April’s Metastatic Triple-Negative Breast Cancer Story
Interviewed by: Alexis Moberger
Edited by: Katrina Villareal

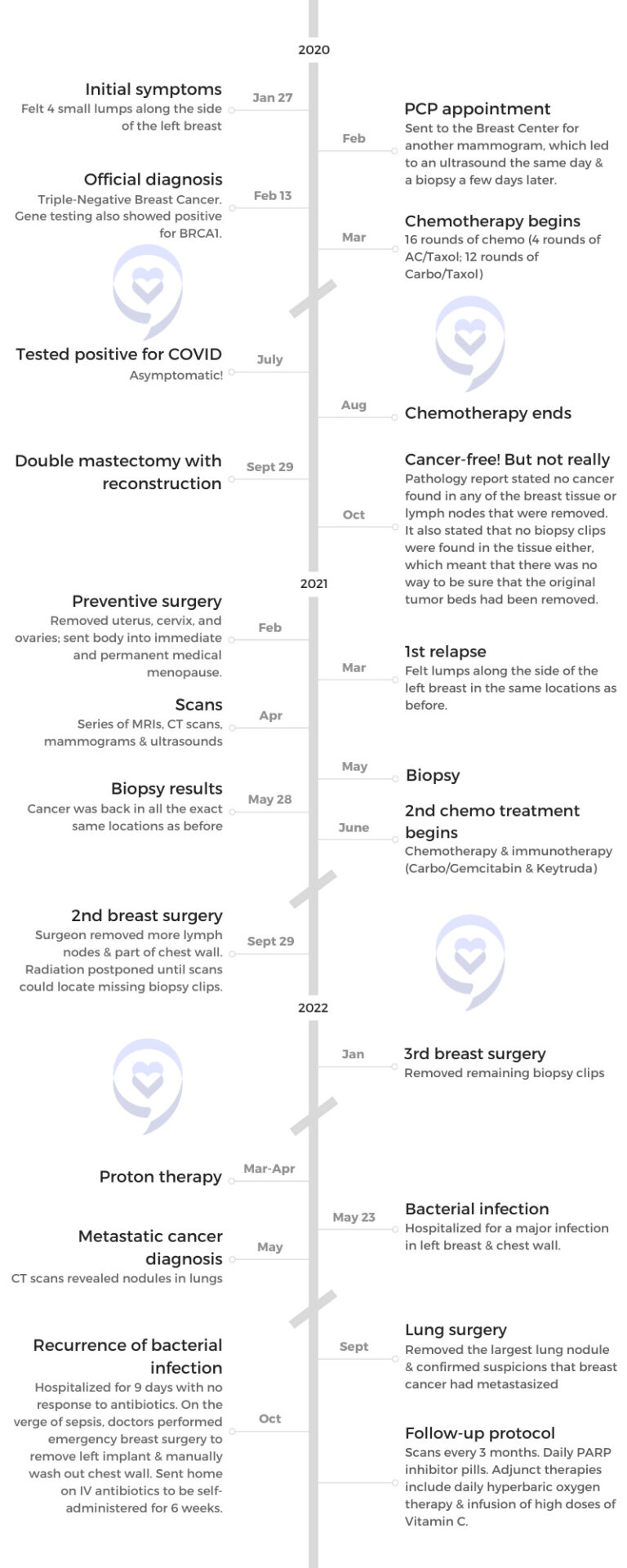
April was diagnosed with metastatic triple-negative breast cancer (TNBC) at age 40, shortly before the COVID-19 pandemic began. She initially found four lumps in her left breast and learned she was BRCA1+ like her mother, who passed away from ovarian cancer.
April underwent chemotherapy, a double mastectomy, and reconstructive surgery. Just 5 months later, the cancer returned and she had to do more chemo and surgery. After finally getting radiation, April was devastated to be diagnosed with stage 4 metastatic breast cancer in her lungs. She has continued to battle infections, side effects, financial hardship, and scanxiety.
Throughout her journey, April has leaned heavily on her faith, grace, and gratitude. She tries to focus on living life day by day, finding joy in her family, and setting future goals. April hopes sharing her story will encourage other cancer patients to have hope and know they can get through this difficult journey. Her resilience in the face of adversity is inspiring.
In addition to April’s narrative, The Patient Story offers a diverse collection of metastatic breast cancer stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- Name: April D.
- Diagnosis:
- Metastatic triple-negative breast cancer (TNBC)
- BRCA1+
- Initial Symptoms:
- Four lumps on the side of the left breast
- Treatment:
- Chemotherapy: carboplatin, Taxol (paclitaxel), Adriamycin (doxorubicin), gemcitabine, Keytruda (pembrolizumab)
- Surgery: double mastectomy with reconstruction
- Radiation: proton therapy

Introduction
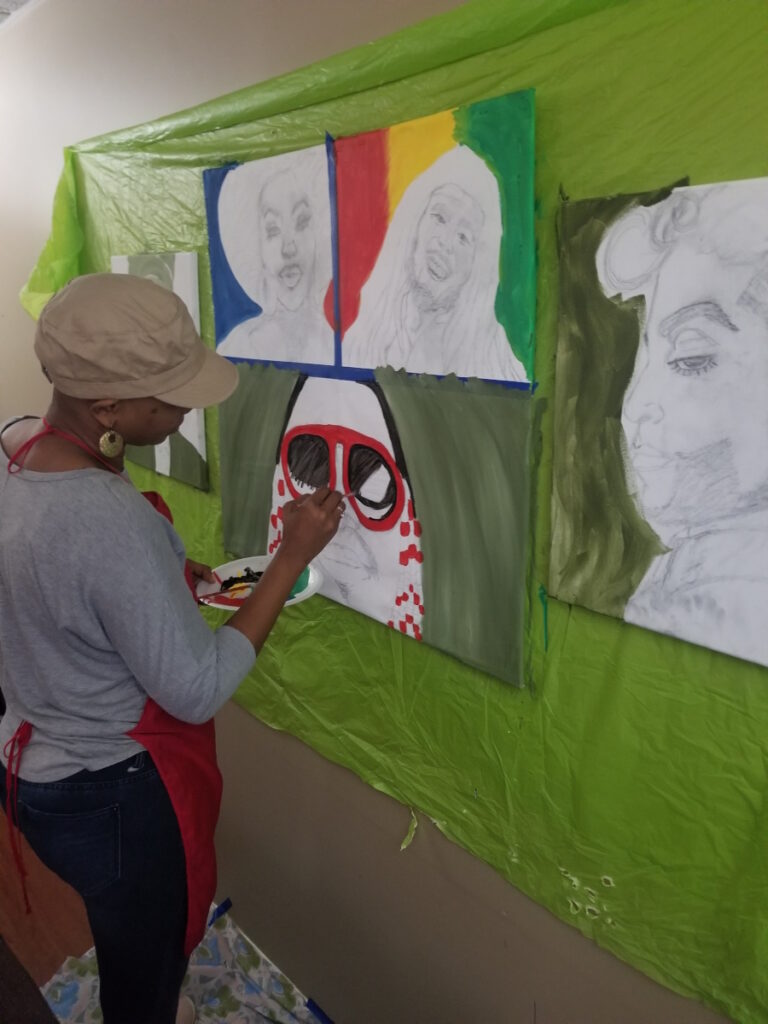
I’m an educator of over 10 years and an author, a mother, and a wife. I love to read, write, and paint.
Most of all, I love spending time with my family, serving in my local church, and, since I’ve been on this journey, being an advocate for other women who are on the same journey that I’m on.
Pre-diagnosis
Initial symptoms
Cancer has been a part of the majority of my adult life. My mother was diagnosed with breast cancer during my senior year in high school. I spent most of my 20s being her caretaker as she went through her journey.
She went into remission. Six years later, she developed ovarian cancer and that was a red flag for her doctors. They did gene testing and found that she was BRCA1 positive. This was back in the 90s when gene testing was just becoming more available.
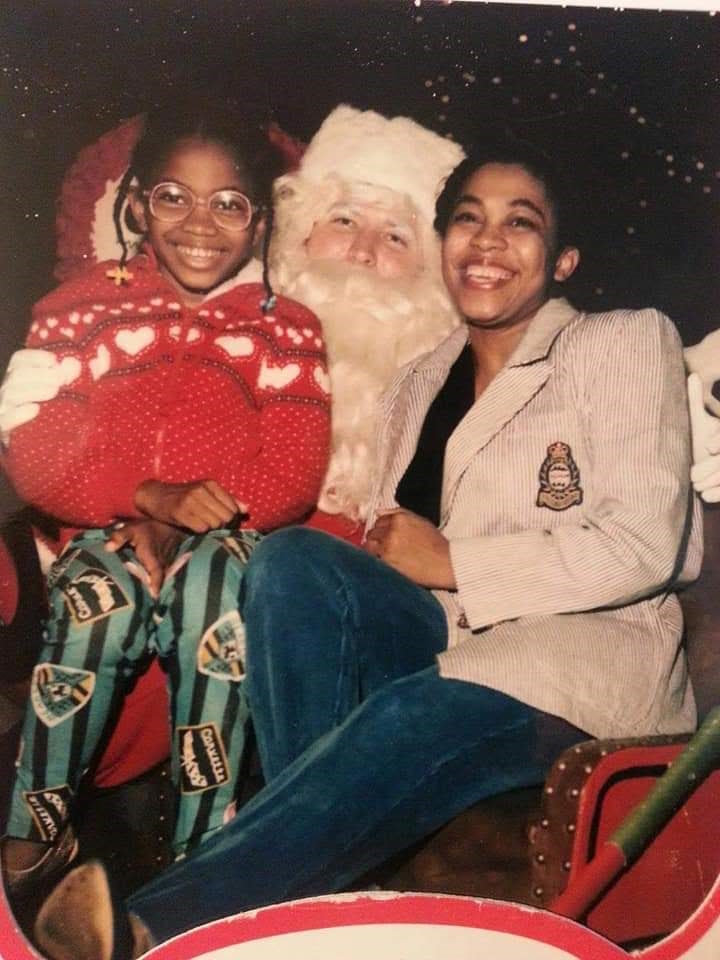
She passed in 2007. They discussed my doing BRCA testing, but the preventative steps were to have preventative surgeries by having your breasts, ovaries, and uterus removed. At that time, I knew I wanted more children. I was early in my career. I was worried about how would it affect my ability to get life insurance and health insurance.
I had a really great OB-GYN when this happened and he said, “Let’s treat you as if you are BRCA positive and, every year, starting at age 26, you get a mammogram and a pelvic ultrasound, and stay on top of this until you have your next child. Then we can circle back around to these preventative surgeries,” so that’s exactly what I did.
For years, I tried to push that fear to the back of my mind. I ended up being blessed to have another child. I had my last son in 2015 and, ironically, my OB-GYN then was a two-time survivor so she was on me. She said, “Okay, you’ve had your child. Let’s get this BRCA test done and start looking at preventative surgeries.”
I did the BRCA gene test finally in 2019 and had my regular mammogram, which came back completely normal. About three months later, in January 2020, while on vacation for my husband’s 50th birthday, I was in the shower doing a breast self-exam. Because of my family history, I’ve always done breast self-exams and been very particular about making sure I know my body, what feels normal, and what feels different.
I felt four lumps along the side of my left breast that were not there before. My husband said, “Okay, don’t worry, we’ll just make an appointment when you get back and get it checked out,” so that’s what I did.
I made an appointment when we got back home. Within a week, I was in my primary care physician’s office. She felt it and was concerned so she immediately sent me over to the breast center. From there, it went from a mammogram the same day to an ultrasound.
The radiologist came in, looked at the ultrasound, and said, “We want you to come back in the next couple of days for a biopsy.” They did the biopsy, which was not a pleasant experience. About a week later, I was getting the call to come back into the breast center.

Diagnosis
Getting the official diagnosis
Ironically, my husband stopped to check the mail and the results of my BRCA gene tests were in. As we drove to get the results of the biopsy, I found out that I was BRCA1 positive.
We got to the breast center and I’m told that I have triple-negative breast cancer, which is very aggressive and fast-growing, which explains why I had a normal mammogram in October 2019 and then had these four lumps appear three months later.
My husband and I were in shock. We sat in the parking lot for about 15 minutes, cried, prayed, and tried to wrap our minds around how our life was about to change.
Being my mother’s caretaker, I was surprised that I wasn’t aware that there are so many different types of breast cancer. I thought breast cancer was breast cancer. I didn’t even realize that there were so many different types.
I was diagnosed on February 13, 2020, right before lockdown.
Treatment
Discussing the treatment plan
I first was sent to see the oncology surgeon. She explained to me all the details of what triple-negative was, that it doesn’t have receptors that a lot of oncologists target for treatment, and how aggressive it is.
The standard treatment for triple-negative was the same for everyone because there were not a lot of treatment options. For all triple-negative patients, it was chemotherapy with ADRIAMYCIN, which we call the Red Devil, a really strong chemo drug that you could only have once in your lifetime because it causes heart damage.
I did the carbo-Taxol-Adriamycin combo for six months and then I would come back to her so she could remove the tumor beds that were left.
She also explained to me that I was stage 2 because even though my cancer was still local to the breast, I had two lymph nodes involved, which automatically bumps you from stage 1 to stage 2, but I still caught it very, very early. It was just because of the lymph node involvement and how quickly it spread.


After surgery, the next step would be radiation. Because of my BRCA, they also wanted to go ahead with the preventive surgery and have my ovaries and uterus removed so that I would not end up developing ovarian cancer. BRCA increases my risk of having breast and ovarian cancer to up to 45 to 80%; the average person has a 12% risk.
The other thing I also learned is that it’s a huge myth that most cancers are genetic or hereditary. Most cancers are not. In my case, if you have the gene, it just gives you that extra tool to be more proactive in the beginning.
It was a lot to digest, particularly for me, because I had watched my mother go through it so I wasn’t going in completely blind. I knew what this was going to look like and I knew how bad it could get. I had to really fight those thoughts and memories that haunted me from being her caretaker and walking with her through the hardest moments of her journey.
I also had to deal with the fact that I had just turned 40. I felt like the year before was the best year of my life. We were doing all these things. My oldest had just graduated from high school.
It was just a shock that, at 40, this was what was about to happen. I was going to have a double mastectomy and deal with having a completely new body and all the side effects of the chemo.
My now eight-year-old was four back then. He needs his mother. Having lost my own mother, I can’t help but worry. Will I be here for him? That was one of my biggest fears. I need to be here for my children and for my husband.
I’m the type of person that I have less anxiety the more information I have. It helps my anxiety. I immediately started trying to educate myself and learn more about triple-negative, all of the treatments, and all of the surgeries.
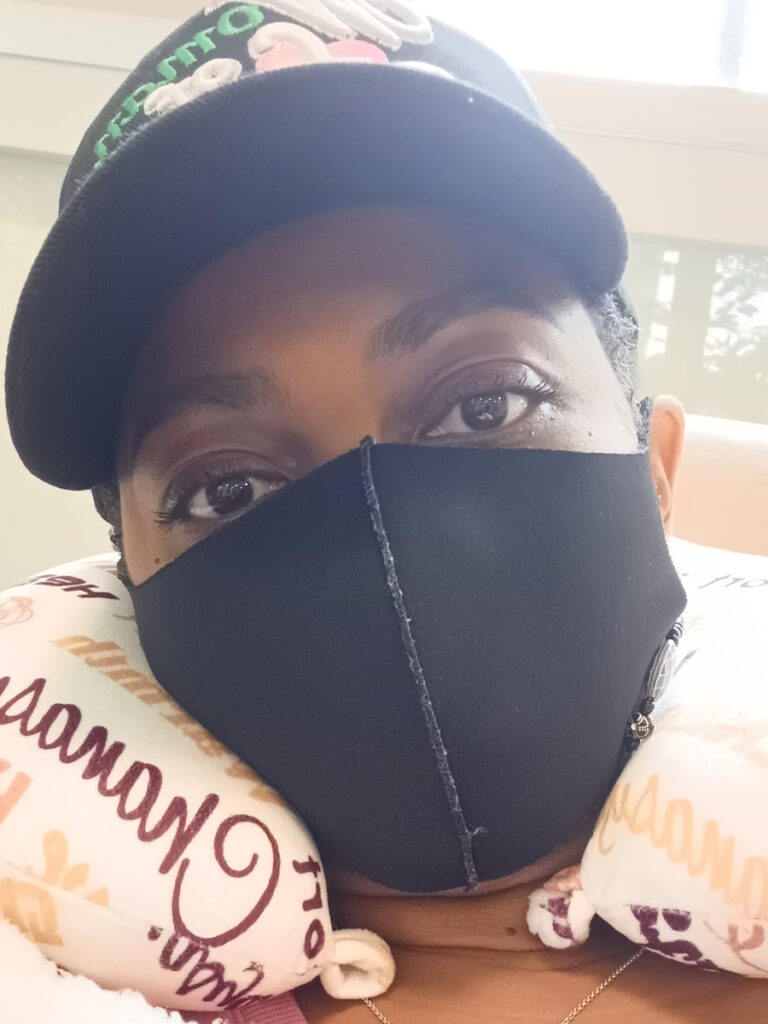
The other fear for me, too, was that it was during the pandemic. I literally started my chemotherapy at the beginning of the lockdown. At that time, COVID was such an unknown. For my treatment team, it was one of their biggest fears.
This chemotherapy was so strong. They’d already told me it was going to basically wipe out my immune system. At a time when you need your immune system the most, they were going to have to completely wipe mine out so they were really afraid of what would happen if I did catch COVID.
My family and I had to be under very, very strict quarantine. Literally, no one left the house unless it was for gas or doctor’s appointments, not even groceries because we were doing deliveries for that. There was a huge fear. I felt like I was having to fight two monsters at the same time, pretty much.


Side effects of chemotherapy
With the Adriamycin and the Taxol, the first thing that happened was my hair fell out. I knew it was going to happen so I made the decision to cut my hair. I didn’t want to see large chunks of hair falling out.
I had a great group of girlfriends who lovingly came over to my house and brought a hairstylist. She cut my hair down to a buzz cut. In their own way, they found a way to keep my mind occupied and make it light and chat with me while she was doing it. They made me feel beautiful no matter what. They loved me and cared for me so much.
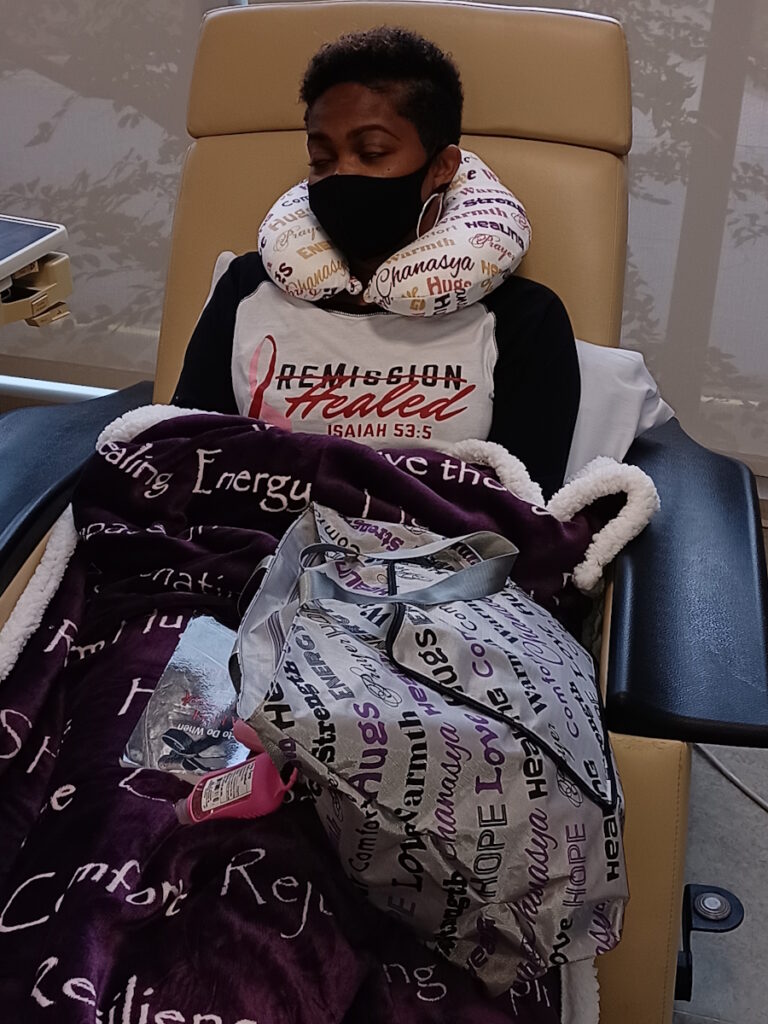
I carried that moment with me when I had to go to the infusion centers alone to remind myself that I wasn’t alone. Just because I was in the infusion center alone, I was still surrounded by so many people who love and care about me and have rallied around me.
After about the third treatment, even with the buzz cut, patches of it just started falling out. My husband ended up just shaving me completely bald.
I also started to feel the really hard hits to my body, which was the nausea. Even though they’ve come a long way with the pre-meds that they give you right before the infusion, I still was very nauseated.
The lining of my mouth, my esophagus, my stomach — everything felt on fire. The chemo attacks any of the fast-growing cells, which are your mucous membranes.
I couldn’t use the same restroom as my family because I’m toxic. I had to worry about kissing or hugging my child. On top of not feeling well, it was mentally and emotionally hard to deal with the side effects of how sick it was making me.
After each treatment, I would spend 2 to 3 days in bed because I was so fatigued. They gave me steroids to help with my appetite because, with everything on fire, you don’t really want to eat.
By the time the three days were over, I’d have two good days to be out of bed and be able to do things with my sons and my husband then it would be time for the next treatment. That became my life for six months straight.

Managing neuropathy due to chemotherapy
The chemo combo that I did could cause severe neuropathy.
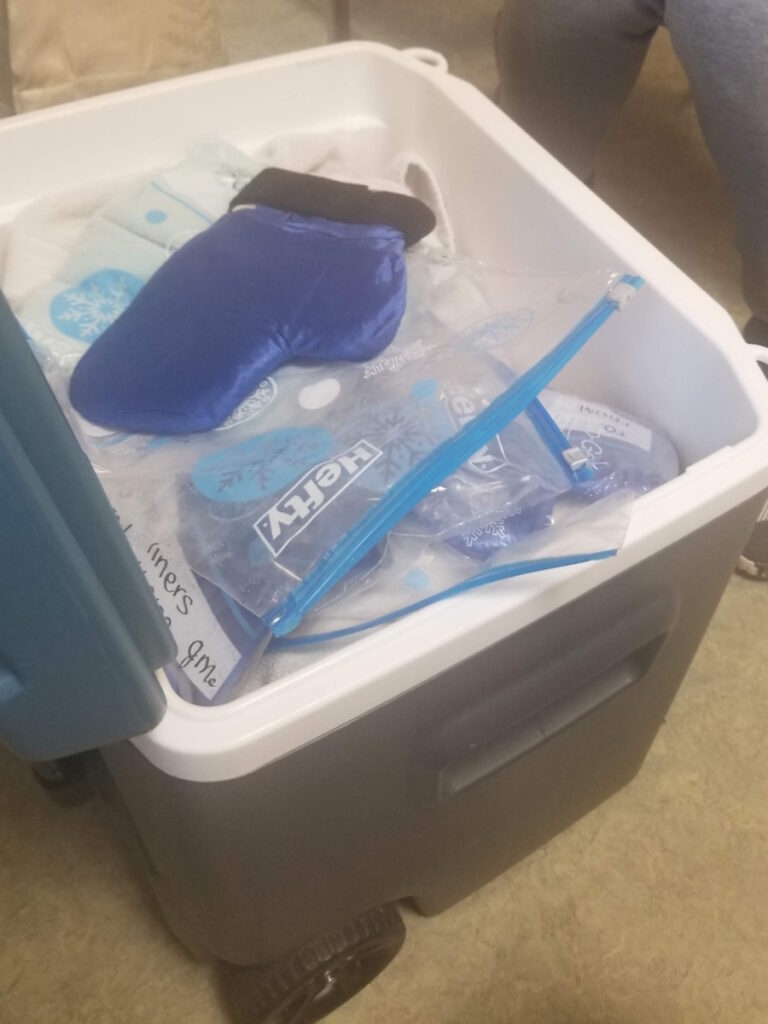
At one breast cancer support group meeting, a survivor spoke about neuropathy and cold therapy kits. I heard that the neuropathy could be so bad that you’d have numbness and tingling so bad that you could lose the ability to button your clothes. There were even women who lost the ability to walk.
I love to paint, write, and create. I don’t want to lose the ability to do those things so it was really important for me if there was a way to help with that side effect to take advantage of it.
I reached out to her when I got ready to start this part of treatment. God bless this survivor. She basically delivered a cold therapy kit, which I had been looking for online. It was so expensive. She delivered this kit that had five sets of gloves and five sets of socks. There’s a special thermometer that has to measure the temperature of the gloves and you have to buy dry ice to go in there because they have to be kept at -15°F.
She delivered it to me and walked me through the process. It was amazing. I’m forever grateful and thankful for that because I don’t deal with neuropathy. I get tingling occasionally, but none of the severe neuropathy that I could have gotten. A fellow survivor was able to do that for me.
Testing positive for COVID during treatment
In the middle of chemotherapy, I ended up catching COVID. I went in to have chemo one day in July and my white blood cell count was too low to get chemotherapy. Then the next day, my whole family contracted COVID.
I initially thought it was a false positive because I didn’t have any symptoms and I don’t have an immune system. This has to be a false positive.
I had to go get tested for COVID every week for a month. I couldn’t go back to the infusion center until I tested negative. For a month straight, I tested positive for COVID. But somehow, by the grace of God, I remained asymptomatic and, to this day, my doctors have no explanation as to why.
It got scary for my husband. Thankfully, we all made it through that. When I finally finished chemo, it was August 2020 and I went to have the next step before radiation, which was to have a double mastectomy.


Surgery
Double mastectomy
When they did the double mastectomy, they also did immediate reconstruction with implants because it was either that or flat for me. They also took out several lymph nodes, not just the ones that were involved initially but several in that area.
Everything they removed, they take to the lab and test it to see if there’s any residual cancer. When I came back for the results in October 2020, everything that they took out came back clear for cancer so that was the best news. That’s the news that every cancer survivor wants to hear and I was super excited.
My surgeon suggested that I leave radiation on the table because, in her mind, there’s only so much radiation that your body can tolerate. She felt like with me being triple-negative and having a high chance of recurrence, that would leave more tools in the toolbox for later down the line, which made sense at the time.
My radiation doctor was not happy. She felt differently. She had her own formula that she called me to go over, but I trusted my surgeon. She was one of the best in the region and sat on a lot of breast cancer boards.
I honestly felt like it was an answer to a silent prayer. That’s one less thing I don’t have to do.
After seeing what my mom went through, I was determined to do everything that my doctor suggested. I was going to follow the entire treatment plan because I have my family to fight for. I wanted to be here for them so I wanted to do whatever it took.
Unfortunately, there was a little part at the bottom of the pathology report that I didn’t pay attention to that said that no biopsy clips were found in any of the tissue that was sent to the lab. Biopsy clips are little metal clips that they put into the areas where they biopsy to mark where they found active cancer cells
In my case, the chemo worked so well. Chemo works really well for triple-negative in that it shrinks the tumor all the way down to where it’s gone and you can’t see it. There’s really no way for the surgeon to see with the naked eye where it was unless there’s something there to be a place marker.
Even if the tumor is gone, it’s really important for them to go in and take out the tumor bed where it was because that’s where the microscopic cells can hide.
I got that pathology report in October. By March, the tumors were back in all the exact same places. Everyone on my treatment team was shocked that they were back so quickly, in five months or less.


1st relapse
Some breast cancer patients are able to get lumpectomies. In my case, from what my surgeon explained, because I had a double mastectomy, they felt pretty sure that they had gotten the tumor beds because all of my breast tissue was removed.
The only problem with that is my breast tumors were along the side of my breast, which was a blessing because it helped me to be able to find them early but it was also why it was important for those biopsy clips to be found.
Also, you have so many lymph nodes in your underarm so there’s no way to know if the correct lymph node was gotten or if there’s no more tumor left behind to see unless you’re counting those clips to say this many were placed and we took this many out.
As a patient, this is something that I’ve been educated about in hindsight. They say hindsight is 20/20. I didn’t know. All I saw was there was no cancer, thank God. I didn’t know that no clips meant that maybe there should have been further investigation at that time to find those clips and make sure that everything that needed to be removed had been removed.
Second round of treatment
I ended up having to go through a second round of chemotherapy in 2021 and another surgery. It was a different set of chemo drugs.
At that second surgery, the radiologist brought it up. She counted the clips and said, “She had this many clips and there were only this many sent to the lab. We need to do some more scans and figure out if there’s still some biopsy clips left to make sure that everything is removed.”
Side effects of chemotherapy
The side effects weren’t as bad. I didn’t lose my hair. I wasn’t as sick. I still had nausea and digestive issues, but it was a lot easier.
They added an immune therapy drug that was approved while I was going through treatment. I started having some side effects from that as well, but they were manageable.
The treatment was shortened because they were trying to get my surgery scheduled and it got moved up. You have to have a four-week break between chemo and surgery.
From that surgery, things spiraled for a bit because the clips were brought up and I had to have an extra surgery to retrieve those clips and that set the schedule back. It was 2022 by the time I started radiation.

Radiation
I was very blessed to get some of these newer options out there. I received a new type of radiation called proton therapy because I have left-sided breast cancer. Your heart sits on your left side.
Proton therapy is supposed to be more targeted and precise so that it can better avoid your heart, your lungs, and other important organs that may not be involved with breast cancer.
I had to go to downtown Atlanta every day for two months.
Side effects of radiation
I did really well. Even though I burned, it wasn’t severe. My skin turned very, very dark along my neck; it still is a different color. It never completely goes back to the original color. But when it burned, it turned very, very dark, dark brown then it started to peel.
Thankfully, because I was constantly putting different things on daily, it was already new skin underneath when it peeled. For some patients, it’s still raw and they have to do antibiotic ointments. I was blessed to not have that severe of a burn.
Compared to all of the other treatments, I have to say radiation was probably the easiest treatment that I had. It’s just that it does do a lot of unseen damage.
You know how when you sit in the sun and get a sunburn but you don’t feel anything and then afterward you get that peel? That’s how radiation felt. I didn’t feel anything. Maybe a little tired or fatigued afterward, but other than that, no major side effects until after the radiation was done.
I started to have side effects from the damage it does to your tissues internally. About two to three weeks after I finished, I ended up in the hospital with a major chest infection.
Radiation damages the tissues and the blood flow so without the blood flow, any normal bacteria that your body would fight off, that tissue can’t fight off. It doesn’t have blood flow, which means the white blood cells can’t get over there and all the things that your immune system sends to defend your body.
After I healed from the radiation, everything looked good. I went on the treadmill to try to get my energy back and get rid of some of the fatigue. When I was going through radiation, I didn’t wear bras because I was trying to be very gentle with my skin. But afterward, I thought it looked good so I put on a sports bra and got on the treadmill for a light workout.
My infectious disease doctor seems to think that because of the friction from the sports bra and because the skin was so thin, bacteria from the sweat got into the chest. I was in the hospital for almost ten days before they could get it under control. They were able to clear the infection. They gave me some really strong antibiotics intravenously.


2nd relapse
Getting a diagnosis of metastatic breast cancer
This was May 2022. While I was there, they were doing scans to look at the infection and saw nodules in my lungs. Initially, I thought this was just inflammation because I just finished radiation.
They did some more tests. The doctor explained that it was very suspicious for metastatic disease and that I was now considered stage 4 with lung nodules.
She explained that the only way to confirm it was to do a lung biopsy. But being in the hospital with a massive infection, I wasn’t in a state to have that done immediately. It was later done in September. I had follow-up scans between May and September.
Initially, they said to just monitor it and see if it grows. That will also be an indicator if this is cancer or not. In August, it showed growth. At that point, they said the only way to be sure was to go in and biopsy.
Surgery to remove nodules
It turned from a biopsy to a lung surgery because most of the nodules were very small. They don’t want to go digging in my lungs so they’re looking for one that was on the edge. The largest one that they felt comfortable to biopsy was right next to my heart. It turned into a surgery so that they could deflate the lung and make it fall off away from the heart.
They ended up taking that entire one out, which was good because it ended up being breast cancer in the lungs. They cut that little wedge out and took out that nodule.
Reaction to the metastatic cancer diagnosis
In September when they confirmed that I have metastatic breast cancer in my lungs, it was devastating. It wrecked us because we were now into year three; three straight years back to back with no remission. We had maybe a month or two here to come up and take a breath. No real relief from this constant fight against this disease. It felt very defeating.
It took some time to process and put it into perspective through my faith and understanding that there is still life after a metastatic diagnosis. It took a while because immediately after I got the results of the lung surgery, the chest infection flared back up, but this time, it came back with a vengeance.


Recurrence of chest infection
It was ten times worse than it was before. This time, I was in the hospital for nine days. They were giving me the strongest antibiotics, but they weren’t working. It got very scary when the antibiotics weren’t working.
My blood pressure dropped down to 40 every day and they could not get it up. That’s when they realized this was going south. This was not going in a good direction.
The surgeon that was assigned to me explained that she was going to have to do emergency surgery to take out my left implant so that she could manually wash out my chest wall and clear out some of this infection.
Thank God she did because she said, “If we don’t do this, you’re probably hours away from going septic. The fact that we’ve given you the strongest antibiotics we have, we’re not going to have anything to help you if you go septic and you can die from sepsis in hours,” and I felt it.
Surgery to clear out the infection
They did the emergency surgery, which was scary because I wasn’t even a year out from the radiation. There’s always a concern with wound healing so they don’t like to do surgery at all on radiated skin earlier than a year, but I didn’t have a choice. Thankfully, she was able to go in there and get out a lot of infection.
When they released me, I had dropped down to 125 lbs. I had to go home on IV antibiotics that I had to administer to myself every day for six weeks to get all of that infection out once and for all.
Adjunct therapies
Hyperbaric oxygen therapy
When I was in the hospital for the second infection, the infectious disease doctor who handled my case had a hyperbaric oxygen therapy center that he also ran. He suggested that I do hyperbaric oxygen therapy, which I had never heard of, ever. Apparently, it was something that he did for a lot of cancer patients who had radiation, especially those who had issues with wound healing.
It was a nerve-wracking experience, but it made a huge difference in healing. When I first got out, my entire chest felt like a statue. It was just so hard and there was just very little blood flow there that it didn’t even feel like flesh. I couldn’t lift my arm. There was so much scar tissue.
I started doing hyperbaric oxygen therapy. The experience with that is a lot like radiation in terms of having to go every day. For two hours, you lay in a pressurized chamber that forces high levels of oxygen into the cells, which forces your stem cells to regrow blood vessels and all these different things.
I did that for 44 treatments over the course of two months. Halfway through it, I started to feel my chest softening. I could feel the blood flow returning. That was the amazing part, being able to see the difference with my own eyes. He felt that would set me up in good standing, in case anything was to ever happen, like another surgery, or protect me against any future infection.
I’ve shared it with every survivor I’ve talked to who’s had radiation. I wish I had known about it sooner, but I’m glad that I was blessed to find out about it.


Vitamin C infusions
I go to a medical doctor to receive high doses of vitamin C by IV. I was 125 lbs. I had no appetite. I was super weak. I couldn’t stay out of bed for very long to do things.
The high dose of vitamin C helped me with the fatigue. It helped me regain energy. It gave me back my appetite. I gained my weight back. I’m up to 149 lbs now, which is much better
It helped with all of the side effects and gave me back my quality of life where I wasn’t weak and in bed all the time. That was an amazing game-changer for me, too.
The only negative side to it is that my insurance didn’t cover it because even though it’s given by a doctor, it’s considered a holistic treatment. They’re now approving certain things like acupuncture but this particular treatment wasn’t on the list so I had to find a way to pay for it myself. It’s been a struggle and continues to be, but it has made a huge difference.
A lot of patients come to this doctor and do it in conjunction with chemo or whatever treatment they’re on. It helps them with the side effects.
Financial toxicity due to cancer
I didn’t realize all the ways that cancer affects you and your family outside of the physical, mental, and emotional. It completely drains your finances even when you have good medical insurance.
There are patients out there who don’t have access to health care. I did have access, thankfully, through the Affordable Health Care Act. I was very blessed that my health insurance covered the majority of my medical expenses. I still had deductibles, copays, and things like that.
However, it’s also the loss of income and not just by the patient. We live in a city where we don’t have a lot of family. We have a church family and friends. They’re a great support, but during the pandemic, it fell on my husband to be my caretaker and take care of the kids. There was a lot of time that was taken away from him being able to earn income as well so we did what we could for as long as we could.
We worked hard throughout our lives to be good financial stewards. We had savings. We had retirement accounts. We did all the “right things,” but this cancer diagnosis wiped all of that out just trying to survive and not being able to go to work. A two-income household and me not being able to work is a whole hit to our finances.

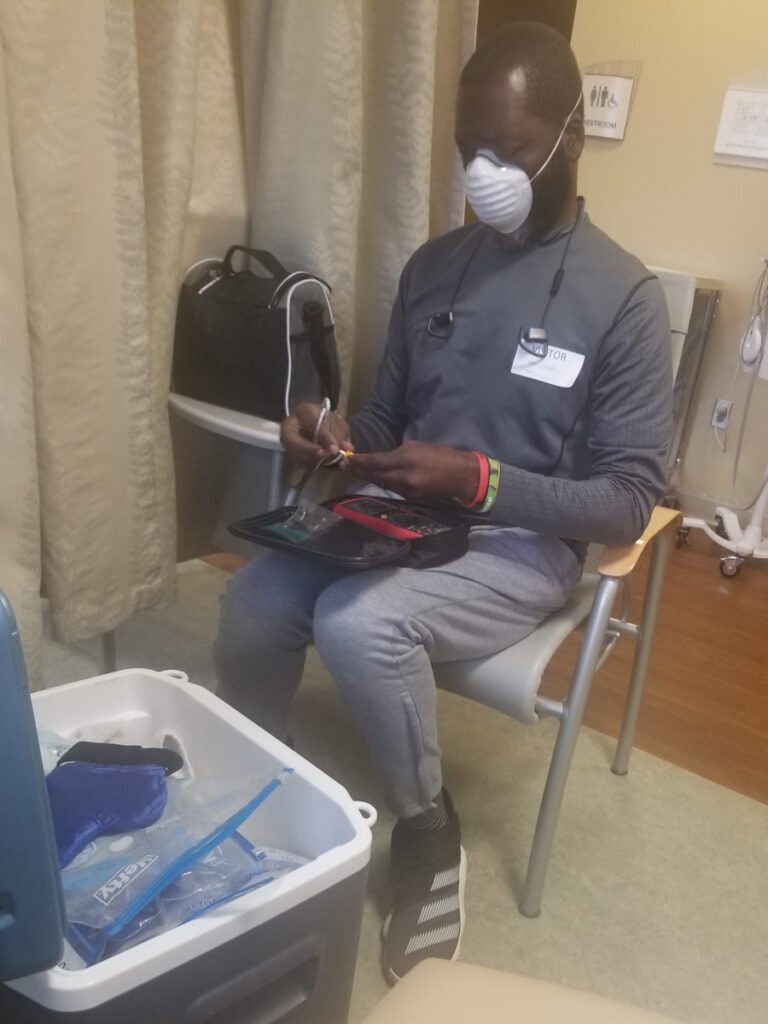
Being unable to work coupled with being my caretaker and getting diagnosed the second time became overwhelming to him. Men handle stress differently. They tend to internalize and he ended up having a massive heart attack.
I can’t help but think that some of that is due to all the stress of being a caretaker and trying to figure things out, provide, and show up every day for his family. We almost lost him. It was a heart attack that they call a widowmaker. He went through his own recovery at the same time.
Now we’re both dealing with health issues and that level of financial toxicity reached a point where we had to make the hard decision to sell our home of 10 years. We raised our boys in that home and all of our memories were there, but it was a decision that we had to make.
We still had to find a way to pay for treatments that I had to have that insurance didn’t pay for. It was just what we had to do, but it was such a hard decision to make.
The last time I got out of the hospital, I had to come home and start packing because we had closed on the house. We had to be out within 30 days after I got out of the hospital. It’s so hard to be dealing with such a horrible diagnosis and then have to figure out financially how to get through this.
Even though there are so many organizations out there for research — and I’m so thankful for cancer research — I have a special place in my heart for the grassroots organizations that are boots-on-the-ground organizations that provide help to patients themselves who are currently on the journey.
There are so many things that you don’t think about. I’m helping the organization that helped me, My Style Matters, founded by Tiah Tomlin, the young lady who got me the icing kits. I’m helping her now with some of her programs and the things that you don’t think about that become a struggle with the diagnosis — school supplies, Christmas, things like that.
They’re not on the priority list, but as a parent, it’s way up on the priority list. Being able to take those burdens off of patients makes a huge difference. It’s all these little things that you just don’t even think about or realize.
Patients are overwhelmed enough. There is a huge need out there when it comes to managing breast cancer patients or patients in general.


Follow-up protocol
It took me a while to recover from the infections to be able to handle treatment. I’m still doing the vitamin C infusions weekly.
My doctor wants to start with a new targeted therapy recently approved for triple-negative breast cancer called PARP inhibitors, which you take daily. She wants to start with the least toxic option since I am metastatic and I’m in it for the long haul for now.
Both doctors agreed that I could do the PARP inhibitor and vitamin C together. It’ll be a mutual benefit because the fewer side effects, the more PARP inhibitor I can tolerate.
My scans have been every three months right now so that continues to be the plan. There have been really good results with this PARP inhibitor, especially for BRCA patients and for triple-negative patients as well so I’m thankful for that.
There are side effects that come with it, like nausea and digestive issues.
The main one is fatigue and severe anemia. It can kill red blood cells, which can cause severe fatigue and anemia. Sometimes you have to have transfusions. My oncologist is very good about titrating, monitoring lab work, and staying on top of those things.
In February, I had a scan that was looking really promising. Everything was stable from August of last year. In February, the scan, everything looked the same as in August, which was great. They actually said a couple of nodules were shrinking so that was great news.
I had another scan in July that said things were growing again, but that’s the nature of this metastatic journey. It’s ups and downs and I’m learning how to not be just thrown off course.


Words of advice
Importance of advocating for yourself
When you get diagnosed, if you don’t have a medical background or you’re not familiar with a lot of the terminology, it’s so important to not be intimidated and to educate yourself.
Google is not a doctor, but it can be a great translator when it comes to some of these medical terms. If there’s something that you don’t understand, ask questions.
Most importantly, read your charts, your notes, and your pathology reports. Don’t just rely on your doctors to tell you what’s going on. Read so that you can understand and be ready with questions.
It’s your body and no one has to live with the results. Doctors are great, but they’re also dealing with however many patients they have coming to their practice on a daily basis. They’re human.
It’s really important for us as patients to educate ourselves and be active members of the team, even though we’re not medical professionals. Make sure you are staying on top of things and understanding things for yourself.
Managing scanxiety
After three years of dealing with this, I had a social worker tell me at the radiation center, “There’s such a thing as medical PTSD,” and I’ve never heard it phrased that way, but that’s exactly what it feels like.
When I go into the infusion center, my body has a physical response to the sight of the infusion center and the smells so there is this high level of anxiety.
I usually manage anxiety pretty well. It definitely feels like medical PTSD because it’s out of my control and it’s an actual physical response.
I dread every piece of information. It’s just information. The doctors are not trying to give you doomsday information. It’s cancer and there’s nothing good about cancer. I do have to mentally prepare myself.


Leaning heavily on faith
I lean heavily on my faith in God, which has gotten me through this journey more than anything else.
Before I go in for a scan, I tell myself, “Today, I feel good. I have my health and strength today at this moment.”
When I walk in, I’m getting information and when I walk out, nothing is going to have changed besides having that information. I’m going to walk out the same way that I walked in — feeling good with my health and strength today.
I try to focus on today and take it moment by moment. There’s a scripture that says that God gives us enough grace and mercy for today and the future belongs to Him so I try to rest in that. Today is what I have and it’s a gift.
There are three things that I’ve used to get me through this and they have become my mantra and that is faith, grace, and gratitude. Those have helped me get through this journey in my hardest and most difficult moments.
I try to tackle everything from a place of faith and not fear. I try to give myself and others as much grace as I need and as they may need. Always try to find a reason to be thankful every day, every moment, no matter how bad, even on my worst days.
I allow myself the moment to cry and to grieve. We’re human. It’s important to allow yourself those moments to curl in a ball on the floor and just let it out, but I know I can’t stay there. I won’t allow myself to stay there. I won’t allow myself to be destroyed or conquered in that way.
Find something to be grateful for, whether it’s my son’s smile and his little face, walking outside and seeing my favorite red cardinal or blue jay flying by, or a sunny day. Take those things in with appreciation and gratitude.


Focusing on the future
I try to set future goals for myself so that I can keep my mind focused on my future.
When you get scan results, it can put you in a mental space where you feel overwhelmed and want to just give up. You think, What’s the point in planning for the future? There’s not going to be a future, why plan for one? To fight that, I set future goals to make my mind focus on having a future with my family.
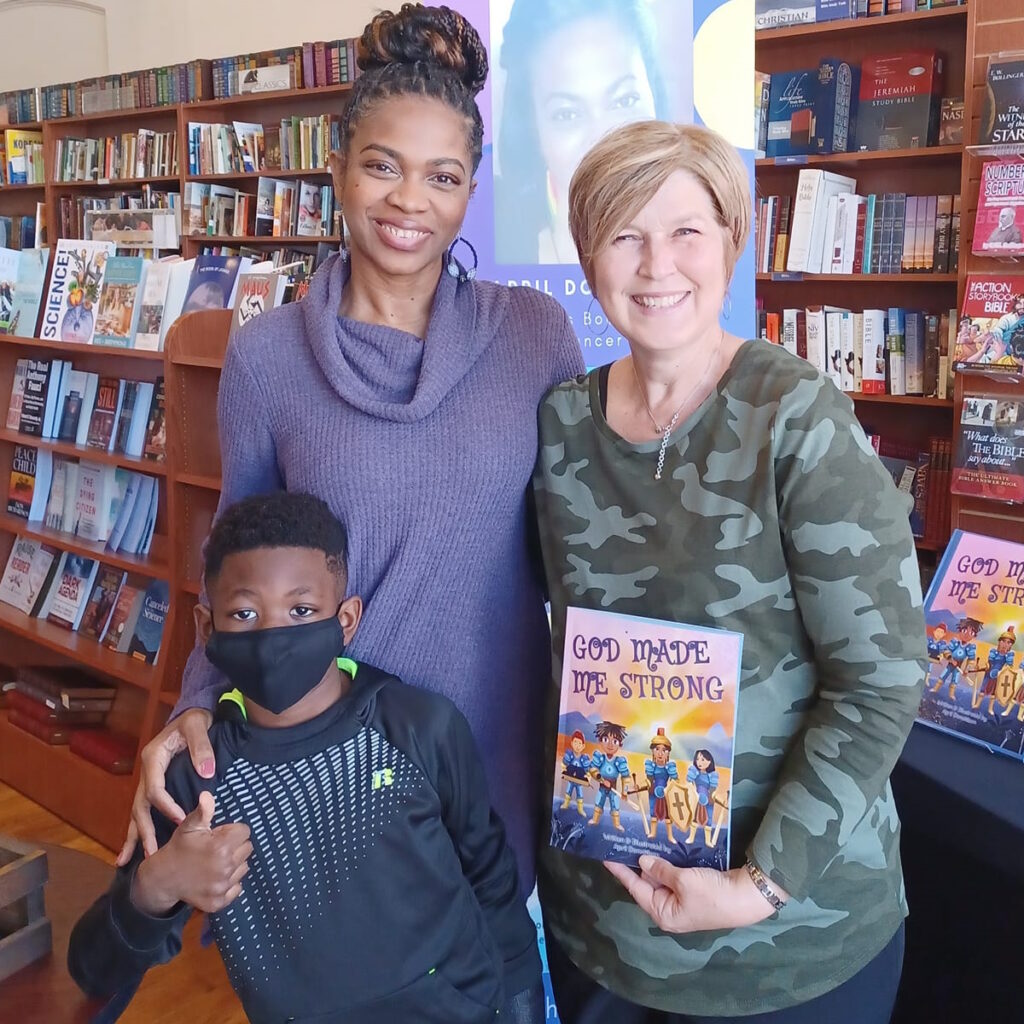
The first time I went through chemotherapy, I decided to get my real estate license so that was something for me to focus on.
The second time I went through chemotherapy, I decided to write a book for my youngest son. I wanted to give him something that we could read together every night and would remind him no matter how hard things get, God promises He will give us what we need to get through those hard times to brighter days. There are always brighter days on the other side.
I wanted him to have that that daily reminder and it was something that we could do together. He helped me with the drawings and the pictures. It was good for us. It was also my prayer that it would help other families with young children who were going through similar hard times and encourage their children as well.
Encouraging other cancer patients
My prayer is that by sharing my journey, I’m able to help some other person out there dealing with a cancer diagnosis.
Be encouraged that no matter what your diagnosis is, it’s simply a diagnosis. It’s simply a journey that you’re on. It’s not a journey that anyone wants to be on, but there is still a joy to be found. There’s still life to be lived.
You’re here for a purpose. Every morning that you wake up, there is a reason that you are still here. I just want them hopefully to be encouraged by a little portion of my story, to have faith and know that with God, you can get through this. You can and you will get through this.

Inspired by April's story?
Share your story, too!
More Triple-Negative Breast Cancer Stories
Maggie C., Triple-Negative Metastatic Breast Cancer, PD-L1+
Symptoms: Bruising sensation in the breast, soft lump
Treatments: Chemotherapy, clinical trial (antibody-drug conjugate and immunotherapy)
April D., Triple-Negative Metastatic Breast Cancer, BRCA1+
Symptom: Four lumps on the side of the left breast
Treatments: Chemotherapy (carboplatin, paclitaxel doxorubicin, surgery (double mastectomy), radiation (proton therapy), PARP inhibitors
Chance O., Triple-Negative Breast Cancer, Stage 2, BRCA1+
Symptom: Lump on breast
Treatments: Chemotherapy (doxorubicin, cyclophosphamide, paclitaxel, carboplatin), surgery (double mastectomy), radiation, radical hysterectomy (preventive)
Nicole B., Triple-Negative Metastatic Breast Cancer, Stage 4 (Metastatic)
Symptoms: Appearance of lumps in breast and liver, electric shock-like sensations in breast, fatigue
Treatments: Chemotherapy, surgeries (installation of chemotherapy port, mastectomy with flat aesthetic closure), targeted therapy (antibody-drug conjugate), hyperbaric oxygen therapy, lymphatic drainage
Kelly T., Triple-Negative Breast Cancer, Stage 3C
Symptoms: Swollen lymph nodes on the neck, high white blood count
Treatments: Chemotherapy (doxorubicin, cyclophosphamide, paclitaxel, carboplatin, capecitabine), surgery (nipple-sparing, skin-sparing double mastectomy), radiation, hormone therapy (tamoxifen)
Lucy E., Triple-Negative Breast Cancer, Grade 3, BRCA1+
Symptom: Lump in breast
Treatments: Chemotherapy, surgery (double mastectomy)
Melissa H., Triple-Negative Breast Cancer, Stage 2B, IDC
Symptom: Lump in left breast
Treatments: Surgery (mastectomy), chemotherapy
Symptom: Pea-sized lump
Treatments: Chemotherapy, surgeries (bilateral mastectomy, reconstruction)
Stephanie J., Triple-Negative Breast Cancer, Stage 3, Grade 3, IDC, BRCA1+
Symptom: Lump in left breast
Treatments: Chemotherapy, surgery (double mastectomy, oophorectomy, hysterectomy, breast reconstruction)







