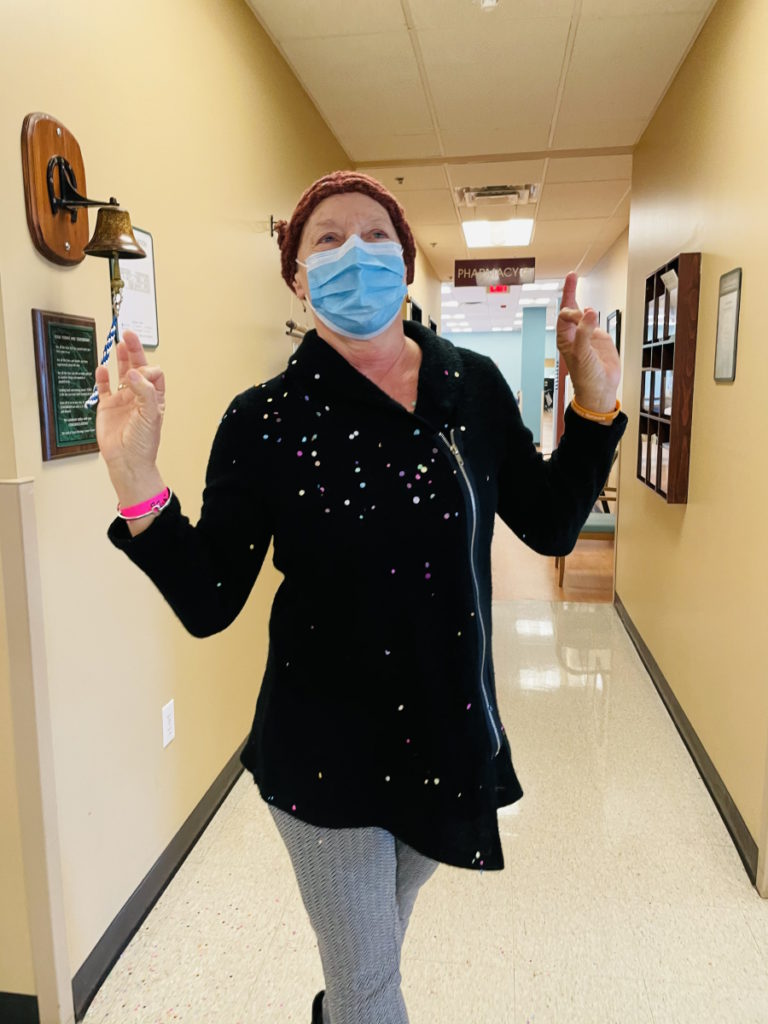
Vickie’s Muscle-Invasive Bladder Cancer Story

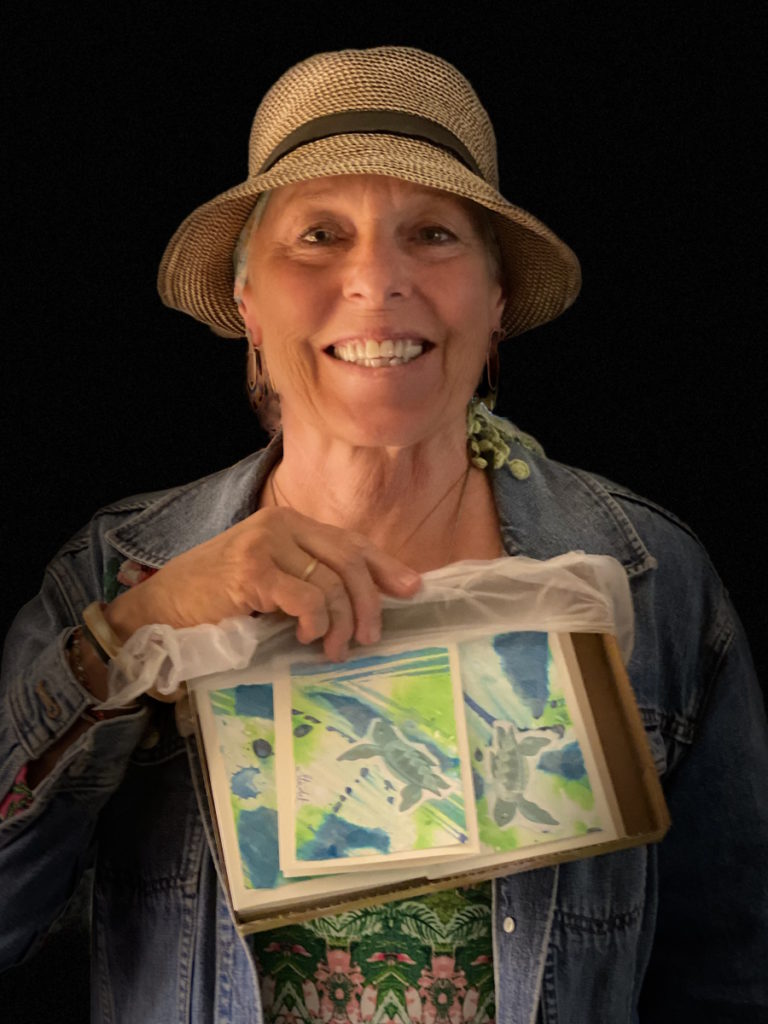
Vickie was diagnosed with muscle-invasive bladder cancer at 66.
She was initially experiencing intermittent pain but after being told that she did not have a urinary tract infection, she knew she had to keep pushing for answers.
Margo, also a bladder cancer patient, talks with Vickie as she shares her journey of how advocating for herself helped save her life.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Name: Vickie D.
- Diagnosis:
- Bladder cancer
- Initial Symptoms:
- Intermittent pain in the gut and burning sensation
- Treatment:
- Chemotherapy: dd-MVAC (dense-dose methotrexate, vinblastine, adriamycin, and cisplatin)
- Surgery: cystectomy
It did not surprise me when I got that phone call that it was a tumor. What surprised me was that the only way out was to do chemo and have my bladder removed.
All of us are doing what we can to increase awareness of bladder cancer… to help bring this conversation to normalcy and share stories, hope, and inspiration for others going through it.
Margo W.
Plasmacytoid Bladder Cancer Survivor
Introduction
Margo W.: I’m a bladder cancer patient who is still cancer-free because I had access to great doctors [and] because I advocated for myself.
We know a fair amount about other kinds of cancer, but not so much about this one. Cancer is not something you want to learn about if you don’t have to so we all have big gaps in understanding what the journey is going to look like.
I had the opportunity to meet and talk with other patients. I love that I get to interview Vickie. She can share her experience and how much it meant to her that she had a bladder cancer mentor who [can] show her what life after [having] your bladder removed looks like. It’s not as terrible as you fear. You have no idea what to expect so that’s why I think it’s so important to share these stories.
We all have some similarities in our stories, but we also have unique experiences. One of the most valuable things to do is to help people not feel alone and to remove a lot of the fear [and] the unknown so that we can see ourselves making it through that journey, get to the other side, and get back to living life.
I hope what it does is inspire and help people feel connected, understand, and reduce fear as we face a variety of different battles.
Vickie, if you had to describe yourself to someone who’s never met you before cancer, how would you describe Vickie?


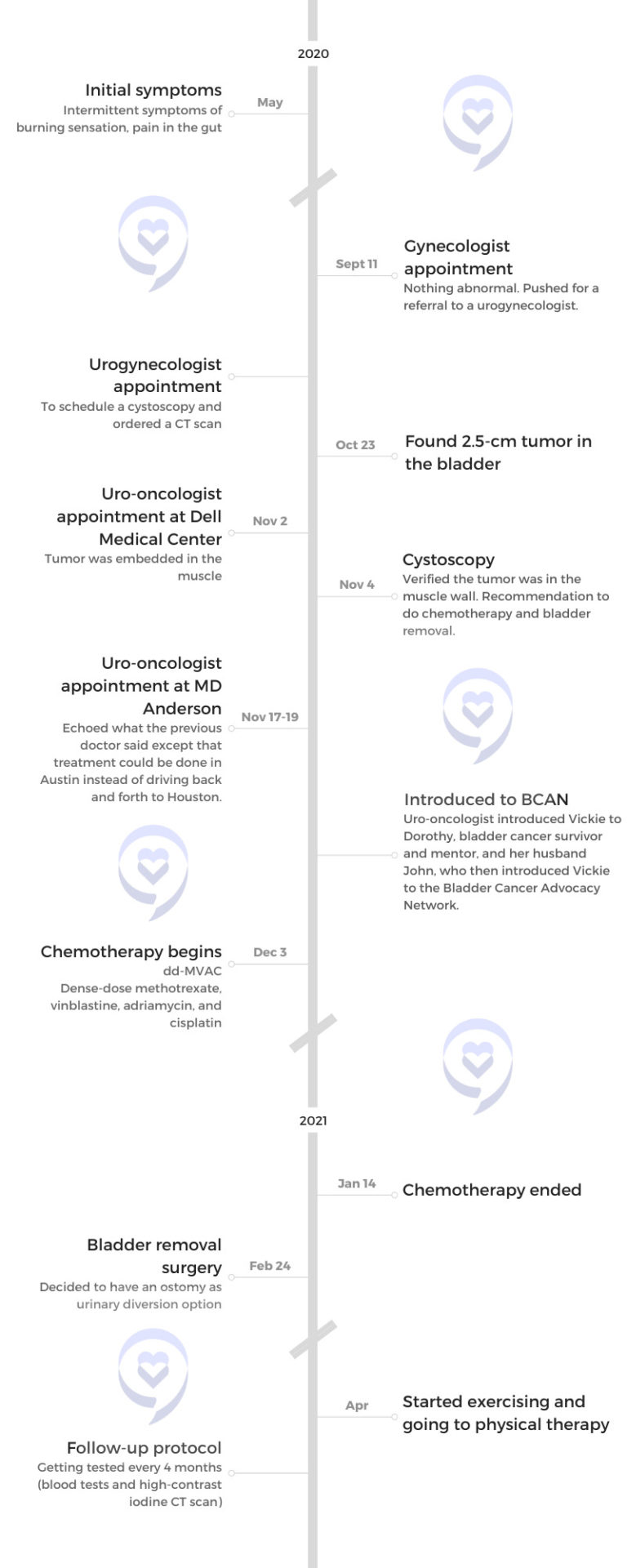
I was diagnosed in the fall of 2020. I was 66 years old.
Before cancer, I was trying to cram as many things as I could into a day, almost aggressively staying busy.
I’m outdoorsy. Tomboy is what they would call me. I have a small lake house. I spend time out there doing projects.
I love the water. I swim, paddleboard, kayak, bicycle, travel, [and] garden. I have some chickens that are pretty fun to have in the city. I live in the middle of Austin, Texas, and I have lived here most of my life.
Margo found me through Dorothy, who is also a bladder cancer survivor. She’s my bladder cancer mentor.
Margo W.: And I met Dorothy and her husband, John, at the bladder cancer think tank in August of ’22. Dorothy and her husband are very involved with BCAN, Bladder Cancer Advocacy Network. They are also Austin-based. They’re working to create more awareness.
All of us are doing what we can to increase awareness of bladder cancer because it is the least talked about of the major cancers. It’s number sixth or seventh most diagnosed in this country. We are doing what we can to help bring this conversation to normalcy and share stories, hope, and inspiration for others going through it.


Pre-diagnosis
Initial symptoms
Margo W.: What made you think about the pain that you were in? What about that told you [that] you needed to keep pushing for answers?
I didn’t feel well and had some pain. The pain was intermittent enough that it was reoccurring. It wasn’t every single day, but it was enough.
I had a doctor’s appointment coming up in September; May 2020 was when I first noticed that the pain was getting to be less intermittent and almost daily.
I did believe I needed to see my gynecologist and not my family practice physician. I realized that I needed to keep pushing until they would see me. But unfortunately, she wasn’t interested in an old woman that was having a little pain.
Margo W.: How did she specifically respond to you?
She responded by saying that all of my tests had always been fine. I hadn’t had any abnormal test results over the years.
Unfortunately, because I was 66, I had seen many gynecologists over the years from having my children. Then as I aged, these wonderful doctors quit taking patients.

‘You do not have a UTI.’ That wasn’t a good answer for me because I knew if it’s not that, then what is it?

This young woman had only seen me once a year before and I guess she’s just going off of all the test results we had discussed and things that had happened in my life.
I said, “There is something wrong. This pain isn’t going away and I don’t believe it’s a bladder infection [or] UTI. I’ve only had one in my life and there’s no blood.” She said, “We’ll go ahead and run that test again [to] make sure it’s not a UTI.”
They ran the test again [and] called me up. “You do not have a UTI.” That wasn’t a good answer for me because I knew if it’s not that, then what is it?
Ironically, the day after my exam, I started seeing blood. I called them right back and said, “I need to see you again. There’s something wrong.” They had me see the assistant and she also said, “You do not have a UTI.” I said, “Then let me see someone else. Who can I go see?” They recommended a urogynecologist.
Seeing a specialist
Margo W.: Your only symptom was persistent, consistent pain and discomfort. You shared it with her. It’s not a UTI.
The gynecologist [was] saying, “I don’t know what it is if it’s not a UTI. I didn’t see any abnormal results from your pap smears. I haven’t seen any other abnormal results. I don’t feel anything.”
I’m freaking out on the table. ‘What do you mean? Why do we need a CT scan? Doesn’t that mean cancer?’ She said, ‘Oh, there’s no chance of you having cancer. That’s an old man, smoker’s disease.’
The next thing was to get that next specialist. I called my friends and no one had a urologist in their phone book. My next step was to rely on this doctor.
I had to call three times to get the name and then the referral. Luckily, the referral was a gyno-urologist. She said, “I don’t think there’s anything the matter here, but just in case, we’re going to take some measurements. We’re going to go ahead and do a CT scan. We’re also going to do a cystoscopy.”
I’m freaking out on the table. “What do you mean? Why do we need a CT scan? Doesn’t that mean cancer?” She said, “Oh, there’s no chance of you having cancer. That’s an old man, smoker’s disease.”
I did smoke for a short while in my 30s, but I hadn’t smoked then for 30-something years. “It’s probably nothing, but let’s do the CT.”
The next step was to make the appointment. No one in Austin could see me for at least two weeks. I finally found a place out in Cedar Park, which is a good 30 miles away.
It was daunting and because it’s COVID, I have no one with me. Everything that I did, I’m completely by myself because no one was allowed with me. I’d have my phone with me and do a conference call.


Diagnosis
Getting the official diagnosis
I was on a trip. The urogynecologist called me up and said, “I have some bad news,” and that’s how she said it. “I can’t help you. I need to refer you to another doctor.” I have a tumor in my bladder. She told me it was about two and a half centimeters and I said, “That’s the size of my thumb. Oh, that’s not good.”
Doctor wasn’t available for two weeks. It’s now [the] end of October. I pushed that appointment up. I said, “No, I need to see this doctor. What’s his next available? Work me in,” so they did. They worked me in and that was November.
That was daunting to see his business card saying that he was not just a urologist, he was a uro-oncologist. I went, “I have cancer.” I’m thinking, Tumor. They get rid of a tumor. I’ve had a benign tumor removed from my breast. I thought everything was fine. He said, “No, let me show you your scan.”
I saw the tumor on the bladder wall. “What does this mean?” He said, “It means, yes, we’re going to do the cystoscopy. We’re going to try to remove it, but it looks like it’s on the wall. And if it’s in the muscle, there’s nothing that we can do but remove the bladder.”
I was by myself. I’m just going, “Please don’t tell me this. I don’t know what that means for my life because I am super active and I don’t want to stop.”
I took his information. I said, “What about a second opinion?” He goes, “Before we get there, I want to do the cystoscopy.” He was putting me out [for] two more weeks. I said, “Nope, I need you to schedule me next time you’re doing this procedure. Please work me in. I beg you.”
He’s 35 years old at the time. He’s my daughter’s age. I’m just going, “I don’t believe this doctor knows what he’s talking about,” but he does. I knew it, but I didn’t want to know it.
We [did] the cystoscopy two days later. He came out and said, “I can’t do anything for you but chemo and remove the bladder.”

I have tried to eat right, stay fit, [and] do everything to be healthy. I always thought it would be a heart attack or a stroke. I had no idea it would be a tumor that I would have to face.

Knowing it was more than a UTI
Margo W.: When you first went to the doctor, the gynecologist said it’s nothing and it [was] not a UTI. What were your feelings at that point?
It was not the news I wanted to hear. I wanted to hear that you can take an antibiotic and the pain will go away. “You need a hysterectomy.” I could handle that. Isn’t that weird?
I could handle someone telling me that [I] need a different operation because I know many, many women that have had a hysterectomy and I’ve watched them go through this process and healing [from] it. You just don’t need the uterus at this age anyway. But the bladder?
Margo W.: Still need one of those. Then you went to the next doctor who was a urologist-gynecologist. She’s the one who said, “No way this is bladder cancer. That’s an old man’s disease.” How did you feel when she told you that?
I felt bad that I had smoked cigarettes in my life. My first thought is, Oh, old man smoker. Well, I’m an old woman and I did smoke, but I haven’t for so long.
Then my brain just went to, I don’t believe her. I believe there’s something much… I don’t want to say much worse because something could be much worse, we know that. Things can be worse. But I thought, I don’t really believe her. I think it is something.
It did not surprise me when I got that phone call that it was a tumor. What surprised me was that the only way out was to do chemo and have my bladder removed.
Going to doctor’s appointments alone
Margo W.: You are doing all of your doctor appointments solo. No one could go with you. What did that feel like?
I’ve always been independent so, at first, that didn’t bother me. But the day that Dr. Laviana said, “You have cancer and this is what has to happen if you want to live,” then I needed somebody. That is the moment I wish somebody had been with me.
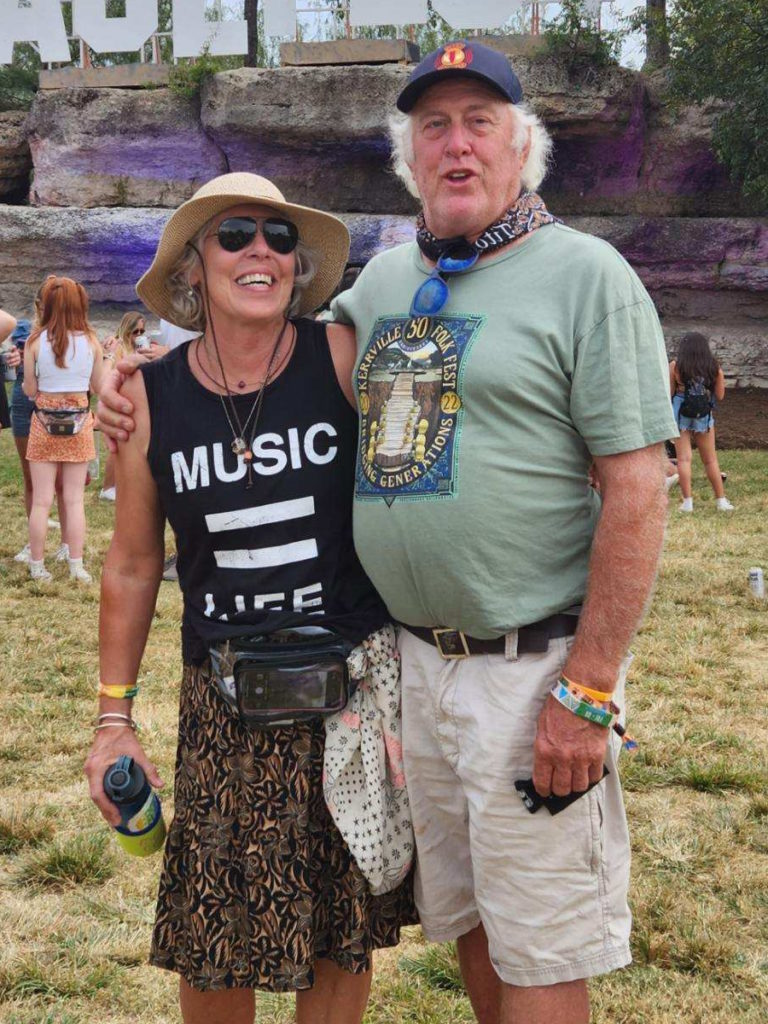
I’ve been with my partner for 13 years. We’ve known each other for longer. At that moment, I needed a person so that I could find out, “Is this reality?”
Anyone that’s ever had this kind of news, it’s hard at that moment to say, “Is this really happening?”
I have tried to eat right, stay fit, [and] do everything to be healthy. I always thought it would be a heart attack or a stroke. I had no idea it would be a tumor that I would have to face.


I felt very alone.
After that appointment, I went to UT Dell Hospital and they did the cystoscopy. Mitch did get to sit in the waiting room there. They did allow that.
When Dr. Laviana told both of us this horrible news, I was glad that he was with me. I needed someone else to hear what he was saying. From that moment on, I realized I needed to always have my phone on me so that it could be a conference call if need be.
A couple [of] days later, I told my daughters, which was really hard. I wanted my daughters, Mitch, and my sister, who has been in medicine — she’s not a doctor or a nurse, but she’s been in the field — to hear whatever the doctor was saying. I needed this support group so it wasn’t me trying to jot down every single fact.
I didn’t cry until chemo. Once chemo hit, then I started feeling sad because the changes were taking place.
Reaction to the diagnosis
Margo W.: I feel so comforted knowing there’s another woman out there who’s been through [something] similar. You want to have as many people close to you as you could. You were jotting down what the doctor is telling you. What was that like for you?
This is a business now. My body is my business. I had run a business and I thought I now have to take care of everything. Even though I’ve got these folks that I’m relying on to listen and hear, I have to make these decisions. No one else is going to make them for me.
He told me, “Yeah, you could just go on with your life, but in five years, you’ll be dead.” My imagination [started] running around. I would jump from, Okay, so I just die. I had a good life. All right. Just throw in the towel and have this horrible cancer in my body. But then I thought, I’m not quite there yet. I still have a lot to do. I don’t know what it is, but I have a lot to do.
My daughters are very important to me. We’re very close. They both live in Austin. My partner and I, we’ve traveled. We have great times. We do a lot of volunteer work. I thought, I need to just keep plowing away.
I don’t think I got depressed. I’ve always found a way to not feel that I can’t handle it. I just told myself this is my new job. My new job is Vickie’s body. Clearly, it wasn’t a good business. I didn’t choose this business. There [are] other things I would have rather been doing, but I just hung in there.
I don’t know how else to describe it. I didn’t cry until chemo. Once chemo hit, then I started feeling sad because the changes were taking place. I didn’t care for the way I felt physically. I didn’t have the energy that I always have. I couldn’t even walk a block down the street and I’m used to walking five miles and hiking.


Treatment
What were your treatment options?
Margo W.: It is interesting how it’s a different journey for everyone. That’s interesting that your go-to was, “Okay, I’m going to project manage this. I’m going to science this,” and I get that because part of us just goes into that mode. How did the doctor present to you what your treatment options were and how did you feel when he told you that?
I remember, he said very quickly, “There’s a couple [of] schools of thought about the chemo regimen. Some people even do radiation.” He handed me the BCAN folder, which, of course, I wanted nothing to do with.
I just thought, Oh, no, I don’t want anything to do with this. It was not that it was scary. It’s just I didn’t really want to read it until I had to. Like for a test.
His idea was, “We’ve got UT Dell Oncology here.” He didn’t mention Texas Oncology. He just started automatically saying, “All of this is right here at this facility.” But he’d only been in Austin for two and a half or three months. He didn’t really know all the resources yet.
The interesting thing was, I did say, “How do you feel about a second opinion?” This is after he’s done a cystoscopy and he’s telling Mitch and me, “You have cancer. This is what you have to do.” I said, “How do you feel about me going to MDA (MD Anderson)? Because I’m going.” And he’s like, “Of course, always get a second opinion.”
I was in excellent hands. [I’m grateful] to have modern science and these two facilities so close to us.
After I told my daughters, I reached out to some friends and one of my friends happened to have aunts and even her grandmother that had bladder cancer and they lived into their 90s. I was like, “Oh, Lord, this is good news.” Then she said, “One of my dear friends from Corpus Christi was diagnosed years ago and she’s about your age, Vickie. You need to talk to her.”
That was probably one of the best conversations I had throughout the journey because Toby is the one who said, “Dr. Kamat, he’s the man. He did my surgery 15 years ago,” and told me exactly what she went through. That was eye-opening.
I got in to see Dr. Kamat and all of those teams of people there. It’s daunting, but it’s amazing, the expertise. Even though I think my doctor is an expert and I’m really glad I have him in Austin, I knew I had these folks and that I was in excellent hands.
[I’m grateful] to have modern science and these two facilities so close to us.
Our mutual friend, Dorothy, and her husband dropped by and brought me the BCAN swag bag. We have the Bladder Cancer Advocacy Network’s coffee cup, brochure, and brochures for the whole family. A wristband that I still wear every day, as does Mitch, my partner. That was really good for me to be greeted into this new community of bladder cancer survivors.
They are my earth angels, Dorothy and John, and the whole BCAN network.

Urinary diversion options
Margo W.: We aren’t innately comfortable talking about bladder cancer. We’re ladies. This is below the belt. We talk about breast cancer. We talk about prostate cancer. We talk about colon cancer.
There is a problem with this kind of cancer being misdiagnosed, especially in women. What I love is that you and I are both willing to go out on a limb and talk about something we don’t especially love to talk about.
The neobladder: did the doctor present that as an option? How was that handled?
I was always going to have the neobladder. I just thought, That’s the only way I can do this. I have to have something that’s not external. I’m so active. I don’t want this extra piece of equipment.
I don’t know what I was picturing. I was picturing another set of organs on the outside of your body. And it’s really not that big.
After seeing Dr. Kamat and that wonderful team at MDA, they were saying the exact same things that Dr. Laviana was saying in Austin.
We had to go [to MD Anderson] twice because the first time, they wanted their very own COVID test. We went down on a Sunday, got the COVID test, turned around, went on a Tuesday, and stayed through that Thursday.
Dr. Kamat, bless his heart. What a physician. He wanted all the tests new. He knew what he saw, but he said, “I’m going to go in and I’m going to see what I find.” All the tests were redone.
He and I talked about neo because Dr. Laviana knew I wanted that. As soon as he told me about the neobladder, I was right on it.
Then Dr. Kamat, his group, and the oncologist there, Dr. Campbell, are looking at me going, “Are you sure you want the neobladder because you’re super active? It takes about a year to ever even figure out how to avoid having these accidents. You’ll be wearing a diaper for at least six months and maybe longer. You will [catheterize] yourself daily.”
I had catheters when I had my children. I am done with catheters. I can’t do that. No, I’m not catheterizing. Up until the day of surgery, Dr. Laviana thought I was going to do it. He said, “Oh, neobladder.” I said, “No, I’m not doing it. Too much.”

Margo W.: What is a neobladder?
It is a piece of your intestine. They cut out the little ostomy. They use part of your colon and create a bladder out of that. It fills up and then you would urinate just the same — theoretically — as you would if you still had your bladder.
However, the problem is, especially with women, they’ve now cut through all of those muscles. They’ve pretty much stripped you of any feeling that your bladder is full. My understanding is that it would take the place [of your bladder], but it’s made out of your own body.
The problem would be that at my age, especially, I don’t have [a] strong muscle reaction to something filling up down there. For me, it just probably would have taken two years to ever get that structure back and not void all over myself.
Two women that I’ve spoken to have neobladders. They were in their early 50s when they were diagnosed and they did tell me how difficult it was.



The third option is the Indiana pouch, which Dr. Kamat recommended not doing [because of] your chances of having infections. That’s the other reason I didn’t want the neobladder.
[With] the Indiana pouch and the neobladder, your chances of having numerous infections the rest of your life, like UTIs, it’s a great percentage.
The last part of that is you can get cancer in your neobladder or the Indiana pouch. I thought, If I’m going to do this, I’m going to try to erase all chances as much as possible.
Margo W.: Can you describe what an Indiana pouch is?
As far as I understand, from the people I’ve spoken with, they also take a piece of your intestine. They’re hooking up your ureters to another piece of your intestine. But instead of it coming out for an ostomy pouch, it stays within your gut.
It is similar to the neobladder, but you do catheterize at least twice to three times a day to void your urine.


Whereas anyone that has an ostomy and the little pouch, you just feel it. “Okay, it’s kind of full. I’m using the restroom,” wherever you are.
Margo W.: Funny question: what’s the best thing about having a urostomy?
I did a five-mile hike in the woods. My friend that I was with [had] to use the restroom. I’m like, “I’ll go and use the restroom, but I don’t have to because I’m out in the woods,” and I just walk behind a tree. There’s no more squatting and I like that.
I like that I don’t have to touch a toilet and that’s the best. My friends all know what my body is now. We all joke about it. “Vickie doesn’t have to use the restroom. She can just go behind a tree.”
I could have gone to the hospital but I liked coming home and being in my little world.
Chemotherapy for bladder cancer
Margo W.: Talk to me about chemo and what you ended up doing. How long you were in? What was that like and how did you feel about it?
The one that I wanted was the dd-MVAC (dense-dose methotrexate, vinblastine, adriamycin, and cisplatin). You go in one day and they give you two of the drugs. Then you go in the second day and they give you the rest of them. That’s for two months, two times a week, every other week for two months.
I went to Texas Oncology. I was very fortunate that Dr. Campbell, the oncologist at MDA, was a resident with Dr. Yorio at Texas Oncology so he actually got my appointment.
I was just about to start it with UT Dell. They didn’t even have the drugs on hand. They were going to have to order it.
They did the port. After a while, especially [with] these drugs, you might have trouble finding that vein.


I picked that one over the other regimen. The other regimen was for four months, I believe, and you do the same thing every other week. However, you don’t lose your hair. It’s not as intense, but I wanted to get rid of this tumor and they said the best way to do it is to use this heavy, dense dose.
Again, I was really glad about modern science because I know that a couple of years ago, and at MDA they still do this, you are in the hospital when you receive your chemo treatments.
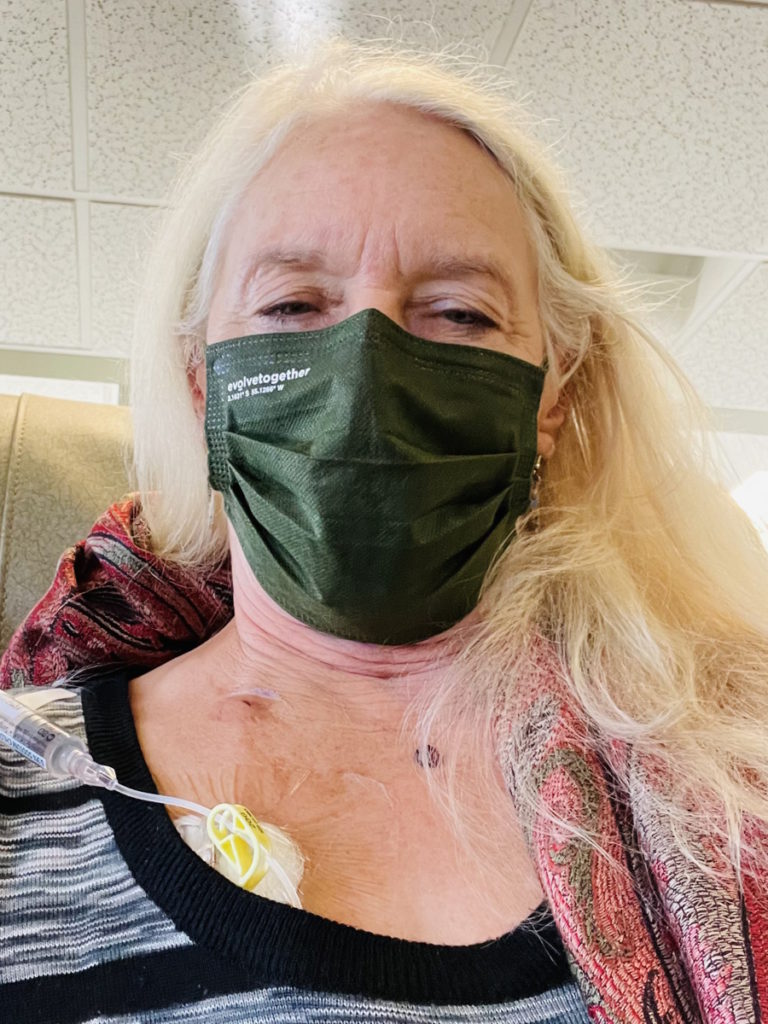
I could have gone to the hospital but I liked coming home and being in my little world. [There] was COVID again and no one could go into Texas Oncology with me. I would just sit there and freeze. It was winter. It was so cold.
Besides the surgery, I think that was the most frightening part of this experience. MDA was daunting and frightening [with] all the tests being done there by myself. Going into Texas Oncology by myself, walking up the steps, and seeing all the patients was very, very, very hard.
I was so sick [that] I couldn’t stand food. Just looking at it…
Side effects from chemotherapy
Margo W.: How long was each session of chemo? How did you feel after?
Day one was about five hours and day two was about eight.
I lucked out. [The] very first day that I went to Texas Oncology, I had a nurse. She was this little firecracker. She was giving me all these facts and saying, “This is what exactly is going to happen. In 14 days, you will lose your hair. In a couple [of] hours, you’re going to feel like this.”
I made this joke about [a] John Prine song where when I go to heaven, I’m going to have a ginger ale and vodka. He has this wonderful song about dying and what’s going to happen when he goes to heaven.
She just said, “I want you to go home and have a ginger ale and vodka tonight.” I was like, “But I’m not drinking. I’m trying to save my organs.” And she goes, “No. You need to because you’re a nervous wreck, I can tell, and this will help.”
I got ahold of my partner and said, “Hey, Mitch, stop at the store and get me a ginger.” I was drinking ginger ale anyway, but it was just funny how that was my first day.
My first impression [was if] this is what it’s going to be like, no problem, right? That first treatment, I went, “Well, that’s not too bad.”
Then I saw that I was going to take seven other pills. Again, modern science [is] amazing. In the hospital, they’re going to give it to you on IV but the second you get home, you start taking these pills and you do that every other week.


I’m taking all these pills. I hate pills, but I’m going to take them. One of them, she said, “You’ve got to take it,” because it was the steroid, I believe. “It’s going to help your immune system. You’re going to feel weird,” and she told me how I would feel and she was exactly right.
I became more ADD than I am. I couldn’t focus. But I was [on] the chemo regimen so I just said, “This is what I have to do.”
Another modern medicine that I just have to be grateful for is anti-nausea because I was so sick [that] I couldn’t stand food. Just looking at it… [On the] third day, [I] was down.
I was lucky because one of Mitch’s brother’s best friends had just gone through the dd-MVAC. He had just had it at MDA and he told me exactly what was going to happen also. “This is how you’re going to feel. Be sure to have some Miralax. You’ve got to have that mouthwash stuff that they’ll mix up for you.”
Margo W.: Did you ever have mouth sores? What was that like?
It was horrible. It was just like my oncologist, Dr. Yorio, told me. He said, “They’re ulcers, Vickie, they’re sores. And if you don’t treat them, you can get infections.”
I did the baking soda salt. Mitch would even mix it up. They add milk of magnesia to it. They pour all this stuff together and you’re supposed to swish it and swallow it because your stomach also has those sores.
Mitch is a great cook. He would fix these meals and I just take one bite and say, “Honey, nuh-uh. I got to have macaroni and cheese if I could even stomach that.”
But my best friend was Mexican Coca-Cola. I don’t even drink Coke but Mexican Coca-Cola was the most soothing drink. I didn’t drink much of it, but it settled my stomach. I felt like I had eaten. It was filling me up. I guess it reacted with those sores because it didn’t hurt to drink it, whereas just water would kill my mouth.
I finished chemo [in] mid-January. I saw my general practitioner in May. He did the blood work [and] he goes, “You know that you’re borderline diabetic.” I said, “Yeah, because I’ve been drinking these Mexican Cokes. I promise I’m getting off of them.” And I did.
I quit cold turkey. I saw them at a store one time and went, “I have to have one.” I’ve got this feeling of I’m going to allow myself to have one. But I got off of them.

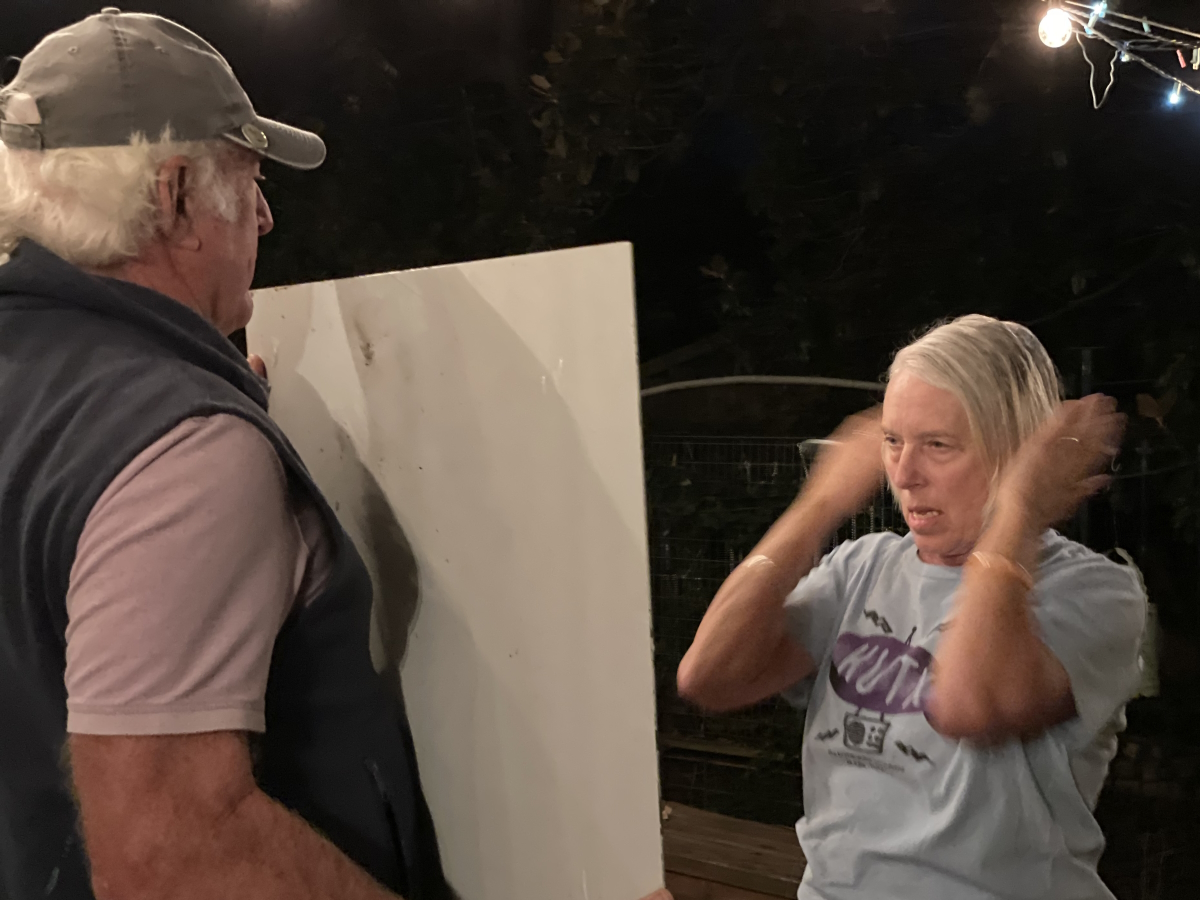


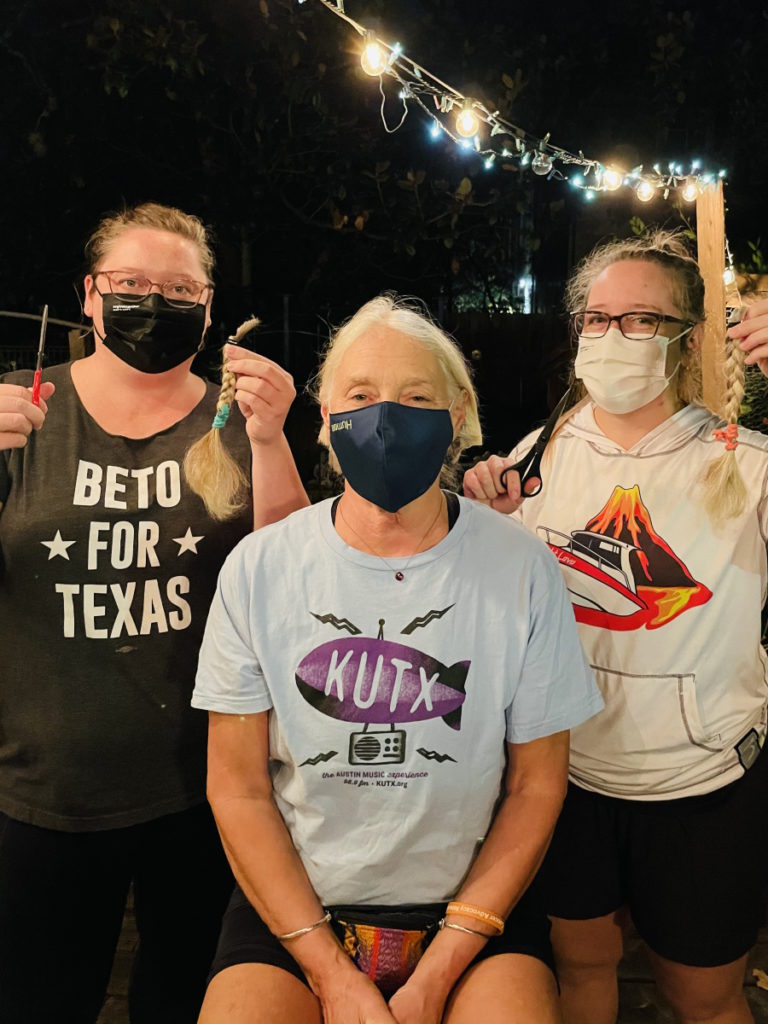
Margo W.: Did your hair start to fall out [on] day 14? What was that like? What did it feel like physically? What did you notice and how did you feel emotionally about it?
I had long, long hair and put them in braids one day. We picked the day. I think it was week two. I’d had chemo. I was feeling good because [by] week two, I always felt almost normal.
My daughters came over. They each took a braid. They cut it off. Then one of my daughters styled my hair. Once they cut the braids off and I had short hair, I didn’t notice the hair coming out as much. We did a punk ’do. The girls came over and we just hacked on it. You could see then that I was going bald and so that’s probably 21-28 days.
Finally, I just said, “Mitch, give me your buzzer. I’m buzzing it. I can’t take it. I don’t want to see these hairs on the floor. I don’t want to see them on my body.” I buzzed it, he buzzed it, and then I just started wearing scarves and hats all the time so I don’t have many photos without a hat or a scarf on.
It was challenging because I always did the bun, the braid, and the ball cap. I just tucked it up and off I went and did my thing so it was weird to not have hair.
This is fun now. It’s fun to have short hair. I don’t think I’ll grow it long ever again. I think I’m going to stay with this because I think I’m so different myself that I don’t really want to have that look that I had. I’m from a generation where we grew our hair and never cut it. I’ve had hair down to my rear end, but now, I just go, “Eh, I’m different now.”
Exactly six weeks after my surgery, when I could start exercising again, I was out there doing everything I could to get my physical strength back.
Self-image and cancer
Margo W.: Personally, I had to wrestle with who am I if I’m not a woman with long blonde hair, which sounds shallow, but it’s a part of who we are. Did your sense of identity change? What did you go through when that was happening?
Yes. My identity of being the strongest person in the room like, “I am strong. I can do anything,” was not that anymore. I felt like, “How can I guide anybody?” People come to me for information and guidance and I thought, I guess I’m not that person anymore, but I’m kind of getting it back.
My children and their friends rallied behind me. They come to me and I was freaking out. I thought, How am I going to help these young people if I am so ill?
Exactly six weeks after my surgery, when I could start exercising again, I was out there doing everything I could to get my physical strength back. Just getting older is scary because I don’t have the balance I used to have. I practiced yoga for over 20 years and I had the best balance around and now like, “Oh, I could fall over.”
When people say they fought cancer, that’s great. I don’t think I fought cancer. I wanted it gone. I didn’t want that to be my identity. I wanted it to be more of, “Okay, everybody, I’m here. I’m who I used to be. I may look different,” because I have to tell myself that. I’m not the same.
Live your life now.

Life after cancer
Margo W.: You have [a] presence and I can tell how you’d be an instant leader and encourager of other people. What’s different now? How are you different now after this journey?
I have this little statement in my home office: “Live your life now.” My personality was always, “I’m going to live my life, but I have to get all these other things done.”
I make my bed every morning. I’ve always believed in it. It feels good to me to say, “Okay, I’m actually out of the bed. I’m actually going to make the bed.” I may stay in my jammies in my room for a while and drink my coffee and I go into my day.
I’m a little less “got to get going.” I’ll sit and look outside. I don’t meditate, but I do try to hear those birds singing or the squirrels running around on my roof. I’m going into everything a little less hurried.
I am trying not to be as negative as I used to be. I don’t want to find fault with things. When I catch myself going, “That was not so good,” I’ll go, “Oh well.” And that’s what I say. “Oh well. That’s not important.”

Living intentionally
Margo W.: I think that’s magnificent. You are now living better than you have before because that sounds very intentional to me. Tell me more about how that feels to be able to be in the present. Being intentional and present is hard.
It is, especially for me. I’m just always looking at what’s next, what’s next, what’s next. I still am that person, but I’m not as apt to think that everything has to be in its place.
I used to think I can’t even enter the room unless all this stuff is organized, put away, and everything has to be in its place. So there [are] a couple of things out of place. I’m okay with that.
To me, the word “now” is better than saying I’m in the moment. I’m trying to enjoy being out in the woods. I want to do more hikes. We’re surrounded by great trails here in Austin.
I’ve been trying to ride my bike more. I like volunteering. I was already doing Meals on Wheels, Keep Austin Beautiful, and other little town cleanups. But now it’s, “What else can I do? Where else can I get out of myself and help someone else?”

I still have major anxiety about bad news from a doctor… Now, when I go into these tests, I just have to say I’m going to be accepting.
Follow-up protocol
Margo W.: That’s so cool. Are you cancer-free today?
I’m tested every four months. The first was [at] one month and then the three-month test. The six months is what I’m looking forward to.
Dr. Laviana, every time I get my test results, he’s like, “Oh, I told you. It’s gone, Vickie. We destroyed it. It’s gone.” Talk about an optimist. I hope.
Everybody has that scanxiety. I don’t care at all to look at my calendar and see what the date is. It’s coming up, I just know that.
Dealing with “scanxiety”
Margo W.: The sign in your office says, “Live your life now.” How do you think this experience — getting rid of cancer and all the extreme measures you had to [do] — has changed how you approach every four months [when] you’ve got to go back and find out if you’re still cancer-free or has it?
I don’t think it’s changed. I still have major anxiety about bad news from a doctor.
Everyone that has to go through this, you look at your history and [say], “I made it through that. I made it through this. I made it through that. Wow, I can’t believe I did that.”
I did 10 triathlons. I’ve done all these things and I would have done more but I said 10’s a good number because it does involve a lot of training. That’s a lot of hours in my life training.
Now, when I go into these tests, I just have to say I’m going to be accepting. Obviously, there’s nothing I can do about it. I’m nervous going in. My blood pressure is probably super high.
Then I wait for those results. They come on my phone. I see them. I go, “Okay, Mitch, I’m going to read them right now. I’m just going to go [to] the office to sit down. I don’t want to be in bed reading this stuff.”
I start to read through it and go, “Wow. These are good numbers. It says they don’t see anything new in my lungs and other organs. Whew. I made it through another one.” I look forward to that day. I love hearing from people like you and Dorothy. Just positive that it’s gone.
Margo W.: Surreal experience. It’s an overused term, but it really does apply. As you’re walking around going to doctors and doing chemo, did you ever feel out of body? Like, “Is this happening? I feel like I’m walking in somebody’s physical body, but it’s not really me.”
Every time I get scanned. When they put the iodine in, first, I’m grateful that I can have iodine. I’m like, “Wow, at least I’m not allergic to that.” Then the next thing is, yes, I don’t know where I go, but I do feel like it’s not me, it’s somebody else’s body.
I’m going to come out of here in about an hour, an hour and a half. I’ll get my car and drive away. But each time, especially that scan.
I’m always grateful for science. I say thank you very much so we have the science and the machine that can look for these things.

Being grateful is a coping mechanism for me.

Coping with cancer
Margo W.: I love that you’ve said often throughout our conversation that you’re grateful for things. You’re grateful for science, grateful for medicine, grateful for doctors. Has gratitude always been part of your coping skill?
Yes, I think I’ve always been. I have a temper and I could get angry super fast, but then immediately I go, “Okay, I am grateful because that wasn’t a big truck. That truck almost hit me right as I’m cursing him out.” That’s where I go immediately after something gets my feathers ruffled. Being grateful is a coping mechanism for me.
Words of advice
Margo W.: It seems like you’ve come through a journey that left part of you behind and yet the core part of you is enhanced. What would you share with anybody facing a health challenge like you’ve been through or really any difficulty?
Taking the information that’s given to you. The doctors are giving you information. Hopefully, you’ve got a friend group that’s supporting you.
My sister gave me this wonderful binder. It’s like a baby journal that had pages in little envelopes that you could slide things in, like business cards. I would take that. This helped me through the very beginning. Every once in a while, I’ll pull it out and add something, especially if I meet someone.
I really believe in writing it down. It doesn’t have to be journaling. It’s more of information and who’s helping me.
I realized I had people on a list that I was keeping abreast of what was going on. I did not put it on Facebook. I wanted these people to know that I was doing okay because they were going to hear about it and then I would get information from them. Stay informed.
Everybody has said, “You’re a warrior.” And then, “Oh, by the way, I’m going to drop off cookies,” or “I’m going to do this,” or “What do you need done?” That support is what carried me through even though I’m independent.
My mother, if she were alive, would probably say, “Oh, Vickie let you do that? Wow. She allowed you to?” My mom would have said, “How did you become so reliant on folks?”


Importance of a support system
Margo W.: It sounds like you’re talking about how valuable the connection and the support from your community [is]. It had to look different during COVID. But it sounds to me like you knew, at the time and now still do, the value of that community and support.
If I were sitting with someone that had just been diagnosed, have your friends, family, and connections. I know that’s what church is for. I know that’s what we’ve had in the past in our culture. That’s what’s gotten a lot of people through all these hard times.
Just to have those people, even though they couldn’t see me. [For] anyone that had to go through any kind of health crisis during COVID, it was especially difficult because you couldn’t have those loved ones with you.
Margo W.: Would you say that having a phone call or a FaceTime call with people you care about is as good as seeing them in person?
We have relatives in South America and Mitch’s son lives down in South America with three of the grandkids. They’re like mine. I just am in love with these children. We do WhatsApp with them and so I was already accustomed to doing WhatsApp before COVID.
When COVID hit, it wasn’t the same and I don’t think it can be the same, but thank goodness we have it.
I was imagining all the phone conversations I had with my children. They’re listening to the doctor give us all this news. My girls are listening to everything. Mitch is in the car listening. If we didn’t have that technology and I was by myself in there, jotting notes down, trying to remember everything, how do I tell them this is what I’ve got to process?
It is important to have Zoom and everything. But no, I don’t think it’s anything like having anyone in your house and saying, “Hi, come by for dinner,” or meeting them at a restaurant.


Margo W.: It’s a distant second, but it’s better than nothing.
It is.
Margo W.: What was it like when people wanted to bring you meals? Across multiple cultures, this is one of the things we know to do when things are tough for people. What did that look like during COVID?
That was hard. I really didn’t want anyone to put out. I did not want them to have to cross town. I didn’t want to have them come over, especially since they weren’t getting out anyway.
I would just say, “I’m going to peek out and say hi and hugs to you,” and they would leave it on my porch so we would have social distancing. What a difficult time.
I would accept what I could, but a lot of times, I would say, “Please, please, please, please just take care of yourself. Be safe. I love you. Thank you for thinking of me. When this is all over, we will get together and you can fix me a meal.”


Margo W.: Is there anything else you want to share with people who are dealing with any part of this journey?
You must advocate for your body and for your family. You have to show up and tell them you’re not going to be blown off because that’s what it felt like. It’s a terrible journey.
As you have these tests or whatever they’re recommending, if it doesn’t sound soon enough, I say keep pushing it. Get in there. Go for it.
I remember seeing my general practice physician in February 2020. I went back to him and said, “Why didn’t you do a urine test that day?” He said, “You were in a hurry.” And I said, “I was not in a hurry. You’re a doctor. What are you talking about?” He goes, “No, no, no, I don’t think we did it because you said that you’re in a hurry.” And I was like, “No, I don’t like that answer.” So, of course, he’s not my doctor anymore.
COVID was hitting and I think everybody was afraid to keep you in the office very long because it was right before everything shut down. And that, I realized, was a turning point where I could have stood up for myself and said, “Hey, don’t you do a urine test? Isn’t that part of the physical?” Because that was my physical. That’s why I went in that day.
No matter if you’ve been diagnosed or not, you must advocate for yourself. I remember always thinking, I don’t want to insult the doctor. I can’t tell them what to do. But I do believe you need to stand up for yourself.

Be your own advocate. Don’t let them blow you off.

Margo W.: I think that’s a really good observation. We do have this reverence for doctors [and] rightfully so. They’re in school forever and they know a lot more than we do. But the bottom line is it’s our body. We have one.
I love that you’re advocating for advocating. We need to be willing to be uncomfortable with whether we think we are hurting their feelings or disrespecting them because in your case, advocating for yourself helped save your life.
I don’t have a clue what would have happened if I hadn’t said, “I need to see another doctor. If you’re saying it’s not a UTI, get me the name of that next doctor.”
I really believe in second opinions. If you’re not feeling like this is the right answer, you’re probably right. It’s not the right answer. They’re not giving you the information that you know your body is telling you that something’s the matter.
If I had a class on cancer, that would be one of the first 101. Be your own advocate. Don’t let them blow you off, especially when you’re an old lady.
Margo W.: Regardless of your age. Advocating for ourselves is really key. I don’t think it’s 100% natural for a lot of women for a million reasons.
Thank you so much for sharing your story. It’s heartwarming to hear your story and I’m so glad you’re cancer-free as far as we know right now.


Inspired by Vickie's story?
Share your story, too!
More Bladder Cancer Stories
Laurent Gemenick, Bladder Cancer
Symptom: Presence of blood in urine
Treatment: Surgery: transurethral resection of bladder tumor or TURBT
Jon T., Locally Advanced Muscle-Invasive Bladder Cancer
Symptom: Darkening urine, blood in urine, dull right flank pain
Treatments: Surgery(transurethral resection of bladder tumor or TURBT), antibody-drug conjugate, chemotherapy
Michael V., Bladder Cancer (Non-Invasive High-Grade Papillary Urothelial Carcinoma), Stage 1
Symptoms: Frequent urination, burning sensation when urinating
Treatments: Surgery (transurethral resection of bladder tumor or TURBT), immunotherapy (Bacillus Calmette-Guérin or BCG treatment)
Dorinda G., Bladder Cancer
Symptom: A significant amount of blood in the urine
Treatments: Surgery (transurethral resection of bladder tumor/TURBT, surgery for papillary lesion), immunotherapy (BCG), chemotherapy
Healing Together: A Mother and Daughter Navigate High-Grade Bladder Cancer
Mary Beth’s story about caregiving starts with an important awareness message about female bladder cancer symptoms.
Danny G., Non-Muscle Invasive Bladder Cancer
Symptoms: Fatigue, back pain, erectile dysfunction, nausea
Treatments: Surgery (transurethral resection of bladder tumor or TURBT), chemotherapy, immunotherapy