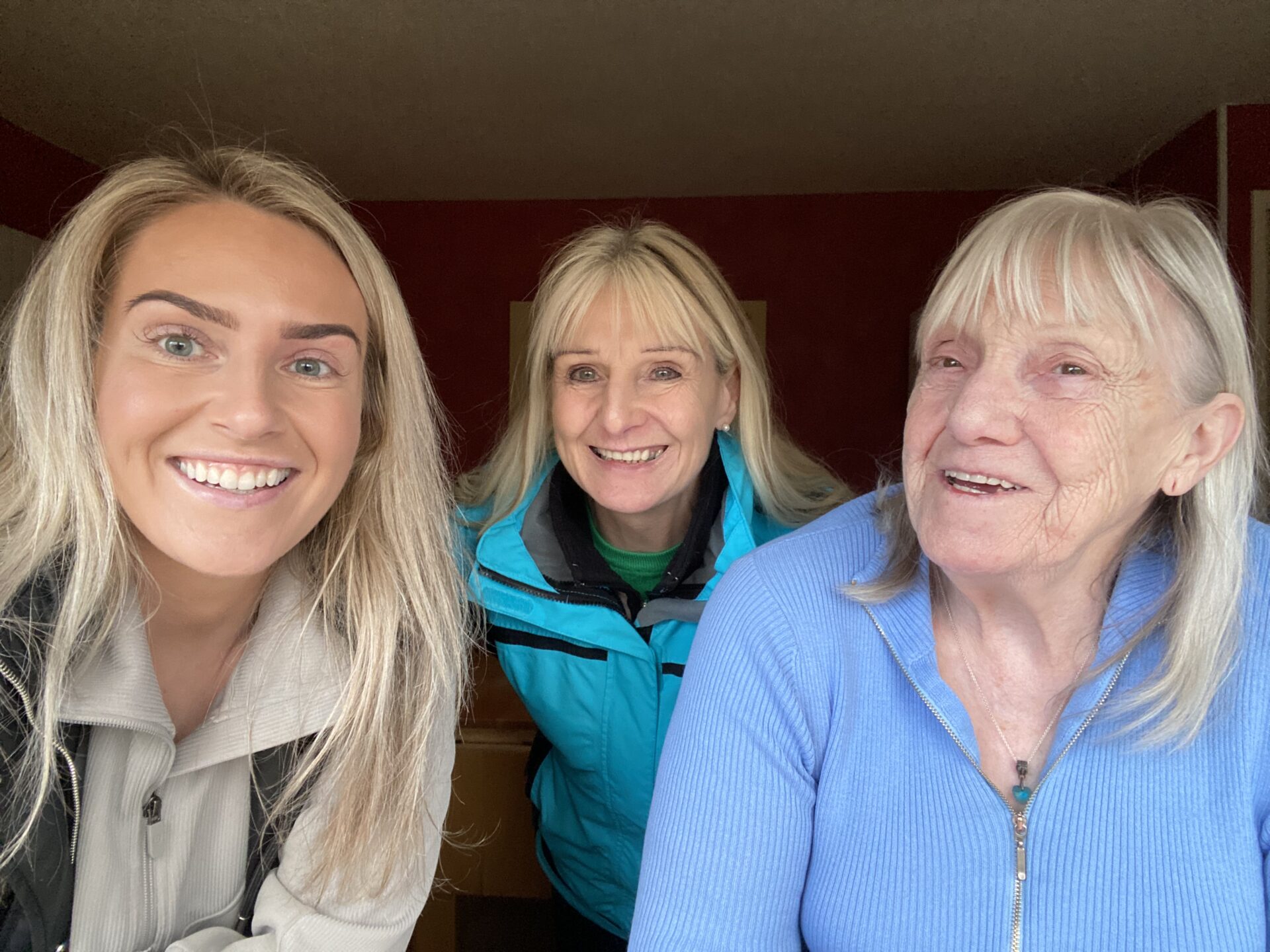
We were in a shared ward. I think there were maybe 6 other ladies there. I thought this wasn’t good if she wanted a private chat. She said, “We could do it here if you’d prefer, but I think it would be better for it to be private.” Luckily, my mum and my auntie had walked through the door to take me home. I messaged them and said, “It’s done.” Little did I know, it wasn’t done.
The three of us, me, my mum, and my Auntie Shirley, went into her little room and she knelt in front of me and put her hand on my knee. I thought, oh, this is terrible. She said, “I’ve gone in to remove the cells. Unfortunately, I wasn’t able to do that today. I think we’ve gone beyond cell removal.” I asked, “What does that mean? Do I have cancer? Am I going to die? Am I going to lose all my hair?”
I don’t remember what she said after that. Everything just went silent. My brain was rushing so I wasn’t able to process what else was happening in the room. I do remember her saying, “Cara, I’m so sorry, but I can’t answer those questions right now because we don’t know what we’re dealing with. What I have been able to do is take biopsies. We’re going to send them away to the labs and they will give us those answers. I’ll just leave you for a moment with your family.”

How did you process your cancer diagnosis?
Due to naivety, I thought cancer meant I was going to die and there might not be anything they can do for me.
I didn’t know how serious it was, if I had a diagnosis or not, how unwell I was, and unfortunately, the consultant wasn’t able to answer my questions. I completely understand why she wasn’t expecting that situation either.


That day we left the hospital, and naturally, my brain went to the worst place. I thought I was probably going to get quite a serious diagnosis here. Due to naivety, I thought cancer meant I was going to die and there might not be anything they can do for me. I suppose my experience of cancer is in much older people, and usually, the result is that they do pass on. I suppose I’m very lucky that I don’t know lots of people who have experienced a cancer diagnosis.
Now I know there are lots of cancers and treatments, and there is so much hope and success with those treatments that the result isn’t always dying. I wish I knew that at the time. I think I was just looking for a bit of reassurance, but I also understand she can’t give me reassurance in case what she was saying wasn’t right. I lived in a bit of a haze for a few days.
Staging
When did you receive an official cancer diagnosis?

The labs are back and cancer has been detected.
The gyno team at the hospital contacted me and said, “I would like you to come in. I specialize in gyno cancer.” He was able to answer all my questions and said, “Right now, we don’t have your diagnosis because of the biopsies that were taken, there’s not enough tissue there. I’m going to do the same procedure again. But this is what I do. This is what I specialize in. I want you to come in tomorrow morning and we’re going to squeeze you in as an emergency case.”
He took the biopsies. At that point, he was able to answer all the questions. What happens if this happens? What happens if it is cancer? He gave me lots of different scenarios and what would happen in each of those. I was like, okay, this might not be the end. After he took the biopsies, he also referred me for an MRI. He said, “Let’s just get this ball rolling.”
I think about a week later he phoned and it was the day of my MRI. In the morning I went in for my MRI and in the afternoon he phoned and said, “Cara, I just wanted to let you know the labs are back and cancer has been detected. At this time, we’re not able to give you your staging until we get all your scans.”
What staging were you?
There was also a question mark around my lymph nodes from the MRI. They were slightly swollen, [doctors] were curious as to whether they were swollen because they were trying to fight what was going on down there, or was there cancer involved in the lymph nodes. I was then sent for further scans. Thankfully, the lymph nodes were not infected. They were just inflamed.


The cancer was contained to the neck of my cervix, which they called a large tumor. I believe it was somewhere between 3 and 4 cm. It had gone slightly into the surrounding tissues so that it impacted the neck of my womb as well as my cervix. That made me stage 2C. I think I would have been stage 3 if the lymph nodes were involved, but thankfully they weren’t.
Fertility Preservation
Did you discuss fertility preservation?
We started to talk about fertility. He asked, “Are you a parent?” I said, “No, at the moment I’m not.” He said, “I really need you to think about if you want to be a parent.” I said, “Absolutely.”
Although children were not in my or my partner’s imminent plan, they were definitely always the plan for the future. I think you always just assume that you’re going to have babies and have a family. Me and my partner had been together a long time.
He referred me to a fertility clinic in Aberdeen about 100 miles away from my hometown. That process started.

Describe the fertility preservation process
The next stage was fertility preservation. I got my diagnosis and we had the chat on Wednesday or Thursday of one week. The gyno doctor had referred me to the fertility clinic. I think I started treatment that following Monday. It was so quick. I had an injection every day for 5 days. On day 5, that went up to 2 injections. Then at the end of the second week, I believe there was a third injection.

The first injection was to harvest my eggs and to get my ovaries nice and juicy. I’m not going to use all the technical language because I don’t remember it, but this was the way it was explained to me. The second injection on the second week was to stop my ovaries from releasing the eggs like a period. That third and final injection – I think they called it a trigger injection. Exactly 36 hours after that injection was administered, that’s when they took the eggs out.
I was very, very lucky that on my 34th birthday, I was in the procedure for egg retrieval. They managed to successfully take out 14 eggs that they had frozen. Through freezing and thawing, they’ll not all survive, but 14 is a lovely number and I’m really happy with it. It was our only opportunity. It was now or never.
Pregnancy success rate post-cervical cancer

It was explained to me right at the start that any treatment to your pelvis is really going to impact your fertility in the future, and it’s probably unlikely you will successfully carry a baby to term because of the impact on your cervix. Apparently, from treatment, it shortens your cervix. Even if I was to fall pregnant, unfortunately, I’d be very likely to miscarry because of the weight of the pregnancy on the cervix, it wouldn’t be strong enough to hold. It was explained right from the get-go and we were very lucky to have that opportunity.
»MORE: Fertility After Cancer Diagnosis
I know other women, I’ve heard their stories and fertility just wasn’t something that was discussed with them and they missed the opportunity. It wasn’t offered to them and it was straight into cancer treatment. I got my egg retrieval on the 5th of June, which was my birthday, and then we had a few more scans to do. That was when I met with my oncologist for the very first time.
Cancer Treatment
Beginning cancer treatment
[My oncologist] is the person that pulls all the strings and he makes all the decisions about my treatment and everything else. He took me and my partner in to discuss what it was going to look like and how it was going to be done. He answered all our questions.
It was decided that I would have 6 chemotherapies. I started them on the 6th of July. Every Thursday for 6 weeks I had chemotherapy on a Thursday, and running alongside that Monday to Friday, I’d go in for radiotherapy each day for 25 sessions. On a Thursday morning, for example, I would go into my radiotherapy. When you’re on the bed doing the actual radiotherapy, it doesn’t take very long and you’re on the bed for about 10 minutes. It’s high doses of radiation targeted at your pelvis or to the tumor area.

»MORE: Chemotherapy FAQs & Patient Stories
On a Thursday, I had just enough time for a wee cup of tea and then I was straight into chemo. I was there most days till about 4 or 5. It was a really long, exhausting day on a Thursday. Every other day was just radiotherapy. I had to drink a certain amount of water and then wait for my bladder to fill, and then I would go on to the bed and they would do the treatment from there. It’s so surreal thinking about it. It doesn’t feel like I did it, but I did.
Describe your experience with brachytherapy

That was for 6 weeks, then I had a week off, and then I came back down to Aberdeen and did what’s called brachytherapy. That’s direct treatment to the cervix. An applicator is inserted into the vagina and connects to your cervix. Targeted radio pellets run up through this machine. I did that over 3 days. It’s a proper procedure to get the apparatus inserted, and it stays there for 3 days.
You lie flat on this bed and try not to move. You don’t want it to be moving inside of you because it’s programmed so perfectly that the radioactive pellets hit just at the right spot at the right time. It’s incredible equipment and an incredible way of doing things. Apparently, it’s one of the oldest methods of radioactive treatment, and they still use it today.
I’m not going to lie, that was quite horrific. I think it’s the invasiveness of it. Your dignity is all gone as you’re being wheeled around a hospital with a catheter hanging out, and this apparatus inside you. It wasn’t pleasant, but that was a really important part of the treatment. I think the consultant said, “This treatment is going to give you another 50% of the amount of radiation you’ve already had.” I had a certain amount over 5 weeks, the 25 sessions. “This is going to give you 50% of that again targeted over 3 separate sessions.”
Overcoming mental barriers to receive treatment
Again, my mind was blown. I’d never heard of brachytherapy before in my life. I did consider declining that part of the treatment. When I read about it, I thought, I just don’t know if I can do this. I struggled to get a smear test, never mind having this procedure done. It just felt so invasive and undignified. I was mortified thinking about it.

I decided that it was really important that I did it, and I had to do everything I possibly could to make sure that my outcomes were positive, and that I was going to hopefully live a long and happy life. I just had to get over myself at that point and decide. This could be life or death. Cara, get a grip. Just go in, get it done, and hopefully, you never have to do anything like that again.
Did you have any side effects from cancer treatment?
The chemo definitely made me tired, super tired. I was very lucky though. I know that lots of chemo makes you lose your hair. I was very fortunate that that wasn’t the case for me. I wasn’t overly telling everybody [about my diagnosis], so not everybody knew. I told the people who needed to know – my best friends, family, and work colleagues. Beyond that, I wasn’t shouting it from the rooftops. I felt like if I lost my hair, everyone would then know. Sometimes that’s not a conversation you’re ready to have, but you’re almost forced to because people can physically see you’re not okay.
Everybody warns you about how brutal it’s going to be, but it’s just a case of showing up and taking each session as it comes.
I know chemo makes people vomit a lot and physically sick. Again, I was very lucky that that wasn’t the case for me. My symptoms were nosebleeds, lots of shivering, headaches, and fatigue like you wouldn’t believe. When the chemo goes in, it goes in through your hand through a cannula. It’s so cold, that you can feel it travel up your arm. It’s the weirdest sensation.
The nurses, I have a whole different level of respect for what they do on the daily. They were so happy and chirpy, and they just lifted me up and didn’t stop. My chemo, for some reason, took quite a long time to go into my body, whereas lots of other people were in and out. I saw most of the people come and go throughout the day. I was probably there for one of the longest. I’m not sure why that was. Different chemos, different cancers, different treatments, I suppose.
Everyone was so lovely. Considering it’s a cancer treatment, you would expect it to be quite a sad place, but it wasn’t. They were all so lovely and really supportive. It was a surreal experience.

Hormone Replacement Therapy
What would you tell someone going through cancer treatment?
You’re going to get through it. I was going to get through it. I was so scared because it can be really brutal. Everybody warns you about how brutal it’s going to be, but it’s just a case of showing up and taking each session as it comes. Everybody is going to be different and everybody’s body is going to react differently. I think I just put so much pressure on myself, I was so petrified of losing my hair and of the side effects.

I wish I was more accepting of, what will be will be. If I lose my hair, I lose my hair. I wish I didn’t spend so much time dwelling on those things. Some of those things didn’t even happen, so it just feels like such a waste of energy. It’s not a scary place. I mean, it is scary, but the ladies that treat you truly make a difference. They’ll look after you and they’re going to make sure you’re alright. There’s no need to be any more scared than you already are of your diagnosis.
Experiencing premature ovarian insufficiency
After brachytherapy, I knew I was going to have to physically recover. I was very sore and on lots of medication. My head was quite hazy for a few days until I got home and slept. After that, it was very quickly that menopause started to hit me. I thought it was treatment. I was getting really hot flushes and my body was getting really sweaty. I could almost feel a heat rise through my body. It would rise up my back and feel quite prickly.
At first, I didn’t make the link. One day I was with my mum and she was drinking her tea. I could hear her gulp and it irritated me beyond words, which is completely irrational. Poor mum, just having her cup of tea, but it made me angry, which is so silly. I knew at that point, something was not right. I would never have noticed that before. Never mind, let it bother me. There were a few other things besides the agitation like a really low mood. When I say low, I’m talking way lower than at any time during treatment. I just could not see the silver lining.
Throughout treatment, I always found 3 things I was grateful for in a day. It was something I learned from a coach years ago, and I’ve done it intermittently. I thought it was really important that I look for things that I’m grateful for through this time, and it made a difference to my mindset. Life is good, and I am very lucky. It gave me that positive something just to get me through. On some of these really low days, I couldn’t find a thing. I was so low and the headaches and my skin were so itchy, it was crawling, oh my goodness. Some of the side effects were just horrendous.

It was very quickly that menopause started to hit me.
I went to my GP, I contacted the hospital and they said, “Speak to your GP. This sounds a little bit like menopause, which is likely with the treatment that you’ve had.” I went to the doctor and true enough, it was premature ovarian insufficiency. My ovaries were now no longer producing eggs the way that they would have or should have as a result of treatment. They were so damaged.
Receiving hormone replacement therapy
Over time, my ovary’s ability to produce estrogen will fluctuate and slowly decline to when it just won’t [produce] anymore. Because my GP was amazing and really knew her stuff, she walked me through all the options and said, “I think that hormone replacement therapy is a good idea for you. The way I look at it is that your body is no longer producing, so your body is losing its estrogen production. All we’re doing is topping up that bucket. We’re just giving you what your body would have been making itself. We’re replacing what your body’s losing.”
She sent me away to have a think about it. I did a bit of my own research. When I realized what estrogen does for your body in terms of your cardiovascular health, your brain health, your eyes, and your female organs, I was blown away. I thought, whoa, I cannot allow my estrogen levels to just deplete and not replace them. That’s going to set me up in a world of being scared of having a heart attack. And what about my bone health?



Basically, my womb is aging much quicker than it ever would have. I think in the UK, they say an average age would be about 50 to 51 [to have menopause], and at the time I was only 33. We’re talking almost two decades earlier. It petrified me to think that my body wouldn’t have estrogen. My consultant said I was okay to have hormone replacement, so I went for it.
I have to say, it’s made a huge difference to my mood and to all the other side effects. It is definitely still a daily struggle in terms of the symptoms that just come from nowhere. Some days I feel like a little kangaroo and I’m ready to take on the world, and other days I just can’t. My energy levels are really low. Lots of fatigue, and headaches, my eyesight is a little duller than it was before, and I have aches and pains. The list really does go on. It has such an impact on your body.
Reflections
A need for more education on women’s health
I was lucky that my GP was fantastic. I know not everybody has the same experience. Lots of GPs are not educated and they don’t have to keep up with hormones, or they don’t have to keep up with the newest studies and trends in terms of knowledge around female health, hormones, or menopause. It’s only if you have a keen interest that you then take it upon yourself to learn more.
There’s definitely a gap there in education too in terms of GPs. I know that they have a huge curriculum to get through, and I don’t think the hormone and the menopause stuff takes up very much of that time. Maybe a few hours, a few modules. I don’t know the exact specifics, but I do know that it’s not enough to support 50% of our population at all ages. It’s going to impact all women.

Also, there’s a real thing of [people assuming] you’re too young. No, we’re not too young. Women go through premature ovarian insufficiency (POI) way earlier like in their early 20s, late 20s, their 30s. Menopause isn’t just for a woman in her late 40s, or early 50s. It’s really not. I think the sooner we raise awareness about it the sooner the government takes it more seriously and realizes that our GPs really need to be educated to a much higher level to support these women…
Some women are going back and forth to their GP for 10 years and still not getting a diagnosis, which means that for 10 years, the estrogen in their body is depleting, sometimes progesterone and testosterone too, but 10 years? That’s really putting them at risk. Not to mention the daily struggle and suffering because they think they’re bananas. They think they’ve lost their minds because that’s what they’re being told. But no, you’re just experiencing early menopause or perimenopause. We’ve got a lot of work to do.
»MORE: What Does Cancer Feel Like?
What do your current scans show?
I was scanned on the 18th of December, just at the start of the new year. I had a call from the consultant to say that the scan was good and not so good. The tumor is now mostly gone, and lots of the surrounding tissues that were showing as cancerous are now showing as scar tissue, which is what they would expect. However, there is still this cluster of cells that are visible.

At the moment, they’re just going to monitor me because unfortunately, the scan is not completely clear. What they’re going to do from December to April is they’re going to leave me and I’m going to be scanned on the 23rd of April. I suppose I’m just praying that the scan is completely clear and hopefully, I can just move on. That’s all I’m praying for.
What would you tell someone on their cancer journey?
If you’ve had a diagnosis, you’ve absolutely got this. I’ve had lots of people say, “I don’t know how you’ve done it.” You do it because you have to. You don’t have a choice. I can promise you that you are going to absolutely surprise yourself with your resilience and your strength. I mean, that won’t be every day. There will be days where there are lots of tears and you lose hope, but you can do it and you will do it 100%.
If you don’t have a diagnosis but you’re supporting someone who does, just be there. Sometimes a cuddle is enough. Sometimes listening is enough. Sometimes a hand of reassurance or that little cup of tea is absolutely enough. Make sure you’re checking in on that friend even if they go silent. Treatment is so all-consuming. That little text message of a love heart or that text message that says, “I’m thinking of you today. You’ve got this. Love you.” Those very messages and check-ins make a world of difference. I think for everybody when you’re healthy and well, we all need to do better.

If you’ve had a diagnosis, you’ve absolutely got this.
We need to educate ourselves on female health. We need to educate our daughters, our sisters, our aunties, and our nieces, and we need to talk about it. There is no shame in having a vagina, or a cervix, or going for these health appointments. They’re so important. We go to the dentist for our teeth. We just need to go to the doctor or the GP for our smears. It’s so important.
Please keep on top of all your health issues. Any changes? Report them. Get to know your symptoms. There are 5 gyno cancers and there are symptoms linked to each. If you know them, you know what you’re looking for and you can detect a change. It was silly that I didn’t know so it took longer. Don’t get me wrong, those symptoms can be other things, but if you go to a GP, they can really look into it for you. We need to be empowered by our knowledge and by our actions. Hopefully, bigger change will come government-wide and in education in schools, youth clubs, and anywhere else that we go.
More Cervical Cancer Stories
Willow B., Pelvic Cancer, Grade 1, Stage 2.5
Symptoms: Persistent fever-like chills, scratchy throat, fatigue, post-orgasm pain, heavy bleeding, severe cramping
Treatments: Surgery (radical hysterectomy), radiation, chemotherapy, hormone replacement therapy (HRT)
...
Samantha R., Adenocarcinoma Cervical Cancer, Early Stage
Symptoms: Irregular bleeding, pain
Treatments: Surgery (radical hysterectomy, pelvic exenteration), chemotherapy, immunotherapy, radiation therapy, hormone replacement therapy, hyperbaric oxygen therapy
...
Amanda L., Cervical Cancer, Stage 3
Symptoms: Heavy periods, abnormal bleeding, large blood clots, severe cramping, severe abdominal pain, pain radiating down the left leg, loss of mobility in the left leg, loss of appetite, fatigue
Treatments: Chemotherapy, radiation therapy (external beam radiation therapy & brachytherapy)
...
Mila L., Squamous Cell Cervical Cancer, Stage 1B1
Symptoms: Abnormal lump in cervix area, bleeding after sex
Treatments: Chemotherapy (cisplatin), radiation, adjuvant chemotherapy (carboplatin & paclitaxel
...
McKenzie E., Cervical Cancer, Stage 3C2
Symptoms: Severe abdominal & back cramping, persistent & extreme pain, heavy discharge & bleeding
Treatments: Radiation, chemotherapy (cisplatin), brachytherapy, immunotherapy (Keytruda)
...
Marissa N., Squamous Cell Cervical Cancer, Stage 3B
Symptom: Excessive and prolonged vaginal bleeding
Treatments: Chemotherapy (cisplatin), radiation, brachytherapy
...
Alicia P., Bile Duct Cancer (Cholangiocarcinoma), Stage 4 (Metastatic)
Symptoms: Bleeding for a month, passing large clots of blood, severe pain in lower back
Treatments: Chemotherapy, radiation therapy
...
Leanne B., Cervical Cancer, Stage 4
Symptoms: Fatigue, irregular periods, pain after sex
Treatments: Radiotherapy, brachytherapy, chemotherapy (carboplatin & paclitaxel)/p>
...
Kristine M., Adenocarcinoma Cervical Cancer, Stage 2B
Symptom: Tumor found during postpartum pap smear
Treatments: Colposcopy with endocervical curettage, cone biopsy, total abdominal radical open hysterectomy with lymph node removal
...









