Lainie’s Multiple Cancer Story

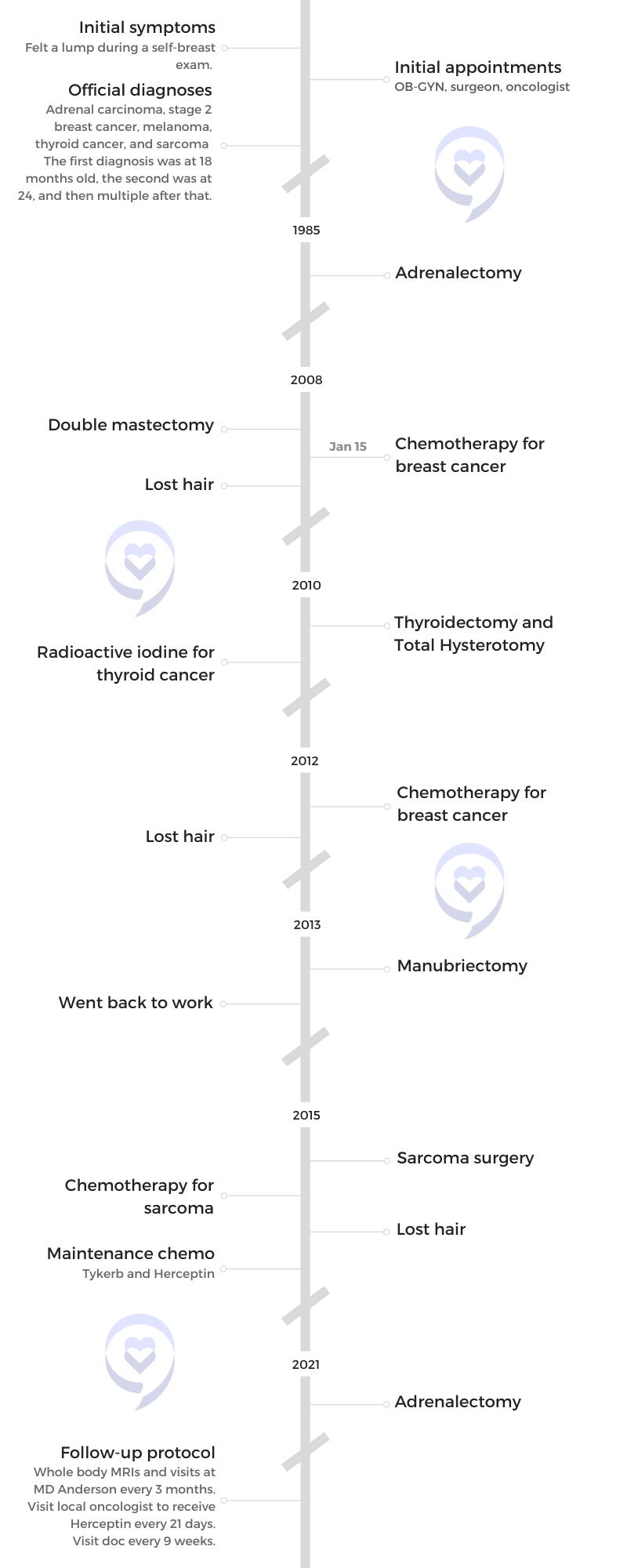
After feeling a lump in her breast, Lainie never thought she would be diagnosed with stage 2 breast cancer at 24, especially after beating cancer when she was 18 months old.
By the time Lainie was 26, she had been diagnosed with four cancers and then a fifth one only a few years later.
She shares how she’s been diagnosed with adrenal carcinoma, breast cancer, melanoma, thyroid cancer, and sarcoma. She discusses the different treatments and surgeries she’s undergone and how being an advocate for her health has saved her life.
She opens up about how she lives with Li-Fraumeni syndrome, a rare disorder that makes her more susceptible to growing cancer, her experience of hair loss right before her wedding, and how her support system has been crucial to her cancer journey.
- Name: Lainie J.
- Diagnoses:
- Adrenal carcinoma
- Breast cancer (Stage 2, HER2+)
- Melanoma
- Thyroid cancer
- Sarcoma
- Symptom:
- Lump in breast
- Treatments:
- Chemotherapy: for breast cancer (2008 & 2012), for sarcoma (2015)
- Radioactive iodine: for thyroid cancer (2010)
- Surgeries: adrenalectomy (1985 & 2021), double mastectomy (2008), thyroidectomy (2010), total hysterotomy (2010), manubriectomy (2013) sarcoma surgery (2015), multiple surgeries for recurrence
- Maintenance Treatments:
- Tykerb
- Herceptin (every 21 days)
- Follow-up Protocol:
- Whole body MRI and visits at MD Anderson (every 3 months)
- Visit doc (every 9 weeks)
That’s something that I live with every day now. I have this gene and my body’s susceptible to developing cancer.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Introduction
My husband and I live in South Florida [and] moved back from New York. I am 38 years old. We’ll be celebrating our 20th dating anniversary [in 2023]. We’ve been married [for] 10 years so he’s been with me throughout my cancer journey.
We have two wonderful little Boston terriers. I love shopping. I love going to the beach. I love being outdoors, doing fun things, and spending time with family and friends.



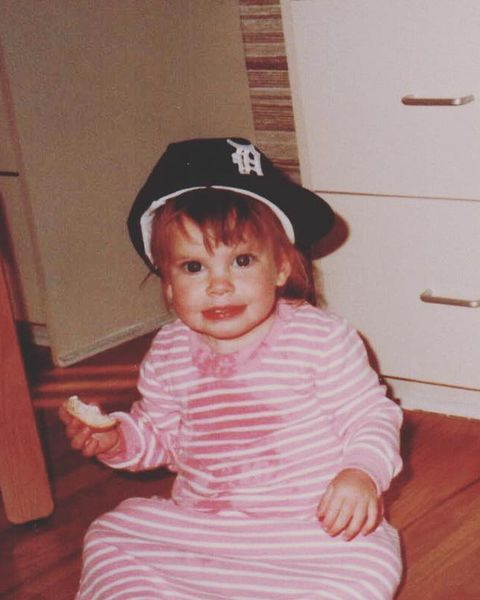
My first cancer diagnosis was when I was 18 months old… I had adrenal carcinoma.
Pre-diagnosis
Can you describe some of your first symptoms?
My first cancer diagnosis was when I was 18 months old so obviously, I don’t remember many of those. I had adrenal carcinoma.
Growing up, I knew that I was a cancer survivor and that cancer was a part of my life at some point but was too young to remember. It led me to being a nurse.
I turned into a hypochondriac [by] becoming a nurse because when you’re in school and you’re learning about all these things, you constantly think something’s wrong with you.
I was late [to] the nursing school game. I switched my career path. I started in fashion and then I’m like, “No, I want to go for what I have always dreamed to be, [which] is a nurse.”
I was doing a self-breast exam [in] July 2008 and I felt the lump. I went to my OB-GYN and he felt a lump, too, and he gave me a prescription for an ultrasound. I neglected to do it because I’m like, “I’m 24. I’ve already had cancer once. There’s no way I can get cancer again, right?” That was just my mentality so I neglected to do it.
Six months went by and it was December. My parents were like, “You need to go get the rest of your scans because you’re turning 25 and you’re going to be off of our health insurance,” so I got all my tests done. I went to my OB-GYN again and I’m like, “You know, I think the lump got bigger.” So he ordered a mammogram. I didn’t have any symptoms. It was mostly just a lump that I had felt for my initial breast cancer diagnosis.
‘I’m 24. I’ve already had cancer once. There’s no way I can get cancer again, right?’


Did you go get the mammogram or the ultrasound?
Yeah. It was the end of the year. I went to go get a mammogram. I went to this guy in South Florida who read mammograms right away. We went there and he read my mammogram.
I’ll never forget him telling my mom and [me]. He read it to us right there. He’s like, “It doesn’t look good.” And we were like, “What do you mean?” Here I am, just about to start nursing school, three and a half [to] four weeks away, and he’s like, “I want to do a biopsy.”
He ended up doing a biopsy and I was diagnosed with stage 2 breast cancer at 24 years old. It was two weeks before my 25th birthday. It was pretty crazy, pretty shocking. I never thought that I’d become [a] patient, let alone not be a nurse.
I didn’t go to nursing school because I had to have surgery. I did a double mastectomy and then I went through 12 weeks of chemotherapy.
I was diagnosed with stage 2 breast cancer at 24 years old… two weeks before my 25th birthday.
Were there any other symptoms other than the lump?
No other symptoms. I was perfectly healthy.
I’ve had multiple cancers. I’m very fortunate — fortunate, unfortunate — [that] I don’t have any symptoms. I feel great. I always say that the craziest thing about cancer is sometimes, you don’t have symptoms, but that’s a good thing, right? Because then you catch it early and that’s so important to me. Spreading awareness and creating the importance of early detection because that’s truly what’s saving my life.


Diagnosis
When you felt that lump, did you ever think this could be cancer? How did you process that diagnosis when you heard those words?
I always felt like my intuition told me that something wasn’t right but then I was also going into nursing school so I’m just like, “Maybe I’m just overthinking these things.”
As a person, I was always extreme. Everything was always just me making things up in my head that it’s worse than it really was. I never thought it was going to be anything. I thought it was just going to be maybe a cyst or something.
When I was diagnosed, I literally was shocked. I couldn’t believe it. When you get a diagnosis, you’re like, “Oh my god, I’m going to die.” Literally, that was the first thing that I said to myself. “I’m too young. I don’t want to die.”
I think the scariest part for me was having to get additional scans after that because you worry. You’re like, “Where is it?” I just always feel like [with] cancer, sometimes you don’t have any symptoms. My bloodwork was never abnormal so I didn’t really have any symptoms.
In that moment, it was a pure state of shock. I processed it. Then I think what really helped me was I spoke to a volunteer through the American Cancer Society Reach To Recovery program. She was like 60 years old, I want to say. I didn’t know her. It was just a phone call and it was about 48 hours after I came home from my double mastectomy. I was like, “Wait. If she’s 60 and I’m 24 and she survived breast cancer, I can do this, right?” That’s why I think it’s so important what you guys are doing because it’s really just giving another lens.
We need to take away that stigma of thinking of cancer as a death sentence and think of it with a positive attitude. That’s so important. I know it’s easier to say than done, but I always tell people I cried for one day and that was it. I said, “You know what? I’m going to do this.”
Unfortunately, there [are] so many younger people being diagnosed, especially with breast cancer. At that time, I was like on a lone island. There [were] not a lot of people who had breast cancer. It was 2008 — not a lot of people my age. I did meet a few young people. I was so grateful that I had an amazing, supportive family and I had an incredible husband who stood by my side the entire time.


Getting tested for Li-Fraumeni syndrome
When I was diagnosed with breast cancer at 24, I was tested for the BRCA gene. I did not have it so in my oncologist’s mind, “You don’t have BRCA. I think it’s just kind of like maybe a hormonal thing that you got breast cancer.”
When I got melanoma, I started to really question. I’m like, “Again, something’s not right. I’m 25 years old. I’ve had three cancers. This is crazy.”
My mom and I were listening to Doctor Radio on SiriusXM and they were talking about adrenal cancer and this genetic predisposition called Li-Fraumeni syndrome. They were basically saying that if you’ve had adrenal cancer, there’s a 90% chance that you could have Li-Fraumeni syndrome. We’re just like, “This is crazy.” At the time, again, genetics were not widely talked about. It was really just BRCA.
I asked my doctor if I can get tested for this gene. He’s like, “Yeah. I doubt you have it. That’s a textbook thing.” So I was like, “Okay, fine.” He told me I was negative. And you trust your doctors. Again, you have to trust your gut. You always trust your doctors, right? But also make sure you get that physical piece of paper. I didn’t do that.
Age 26 comes along and I get my one-year follow-up for my breast cancer. They did the whole body PET scan. The next day, the doctor calls and he’s like, “There’s a really big mass in your neck and it spread to your chest.” It ended up being thyroid cancer.
I had to go to an endocrinologist and I’m just like, “What? I’m 26 years old and already I’m at four cancers. And I’m told I don’t have Li-Fraumeni syndrome.” That was in the back of my head.
At that time, my endocrinologist, my surgeon they sent me to MD Anderson. That’s when you know you have amazing doctors. They’re like, “We’re not touching you anymore. We’re done touching you here in Florida. You need to go to a cancer-specialized hospital because something is just not right.”
The first question they asked me when I got there was, “Have you been tested for Li-Fraumeni syndrome?” And I’m just like, “Yeah! I’m negative.” I did end up having it and I was never correctly tested.
I don’t hold grudges. Maybe he didn’t know. He just thought it was textbook. Maybe he did the wrong test. Whatever it was. People are always like, “You should go back to that doctor. That’s terrible.” I’m like, “No. It’s fine.” I’m just moving on and now I know I have this genetic predisposition.

For me, it’s so important because it really changed my protocol in my testing. I was getting PET scans all the time. PET scans and CT scans [are] not good for somebody with Li-Fraumeni syndrome because of the radiation.
My parents, thank God, don’t have it. Neither do my brothers. They don’t have Li-Fraumeni syndrome. Nobody in my family has it. But my parents are both cancer survivors, but they don’t have the gene. We are also Ashkenazi Jewish, so a lot of times, that could be a triggering factor.



Being diagnosed with 5 different cancers
I was getting those tests because that was the standard protocol. When I started getting the PET scans, things changed. I always say it’s just so crazy.
I feel so lucky that we’ve come a very long way [from] when I was diagnosed in 2008 until now. Sometimes it’s very hard for people to see that. But I’ve been living it. I see people, like myself, who were diagnosed in 2008 and things were different. Everything was different.
I always tell people, as weird as it sounds, it’s a good day and age to have cancer. There [are] so many options out there. People are living with this disease and thriving.
I’m on maintenance chemotherapy for the rest of my life and it’s literally keeping me alive. I tell people, “You take blood pressure medicine every day. I take chemotherapy and it’s amazing.”
There was a mole on my back… and it ended up being a melanoma… Here I am. I’m 25, now with three cancers and I’m just like, ‘What is going on?’
Treatment
What was your treatment?
I’ll just backtrack a little bit. When I was diagnosed, I was treated, I like to say, as the typical breast cancer patient. I went in. My doctor knew I had adrenal cancer as a baby. But again, that time, seeing a 24-year-old was kind of rare. I [had] a standard treatment. My breast cancer was HER2-positive so I had the HER2 receptor gene. I think I did TCH. My memory is completely fogged because I’ve done chemo a lot. It was like a TCH combination — Taxotere, Carboplatin, and Herceptin. Then that was it.
I did a double mastectomy initially, then I did expanders, and then I had the expanders transferred out for regular implants. I lost my hair, of course. My treatment stopped in July of 2009.
Then there was a mole on my back and my mom’s friend was like, “Oh no, I know she has a lot going on, but I just want to let you know, she needs to get that mole looked at.” I got it taken off and it ended up being a melanoma, which was crazy. Here I am. I’m 25 now with three cancers and I’m just like, “What is going on?”


I think the important thing is, and this is something I really kind of learned along the way, a lot of times people go to a breast oncologist who specializes in breast oncology and that’s amazing, right? If you just have breast cancer. But something I learned is, a lot of times, when you have one cancer, you could get two cancers. It’s something I never knew.
I never look back but something that I would have done a little different is gone to a general oncologist given my history [of] adrenal cancer. Sometimes that’s not spoken about a lot is that if you’ve had multiple cancers, maybe it’s better to be with a general oncologist.
In that moment, my oncologist was like, “Well, I only do breast cancer.” So then I was kind of like, “Oh my god, I’m stuck here.” I don’t know what to do. This is my third cancer. Something’s not right.
Did the treatments overlap?
I have a little bit of breaks in between. I did the chemotherapy first for breast cancer and then I don’t think I was on anything. I was always on Herceptin though till a certain amount of time after my treatment.
Then [for] the thyroid cancer, I had what’s called RAI — radioactive iodine. I was in the hospital for three days. That never overlapped with the breast cancer because I wasn’t on anything.
Then there was a point where I think I was on oral chemo. I did have some intermittent metastatic reoccurrence. Those were treated with oral chemo and then I did radioactive iodine.
I can’t remember if they overlapped but I think if they did, they stopped and then started.
In 2011, I was re-diagnosed with breast cancer and I think it was one or two lymph nodes. They did stop my Herceptin and the Tykerb that I was on initially and another drug called Xeloda. I was off of it for eight months and this lymph node showed positive.
I was at MD Anderson at the time so I saw breast oncologist there and they’re like, “We want to take an aggressive approach with these two lymph nodes because it’s concerning that your cancer came back and you were on a chemotherapy and then you stopped it. So something’s not right.”

I was eight weeks away from getting married. I was so bummed.
We were together seven years before we got engaged. My running joke with my husband was, “You cannot propose to me until my hair is long.” Then it turned out, I had to lose my hair four weeks before my wedding. But it’s okay. Everything happens for a reason.
They did aggressive chemotherapy. In 2012, I had radiation, which was a little risky because of Li-Fraumeni syndrome. But, thank God, I have not had a reoccurrence of breast cancer since 2012. The radiation really helped, but it led to also another cancer.
It’s crazy but they knew it could cause another cancer so the doctors aggressively watched me. Every three months, I would get whole body MRIs and ultrasounds. In 2015, they caught three tiny spots of sarcoma in my chest wall through an ultrasound.
Again, back to early detection. I’m on top of my health. They caught it. I ended up having to do a different type [of] chemo again, super aggressive, in 2015. But in between all of those, I’ve always been on Herceptin. That’s a drug I’ve been on and still on it to this day. Since 2012, I’ve been on it consistently, every 21 days. [I’ve also been on] a pill called Tykerb, though I did stop when I had my sarcoma because it contradicted [with] some of the meds. But they always added Herceptin to any type of chemotherapy I was going through.
Learning that your cancer treatment caused another cancer
As crazy as it sounds, I feel like it was like a watch and wait. I think that that’s something that I live with every day now. I have this gene and my body’s susceptible to developing cancer. That’s literally what it is.
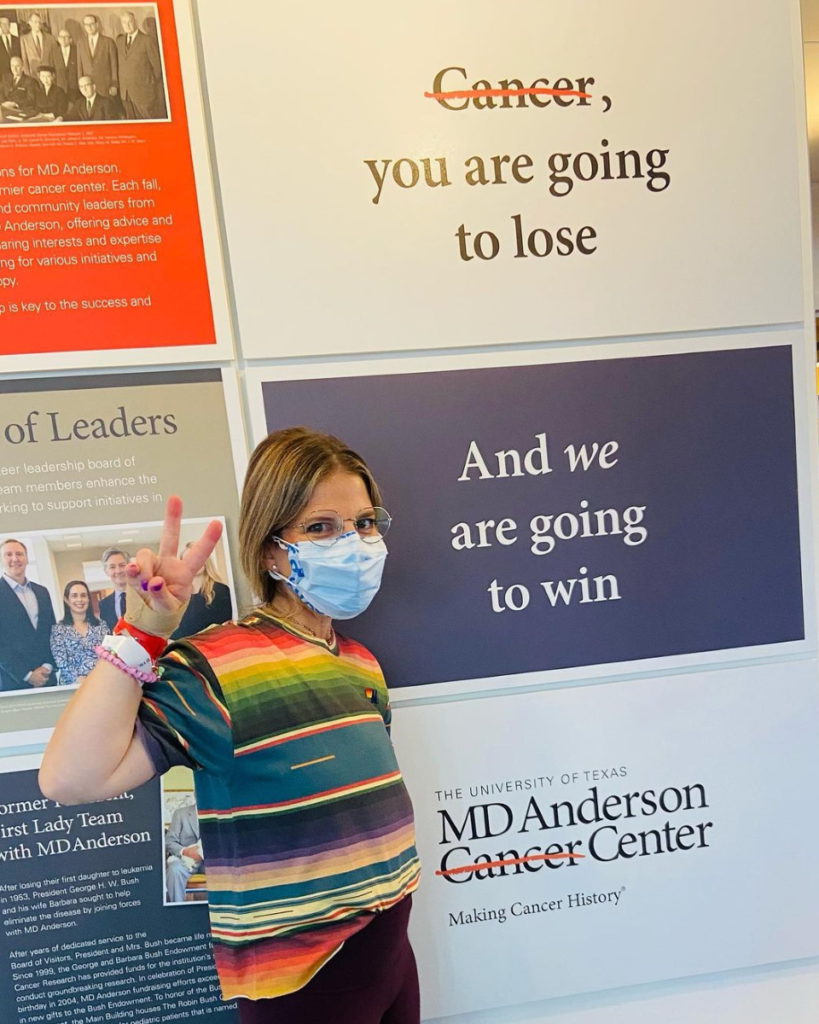
I tell people I live my life in three-month increments. I go to Houston every three months, get whole body MRIs and ultrasounds, and see my doctors there. I tell myself if there’s something there, it’s only three months old. It really helps me process everything. I’m very fortunate.
I always put a disclaimer. Everybody is different. Everybody’s cancer journey is different so never compare yourself to someone else. Somebody might be [reading] this and say, “Oh, I have Li-Fraumeni syndrome. That means I need to get my whole body MRIs every three months.”
I think every single person is their own patient. That’s why I love going to MD Anderson because they treat me like I’m not like the patient who was in there before or the patient after.


Of course, I get scanxiety. I’m human. I live with that. In the moment, if there is something there, I freak out like any human would. Then I just tell myself, “It’s only three months old.” So that’s really where I’m at with everything.
Did I know that I was going to probably get another cancer from radiation? Yeah. Is there still a chance that I could get another cancer from that radiation? Absolutely. It’s just the life I live. I’ve chosen to just take it and turn it into my purpose and not dwell on it. It’s out of my control.
What were some of the side effects from treatments?
Nausea was the worst. I think that that was terrible. I did a lot of lemon ice cubes. I made my own ice cubes with lemon drops in them.
Every treatment was different. Neulasta was terrible for me. A lot of people don’t have that.
Dairy was something I loved eating. It was so weird. Each chemotherapy, I had different cravings. I always say it was like being pregnant. I had all these crazy, weird cravings. I was craving feta cheese at one point.
How did you deal with the side effects?
Just exercising, like walking, making sure you’re moving [and] hydrating.
Mind over matter. Staying positive. You can have your days. It’s okay.
And just living in the moment and making the best of a crappy situation. Lemons into lemonade, as cliché as that sounds. Surround yourself with positivity. That’s really what helped me get through everything.





What was going through hair loss like for you?
Losing my hair the first time was the hardest thing for me. I want to say I was vain, but my hair was my favorite part about myself. That was my thing. I had a wig and it grew back.
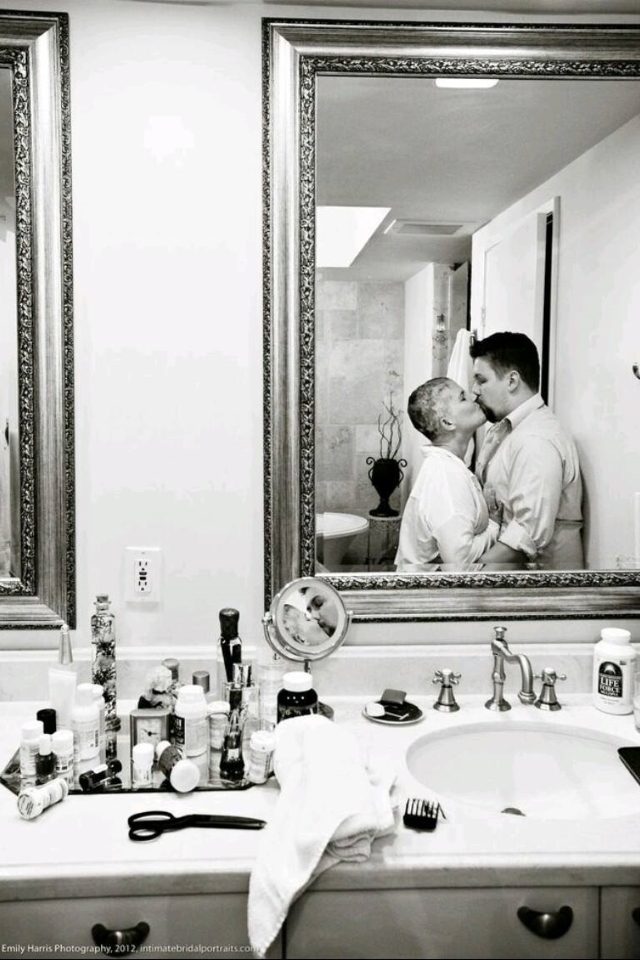
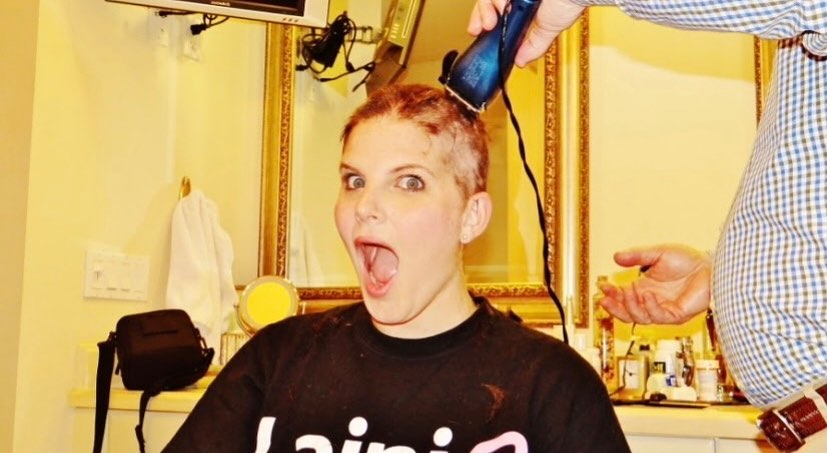
I told my husband he can’t propose to me until my hair is long and then I had to lose my hair. I actually had my wedding photographer document my head being shaved right before my wedding, which was so amazing. I was known as the Cancer Fighting Bride.
Losing my hair was probably the hardest time. It was not the bride I envisioned [myself] to be. I didn’t look like myself. I was on steroids for chemotherapy and I just didn’t feel like myself.




I look back at the pictures and I’m like, “Oh, God, I didn’t look like who I was.” But my husband’s like, “You’re here. And that’s all that matters.” I think that that’s something to always remember. Never lose sight of what is going on, especially for people who are brides. It shifted life into perspective.
Your wedding isn’t about the flowers, what everybody’s wearing, and all that drama that goes along with it. It’s about the people surrounding you in that room and the person you’re marrying. It’s all about love and family. And that was really captured at our wedding and through our incredible photographer.



When I had to lose my hair the third time, I’m just like, “Okay, whatever.” At this point, it is what it is. I’m just like, “You know what? This time, I don’t want to shave it. I want to see what it’s like for it to come out. Let’s experiment this.” Then I ended up shaving it.
Each time was different and it sucks, but your hair grows back. That’s something to always remember. There [are] cold caps nowadays that people do and so many great things now that you don’t have to necessarily lose your hair, but also amazing wigs.
You’ve got to find the positive in everything. Not having to do your hair every day and just slapping on a wig was the best thing ever. During my wedding, my hairdresser did my hair and it stood on a stand [while] I was able to just roam around and get my makeup done. It was like killing two birds with one stone.
What is your current maintenance treatment?
I take oral chemo every day and then I get Herceptin every 21 days. Thankfully, the only side effect I get is some headaches. But other than that, it’s very easy.

I have such an amazing support system. It takes a village. I couldn’t do this on my own.

Importance of a great support system
I’m so grateful. I just feel like my whole family, everybody… My husband is a saint. He sometimes has to remind me, “You got to stay on top of your health.” I mean, I’m always on top of my health but he reminds me [about] certain things. He’s so incredible, too, because not everybody is that lucky.
I have such an amazing support system. It takes a village. I couldn’t do this on my own.
Did your parents being cancer survivors impact you in any way?
Totally. All I can say is God bless our caregivers. I’m a hypochondriac and I’m neurotic so I was crazy. It’s funny being on the reverse end because I was never in that seat.
My parents, thank God, are both doing great. My dad had prostate cancer and thank God my parents are really diligent about their health, too, just given what I’ve gone through, which I’m also so fortunate about.
My mom had a rare blood cancer called myelofibrosis. She ended up having a bone marrow transplant and she, thank God, is doing amazing. She had an anonymous donor who she fortunately got to virtually meet a few years ago. [The] donor was a 12 out of 12 match. That process she went through was eye-opening and scary.
I can see where I get my strength from — my parents. I work at the American Cancer Society. I tell people this is our purpose in life. We are a family who rallies together to really just make a difference.
I’m so grateful I have my parents as my examples. They would probably say that I’m their example but I think we all feed off of each other’s energy. We’re just very lucky that we’ve had great outcomes.
I have a lot of cancer in my family, too, so it’s crazy. My mom’s parents, unfortunately, passed away from cancer, but my dad’s parents lived till 94 and 96. It’s a good situation to be in, right? I have cancer and longevity.





Being your own advocate
It’s so important to trust your instincts. Doctors are amazing. It’s okay to have another opinion. I think that’s so important if that’s something that’s very important to you.
You need to feel comfortable with your physician. That’s so important. Making sure if something is not right, you know your body best. You live in the skin you’re in. You know your body the best and if a physician is not willing to act on it, move on.
If somebody calls me and they’re newly diagnosed, don’t get too many opinions. You can drive yourself crazy with opinions. Narrow down to [whom] you feel the most comfortable with. You could get so many opinions then by the time you find somebody that you really like, it’s too late. That’s really what it boils down to. Listen to what your heart is telling you, really.



Importance of documentation
It’s very important to get everything. I always ask for my blood work. We live in a virtual world these days. Have everything in hand, make a file folder, and keep everything, as annoying as it sounds. Or just get the paper, scan it, and throw it away. Visibly see them.
Even if you look at it and it’s in your MyChart, once they give you your results, always take them and look at them so you understand what’s going on and make sure that that’s exactly what you see and what they see. Doctors are very busy people. We’re all humans. We all make mistakes. That’s definitely a lesson I learned. I always get my paperwork.
I’m old school. I take all my paperwork with me. I think really just following through. I always revisit all my tests.


Every time I get a scan, I ask for it and put it in a file folder. Then I really make sure I have everything together. Review it.
A lot of times, I get rid of them just because everything is in like a MyChart but I like to review everything. It’s just one of those things. I review everything in detail. I have no adrenals and my scans sometimes say that my adrenal is present and I question.
It’s okay to ask questions. It’s so important. Always ask questions. If there’s something you’re a little confused about, ask. The worst thing they’re going to say is, “You’re fine. Don’t worry about it,” or it raises a concern.
I had an incident a few months back when I was in Houston and I had blood work. My BUN was elevated and the doctors weren’t concerned. It was elevated two points, nothing crazy. But I asked. It didn’t look right and it was higher than before.
Never be afraid to ask a question. Like I said, we’re all human and things can get overlooked. Most of the time they’re nothing but it just shows you’re doing your due diligence.
Words of advice
If you feel something that’s not right or something wasn’t there that you were born with or something looks abnormal, even if you’ve never been diagnosed with cancer, go to your primary care physician or go to your oncologist. If something’s not right, again, you know your body best so you need to speak up and say something. It’s so important.
Having a positive attitude
I think my purpose is to help others and that has really helped me through my journey. When somebody is diagnosed with cancer, I’m always the first person they turn to, which is totally cool with me. I’m there to help people. I’ve turned my diagnosis into my purpose.
As much as people think it might define who I am, I let it empower who I am. It’s really helped me get through things.
At the end of the day, life could be so much worse, as crazy as it sounds. I’m so grateful that I’ve been able to shift everything and shift my mind.




It’s not always easy. Cancer is not sunshine and rainbows and I know that. But I think, for me, I just really hope that my story helps others and not let people be scared of cancer. Because a lot of times, people delay getting screened or delay getting something because they’re scared they’re going to get cancer.
It’s so important not to delay any of your screenings and stay on top of your routine screenings year after year. Early detection is really a testament to why I’m here today. It saved my life.
How do you deal with scanxiety?
It’s really just the three-month thing. That really just helps me. I just stay positive. It’s that saying, “It is what it is,” and that’s really what it is.
Just knowing that I’m able to have those scans every three months and knowing that if there is something there, it’s not that old. That’s just really kind of what gets me through it.

How far we’ve come with cancer research and treatments
It’s a good day and age to have cancer. Treatments have come such a long way. From when I was diagnosed in 2008 till now, everything has changed immensely, which is so incredible.
There’s people taking pills right now for cancer, not having to lose their hair, and not having as many side effects. I think that that’s just so incredible.
If that can be any hope and push for those to get screened, I think that that’s so important because there’s so much out there. The most important thing is to catch it early and not ignore any type of symptoms. Even if you don’t have symptoms, if you just feel something, don’t ignore it.

It’s so important not to delay any of your screenings and stay on top of your routine screenings year after year. Early detection is really a testament to why I’m here today. It saved my life.


Inspired by Lainie's story?
Share your story, too!
More Invasive Ductal Carcinoma Stories
Amelia L., IDC, Stage 1, ER/PR+, HER2-
Symptom: Lump found during self breast exam
Treatments: TC chemotherapy; lumpectomy, double mastectomy, reconstruction; Tamoxifen
Rachel Y., IDC, Stage 1B
Symptoms: None; caught by delayed mammogram
Treatments: Double mastectomy, neoadjuvant chemotherapy, hormone therapy Tamoxifen
Rach D., IDC, Stage 2, Triple Positive
Symptom: Lump in right breast
Treatments: Neoadjuvant chemotherapy, double mastectomy, targeted therapy, hormone therapy
Caitlin J., IDC, Stage 2B, ER/PR+
Symptom: Lump found on breast
Treatments: Lumpectomy, AC/T chemotherapy, radiation, hormone therapy (Lupron & Anastrozole)
Joy R., IDC, Stage 2, Triple Negative
Symptom: Lump in breast
Treatments: Chemotherapy, double mastectomy, hysterectomy




