Kristine’s Stage 2B Adenocarcinoma Cervical Cancer Story

Kristine shares her stage 2B cervical cancer story, which began with a postpartum pap smear. She underlines going through a colposcopy and how she chose a radical hysterectomy.
In her story, Kristine also highlights how she was able to navigate quality-of-life issues, including being a self-advocate as a patient, dealing with loss of fertility, guidance on parenting and marriage with cancer, and how to ask for help and support, no matter how hard it is.
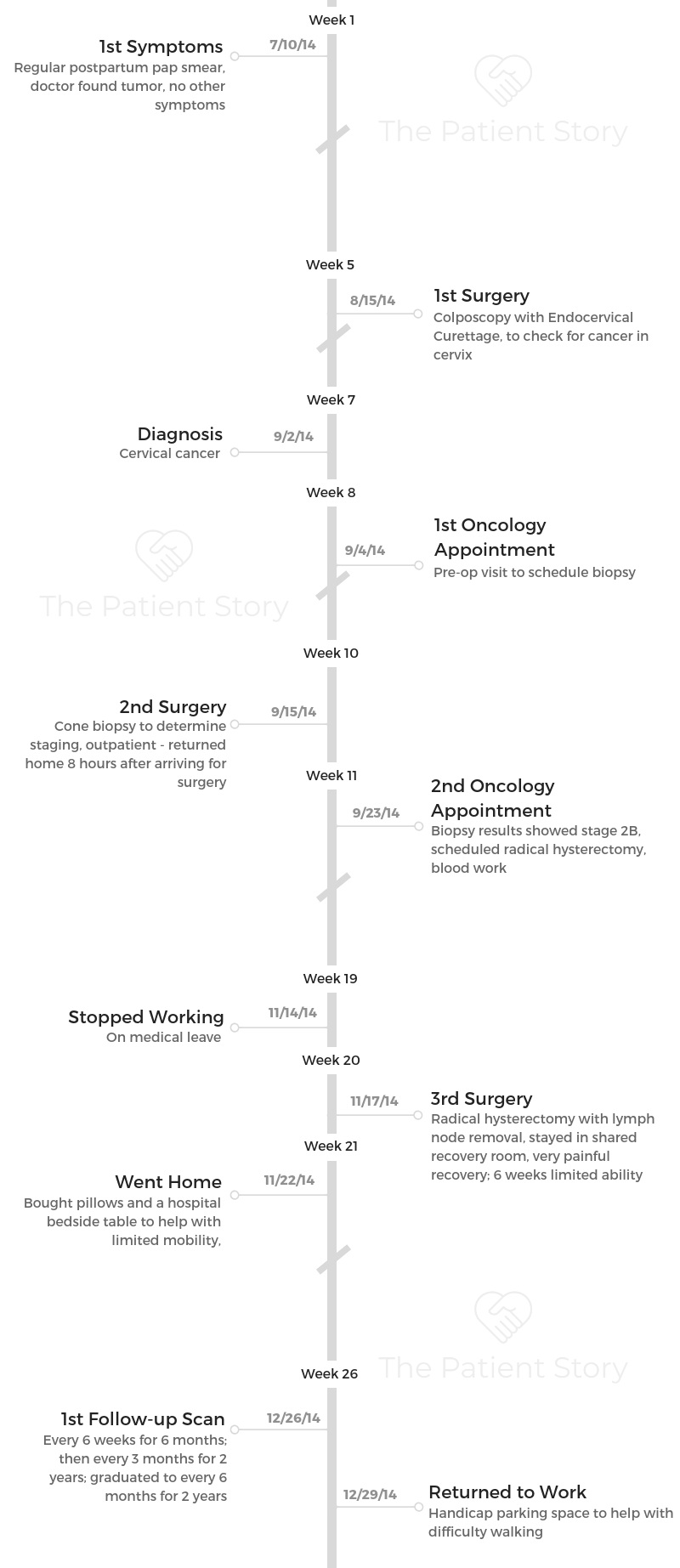
- Name: Kristine M.
- Age at DX: 30
- Diagnosis:
- Cervical cancer
- Adenocarcinoma
- Staging:
- 2B
- 1st symptoms:
- Tumor found during postpartum pap smear
- Treatment:
- Colposcopy with endocervical curettage
- Cone biopsy
- Total abdominal radical open hysterectomy with lymph node removal
It will be okay. You will eventually get to a point in your life where you like yourself more as a result of what you’ve gone through.
You won’t believe it now, but you’ll be a stronger and better version of yourself.
Kristine M.
- Pre-diagnosis
- Diagnosis
- Describe the moment you knew you were dealing with cancer
- Did you get a second opinion?
- Why was your reaction to the diagnosis “different”?
- Describe the mental stress of dealing with your diagnosis
- Did you have anxiety waiting for staging results?
- How did you break the news to your husband?
- How did your husband handle the diagnosis?
- How did you approach telling your young kids about your diagnosis?
- Was there anything specifically to consider about being a young mother diagnosed with cancer?
- Did your doctors recommend any resources for your family?
- Treatment & Surgery
- Describe your cancer treatment center
- Any advice on how to choose a treatment center?
- What happened at your first cancer center appointment?
- What was the timeline for tests and biopsies?
- Describe the colposcopy
- How did the staging happen?
- Describe the cone biopsy
- Any tips for people before undergoing a cone biopsy?
- How did you decide on the radical hysterectomy?
- What was the pre-surgery routine for the hysterectomy?
- Is there anything you wish you had asked or done before the hysterectomy?
- Describe the cleaning prep process
- Any surprises heading into surgery?
- Any apprehension about the general anesthesia?
- Post-Surgery & Recovery
- Do you remember having any side effects after you woke up from surgery?
- What would you change about your post-op hospital stay?
- What was the short-term recovery after surgery like?
- Are you still dealing with long-term side effects?
- What was your first follow-up appointment like?
- How long after your hysterectomy did you have to wait for follow-up results?
- What has your experience with post-op scans been like?
- Did you ever have to self-advocate?
- Do you have a message to patients and caregivers about being their own advocates?
- How did it feel to realize you would lose your fertility?
- Have you found your “new normal”?
- Did you need outside help with your kids?
- Do you have specific advice for a parent who is undergoing cancer treatment?
- How did your treatment affect your work?
- How did you deal with the financial aspect of treatment?
- How did you change your lifestyle after surgery?
- Mental & Emotional Stress
- Support & Survivorship
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

Pre-diagnosis
What were your first symptoms?
It’s scary to say this, but I had no physical symptoms. When I was in college, I was moving to the city that I live in now. As most people do when they are done with college, they move to where they’re going to get a career.
Part of my plan was to move on. I figured I had a doctor where I was. I would get everything I need taken care of before I moved. It was after I moved to Ohio when my doctor’s office called me.
They said not only that they had found irregular cells, but that they had found cancerous cells during my regular pap.
What was the next step?
I was in my early twenties at that time, and they recommended that I have another gynecology appointment in Columbus, so I did. The doctors that I had in Ohio didn’t find anything wrong with me.
I was told that it’s very common for test results to get mixed up. It didn’t feel very reassuring, but I believed them and went on with my life.
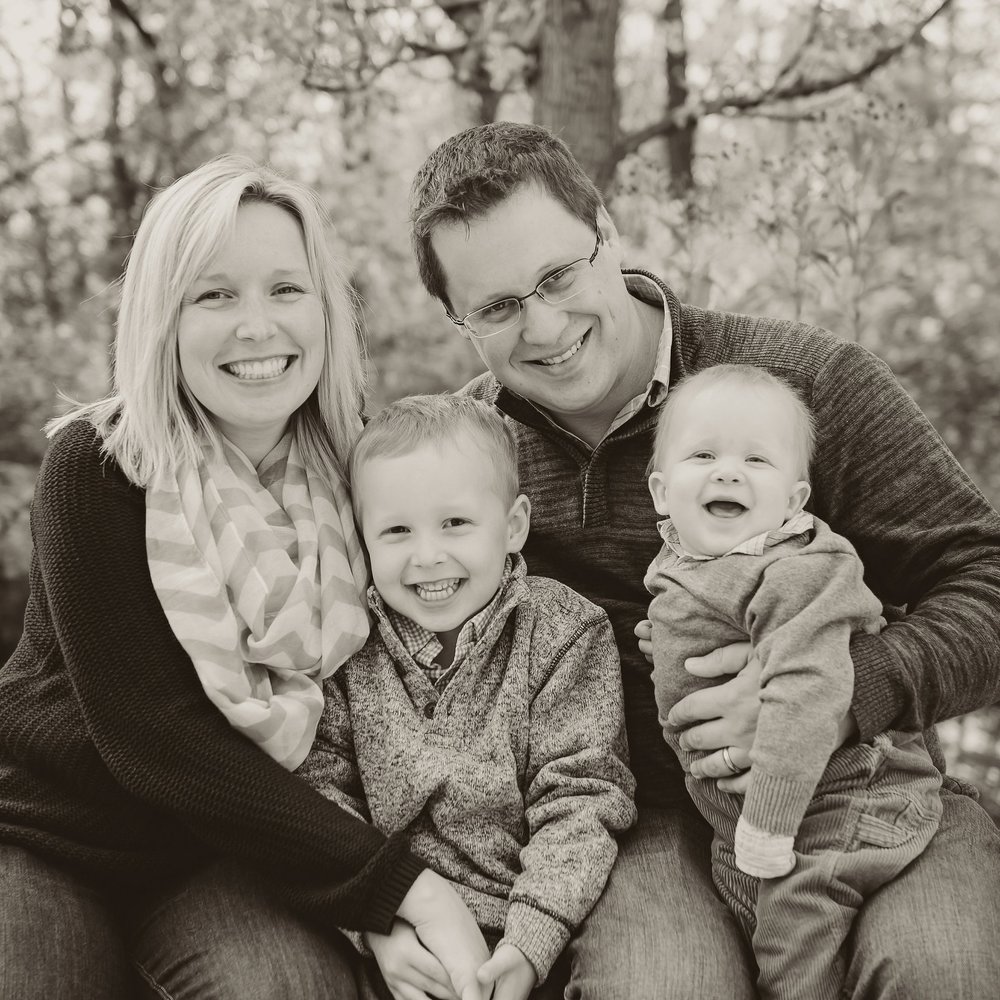
Then 2 years later, I was married. A year after that, I had my first son. I had no unusual symptoms. He was a large baby. I never dilated and never went into labor, but because he was big, they just assumed that that was the reason for it.
I had a cesarean and a healthy baby. I continued with my regular gynecological care through that whole process. 4 years after that, so 6 years from my original cancer scare, I had my second son.
Usually if you have one C-section, they want you to have another C-section. That’s how that happened for me, but again, I never dilated. I wasn’t going into labor.
Why did your original abnormal test results not produce an official diagnosis?
What they think happened is that I had a lower stage of cancer cells that whole time.
It had gone from stage 1 to stage 2 and from A to B, had started spreading, and had gotten to the point where stage 2B is over 4 centimeters as far as the size of the tumor, and then it’s different types of cells. It progressed.
Once it gets to a certain point where it can be very aggressive, I guess it can spread fast. I’m lucky I found it when I did, but it’s unfortunate that it had been in there long enough for it to evolve to that point.

How did you deal with doctors not catching this sooner?
My peace of mind came from the fact that I never missed a gynecology appointment. I never missed a well visit with a doctor. I’ve taken good care of myself. I was going to the dentist when I needed to.
I hadn’t neglected my medical care, so I don’t felt like I shouldn’t have known any different. I love my gynecologist. She delivered both of my children, and she saved my life. I’ve had great physicians as a result of my treatment.
My oncologist is amazing. His staff is amazing. It’s weird to say this, but I wish I could see them forever, even though I know you want to not be seen by them at some point. I really like them.
I didn’t have any ill will or feelings of regret. I feel like I did everything I could have. I’m really grateful that they found it when they did because if it had progressed to the point of having symptoms, I don’t know if I would be at the point where I am now, coming up to my 5-year anniversary.
Diagnosis
Describe the moment you knew you were dealing with cancer
It was at my OB-GYN’s office during my 6-month postpartum pap smear. I could tell during the appointment that something wasn’t right.
She said she could see something that didn’t look good. She called me the same day and actually diagnosed me with cancer before I was a patient of the James Cancer Center here in Columbus, Ohio, but that I’d be referred to them for my treatment plan.
They called me the very next day. I was actually at work. She did labs on the swab that she had taken at my appointment and called me the same day. They rushed it through.
During our call, she said I had cancer. It is so surreal to have someone tell you you have cancer. You feel like, “That just can’t be true.”
I’m really lucky that they found it when they did. I lost my fertility as a result of the treatment. As unfortunate as it is that we found it later, I wouldn’t have had the kids that I have if I had found it earlier, so it worked out in a really weird way.
Did you get a second opinion?
I did not. Things like why I never went into labor and why I never dilated simply started to make sense. I didn’t feel like at that point that I needed a second opinion from my OB-GYN’s diagnosis. It just started to make sense, even though I had no other physical symptoms.
»MORE: Reacting to a Cancer Diagnosis
Why was your reaction to the diagnosis “different”?
From diagnosis, for a year, my mental state was disbelief. It almost felt like I didn’t need to do anything because nothing felt wrong.
It was really hard, and because of my mixed-up results before, I almost thought, “I don’t think they know what they’re talking about. This can’t be me. There’s gotta be a mistake.”
I guess if you don’t feel sick and someone tells you you have cancer, it’s really hard to believe.
I would assume if you had symptoms or if you found something that was bothering you, maybe it’d be a relief to know that what you felt or what you were going through had a cause, but I didn’t feel like I had anything happening.

Describe the mental stress of dealing with your diagnosis
Even sometimes now, going back and talking about [my diagnosis], it doesn’t feel like it happened to me. It’s sad because I feel like the first year of my child’s life, I don’t remember a lot of his milestones or a lot of it.
We were on autopilot, trying to get through day to day.
I do remember my mental state at one point when I had been diagnosed. I knew it was bad. I knew my cone biopsy hadn’t gotten clear margins, but we were waiting to hear back to see what the next steps were.
It was after my hysterectomy to just see what’s the chance that I’m going to be okay. I guess everyone wants to know, “Am I going to be okay?”
This is awful to say, but I was thinking at one point, ‘I have 2 young kids who won’t remember me if I die, and if I’m gonna die, I would rather go quick before they remember things as only being so sad.’
I didn’t say anything to my husband about it, but that’s where my headspace was.
I couldn’t tell anyone because there were still so many unknowns. It just kept getting worse the more we learned about it. I couldn’t talk about it. I couldn’t deal with anyone being upset.
It was really hard, so I would stay in the car, and my husband went to pick up the kids and tell them that it wasn’t good news and I wasn’t coming in. I know a lot of people were concerned. We have wonderful friends and family that tried to talk to me about it, but I didn’t.
There’s an unknown. The time you’re learning about what’s wrong with you, there’s a lot of unknowns and continual tests and things to see, “Did we get it all? What do we need to do next?”
He had never yelled at me, but he did yell at me during that time. He basically told me that I was acting like I had given up and shook me back into remembering how strong I am.
Did you have anxiety waiting for staging results?
In the beginning, I didn’t have a lot of anxiety because I feel like everything happened really fast from the original diagnosis to being referred to an oncologist to getting in for my cone and things just starting to happen.
Those happen really fast, so there was not enough time for me to even process what’s happening, which is why I think I was in denial.
It was the time period between the cone biopsy and knowing about the radical hysterectomy that I started to get depressed, because you don’t know what the outcome will be. You want it to be the best, and you Google it.
We all Google it, and everything on the internet is so depressing and so sad. Every story is about someone who died, so then you’re convinced you’re going to die. The beginning of my mental downfall was that wait for good news.
When you keep getting not the best news, then you start thinking that the next thing you hear won’t be good either. That’s difficult on your psyche.
»MORE: Dealing with scanxiety and waiting for results
How did you break the news to your husband?
I called my husband. I remember calling him from work, and he made me leave work. I was in shock for a really long time. I was in shock and denial for probably a year.
We went home to talk about everything, but I just couldn’t even grasp the reality of it. I didn’t feel sick. I have no issues. I had no problems. I didn’t feel anything different.
It just was very surreal. I don’t know how to describe it. It just felt like what they were saying was wrong.
»MORE: Breaking the news of a diagnosis to loved ones
How did your husband handle the diagnosis?
My husband is an amazing, supportive person and a really wonderful nurse. He has always been really good at processing things, but men internalize their stress.
We joke about it now, but my husband and I had a toddler, a newborn, and a new cancer diagnosis.
As much as he tried to be the rock, he ended up getting shingles from the stress. I’ve talked to some other support people that went through some physically difficult reactions to stress as well.
That was hard because the newborn wasn’t vaccinated for anything yet. Matt had shingles, so we had to keep him away from me and everyone else just in case. It’s funny now, but it was chaos at that time.

How did you approach telling your young kids about your diagnosis?
I probably didn’t handle it the best way, because our kids were so young, under 1 and 4. My husband needed to be at every appointment. Not just because I was emotional, but because I was very stoic for a lot of my appointments.
It’s really hard when someone’s talking to you because you’re processing your feelings, and you’re not always able to take in the information.
It was nice to have my husband there because he, even to this day, remembers things that they said that I just didn’t hear. [It was] not because I wasn’t there.
I wasn’t capable of receiving information. I was shutting down mentally.
We had family members watch the kids through my appointments. They knew that we were going to the appointments and there were several appointments.
I couldn’t pick our toddler up, I couldn’t carry him, and he couldn’t sit on my lap. He actually still can’t sit on my lap, but we said that mom had germs in her belly. Kids are so innocent. They don’t fear anything you don’t make scary. We used the word “cancer” a lot, but that didn’t scare them.
We just explained to the kids that cancer is like having bad germs they had to cut out of my belly. I still have limitations today, so I’ve been open about what I can and can’t do. The kids don’t see anything differently, though.
That’s the beautiful thing about children. They don’t see ability, disability, color, or anything; they just see who they love. It was harder on me than it was on them to say, ‘I can’t pick you up,’ or, ‘You can’t sit on my lap, but you can sit next to me.’
We found new ways to be close when I couldn’t physically handle doing what I was doing before.
»MORE: Parents describe how they handled cancer with their kids
Was there anything specifically to consider about being a young mother diagnosed with cancer?
It’s difficult being a new mother, period, and going from 1 kid to 2 is a whole new level of stress. Not to mention going through cancer treatment at the same time. There was a lot of adjustment, and I’m glad that I have the family I have. It ended up working out, but it was a tough year.
The first year of my son’s life was a blur between the emotional stress and getting through everything that we needed to. I had to consider an older child getting a sibling for the first time.
You’ve got to make sure that there’s not any jealousy. There was so much going on for everybody emotionally and developmentally, so I’m glad we got through it.
My husband really encouraged me to let them see me cry. We want our sons to know that emotions are healthy. We were pretty open with that piece of it. We made sure they saw that some days are bad and some are good.
Did your doctors recommend any resources for your family?
My oncologist recommended an online calendaring tool. It’s a website where people can sign up to volunteer to bring food, babysit the kids, or take me to an appointment. They can sign up, and everyone knows which days and meals are covered.
That was wonderful because my husband is great, but with a newborn, me being completely immobile, having a toddler and dinner and everything else to worry about — it was too much.
Treatment & Surgery
Describe your cancer treatment center
I was referred to the James Cancer Center in Columbus, Ohio. It is amazing. People come from all over the country to be seen there. I knew I was getting the best care, so anything they said that they needed to have done, I never second-guessed.
It’s enormous. It’s funny because when I started going there, the first thing they would always ask you is, “What hotel are you staying in, and what airline did you use to get into Columbus to be here?”
So many patients are flying in for treatment. They were surprised that I was fortunate enough to live nearby and I could just drive in for treatment. People come from all over, and it’s growing exponentially. It’s an amazing facility, so I’m very lucky that it’s in my backyard and that I have the accessibility to see them.
I can’t imagine the cost that people incur that have to travel for treatment and the inconvenience of being in a car or a plane when you don’t feel well, so I’m very, very lucky. The care was amazing. The staff is amazing.

Any advice on how to choose a treatment center?
You’re in the right place if you trust the advice from the people that are giving it to you and if you like the way they are treating you.
I never second-guessed my care because the people that were treating me were amazing not only in their intelligence but in their bedside manner, too.
If you don’t feel that way, then you absolutely have a choice to be treated by anyone that you prefer, so don’t feel stuck.
My father is a melanoma patient, and he was going to a small country physician. I moved him over towards the James, which is a bigger institution.
What happened at your first cancer center appointment?
They looked at the results from my pap. Ideally, what should happen is the cells come down and you find them. I’m sure they did at some point come down on the one side, and that’s how it was originally found for me. What had happened is it had grown width-wise through my body, not just through my cervix.
It grew through through my abdomen. I had had a CIS cesarean, and we had to postpone my radical hysterectomy for several months because you can’t have abdominal surgeries of that degree so close together.
It’s very dangerous. It was a really weird dance between beating the clock and not doing anything that’s dangerous for my health as a recovering new mom. It was really weird.
What was the timeline for tests and biopsies?
I had my regular pap, then I had the colposcopy. After that, I was scheduled for a cone, which was a day surgery, so I had a pre-surgery visit. I had the day-surgery cone.
I had a post-op visit. Then we had a separate discussion about additional treatment. That’s when we had to do the radical hysterectomy. Then we had pre-op visit for the radical hysterectomy. There was a lymph node dissection and then post-op visit after that.
Describe the colposcopy
I had had a colposcopy before, so I wasn’t really concerned about that. A lot of people asked me if cervical cancer runs in my family, and I say no because that’s true.
However, a lot of women in my family have abnormal paps, and it’s becoming a lot more common for women in general to have abnormal paps.
A colposcopy can be done at your gynecologist’s office. There’s different ways to do it, but they’re burning off some of the cells that your body isn’t naturally shedding when you have your period.
If they can get rid of them and you have healthy cells underneath, then you don’t need anything further. I had that done in the past. There’s a little bit of cramping.
It’s a bit annoying, but it doesn’t take long, you can go home, and you don’t really need anything more than Ibuprofen after it.
How did the staging happen?
I was referred to the oncology department. The way they planned to stage me was by doing a cone biopsy. That’s where they take a cone-shaped cut out of your cervix. Ideally, what they want to get are clear margins. They want to be able to encase the entire tumor and remove it from your body.
I did not get clear margins, so we did the cone biopsy. The cone didn’t contain all of the cancer cells that had gone broader than my cervix. At that point, we were scheduled for a radical hysterectomy.
Describe the cone biopsy
The cone biopsy was more extreme than the colposcopy. It’s done at the hospital, and it’s a day surgery. I had general anesthesia and a bunch of medications. I don’t think I’d ever been put out because you stay awake when you have a cesarean.
That was my first time with general anesthesia, and I had a really embarrassing reaction to it. I woke up in the recovery room in awful pain. It felt like I had squatted on top of a burning fire. It was extremely painful. I had a cold knife cone.
That’s where they’re actually cutting and burning, as part of the treatment, a cone-shaped tissue sample out of your cervix. You definitely wake up feeling awful, and you go home. I had medication, painkillers, and some bleeding, but I was fine within a day as far as the pain is concerned.
The risk for a cone biopsy was that removing any of the tissue in my cervix could affect my ability to hold a pregnancy full-term or even have a pregnancy at all.
That was the beginning for us as far as the realization that everything that was happening was going to affect my fertility.

Any tips for people before undergoing a cone biopsy?
There are things you could probably do that would help. Have a frozen pad or something that people have used when they have a vaginal birth that helped relieve a lot of burning and pain. Had I been prepared, that would’ve been great, but I had no idea that it would be that painful.
How did you decide on the radical hysterectomy?
The thing that stands out to me, which was odd, was you expect your doctors to tell you what you have to do, and they don’t. They give you a whole bunch of options, and they let you pick your method moving forward.
I had had the initial things done already that would have made it more difficult to hold a pregnancy, but it didn’t mean we could never get pregnant.
My oncologist had said, “If you want to have more children, we could try to salvage your fertility and do a partial hysterectomy. That’s where they try to take half of your uterus and cervix, and you would potentially be able to still have children.”
When you say you had a hysterectomy, there are stages of it. A radical hysterectomy is the most extreme type of hysterectomy they offer. I remember being in his office, and he had this piece of paper.
It had the outline of a person’s body and a medical diagram of the internal reproductive organs of a woman. I remember him circling when we had said, “What’s the radical hysterectomy?”
He circled 6 things. It was like, “We’re going to take this and this and this and this and this and this.” I remember thinking, “That’s a lot.”
You want them to tell you what you should do, but they don’t want to make decisions for you. They’re like attorneys that way, which is kind of funny.
My husband, who is very passive and very nice, got irritated and basically had said to the doctor, “If this was your wife, what would you do?”
It was at that point where he said, “I’d be the most aggressive, and we would do the radical hysterectomy.” So that’s what we did, because if he would do that with his family, then that’s probably what we should do for ours.
It’s weird that you pick your poison as far as what you want to put yourself through. You don’t really want to go through any of it, so it’s weird to select your own treatment.
I was basically given the option of, “Do you want to have more kids?” It’s hard to ask the one that just had a baby if you want to have more kids. You’re tired, but you’re thinking, “Maybe I do.”
What was the pre-surgery routine for the hysterectomy?
There were no scans. I know I had to do blood work to make sure I was healthy enough, but it was a lot of weird pre-op sanitation stuff, full body chemical shower, [and] things to prepare my body for surgery.
I didn’t know if I wanted to give up my fertility, but my husband and I had to make a decision. The best one was the most aggressive treatment plan that would guarantee the longevity of my lifespan to be there for the kids we had.
We went very aggressive with the treatment and did basic amputation of almost my entire reproductive system and all of the muscle tissue surrounding it.

Is there anything you wish you had asked or done before the hysterectomy?
I would just recommend that people bring someone with them that they trust and they love. They can be a sound voice of reason and ask questions.
I didn’t ask any questions. No, that’s not true. I asked one question, and it was really dumb. We had planned a trip to Disney before I was diagnosed. If anyone’s gone to Disney World, it’s like a year of advanced planning, and you pay an egregious amount of money to go.
We were supposed to be going in November. That’s when they wanted to plan my surgery. When my oncologist asked me, “Do you have any questions,” my only question was, “Can I go to Disney World?”
My husband jokes about it to this day that that was my one burning question to my oncologist. I was thinking, ‘Will this be my last opportunity to have a vacation with my children?’
My oncologist did not want me to prolong this surgery for too long, and he explained the risks to us of prolonging our surgery. We put it off for several weeks. It’s not like we put it off for too long, but we put it off for a couple of weeks. We went on our vacation.
I’m glad we did because I’m 5 years out, and flying is still painful. Walking has been painful. There’s a lot of things now that I don’t enjoy, and I definitely would not have been able to do it that close to the procedure. It’s embarrassing, but my one question was, “Can I go to Disney world?”
If there’s something you’re looking forward to or something you want to do, I wouldn’t just assume that you can’t do it beforehand, because those things are very important for your mental health, especially when you’re in a fragile mental health state.
We went to Disney, and it was great. I’m glad we did, but I probably could have asked other questions.
Describe the cleaning prep process
There were 2 solutions I had to wash my body in and a sequence — one and then the other.
It’s localized to your abdominal area. I did the chemical shower at home before the surgery. Then they had me clean myself for surgery while I was at the hospital after I got into my gown. Then when I went into surgery, the staffed cleaned me.
I had 3 antibacterial wipe-downs before they would cut me open. They were on top of it. I remember thinking, “Gosh, I hope they don’t hand me a scalpel and ask me to cut myself open.”
Any surprises heading into surgery?
I remember thinking that we were going to be in and out. I thought it would only be a 5-hour procedure. We took our kids to daycare. We were one of the first surgeries, so we figured my husband would see me right after lunch. We thought we would hang out for a little while, and he’d go back and pick up the kids.
During surgery, I needed blood transfusions. I had a lot of scarring from having a cesarean. I was in surgery for 9 or 10 hours. I would recommend people to be prepared for the worst and don’t expect it to go smoothly, just in case. That way you don’t have to worry about rushing out and getting kids or anything.
Any apprehension about the general anesthesia?
I asked the anesthesiologist to be aware of everything he gave me and to let me know what he could give me that would flush out of my system the fastest since I was a nursing mother.
He said he would need to Google it, and he’d come back with a recommendation. He hadn’t even considered someone needing to get whichever drugs or sedatives are given to them out of their system before.
We had to make a decision before my hysterectomy to stop nursing my child. He was 9 months. Some people think, ‘At nine months, kids should be done nursing by then anyway.’ I nursed my older son for over a year. Just because I had to stop didn’t mean I was okay with it.
My oncologist was worried because sometimes when you stop breastfeeding, you can get an infection in your chest. I had to get that taken care of first. I didn’t want to be in the pre-op room for my hysterectomy and have to pump or be unconscious and have them do it. That was a whole other bag of worms.
Post-Surgery & Recovery
Do you remember having any side effects after you woke up from surgery?
I had never had general anesthesia before. I don’t think I handled it very well. When I had it the first time, I woke up feeling like I had like squatted on top of the campfire.
Imagine someone voicing how that would feel when they’re unconscious. That was embarrassing, but the nurses said it was very entertaining. Witnesses explained to me that I was very belligerent the second time.
was in awful pain. I was on a morphine drip. The nurses needed to come in together and do a turnkey at the same time because the amount of morphine I was on was not something they were allowed to administer individually.
They needed to have a shift manager present to give me the amount of morphine I was on. I don’t remember a lot in the hospital except for being in pain.
I was in a shared room, and my roommate was there for cancer. She had her limbs amputated. She was in pain, and I was in pain. It was awful.

What would you change about your post-op hospital stay?
I would prepare for a longer hospital stay. I knew I’d be in the hospital for a couple of days, but I didn’t think it would be that long.
I had so much scar tissue, a blood clotting issue, and transfusions after my procedure. It didn’t go as easily as we had planned. I was in the hospital for a long time, and my husband stayed home with the kids.
I really wish I had people there 24/7 because as much as the nurses are there to help you, they’re not able to sit with you constantly.
What was the short-term recovery after surgery like?
Pain management was the big thing. There was a lot of pain.
The doctors explained because they were taking so much tissue around my cervix, fallopian tubes, and uterus, my bladder and bowel could go into a medical coma.
If that happens, you have to catheterize yourself. They were going to teach me how to catheterize myself before I went home. I didn’t want to have to do that. I didn’t want to learn how, and I didn’t want to have to shop for catheters.
Luckily, within a day of waking up from the surgery, I had successfully gone to the bathroom by myself. I didn’t have to go through with that process. That was a big win. I had a lot of weakness in my abdomen, and I couldn’t tell when my bladder was full. I had no sensation at all.
I still have issues with knowing when I need to go, but it was completely a problem for only about a week.
Hormones are a big deal. You go through a medical menopause, even if you get to keep your ovaries. You’re going to have night sweats, mood swings, [and] weight gain on a whole other level.
It’ll get better, but for the first few weeks, that was awful. I actually thought originally that I had been urinating in my sleep, but it was just the sweat from medical menopause.
Are you still dealing with long-term side effects?
I’m 4.5 years since treatment. I’ll be at 5 years in November. I had 28 lymph nodes in my groin removed as a result of my radical hysterectomy, which is very common.
Taking lymph nodes is the best way to tell if it’s gone to other organs in your body. As a result, my oncologist told me to look out for lymphedema, which would present as heaviness.
Within a couple of weeks of being mobile, I could tell that my feet were heavy and tired. I had pins and needles, like a diabetic neuropathy feeling. I called my oncologist, and they got me in right away for physical therapy.
They taught me how to do a manual lymphatic drainage massage. They showed me equipment that I could use at home. I started wearing medical grade compression garments, and that helps to reduce swelling. When you reduce the swelling, you also reduce your pain.
They say you shouldn’t use a razor. No hot tub, no sauna, no pedicures or anything that could cut you because you don’t want to get an infection. If you do, it’s really hard to fight it.
In extreme cases, that can lead to amputation or death. Now, I’m very cautious about how I take care of my skin. I used to be a lot more active, and now it’s hard to lose weight. It doesn’t matter what I eat.
I can stop myself from gaining by watching what I eat, but I can’t lose weight because my lymphatic system can’t process fat. They tell you to have a new normal after cancer. That really is the hardest thing — thinking you’re going to feel the way you did before and knowing that will never happen. You need to be okay with modifying things.
Because I had lymph nodes removed and because I have issues with lymphedema, they’ll continue to see me for the rest of my life, but not as much.
I’m out of the risk of recurrence. I won’t need to be under the watchful eye anymore on my 5-year anniversary from my last surgery and treatment without any signs of recurrence in between.
I’ve had no other signs of recurrence. November will be my anniversary, and after that I won’t see them more than once a year.

What was your first follow-up appointment like?
The first sign that it was going to be good news was that we didn’t have the last appointment of the day. They save the last appointment of the day for people who need more time and don’t get good news.
Now I have morning appointments, which is nice. I’ve been going in regularly. I was on an every-3-month check-up program. Then it went to 6 months, and I’m still doing that.
How long after your hysterectomy did you have to wait for follow-up results?
I had been waiting to hear my results for a couple of weeks, and that was my darkest time. Emotionally, that was difficult because I also physically felt the worst I ever had in my entire life. I thought I wasn’t gonna make it because it was too much for my body to go through. Waiting to hear back if the cancer had spread and if I needed additional treatment was rough.
I had scheduled a family photo session, so we did family photos, which my husband doesn’t really like doing. We did the staged outdoor photo shoot. I started writing letters and things I wanted the kids to know because I didn’t know what was going to happen or how much time I would have.
That’s when my husband gave me a come-to-Jesus talk about needing to buck up. I started to come around, but that was probably the hardest time I had. When you keep hearing bad news and you feel so bad, you start to think you’re not going to get good news.
It ended up being okay. I didn’t need any further treatment. We managed to contain all of the cancer. Luckily, I had cancer in a part of my body that I could amputate instead of having to fight it.
I really feel bad for people who have cancer in organs and places on their body where their only treatment plan is to fight it with radiation and chemo.
»MORE: Dealing with scanxiety and waiting for results
What has your experience with post-op scans been like?
I’ve done everything because I am terrified that I’m going to have cancer again and I’m not going to know. I had no symptoms before, so I basically begged my doctor to give me scans.
We did a bunch of scans at my 2-year mark, and we use those as a baseline. I’ll do scans again in the next few months, and we’ll reevaluate them. It was scary to think that could be missing something, so I opted for more scans.
We did brain and chest CT scans. My brain, chest, and abdomen were my biggest areas of concern as far as recurrence since brain and lung tissue are very similar to cervical cancer tissue. Also, my bladder and bowel area since those are so close to what I had dissected.
We couldn’t do it all at once. For one, you have to drink dye. In another, they inject you with dye. It’s this whole process, and I did not feel well after having the dye injected.
Because of my lymphatic system lagging, it was more to flush out. The big picture is why we’re doing it, though, so we went through with it.
I’ve longed to find people that have a similar story. I get that feeling. You want to meet people so you’re not alone. It’s nice when you do, but it’s also awful because a bunch of people at my stage of cancer have had recurrence.
Did you ever have to self-advocate?
I have a really great doctor, and he’s never withheld information from me. As time went on, I asked a lot more about recurrence. That’s my biggest fear.
He outlined things I could do to ease my fear, but informed me they weren’t insurable. He said he understood that I didn’t care what would be covered.
It really opened up a lot of doors to information.
Now, I see a vascular surgeon, as well as an oncologist. The vascular surgeon has helped me with pain management.
I pushed for post-surgery scans. My doctor wouldn’t have recommended them because insurance didn’t cover it. We’ve gone above and beyond what is insurable as far as some of our tests and appointments and therapies, but it’s been beneficial to me.
»MORE: How to be a self-advocate as a patient
Do you have a message to patients and caregivers about being their own advocates?
There’s no such thing as a stupid question. Don’t be afraid to ask anything.
Make a list of the things that cross your mind to ask. It’s easy to forget in the moment what you wanted to know, so making a list helps you get the most out of your doctor’s attention.
How did it feel to realize you would lose your fertility?
Being 30 and diagnosed with cancer after having had a kid in the same year and then being told, without making the decision ourselves, that we couldn’t have any more kids was really difficult.
I also had an identity crisis moment, where I felt like I lost my femininity. My sense of self. Now, years later, I’m really glad I don’t have to buy anything from Tampax anymore.
But at that point in time, I felt like less of a woman, which is really absurd for some people, I’m sure, but it makes to those going through it.
I can’t imagine how women that have a breast removed from a mastectomy feel. I joked at the time, “I’m just one of the guys now.”
My husband was very in tune to how I deal with my feelings and never let a joke like that pass without reassuring me that I hadn’t lost my femininity as a result of treatment. That’s something that’s really heavy. There isn’t a lot of attention paid to the mental self-image after treatment.
My power came when I asked myself, “When my kids look at me, do I want them to remember me as someone that tried their best, or do I want them to see someone who gave up?” I still use that today.
Having them and knowing they’re watching and imitating things I do forced me to be a better version of myself. It would be really hard if you didn’t have a family or friends or a support person there who you wanted to live for.
For people who don’t, I really hope that you find the strength in yourself to do that, because it’s definitely worth it. You’re in control of how you react, and that’s really important.

Have you found your “new normal”?
I’m still dealing with that. Sometimes you’re over it and want whatever is still difficult to go away. When it doesn’t, some days are hard, but it’s a process. I think as time goes on, it gets easier. It hasn’t gone away, but it’s getting easier.
For example, mobility is a problem for me sometimes. I try my best to be active. I work in a sky-rise on the 18th floor, so I take the stairs up to my office every day. I started that in moderation.
I worked my way up to it, and I’ve been doing it for more than a year. It’s my way of doing something that is physical that challenges me and makes me feel like I can do something that no one else can do.
I can’t be on my feet all day, though, and I had to get a handicap parking pass recently. I almost cried at the DMV because it felt like I was giving in or accepting limitations.
My husband has reassured me that I’m not. I am disabled in some ways, and there’s nothing wrong with taking the steps you need to push yourself to your limit but not over it. I’m still learning the best way to handle that process.

Did you need outside help with your kids?
We had a really great daycare program, so we tried to keep every day normal. My kids really like a routine, and we kept the routine. That made things a lot easier.
The worst thing is for them to not be around you because they know if something’s wrong, so we didn’t send them away to stay with anyone or anything.
Do you have specific advice for a parent who is undergoing cancer treatment?
Hang in there. It’s hard because it’s hard, and it’s hard because being a parent is hard. Try not to fear the worst and try not to do too much to prepare for the worst.
I look back now at that family photo shoot we had. We have some of the pictures hanging on the wall, and all I see when I look at them is the photo shoot that I thought would be the last time I ever saw my kids and my husband.
It’s really morbid, but that was my mental state at the time. It gets easier. Time does heal all wounds. You’ll grow from your experience in a positive way, but it’s hard.
»MORE: Parents describe how they handled cancer with their kids
How did your treatment affect your work?
I had a difficult situation because I had been on maternity leave, and my employer at the time didn’t want me to take time off for medical leave because of that.
I obviously hadn’t planned on having a baby and cancer so close together, so that was a problem. I ended up taking the time unpaid. When I went back to work, it was good to feel like I was doing normal things again.
Don’t sit at home too much because you’ll think about everything. It will drive you crazy. Don’t be on the internet too much because you’ll read bad stuff. Working was a good distraction for me.
»MORE: Read more on how others dealt with work after a cancer diagnosis
How did you deal with the financial aspect of treatment?
It’s expensive. Insurance doesn’t cover everything. Don’t be upset about asking for help or making changes and scaling back. What you’re going through is temporary, and you can put all of your resources towards it.
There are a lot payment programs offered by the hospital and even non-profit organizations that help cover treatment. I didn’t need that for mine, but I know they’re available.
Talk to your doctor if you have any concerns, because that really shouldn’t determine your treatment plan. I can’t imagine people that have to consider what the bill will be before they would do what’s best.
How did you change your lifestyle after surgery?
I couldn’t find anyone who sold fashionable, medical-grade compression wear in the Columbus area, so I’ve started my own business.
I sell medical-grade clothing, and I can be my own resource for that. I’ve trained in lymphedema and vascular issues to know the best preventative care treatments.
I’ve done medical studies including a nutrition-based medical study about reducing your risk of recurrence. I’ve changed my diet and my lifestyle and done everything that I can to live the best and longest life that I can.
Mental & Emotional Stress
What about your cancer experience was most isolating?
Friends stopped really talking to me. They stop telling you the juicy things about what’s going on in their life because they feel like what you are going through is so extreme.
In a sense, it’s kind because they’re trying to save you from additional stress, but it becomes isolating when people stop talking to you about what’s happening in their life. Then it feels like when you’re not hearing about other people, you start thinking that you’re the only one that has issues.
I had to put my foot down and tell my friends if they didn’t tell me about their bad boyfriend or their fight with their husband or their bad day at work, I was going to lose my mind.
That was helpful. When people treat you different or when they feel bad for you, it makes you feel bad for yourself, so that’s hard.
»MORE: What kind of support cancer patients say helped the most
What caused the most emotional and mental stress?
The fear of not having more kids and the fear of the cancer coming back and wondering how much time I have here. Nobody knows. You have to learn to be okay with who you are and know that these things don’t define you.
They definitely change you, and they changed me in a good way. I enjoy things that I probably wouldn’t have before. If I hadn’t gone through this experience, I would have naively blown through my younger years and not appreciated the little things.
There’s another thing I went through, which is survivorship guilt. When you hear about stories of people that didn’t make it or when you hear about other people’s treatments, you feel like, “I only had surgery, and I didn’t have chemo,” or, “I only had radiation; I didn’t have this.”
You have this guilt telling you that you shouldn’t talk about your experience. I had that a lot. I would tell my husband that I felt too cancer-y for my normal friends, but not cancer-y enough for the cancer crowd because I didn’t have chemo.
Survivorship guilt, loss of fertility, the sense of new self — all of that was really heavy.
How did you deal with it?
I tried to focus on online groups and meeting people that were similar to me. My doctor’s office had some resources available, which is nice to meet people. Believe it or not, YouTube and Instagram have been good for me as far as finding information. I’ve been sharing information on those mediums and have met people as a result of it. That was really the best thing for my mental health.
Support & Survivorship
How did the cancer diagnosis affect your relationships?
I hate to hear people’s assumptions that because you’ve been through cancer and you’re married, you must have the strongest marriage. In theory, saying you’re better off after having gone through it together sounds nice, but it was extremely difficult.
My husband is a very level-headed and kind caregiver. This whole experience forced him to imagine me not being around, and that caused a lot of depression and anxiety for both of us.
It changed us and what we worry about. We’re too young to worry about the stuff that we worry about, but as much as we’re together and we’re strong, I feel like we would have still been strong had we not gone through it.
When I was weak, he was strong, and vice versa. We took turns, but I think it’s harder for the support person because he remembers everything, and I do not. Between medication and the shock of it, I’ve forgotten things, but he hasn’t, which is sad.
Sometimes I feel guilty for putting him through it. I shouldn’t accept fault for it, but there is some guilt to think that we had to go through that so young and together.
It’s hard recognizing when your spouse needs to talk, especially if they won’t talk to you. It’s the same situation with friends who don’t want to share their feelings with you because they don’t want to bring you down. Making sure that they have someone they can talk to is important.
My husband has admitted to me things he thought that were really negative. I’m glad I didn’t hear him say them. He seemed so positive. That kept me positive, but he needed to talk to somebody.
He internalized a lot of it, which is why he got shingles, and that’s not good. Don’t internalize your feelings; they’re going to affect you physically and mentally.
Do you have any advice to other patients on how to ask for help?
If I learn how to do it, I’ll let you know. I’m still having that problem. It’s hard. I think it’s even harder for moms to ask for help. It’s hard for people who are trying to prove to themselves that they’re still who they were.
My husband is very in tune to my limitations, and I’m really fortunate that I have him. I have friends and family and even coworkers in my life that are aware and can recognize the signs when I’m pushing myself too far.
Surround yourself with good people, [and] not just because it’s nice to have help. If you’re around good people, then you’re in a good place.

What do you wish you could have told yourself at the beginning of your cancer experience?
It will be okay. You will eventually get to a point in your life where you like yourself more as a result of what you’ve gone through.
You won’t believe it now, but you’ll be a stronger and better version of yourself.
You’ll be a better mother as a result of going through this horrible experience.

Inspired by Kristine's story?
Share your story, too!
Cervical (Adenocarcinoma) Cancer Stories
Kristine M., Adenocarcinoma Cervical Cancer, Stage 2B
Symptom: Tumor found during postpartum pap smear
Treatments: Colposcopy with endocervical curettage, cone biopsy, total abdominal radical open hysterectomy with lymph node removal
...