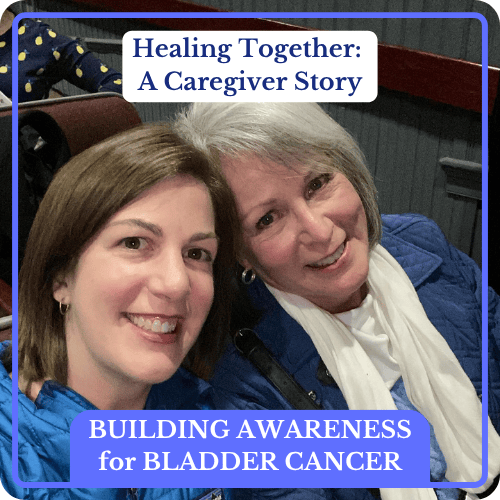
Healing Together: A Mother and Daughter Navigate High-Grade Bladder Cancer
The Many Faces of Bladder Cancer: Voices of Strength and Resilience
Subtle female bladder cancer symptoms—a faint trace of blood in the urine and nagging UTIs that didn’t respond to treatment—triggered 28-year-old Mary Beth’s diagnosis. Our series, The Many Faces of Bladder Cancer: Voices of Strength and Resilience, completes with a story of an adult daughter battling high-grade, non-muscle invasive bladder cancer (NMIBC) and her mom’s dedication as her caregiver. These powerful stories highlight the experiences and the challenges faced by bladder cancer patients and survivors. This series intends to foster hope, understanding, and a fresh outlook on dealing with this condition while raising bladder cancer awareness.
When Mary Beth was diagnosed with high-grade non-muscle invasive bladder cancer (NMIBC) at 28, the news came as a total shock, not only to her, but to her whole family.
It started when she noticed a little blood in her urine. At first, she thought it was a minor issue, like a urinary tract infection or her menstrual cycle. But when the bleeding returned intermittently despite treatment for UTI, she trusted her instincts and saw a urologist, even though the symptoms had mostly disappeared. [note: these are both signs of common ailments and female bladder cancer symptoms. It’s important to get checked}
That decision changed everything. A quick in-office procedure revealed tumors and after surgery to remove them, Mary Beth received the difficult diagnosis: high-grade non-muscle invasive bladder cancer. The initial consult felt cold and overwhelming, so she sought a second opinion at Vanderbilt University Medical Center, a move that made all the difference.
Throughout it all, her mom, Mary, stood by her side and offered steady emotional support. A retired nurse, Mary showed up for the weekly treatments, cooked meals, created calm, and just listened. Their relationship deepened as they moved through this life-changing experience together.
Mary Beth highlights the vital role caregivers play, not only in helping manage logistics and appointments but in creating a healing environment. Through her connection with Imerman Angels and the Bladder Cancer Advocacy Network, she became a mentor to other young women navigating high-grade bladder cancer. That sense of shared experience brought purpose and healing, allowing her to give back while continuing her recovery.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make treatment decisions.
Thank you to Imerman Angels for their partnership. Imerman Angels is here to provide comfort and understanding for all cancer fighters, survivors, previvors, and care partners through a personalized, one-on-one connection with someone who has been there.
Interviewed by: Nikki Murphy
Edited by: Katrina Villareal
- Introduction
- Red Flags I Noticed Before My Diagnosis
- Getting the Official Diagnosis
- Hearing the News from My Parents
- Discussing My Treatment Options
- Getting a Second Opinion
- My Mom’s Role in the Treatment Decision-Making Process
- My Treatment Regimen
- The Importance of Having My Mom with Me During Treatment
- How My Mom Felt Seeing Me Go Through Cancer Treatment
- Discovering Imerman Angels
- What My Mom Didn’t Know While I Was Going Through Cancer Treatment
- Cancer’s Impact on Our Relationship
- My Advice to Fellow Bladder Cancer Patients
- My Mom’s Advice to Fellow Caregivers
I noticed blood in my urine… there wasn’t that much blood, so I didn’t think much of it.
Mary Beth
Introduction
Mary Beth: I was diagnosed with bladder cancer in 2014. I’m a mom of two boys. We live in Danville, Kentucky. My friends and family would describe me as a social, outgoing person who loves to make new connections. I’m very curious and a lifelong learner, interested in expanding and exploring the world around me in any way I can.
Mary: I’m Mary Beth’s mom. My friends and family would describe me as curious, creative, social, and fun-loving.


Red Flags I Noticed Before My Diagnosis
Mary Beth: In the fall of 2013, I noticed blood in my urine. I was with my mom when I first noticed it. We were at a family member’s wedding at that time. I thought it was weird, but we were busy and there wasn’t that much blood, so I didn’t think much of it. I thought I had a urinary tract infection (UTI) or was starting my menstrual cycle. I was experiencing it intermittently.
A few months passed and I noticed that it wasn’t going away, even though I had been treated for a UTI. I decided to make an appointment with a urologist to have it checked. I almost didn’t go because I stopped seeing the blood at all. My urine was a teeny bit pink, so it wasn’t alarming. I almost canceled my appointment because it was gone that week, but it was a good thing I didn’t.
I lived in Nashville at the time. I went to see the urologist and he scoped my bladder in his office. He could see that I had tumors in there and wanted to have them removed within a few days. I proceeded to have an outpatient laparoscopic surgery to remove the tumors he saw.
She’s awfully young… She didn’t fit the medical picture that we were familiar with.
Mary
Getting the Official Diagnosis
Mary Beth: A few days later, I received the diagnosis from his office. They told my parents first because they wanted to know what was going on. My parents told me that I had cancer. That was a hard day.
At the private practice I went to, they did a CT scan on the same day I got the scope done. They also did a test that showed a lot of microscopic blood in my urine.
There was a waiting period after the biopsy. That was in February 2014. I remember the day. It was storming outside, which was unusual for February.

Mary: We were in Danville and she was in Nashville. This happened through a phone call. Her dad is a retired physician and I’m a retired nurse, so we have a medical background. He primarily got the report. If I remember correctly, he talked to her and I talked to her after that.
We were shocked, to say the least, because there’s no cancer in our families. She’s awfully young and in our experience, bladder cancer typically is for a heavy smoker and usually a middle-aged to old age man. She didn’t fit the medical picture that we were familiar with.
I knew she was very upset. I tried to calm her as best I could on the phone, but that doesn’t help when you’re in shock at something that you were not expecting at all. We all felt like it was an emotional blow.
Her dad and I felt that treatments were the answer and that this could be taken care of. At that time, we were trying to help her cope emotionally, which wasn’t easy because we weren’t in the same town.
All I can remember from that initial consult was the percentages of my cancer getting worse or coming back, which was overwhelming at the time.
Mary Beth
Hearing the News from My Parents
Mary Beth: I was glad that they talked to me about it. It would have been harder if I had gotten the news in the doctor’s office. I felt grateful that I got the news that way because it was softer.
I was thinking, “How did this happen? What could have caused this? How bad was this going to be? What do I need to do next?” I was shocked. I couldn’t believe that it was me that they were talking about. It felt like an out-of-body experience.

Discussing My Treatment Options
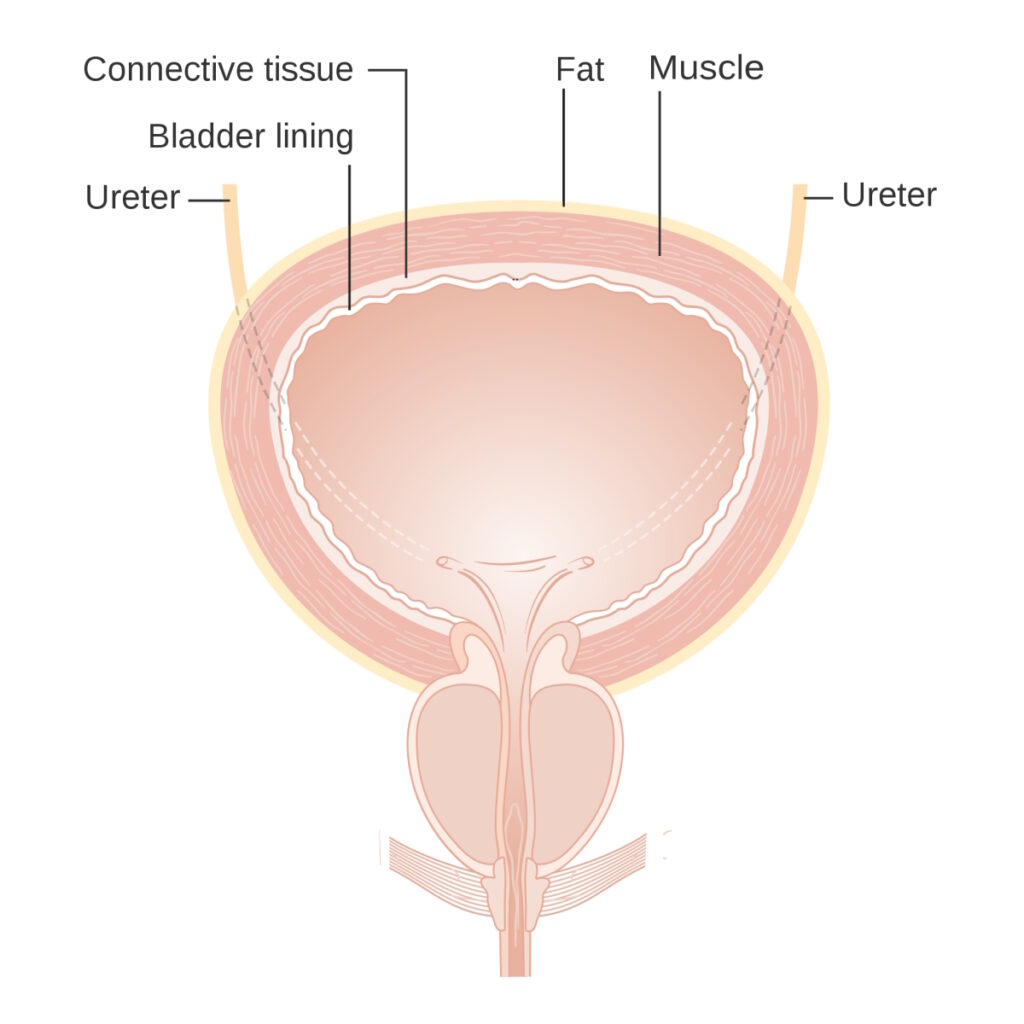
Mary Beth: It was a pretty intense appointment. He talked about how I could do the first line of treatment, which would be BCG immunotherapy. He also talked about bladder removal (cystectomy). He talked about how my bladder cancer was high grade and the type to recur, and how the odds of it coming back were high. I felt bladder removal was more on his mind for me, so that I wouldn’t have to keep dealing with it. I also think there were other chemotherapies I could mix with that.
There were a few different options, but all I can remember from that initial consult was the percentages of my cancer getting worse or coming back, which was overwhelming at the time. Truthfully, it wasn’t warm and compassionate. I decided to get a second opinion.
We felt she was in the best hands. You could tell that he cared about her and was doing all he could to help her.
Mary
Getting a Second Opinion
Mary Beth: I got a second opinion with Dr. Sam Chang and his team at Vanderbilt University Medical Center. He was awesome from the beginning. He talked about a long continuum of what could happen, from BCG to bladder removal. He talked about how we could start with the basics and see if that works. He was very good about bringing it back to the next step. It wasn’t as overwhelming. He was also a very warm, personable, and compassionate man.
I decided to do BCG at Vanderbilt. I immediately switched my care and records over to Dr. Chang. I immediately felt better because there was a shift in the delivery, energy, and research by the medical team at Vanderbilt.
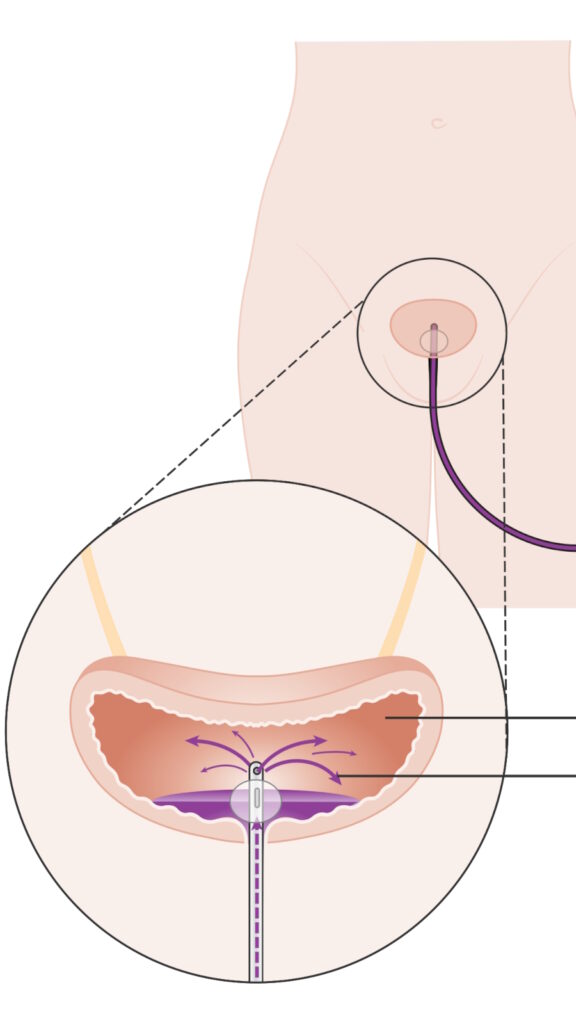
He was using cutting-edge technology for bladder cancer at that time, which was called Blue Light Cystoscopy (BLC®) with Cysview®. He could perform the procedures using an agent that lights up the cancer cells, almost like a black light, so he could see them more clearly and remove them more easily compared to a normal white light procedure, which is what most urologists offer.

My Mom’s Role in the Treatment Decision-Making Process
Mary: As a surgeon himself, my husband took the reins with her at the appointments or at least to hear about her options. He took care of the medical aspect of what they were proposing. I was the emotional support and went with her to treatments because he was still practicing at that time.
I was able to stay in Nashville and accompany her to the clinic and help with anything we could do to help at home, so that she could take it easy. That was my main function and where I could help the most, whereas he was more aware of the technical side.
We liked Dr. Chang so much. We felt she was in the best hands. You could tell that he cared about her and was doing all he could to help her, which helped her get through all this.
By October, he didn’t find any cancer. There was no evidence of disease.
Mary Beth
My Treatment Regimen
Mary Beth: After I was diagnosed in February 2014, I had another transurethral resection of bladder tumor (TURBT) in March. Dr. Chang waited a month or so to let my bladder calm down. I did the BCG treatment, which was six weeks of weekly treatment. Afterward, he did another TURBT to check. I waited a longer period and then had three more treatments.
Then I was moved to maintenance treatment. He saw a little bit of cancer remaining after my first six-week treatment, so he looked again and took out a little bit more that he could see. I went on maintenance treatment after those three weeks, waited, did another TURBT, and by October, he didn’t find any cancer. There was no evidence of disease. I consider October 2014 as when I was cancer-free, but I continued to do maintenance.
I had another three-week round and another TURBT in January 2015. It was still clear. I did more maintenance treatment and had my last one in the spring of 2015. We were monitoring and did imaging every three months and then progressed to every six months. In 2016, he said I was good. We wanted to have children at the time and he gave me the green light.
From the diagnosis to the end of treatment was a two-year period. I didn’t have to do chemo. With bladder cancer treatment, there are different combinations they can do, but the BCG worked, which was the least toxic. It left my system when I was done. It was not a fertility concern, which was great.

The Importance of Having My Mom with Me During Treatment
Mary Beth: My treatments were on Friday afternoons. I worked a full-time job and would take Friday afternoons off to get the bladder installations in the clinic.
My mom would keep me company. I had to wait a long time to go in and get the treatment. Then I had to wait a little more, having it in my bladder, before I could leave. Sometimes my mom drove me, but other times she was there to accompany me then we would go back to my house.
I needed to hold the BCG in my bladder for two hours for it to work, which could be challenging, especially when you have sensitivity. It can be very uncomfortable. After two hours, I would go to the bathroom and let the BCG go.
I would have a pretty sensitive bladder for 24 to 48 hours. There was a lot of stinging, burning, and a frequent urge to urinate. I would try to take it easy and have fun, like watching TV, eating good food, and trying to enjoy myself as best I could to distract myself from it. We would usually do something fun that weekend, but those were six weeks in a row.
By my fourth or fifth treatment, I felt like I had the flu. I felt tired and achy, as if I had a low-grade fever, but not to the point where I couldn’t go to work or do things. I just had to rest a lot more.
At the time, I was 28, so I wanted to be active. I’m a pretty energetic person, but I was forced to take it easy on the weekends. My mom was good about hanging out with me and doing low-key activities.
I would let her energy and desires drive whatever we would do or not do. I kept her comfortable and distracted.
Mary
How My Mom Felt Seeing Me Go Through Cancer Treatment
Mary: Being a nurse, a clinic environment and patient care are very familiar, so it wasn’t as intimidating or frightening as it might be for a lay person. When we would get back to her house, I would make some food and we would watch movies. We might walk a little bit in her neighborhood — she had a beautiful neighborhood. But mainly, we hang out. I would let her energy and desires drive whatever we would do or not do. I kept her comfortable and distracted.
We love good old movies, so we watched movies and spent time together. Simply being there made a big difference to us. When she didn’t feel like doing anything, we let her rest, and I would cook, clean, or do whatever needed to be done.


Discovering Imerman Angels
Mary Beth: When I was diagnosed in 2014, especially that spring and summer, it was difficult to feel positive because I was worried and frightened. It was also hard because my family and friends were worried about me. I decided to join a walk for bladder cancer awareness in Lexington, Kentucky, with a lot of my family members and friends, and it was great.
Nashville doesn’t have a bladder cancer walk, and I thought we should because we have a huge medical community and great urology programs. I worked with the Bladder Cancer Advocacy Network (BCAN) to start the walk in Nashville in 2015. At this point, I was through the worst of my diagnosis and treatments.
Helping other young women who are dealing with this diagnosis helped me heal as well.
Mary Beth
It put me in an advocacy mindset about sharing my story and helping others. I found ways to connect as a patient advocate. Imerman Angels came up immediately when I was searching for that type of work and outlet for myself. Helping other young women who are dealing with this diagnosis helped me heal as well. I connected with them.
Every time I had a phone call or matched with another patient, I felt great being able to answer questions, share my story, and help them. I did the same thing with BCAN, which has a patient advocacy program. If there are others, I’m all about signing up as a mentor and a person to chat, but Imerman Angels has always been very professional and on top of how they match and follow up. It’s been a good experience for me for sure.

What My Mom Didn’t Know While I Was Going Through Cancer Treatment
Mary Beth: Sometimes, I didn’t show how scared I was. I expressed how grateful I was that she came, but I want to reinforce that. It was a huge time commitment on her part to drive three hours to see me and spend time with me. They were even able to get a place in my neighborhood so they could be close by. To be spending so much of her time away from her other responsibilities was a major time commitment and I appreciated that.
I needed the caretaking, but I also needed a lot of positive energy. My mom is very upbeat. She tries to help with peace, hope, and faith. She’s a very spiritual person, and the spirituality that she brought and the conversations that we had during that time helped me get through. It was impactful to me, so I started my own journey.
Mary: I was sure she was scared, but she was brave. It’s very devastating emotionally and physically, but I felt like she would get through it and be cured of it. I also knew that if looked at correctly, this could teach her a lot about her inner strength and spiritual strength. I felt like we had the same goal. Whatever she shared with me was something for me to learn from, too.
We connected on a deeper level… It’s been very valuable for us to know each other deeply through a crisis where we came together.
Mary
Cancer’s Impact on Our Relationship
Mary Beth: The experience brought us closer. I was going through it as an adult, but I also needed some guidance. We were not communicating as frequently or spending as much time together, but that time helped us bond more. One of the bigger things out of the whole experience was having a genuine time to connect.
Mary: I would agree. Her brother married and moved away, so I’m not involved in his life frequently. When she moved to Nashville, I thought it would be the same pattern. Your children have flown the coop and are setting up their nests, and you’re visiting and enjoying being with them.
This was the call to come to her aid. Since she went away to college and got married, she has never lived with me again. It was a time for us to get to know each other as women, not just as mother and daughter. As time goes by, I’m going to need some help from her.
We connected on a deeper level. I don’t think that would have occurred if she continued to live in another state. It’s been very valuable for us to know each other deeply through a crisis where we came together.


My Advice to Fellow Bladder Cancer Patients
Mary Beth: The biggest thing that I can say is to advocate for yourself. When you know something’s not right, follow your gut instinct and persist through the medical system, though it can be challenging and confusing. Seek out other opinions. You don’t have to do this one certain way. Be open to other modes of treatment.
Expand your sense of care to family and friends who want to be there for you. Don’t feel like you have to be strong all the time. Allow yourself to feel vulnerable. You can feel scared and sad. Getting the help that you need to move through those feelings and finding the pathway that fits you best is a process.
Don’t feel like you have to be strong all the time. Allow yourself to feel vulnerable.
Mary Beth
At that time, I was in a place where I could explore different avenues to help me on all levels: mind, body, and spirit. I felt very fortunate. I encourage anyone going through this to be open to asking others who’ve been through it themselves to know that they’re not alone.


My Mom’s Advice to Fellow Caregivers
Mary: Listen to your family member or friend because they’ll tell you what they need, even though sometimes they might not tell you directly. The doctors will give instructions post-treatment, but being with somebody who can care for you is powerful and healing.
Be there for them. Don’t take away their autonomy of how they want to go through this. Be a sounding board. Your fear will probably make you want to fix them quickly.
The lessons are there for both of you. If you can meet them where they are and go through it with them, the experience will have many blessings, even though it doesn’t seem like it on the outside. It could be the best thing.
Be there for them. Don’t take away their autonomy of how they want to go through this.
Mary
Mary Beth: I remember participating in these walks, which were positive experiences and a focus for me for those two years that I was in the thick of it. I could gather my family and friends, and do something positive. It shifted the energy and focus from me to a bigger picture, being a part of a larger community and a larger cause.
It took away a lot of focus on what might be going on with me. I didn’t do it as an escape but more to shift the energy. It worked because my parents were involved. We had family and friends come from out of town. It helps to find the larger connection with others during a difficult time. You’re not alone. You can be connected through challenge.

Thank you to Imerman Angels for their partnership. Imerman Angels is here to provide comfort and understanding for all cancer fighters, survivors, previvors, and care partners through a personalized, one-on-one connection with someone who has been there.
More Bladder Cancer Patient Stories
Laurent Gemenick, Bladder Cancer
Symptom: Presence of blood in urine
Treatment: Surgery: transurethral resection of bladder tumor or TURBT
Jon T., Locally Advanced Muscle-Invasive Bladder Cancer
Symptom: Darkening urine, blood in urine, dull right flank pain
Treatments: Surgery(transurethral resection of bladder tumor or TURBT), antibody-drug conjugate, chemotherapy
Michael V., Bladder Cancer (Non-Invasive High-Grade Papillary Urothelial Carcinoma), Stage 1
Symptoms: Frequent urination, burning sensation when urinating
Treatments: Surgery (transurethral resection of bladder tumor or TURBT), immunotherapy (Bacillus Calmette-Guérin or BCG treatment)
Dorinda G., Bladder Cancer
Symptom: A significant amount of blood in the urine
Treatments: Surgery (transurethral resection of bladder tumor/TURBT, surgery for papillary lesion), immunotherapy (BCG), chemotherapy
Healing Together: A Mother and Daughter Navigate High-Grade Bladder Cancer
Mary Beth’s story about caregiving starts with an important awareness message about female bladder cancer symptoms.
Danny G., Non-Muscle Invasive Bladder Cancer
Symptoms: Fatigue, back pain, erectile dysfunction, nausea
Treatments: Surgery (transurethral resection of bladder tumor or TURBT), chemotherapy, immunotherapy
Bladder Cancer Resources
Bladder Cancer Causes & Symptoms
Understand common bladder cancer causes, urine color, symptoms, and treatments as described by real patients.
...
Bladder Cancer Series
Bladder cancer patients Ebony & LaSonya talk about their cancer journey, including their first symptoms, how they processed their diagnosis, treatment options, and how they found support. Dr. Samuel Washington, a urologic surgeon, also gives an overview of bladder cancer and its treatments.
...
Diagnosis and Treatment for Bladder Cancer
Learn about the diagnosis and treatment process from bladder cancer survivors and medical experts. Discover diagnosis and treatment options./p>
...