Bethany’s Stage 4 Metastatic Breast Cancer Story

Bethany achieved remission after being diagnosed with stage 2 breast cancer, at 34. After learning she was cancer free, she started to make big changes in her life including, separating from her husband, moving to Colorado and falling in love.
But not too long after, she started getting severe back pain. After being told she didn’t need a scan, the pain worsened until she finally begged for one. A lower back MRI revealed lesions all over her bones and she was diagnosed with stage 4 metastatic breast cancer.
- Name: Bethany W.
- Diagnosis:
- Metastatic Breast Cancer
- Staging: 4
- Initial Symptoms:
- Lower back pain
- Treatment:
- Chemotherapy
- Radiation
- Maintenance Treatment:
- Zometa (bone strengthener)
- Anastrozole (hormone therapy)
- Ibrance
I just crumpled into pieces… I felt like I did everything… ‘What more do you want from me, life?’
I was so angry. So angry. Now I have metastatic breast cancer, stage 4.

This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Starting a new life in Colorado
It was exhilarating. I felt amazing and just fell in love with Colorado, with the adventure, with nature. I got really connected with a cancer community called First Descents. They work with young adults impacted by cancer and create these free adventure trips. I had gone on some trips with them and it was so fun to connect with young people who were going through cancer.
When I’m in the treatment center, everyone has gray hair and they’re like, “You’re too young to be here.” I’m like, “Apparently not. I’m here. I just felt like I couldn’t relate to people. Same thing with cancer support groups. It was just all older, older people. Finding a younger community, I got to come right into that.



I started dating. I was very scared about dating post-cancer. I dated for fun… Then I met this guy named Tim.
I ended my marriage. I started dating. I was very scared about dating post-cancer because I had so many scars and changes, and I was worried that it might be some kind of baggage, you know? Like, “Oh no, who’s going to love me now knowing that I’ve been through this and that it could come back?” I didn’t live in that fear, but I acknowledge that that’s possible so it was really interesting.
I dated for fun. It was just a fun, playful thing. Then I met this guy named Tim. We met on a dating app, had dinner at this tea house in Boulder, and just hit it off right away. We just fell in love. We met one month before the COVID pandemic, which was hilarious.
If I’m going to be with someone, I need to be with somebody that I can really enjoy life with, especially when things get hard because they will get hard. That’s just life. Some other curveball will happen so I need someone that can make it fun, make it silly because I can do that. I need a partner for that, too.
Going into a pandemic was perfect for us. We had a freaking ball. We hunkered down together. We danced all night. We cooked amazing meals. We watched movies. We just made it so fun and just fell, fell, fell for each other.
We had been together for a little over a year and we moved into our first home together.



If I’m going to be with someone, I need to be with somebody that I can really enjoy life with, especially when things get hard.


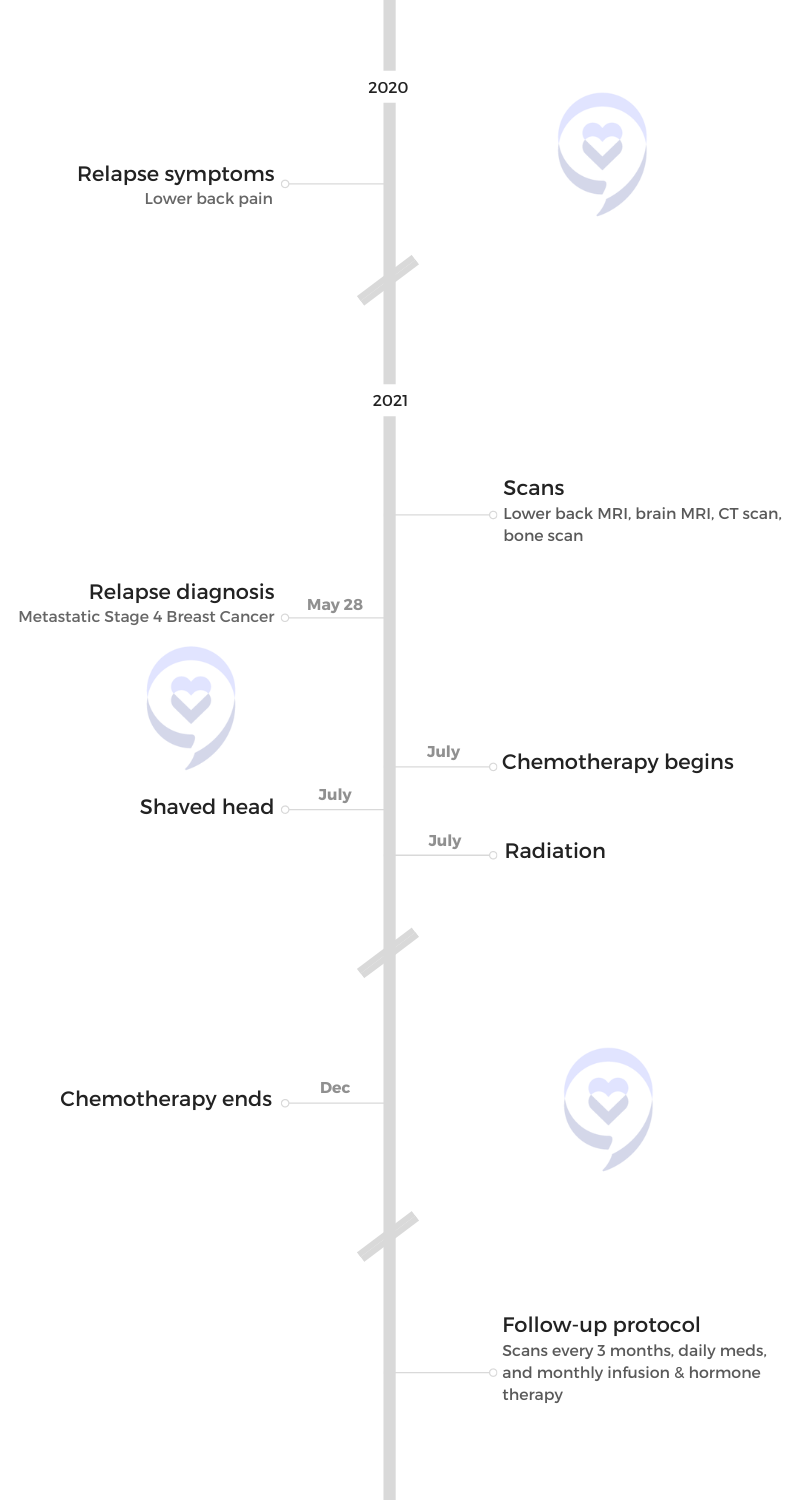
Relapse
Symptoms
I started having [lower] back pain. When people are in remission, every new pain, new symptom, new anything, your mind [goes], Oh my god, it’s cancer. It’s cancer. You got to talk yourself out of a lot of those things. But for me, if it’s consistent like it lasts over two weeks, definitely take it to the doctor.
I called my doctor right away when I started having pain. I took my boyfriend to meet my family in Florida and we did a handstand contest on the beach with my nieces. We wanted to get [a] photo where all of our feet were up at the exact same time so we took a million photos and did a million handstands. My back really hurt that night.
The next day, I was like, “Oh my god, I’m getting old.” By the time that trip came around, I actually was wondering if I needed a wheelchair at the airport. It was so much pain.
When people are in remission, every new pain… your mind [goes], Oh my god, it’s cancer. It’s cancer.
Pushing for a scan
I called the doctor. They’re like, “This sounds like an injury. I think you’re fine.”
I had a follow-up appointment three weeks later. I was limping and they’re like, “You know, 90% of people have [lower] back pain.” I’m like, “Are you sure I don’t need a scan?” And they’re like, “No.” I’m like, “Okay, okay.”
I asked my OB-GYN, “Maybe I should get a scan.” I just kept asking everyone and no one thought I needed one.
I went for chiropractics and yoga and tried to heal it. It kept getting worse to the point where it was so difficult to walk. Some days it would be okay. Because it wasn’t constant, they ruled it out as a recurrence.
Well, I had enough. Again, I hit that same “Enough!” moment and I’m like, “I need a scan. I don’t care. I’m getting the scan.”
I found a spine specialist. He finally ordered a scan. Insurance declined to pay for it because they said it wasn’t medically necessary.
At that point, I’m five years out from cancer and being pronounced physically cancer-free, and I’m like, “But I’m a cancer survivor. What do you mean?” They said, “Okay, fine. We’ll pay for it after you do six weeks of physical therapy.” So I do physical therapy. Later learned that it’s probably doing more damage to my body than healing. It certainly didn’t help.


I finally got a [lower] back MRI. At that point, it was really screwing with my adventure plans in Colorado. I was like, “I just need to know what this is so I can heal it. I want to rule out cancer, but I just need to know what it is.”
The doctor called me two hours later and I was at home alone on the couch. He said, “Are you sitting down?” I’m like, “I am now.” And he said, “We found lesions all over your bones.” I didn’t know what lesions were like. “What was that? Is this cancer?” He’s like, “It appears so. You need to call your oncologist right away.”
Reaction to the possibility of a relapse
I just crumpled into pieces. That’s stage 4.
I felt like I did everything. I did all the treatment. I even wrote and published my book. I tried to help people all my career. I was coaching clients. I have classes that I run and I was like, “What more do you want from me, life?”
I had a PET scan and found out it was in my liver [and] all over my bones. You couldn’t count the spots in my liver. Also in my lymph nodes and my stomach.
I was so angry. So angry. Now I have metastatic breast cancer, stage 4.
I have [a] new medical team in Colorado, but I have humans and while they definitely messed up on the scan part, they were then all over my care.
It was in my liver [and] all over my bones. You couldn’t count the spots in my liver. Also in my lymph nodes and my stomach.
Treatment
I did not want a timeline and they didn’t give me one. They’re like, “This is treatable for many years.” I’m like, “Curable?” They’re like, “It’s not curable.” I know [there are] new medications and everything so I still hold out hope for that but, right now, I’m [accepting that] I am on treatment for life until I’m shown differently.
Going back into that world was absolutely crushing at first. I kept it quiet in the beginning. I was such a big sharer before, but I was like, “I need to work through this on my own first. Just my family and my people.”
At the time, my partner [and I] were only a year in. I’m like, “You are free to go. This is the hardest ask of anything. No one’s going to blame you.” I tried to give him every out and he was just like, “I am so in this with you.”
Everyone rallied. It was just beautiful. I had this moment where it was like, “Okay, you know what? This is happening. Whether I like it or not, it’s happening.” And so that turned on that thing in me, that was like, “Make the best of it. It’s happening.” It’s really what I believe. Live life in every way possible. Not to wait on things that [I] really want to do and just embrace what’s in front of me.
I’ve been living with stage 4 cancer for a year and a half, and I went back into chemo. Two new chemo drugs did a really good job of shrinking things.
I know [there are] new medications and everything so I still hold out hope for that but, right now, I’m [accepting that] I am on treatment for life until I’m shown differently.


Maintenance treatment plan
Now I’m on a maintenance treatment plan. I get a monthly infusion, a shot in my butt for hormone therapy, and then daily pills. It’s really manageable.
How often do you have treatment?
I go once a month. I make a very ridiculous reel every time I go in, which distracts my mind and makes it silly and fun. The infusions, the bone strengthener, it’s called Zometa.
I have a hormone therapy pill I take every day. It’s called Anastrozole.
I’m on a medication called Ibrance — that’s three weeks on, one week off — and that’s what knocks down my immunity. [Sometimes], I have to take an extra week off because my immunity is too low to continue that one so it’s a little bit of a dance with that one. It’s all working.
I also do acupuncture and massage. I eat as clean as I can, but whatever I’m eating, I’m going to love it and that’s more important to me than being super strict and crazy with food.
Side effects from treatment
With treatment, there are some side effects. They’re very manageable. I’m very immunocompromised. Fatigue and low immunity are the two main things. I learned to let my body rest and not push it. Some days, I can do so much. It’s like, “Yeah!” It’s very exciting. But I’m very much living in the present moment.
Follow-up protocol
I get scans every three months and so far, so good.
My scans are phenomenal. I’ve had no new growth and I’m really grateful for that. I know it can change. I’m aware of that reality, but I’m trying not to live in the small world of that reality as well. I’m just like *fingers crossed*.
I follow people [who’ve been] around 10, 20, 30 years, and I’m like, yes! I’m going to soak my mind in those miracle stories because that’s what makes me feel good and empowered. I’m well aware of the other ones. It’s medicine for me. It’s mental medicine.
Live now. Live here now. Appreciate being here now. I would not have that perspective if it hadn’t been for cancer. I’m now in year seven of being in cancer treatment and I’m living a really, really beautiful life that I love. And so I love sharing that with people as well.

If something feels off and not right, speaking up is so important.

The importance of self-advocacy
It’s hard to hear that inner voice because you’re not quite sure. Is that my inner voice or just my fear speaking? If there’s any inkling, it is worth your peace of mind to get it checked out.
In my case in breast cancer, they stop scanning you when you’re pronounced cancer-free. I actually asked for a scan at the end of treatment. They did it but then they didn’t scan me again. I would demand a scan every year. Some doctors actually do that so I’m a little confused [about] how that works. But I would want at least an annual scan for your peace of mind. Your peace of mind is so worth it.
I would have demanded harder for [the] scan for the [lower] back pain. I would have said, “Listen. If the doctor said no, I need you to write in your notes that you’re denying me a scan right now that I’m requesting.” It’s a little bit of a power play, but do it because they’re liable for that and then that’s in the notes, that’s in the records. If something feels off and not right, speaking up is so important.
When my mind is clear, I’m at peace. I’m open. I’m asking better questions. It’s easier to make decisions… I can do that from a place of empowerment rather than panic.
Just getting answers is important. I’ve had to advocate [at] the beginning of my stage 4 treatment, too. I wasn’t getting called back. It was so confusing. Finally, I was like, “I need to talk to a manager now. This is stage 4. This is my life and I need to know that you guys are on top of this.” And she was wonderful. She [talked] with people and then all of a sudden, I did get a callback right away.
I recognize the medical system is busy. They’re so overworked. This was also [during the] pandemic. I was in a pandemic getting stage 4 cancer. So I have to be aware of that but also take care of myself the best that I can and also take care of my mind.
An advocate for my own mind, my thought patterns, what I’m feeding my mind, and what thoughts are running in there. If they are fearful and stressful [thoughts], I really do bring them to that practice of inquiry and question them so I can have a clear mind going into this process.
When my mind is clear, I’m at peace. I’m open. I’m asking better questions. It’s easier to make decisions. It is easier to do research if I’m not in agreement with something I’m hearing. I can do that from a place of empowerment rather than panic, which I’ve done both. Definitely experienced both but one way is a little more fun than the other.
Speak up and take care of your sweet mind and emotions. We’re going to go all over the place. It will be [a] roller-coaster [at] times as well. Falling apart is such an important part of healing, too. We’re letting those emotions flow through and out of our bodies. It’s not bound up and stuck in there then and that’s so healing as well. I really welcome grief. It’s so natural and necessary in the healing process, too.


Living with stage 4 cancer
Within a matter of months, my [lower] back went from it hurt to walk to actually [being able to ski]. I remember getting on the mountain for the first time. I didn’t know if I’d ski again. I thought I might be in a wheelchair. I was just so grateful.
I went skiing. I can hike. I’ve been paddleboarding. I traveled to Costa Rica with my mom. We had a really fun girls’ trip. I got to be there for the birth of my nephew. So many magical, amazing things have happened that I’m like, “You know, this is not what I thought stage 4 cancer would be like. Yay! Oh my gosh, I can still have a great life with this, too.”
Now I’m really, really passionate to keep living, period, and keep sharing and helping others. It’s giving me this amazing sense of purpose. I got to record the audio version of my book as well.
Everything is shrinking and disappearing physically in my body. I very much hope it stays that way. I live in cancer land so I know so many people and my friends are passing away. They’re dying and that is the absolute hardest part of this. [They’re] good people who are making all the right decisions and have great mindsets, too. For some reason, their bodies aren’t responding to treatment and it’s heartbreaking. I think I’ve lost 14 or 15 friends in the [span of a] year and a half and each time, it does not get easier. It just breaks me. And that’s going to be part of my journey.
The longer I live, the more I will see that so I just think: how can I honor them? How would they want me to live my life? They wouldn’t want me to live in grief and crying, but I am going to cry for a bit and then I’m going to honor them by living it up. They have given me so much wisdom, too. Just hug your loved ones and love your life. You’re so lucky to be here. I really want to keep holding that perspective.
If I look at the statistics — which I don’t, but I, unfortunately, come across. If I’m reading an article or [it’s] Breast Cancer Awareness Month, my whole Instagram feed is full of it and I try not to look at it — the odds are not in my favor to be here for very long. But, at the same time, those statistics are based on old medications.
The medication I’m on right now is newer. I haven’t even entered [the] clinical trial phase yet. It’s not based on those medications. For something to become a statistic, it takes years. Years. So it’s old data. It’s not my body. My body isn’t in any of those stats. I have to bring myself back to reality. It’s like, “You’re doing well. Things are disappearing.”
Even though these nightmares happened, it doesn’t have to always be a nightmare. We think of cancer as a death sentence. I look at it like it’s also a life sentence. Let’s really live life and prioritize the things that [we] really want and not wait anymore.
There’s also that pressure [to] do it all now. I can’t do that. My body can’t. My finances can’t. I do have to work with that part of it as well.

What a gift and a privilege it is to be able to live this work and then share it as well.

Words of advice
I birthed [my book] in between my diagnosis. People ask me, “How are you so positive? How are you enjoying?” Not all the time, of course, but how I find that state of mind is all in this book [as well as] humor, silly stories, and tips. It’s how I support myself now with cancer as well.
I’m so proud of this book. It’s the book I wish I could have read when I was first diagnosed. It’s helped so many people [and] that’s such a nourishing feeling. When I get an email from a stranger that [says], “You totally changed my experience of cancer,” what a gift and a privilege it is to be able to live this work and then share it as well.


Look at what every challenge of this journey is teaching you. It might be to slow down, to advocate, to be more present. It might be to fall apart. It might be to ask for help, to say yes to support. There [are] so, so many lessons in this journey.
I’m not saying that if I would have learned those lessons, I wouldn’t be in this situation. We’re in it. Who knows why, but we’re in it. It’s a way to extract a lot of beauty from it as well. That puts me in a state of gratitude and appreciation for what I’m going through instead of fear and anger. To me, that’s also physically healing, to be grateful. I don’t think it can hurt, that’s for sure.
When she was in her late 20s, Bethany used to find lumps that turned out to be either swollen lymph nodes or cysts that would eventually go away. But that one lump she found, which she decided to not get checked, turned out to be cancer. She shares her story of how her cancer journey began.
Read Bethany’s stage 2 breast cancer story here »

Inspired by Bethany's story?
Share your story, too!
Metastatic Breast Cancer Stories
Deb O., Breast Cancer (De Novo Triple Positive and ER+ HER-)
Symptoms: First instance: appearance of lump that later on increased in size, orange peel-like skin around inverted nipple, persistent ache under right arm; second instance: appearance of lump
Treatments: First instance: chemotherapy, targeted therapy, hormone therapy; second instance: surgery (mastectomy), chemotherapy, radiation therapy, CDK 4/6 inhibitor
Tammy U., Metastatic Breast Cancer, Stage 4
Symptoms: Severe back pain, right hip pain, left leg pain
Treatments: Surgeries (mastectomy, hip arthroplasty), chemotherapy, radiation therapy, hormone therapy, targeted therapies (CDK4/6 inhibitor, antibody-drug conjugate)
Nicole B., Triple-Negative Metastatic Breast Cancer, Stage 4 (Metastatic)
Symptoms: Appearance of lumps in breast and liver, electric shock-like sensations in breast, fatigue
Treatments: Chemotherapy, surgeries (installation of chemotherapy port, mastectomy with flat aesthetic closure), targeted therapy (antibody-drug conjugate), hyperbaric oxygen therapy, lymphatic drainage
Dalitso N., IDC, Stage 4, HER+
Symptoms: Appearance of large tumor in left breast, severe back and body pain
Treatments: Surgery (hysterectomy), vertebroplasty, radiation therapy, hormone therapy, clinical trial
Marissa T., ILC, Stage 4, BRCA2+
Symptoms: Appearance of lump in right breast, significant fatigue, hot flashes at night, leg restlessness leading to sudden, unexpected leg muscle cramps
Treatments: Chemotherapy, hormone therapy, PARP inhibitor, integrative medicine
Janice C., Triple-Negative Metastatic Breast Cancer, Stage 4
Symptoms: Appearance of lump in left breast near sternum, fatigue, bone and joint pain
Treatments: Surgery (lumpectomy), radiation therapy (brachytherapy), chemotherapy
Dana S., IDC, Stage 4 (Metastatic)
Symptom: Appearance of large lump in left armpit
Treatments: Targeted therapy, hormone blockers, bone infusions
Maria S., Breast Cancer, Stage 4
Symptoms: Intermittent but severe pain including a burning sensation on the side of the breast, appearance of a cyst and a lump, abnormally warm and pink-colored breast, nipple inversion, strangely liquid menstrual periods, unusual underarm odor, darkening and dimpling of the nipple, severe fatigue, night sweats
Treatments: Chemotherapy, surgeries (mastectomy, lymphadenectomy), radiation therapy, targeted therapy
- 1
- 2