LaSonya’s High-Grade Bladder Cancer Story

LaSonya was diagnosed with high-grade bladder cancer. As a nurse practitioner, she used her experience to do her own research so that she knows that she’s getting the best care possible.
She shares the importance of listening to your body and advocating for yourself, seeking the care you want and deserve, and getting all the information you can to make the best decision for yourself.
The interview has been edited only for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Name: LaSonya D.
- Diagnosis:
- High-grade bladder cancer
- Symptom:
- Blood in urine
- Treatment:
- BCG immunotherapy
- Cystectomy (bladder removal surgery)
Listen to your body. If you feel like something’s not right, it’s not right.
Pre-diagnosis
Introduction
I am a variety of things. I’m a black woman, but I’m also a mother [and] a wife. I am a professor of nursing. I am a nurse practitioner of both family and women’s health.
When did you start feeling that something wasn’t right?
I’m really in tune with my body. If something is off, I find out what’s going on right away. I don’t waste time trying to figure things out.
I had just recovered from an elective procedure and was getting ready to go back to work. One day, I noticed blood in my urine. It seemed like it was a lot of blood. I saw some blood clots and I was thinking, I know I’m not on my menstrual cycle. What is going on? Maybe it’s something from my surgical procedure. Although it was time for me to go back to work, [my surgery] had been a month prior.

I called my surgeon and he said, “It doesn’t seem like something related to your surgery, but we’ll go ahead and have you do a urinalysis and see if you have a urinary tract infection.” I did that [and] it came back negative for infection, but positive for blood.
He said, “You need to follow up with your primary doctor.” Fortunately, I used to work for my primary doctor so I know her well. I called her on her cell phone and she said, “Why don’t you go and do a culture? In the meantime, we need to do a CAT scan of your bladder.”
A few days later, I went in for a CAT scan. It came back [showing] I had a mass in my bladder.
Finding that I had a mass in my bladder was devastating news. I was really, really thrown back by it. I was like, ‘Could it be a mistake?’
When you found out there was a mass, what was your reaction?
Being a nurse practitioner, I knew what that meant. If one of my patients [had] blood in their urine, I would have done the same exact test that my primary doctor did. It could be a urinary tract infection. It could be kidney stones. Worst-case scenario is bladder cancer.
The way I approach my patients is: Tell me why it’s not bladder cancer, like the worst thing. When somebody has a headache, why isn’t it a brain tumor? I was like, “Why is this not bladder cancer?” I would have done the same thing.
Finding that I had a mass in my bladder was devastating news. How did I get this? No one in my family, on either side, has a history of cancer. How could this be? I don’t even know one black person that has this type of cancer. I was really, really thrown back by it. I was like, “Could it be a mistake? It could be a cyst. It could be this.”
The next step was to see a urologist.
The doctor that I currently work with had a good friend that was the head urologist in [the] healthcare system we both work for. This is in January 2021 so we’re in the midst of COVID — a lot of delays trying to get surgeries and procedures done. She called him up and said, “My nurse practitioner [has] this going on. Could you please see her?” Fortunately, I was able to get an appointment the following week.
I felt so defeated and deflated. I just could not believe that this was happening to me.
Diagnosis
How was it hearing the words come out of his mouth?
I was already prepping myself mentally, but it was still devastating. I was a nervous wreck. I remember having to take off work because my blood pressure [was] through the roof. I felt so defeated and deflated. I just could not believe that this was happening to me. It took me a week or two to get myself together mentally for what was next.
Next, they needed to biopsy, resect it, and see what stage of cancer it was. I started doing a lot of reading. My biggest concern was: Is this muscle invasive? Because if it is, that means that I’m going to have to have my bladder removed, chemo, and all this stuff is going to happen really fast.
My first husband passed away [from] lymphoma. My older two kids are still in [a] deep stage of grief. For them to find out that their mom has cancer was really tough.
Being the glue of the family
My first husband passed away [from] lymphoma. At that time, it was about five years prior. My older two kids are still in [a] deep stage of grief after losing their father at 47 years old. He went downhill in a matter of three years. For them to find out that their mom has cancer was really tough.
My youngest son was away at school. He’s a dancer. He’s at the University of North Carolina School of the Arts High School. We didn’t want to tell him until he came home for summer break. There was no reason to let him know right away other than to get him all upset and worried.
It was rough, thinking about your own morbidity and your potential mortality, especially when you’re thinking about cancer.
I’m a very, very spiritual person. I’m a Christian and I very much lean on my faith, which is another thing that helped me get through this. But, at the same time, my grandmother used to always say, ‘The Lord helps those who help themselves.’

Seeking help from a therapist
I knew right away that this was going to be very stressful, not just for me but for my family. In order for me to get through this, I was going to need help.
I contacted [a friend from church] and asked if she would take me on as a client and she agreed. Right away, I started meeting with her once a week. Our meetings continued through my first treatment, from February through May. I would meet with her on a regular basis, which was so helpful for me.
A lot of times people think that you have to take on everything yourself. Especially [in] my culture, mental health is very taboo. People take it as a weakness when you need to seek out help mentally. You always hear people say, “Be strong. Suck it up. You can do this. Don’t be weak-minded.” We are human beings. We are not robots and machines. We have feelings. We have difficulty.
Or they’ll say, “Pray about it. Give it to God.” I’m a very, very spiritual person. I’m a Christian and I very much lean on my faith, which is another thing that helped me get through this. But, at the same time, my grandmother used to always say, “The Lord helps those who help themselves.” It’s important for us to help ourselves. Part of that was interacting with a therapist that could help me — someone that I could trust and someone outside of my house, my family, and my life.
It was enough for me to talk to my husband but there were some things that I was going through that I didn’t necessarily want to tell him and burden him with. He had his own burdens of worrying about my mortality or my morbidity. I wanted to be able to freely talk without having to worry about someone else’s feelings about what I was going through and it was very helpful.
I never have been one to put all my trust in another human being so I felt like I needed to do my own research and have my own questions ready so that I know that I’m getting the best care possible.
Figuring out the next steps
The first thing I did was look for a reputable bladder cancer organization. You can find anything on the Internet — some of it is true, some of it is false. You can find people that will sell you snake oil and a bucket of sand. At the same time, you can find medically-sound information.
Because I am a scholar and also a clinician, the first thing I did was pull research articles and guidelines of practice because I wanted to know what to expect. I wanted to know if whoever I was going to see [was] following the correct guidelines to take care of me or not. I never have been one to put all my trust in another human being so I felt like I needed to do my own research and have my own questions ready so that I know that I’m getting the best care possible.
The experience I had with urologists made it even clearer to me that my approach is the best approach for me. Despite the fact that I was a clinician — I actually worked in the same healthcare organization that he worked in — he did not treat me well as a patient. And thankfully, because I’m a clinician, I was able to identify that right away. But when you’re talking about lay people going to seek care, go with your gut.
If you feel like something is not quite right, get a second opinion. You’re entitled to a second opinion. Some insurance will even pay for a third opinion. Do not feel like you’re stuck with that person.

Go with your gut. If you feel like something is not quite right, get a second opinion.
Appointment with the urologist
The urologist talked to us about the procedure. He scoped my bladder and said matter of factly, “Oh, it’s bladder cancer. It’s definitely bladder cancer. But I think it’s really superficial. It’s probably not a big deal. With COVID, it’s hard to get an OR so we can schedule this out.” I said, “No. If you can’t do it, I can find a surgeon that can do it. I have very good insurance. I have a PPO. I can go anywhere I need to go. I have something growing inside of me that doesn’t belong here and I want it out.” So he was like, “Okay, I’ll go ahead and do it.”

He had someone come up to give me a COVID test because you had to have a COVID test before you could schedule your surgery. He said I can have my surgery in a week. The lady came up and did my COVID test. I didn’t notice at the time but when I think back, I didn’t see her label my specimen. Long story short, the COVID test came back positive.
How do I have COVID? I’ve been home for four weeks because I had that surgical procedure. My husband’s working from home and we’re the only ones here. We’re very, very careful and cautious. For a whole year, I’ve been working in the field, in the clinic, with patients, some with COVID, but I hadn’t had COVID. I was like, “Something’s wrong with this.”
I called my clinic and had them do another COVID test. That test came back negative. I called them and said, “I had a false positive test. This new test is negative. I do not have COVID.” They said, “Oh, well, he’s going on vacation.”
He was gone on vacation. I kept calling and advocating for myself to get on the schedule so I was able to get on the schedule for the following week. Three weeks after diagnosis, I was able to have my surgery for the resection.
During the time that I was waiting to have my surgery, I had questions for this doctor so I [sent an] inter-office message.
I checked into the hospital [on] the day of my surgery. During that time, you couldn’t have visitors so my husband couldn’t go with me to pre-op. I had to go by myself, which was very nerve-wracking. I was nervous. I didn’t know what’s going to happen.
If you’ve ever been into pre-op, there’s just beds and curtains between them so you’re not in a room by yourself. You’re in this big room. I go in pre-op. They prep me. They start your IV, get your history, [have] you sign your consent, and all those things.
He comes in before surgery and says, “Okay, we’re ready to do your surgery. I can tell you’re a very highly anxious person.” I’m thinking, Should I say what I really want to say? Or should I just not say what I really want to say? This man is getting ready to operate on me. I’m going to be asleep. He’s going to have instruments inside of me so I’m not going to say anything to put myself at any risk. So I said, “Yes, I am.” Whatever it takes for you to feel good about yourself to do what you need to do, that was my thought process. And he goes, “Well, you inter-officed me, but please don’t do that again. Do not inter-office me. If you’re going to email me, email me through the patient portal.”
I’m listening to him and thinking, We are in pre-op. You’re getting ready to resect my tumor to find out if I have cancer, if it’s superficial like you think it is. You don’t know everything. How can you tell me that this is not invasive cancer by looking at it with your eyeballs? I was like, “No, I’m not trusting that you saying superficial is enough and I want it out now.” I’m sitting here thinking, Okay, now you’re going to chastise me in the pre-op area for something that we could talk about at another time. That email [was] sent probably a week or two before so this is not urgent. You’re on vacation the whole week before so there was no reason for us to talk about that right now.
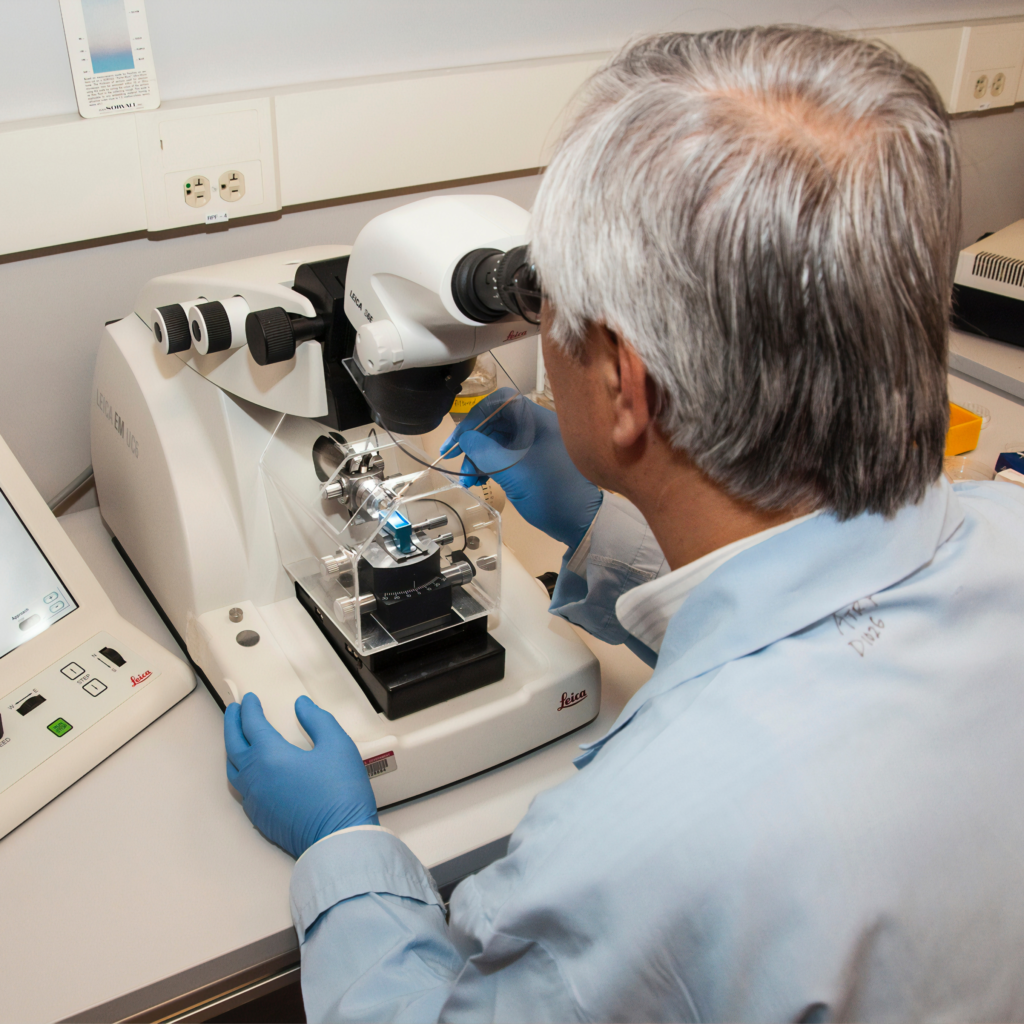
We had the surgery. Everything went well. Then he says, “It’s going to pathology and then we’ll find out what the situation is.” I said, “Okay.”

Feeling like your doctor is talking down to you
He did not see me as a colleague the way he was chastising me, in front of my colleagues, fellow nurses, and other patients. It could have been one of my patients in there with me. We’re all in the same healthcare system. He had no consideration of that. The little respect that I had left for him, I actually lost right in there.
The first thing I thought: I will never, ever in a million years refer any patients to this person. Congratulations. You will be a star in my book and the chapter is probably going to be, “Do Better,” because it was uncalled for.
If you have to drive an hour and a half or two hours to get the care that you deserve, you need to do that. How far would you drive for life?

Treatment
Getting the care you want
When I got home, I talked with my husband. We decided that once I got a definitive diagnosis, I was going to transfer my care to City of Hope. I wanted to do that because my great aunt [who] had melanoma went to City of Hope and they gave her excellent care. I was like, “We have the insurance so we can do it so let’s just do it.”
From where we live, City of Hope is about an hour and a half [away]. My husband just said, “It doesn’t matter how far it is. I’m going to take you wherever you need to go.” And for me, that’s something I can’t express more powerfully.
If you have to drive an hour and a half or two hours to get the care that you deserve, you need to do that. I tried to get my ex-husband to transfer his care to City of Hope. I tried for almost a year. Finally, when he decided that he was ready, he could not transfer. He was too ill.
City of Hope [doesn’t] have an ER. It’s a cancer hospital but you have to enter as an outpatient. By the time he decided that he wanted to go, he was an inpatient at UCLA. He could not leave the hospital. He was so ill. He was there for a month. He came home for one night and was back at the hospital the next day. Never could get him strong enough so that he could be seen there.
I kept telling him they’re doing a special trial for his type of cancer. He really needs to try to get there. But he never did. I think the first thing that he said was, “It’s so far.” It’s only an hour and a half away. How far would you drive for life? And life more abundantly. How far actually would you go?
Getting the results from pathology
We went back to the doctor and the doctor says, “I’m so sorry. I thought that this was superficial but you have high-grade bladder cancer. Even though we removed the tumor, these types of cancers have a very, very high likelihood of returning.”
The good news was that it hasn’t gotten to the muscle, but it is in the lamina propria, which is the lining inside of the bladder and the bladder wall. He said that they took an extra sample just to make sure that they were not missing anything. It was deeper than they thought it was, but it looks like there was no muscle in the tissue.
When he told us, my husband and I began to celebrate. We were happy. We were thanking God because we knew that if it was in the muscle, that [meant] chemotherapy, bladder removal — all that was going to happen, that was the next step. But if it was not in the muscle, I can at least try another treatment, which would have been BCG immunotherapy installations into my bladder over a series of time and then maintenance for three years. And if no recurrence of tumor, then I may be cured at that point.
We started celebrating and he said, “No! No! No! This isn’t anything to get excited about. This is serious. It’s high-grade cancer.” I was telling him, “Excuse me. This is something to celebrate because today, I get to keep my bladder. I’m not worried about what’s going to happen in a year, two years, or three years down the line. But this day, I get to keep my bladder and that is a blessing.”
Then he was like, “I really want you to go and have a second opinion with my colleague at USC.” I was thinking, Excuse me. The way you have treated me, there’s no way that I will ever go to anybody associated with you because they will likely be just like you and I’m not doing it. I tell him, “No, thank you. We’re going to City of Hope.” And he said, “Why do you want to go to City of Hope? It’s so far. Is there a particular reason?” I said, “Because that’s where we want to go.”
My husband interjected and said, “I will take her wherever she needs to go. If we have to get on an airplane, we will be doing that.” And I was thinking, Yes, we are those black people, not the ones that you think we are. I’m sitting here going, How dare he? The audacity to try to discourage me from going to a cancer treatment center, [an] internationally-recognized cancer treatment center, because of the distance.
I’m not worried about what’s going to happen in a year, two years, or three years down the line. But this day, I get to keep my bladder and that is a blessing.
He was saying, “We could do the BCG, which is the immunotherapy here, but there is a BCG shortage.” And this is true. There’s a national shortage of BCG because only one company makes it and I knew that. I also knew if you’re in a cancer treatment center, because of the other drugs that the hospital uses, they’re more likely going to make sure that they give them what they need first.
I felt like I was going to get a better chance of getting my BCG and getting it on time if I went there as well. We don’t think about these things as lay people, but this is something that I was able to think about and pre-plan. He probably wasn’t too thrilled [about] that. I just said, “Thank you very much. I appreciate all that you have done. Goodbye.”

Dealing with preconceived notions in healthcare
He had a picture in his mind of who I was and what my life was like. He already had his own stereotypical thoughts about who I was. Because if he didn’t, he wouldn’t have treated me that way. Not because I was his colleague, but because I was his patient. He wasn’t seeing me as a colleague, even though I was. He was seeing me as a black patient.
I don’t really know. Maybe he treats all his patients that way, but being a black woman and seeing the health disparities that we have in particular compared to other groups, I thought that he felt that he had the right to treat me the way that he did.
Why wouldn’t he say, “Well, you know, City of Hope’s an hour and a half away. Is that going to be a problem for you?” Why not say that? No, he just assumed that we couldn’t do what we needed to do or we wanted to do as far as my care went. My husband should have never had to interject and tell him, “If she needed to get on an airplane to go somewhere to get care, then I’m going to do that for her.” We shouldn’t have even had to have that conversation.
I had an aortic aneurysm. I had heart surgery at 39 years old. My doctor, my cardiologist, he is a man of color. He is Indian. When I first went to him, was diagnosed, and knew that I had to have open heart surgery, the first thing he said [was], “Now I can do this surgery right here. But because of your age, I want to send you to San Francisco. I don’t know if you know this basketball player.” He was telling me about a basketball player who had the same thing, an aneurysm. And he said, “He plays with a vest on. He had his surgery in San Francisco and they did a great job. And I think because of your age, I really want you to go there.”
He never assumed that I wouldn’t be able to go there. He never assumed that we couldn’t afford to go there. He didn’t have any assumptions. He said, “In my personal opinion, you would receive the best care here. And this is where I would like for you to go if you could.” And that’s the approach that the other doctor should have taken. It’s only an hour and a half away. How far would you drive for the best chances? The latest equipment [and] doctors that are doing research actively on your problem. Why wouldn’t you?
He said, “You will never come back here.” I said, “Touché. I’m not coming back here.” He did exactly what we needed him to do — make the initial diagnosis and that was it.
I was looking for a doctor that looked like me because I felt like I could trust a doctor that looked like me.
Transferring care to City of Hope
It was so easy. The first thing I did was pull up their different offices. Come to find out, they have clinics all over. They have offices all over California, not just in Duarte. The closest to us that has urology was in Santa Clarita. From our house, it probably takes us 45 to 50 minutes to get there. If anything needs to be done, like hospitalizations, then you go to the other place. But you can have your regular visits, including the treatment for cancer, right there in that office.
I looked at all the doctors. I was even willing to go to Duarte if I had to. I was looking for a doctor that looked like me because I felt like I could trust a doctor that looked like me. Fortunately, I found one.
When I’m taking care of patients, I look at them holistically. For example, in my clinic, probably 95% of my patients are Latinx. Most of them [are] farmworker families. Majority do not speak any English at all. I speak a little bit of Spanish, but I try to find out everything I can about the culture. I want to learn as much as I can learn about the culture because those are my patients. Those are the people that I’m seeing. When I’m taking care of them, I’m not just taking care of what’s right in front of me. I’m looking at them holistically as people, as a culture, [and] as a community. And that’s what I felt like I needed in my health care.
I need someone who knows the culture so I don’t have to explain every little thing to them and they know how to approach me as a person probably because they have some shared experiences with me. Unfortunately, the doctor I selected was not a urologist. Urogynecologist but not a uro-oncologist, which is what I needed for my problem so I had to pick someone else. And I did and it worked out really well for me.

Discussing treatment with the new team
Even if I were to stay where I was, there should have been a second resection. What helped me is their bladder cancer advocacy. There’s an organization (the Bladder Cancer Action Network) that gives patients tons of information. It’s like the American Cancer Society for bladder cancer. I was able to pull articles, look at the actual standards of care, [and] the procedure so I knew what was supposed to happen.
If it comes back negative for muscle invasion the second time, after your bladder recovers [in] about four to six weeks, they start you on immunotherapy, which is installation of the treatment into the bladder. I had to do that for six weeks.
The new doctor did the resection. I really liked her a lot. Liked her personality. She was very positive, which is what we were looking for. The resection turned out really well. Then we were going to start the BCG.
BCG immunotherapy for bladder cancer
My path was a little bit different. They did the first six weeks of BCG. During that time, I had one bladder infection that delayed treatment for a week because I had to take antibiotics then I had to go back and finish. At the end of it, they wait eight weeks and then they scope you.
It’s an infusion directly in your bladder. You have to hold it in your bladder for two hours then you can pee it out. When you start peeing it out, you have to put bleach in the toilet and be careful that nobody else uses the toilet.
The BCG was better than chemo, but it was hectic.
Side effects from BCG immunotherapy
The first day, I would be fine. Second day, I would have joint pain, flu-like symptoms, [and] fatigue. I might have pain with urination [and] bladder spasms. The more treatments I had, the more irritated and the more irritable it became.
The BCG was better than chemo, but it was hectic. With the burning with urination, it didn’t matter what they gave you, it just was not going to do it. It might take the edge off, but that was pretty much it. It’s like making your bladder raw on the inside, too, to make the environment not conducive for the tumor to grow.
Maintenance therapy for bladder cancer
The following month was my first maintenance dose of BCG, which was for three weeks — a lot better than the six weeks. Then eight weeks later, I would be scoped.
On the eighth-week scope, I had no new tumors that they could see, but they saw a bumpy area. She wanted to watch it. At that point, you would be having maintenance BCG immunotherapy every three months for whatever the prescribed time was going to be. It could be two years, three years, [or] five years. Maybe two years and then [on] year three, you do it every six months. It just depends on how well your progress is going.
My bladder is actively trying to kill me. It’s my bladder or me. What’s it going to be? I decided I’d rather it be my bladder to go.
Bladder removal surgery
New development leading to bladder removal surgery
When I had my second scope after the three-week BCG maintenance, that’s when my treatment took a different turn.
When they went in to scope my bladder again, I didn’t have any tumors but that bumpy area had gotten bigger. The doctor said, “I want to take it out.” And I said, “I want you to take it out.” I was so happy that she wanted to do the procedure.
She went in, resectioned it, pulled it, took it out, [and] sent it to pathology. When she was in there, she found another small tumor that wasn’t even detected on the scope so she took that out, too, and sent that to pathology.
That area that was flat and bumpy was the same cancer that I originally had. It just wasn’t growing in the bladder. It was growing down so it had not reached the muscle yet, thank God. It had gotten to that layer, but it hadn’t broken through to the muscle wall. Again, that makes the difference between chemotherapy [and] something else.
She also found another type of bladder cancer: carcinoma in situ. I had already done some research and I knew that most people who have that, it just comes back. It’ll be one now. Next time, it’ll be three. Next time, it’ll be five. All roads eventually lead to bladder removal for most people.
Every time, in all these treatments, you’re rolling the dice that it’s going to get to the muscle. My bladder is actively trying to kill me. It’s my bladder or me. What’s it going to be? I decided I’d rather it be my bladder to go.

I’m going to stay here. I’m determined to be here. If I go ahead and do the surgery, I have choices [regarding] the outcome. If you wait too long, it can get into the bladder wall [or] outside of the bladder wall. The wall of the bladder is very thin. It sits right on top of the uterus. Once it gets out, it goes [quickly].
You’re taking chances. And I’ve never been one to really take a lot of chances, especially with my life. I know my kids need me. I know my husband needs me. I have a lot of responsibility and I really want to be here.
At that point, I made the active decision to have my bladder removed. I talked to my doctor and when she gave me the final pathology, I said, “I really think that I want to have my bladder out.” And she goes, “You know, I was going to tell you, you could do inter-bladder chemotherapy because it’s not in the muscle. We can put the chemo in your bladder but [it] may not work. It probably won’t, long-term. If it were me, I would do the same thing.”
At that particular point, that was the reassurance that I needed. But I already made up my mind that I was going to do it.
I’ve never been one to really take a lot of chances, especially with my life. At that point, I made the active decision to have my bladder removed.

Urinary diversion options
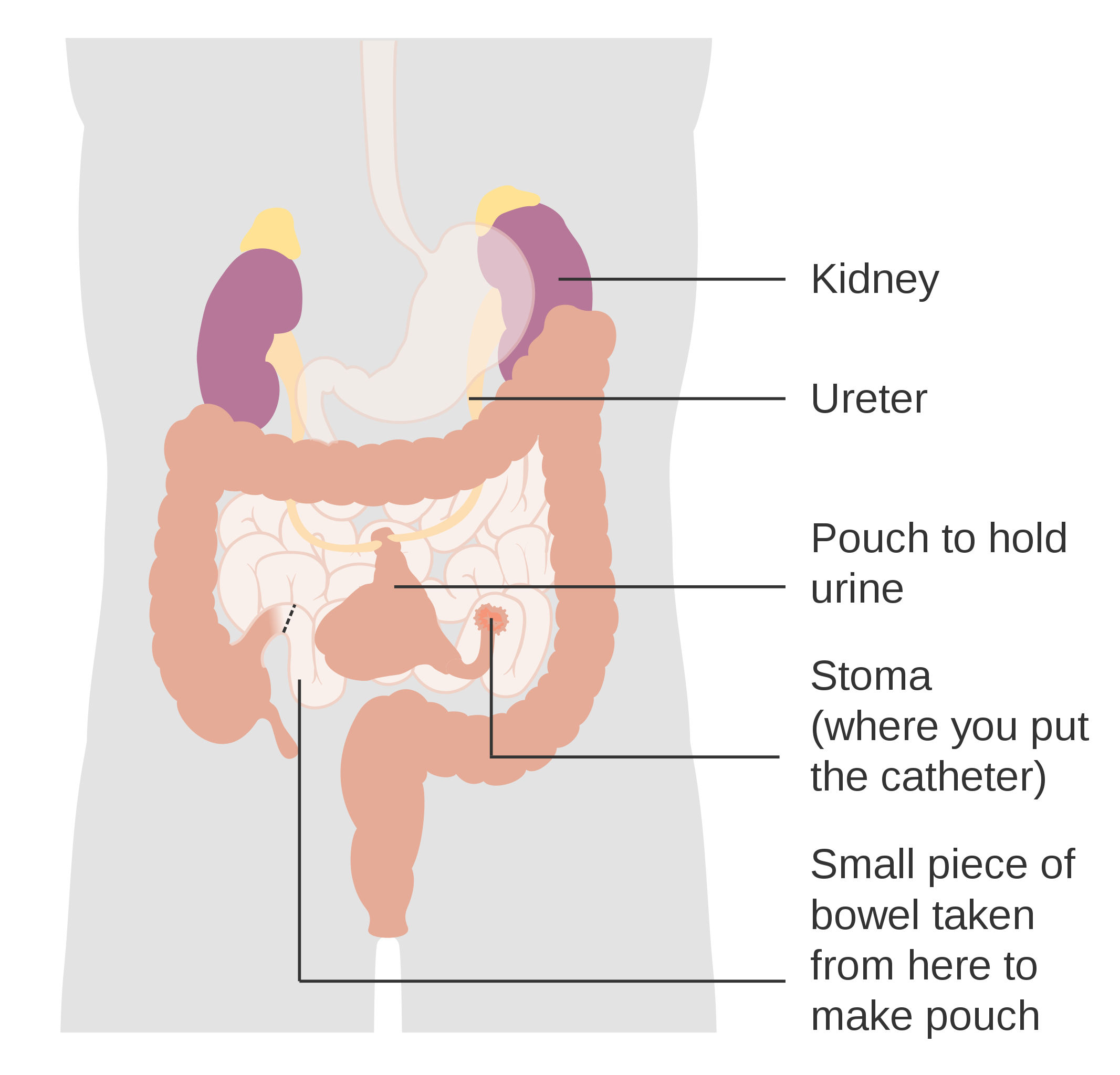
What type of diversion am I going to have? Did I want to have a bag? No, I’m 52 years old. Why would I want a bag if I don’t have to?
The next choice was a neobladder, [where] they make the bladder out of [the] colon, put it back to where the old bladder was, and you can urinate like usual. But there [are] some challenges with that. One is my urethra. I didn’t want to keep my urethra because that could have cancer later. Two was that usually, the neobladder works better with men because women tend to have more incontinence and bladder leaking or retention. If I have bladder retention, that means that I’m going to have to cath myself so I can pee. It doesn’t mean it’s going to happen every time, but it happens a lot. And then leaking. We already have enough bladder leaking after you have so many kids. I was thinking, After all this, I don’t want to have to deal with any of that. For me, that was not the best choice.
The next thing was Indiana Pouch. I knew that was an option for me. The problem is [in] a lot of places, the doctors don’t know how to do it.
When you’re advocating for yourself, think about where you’re going to get your care. Because if they don’t know how to do certain procedures, they’re not going to recommend those to you even if they’re the best things for you. That’s left out because when you ask, “Can you do the Indiana Pouch?” They’re like, “We don’t do those here.” You’ve been having all your care there. Then sometimes we say, “Okay, I’m not going to do that one.”
Another reason why I went to City of Hope [was] because I knew that they did everything there and they may be doing some things that I don’t even know about. And if it sounds right, I’m going to be down.
Think about where you’re going to get your care. Because if they don’t know how to do certain procedures, they’re not going to recommend those to you.
I decided to do the Indiana Pouch. Great things about it. I can pee standing up. I have a problem with public bathrooms. And for now, there is no problem with a public restroom. I can go to the porta-potty. I don’t have to touch anything. Unless I have to have a bowel movement, I don’t have to sit down in a public restroom.
There is a risk of infection because you are putting the catheter in, the little stoma. People have different types of stoma. The one that I have is really low, below my bikini line, so I can wear a bikini and you can never even tell. Some people have [it] above the bikini line so that would show but they just put a waterproof dressing on it. Some people have it in their belly button, so they actually cath their belly button. For me, that wasn’t an option because I had another surgery [so] it wasn’t going to be a good choice for me. I didn’t think I wanted that anyway because some people end up with hernia and I don’t want to deal with that either.
I decided I would do the Indiana Pouch, so I just have a little catheter. It can fit in the palm of my hand. [When] I go to the bathroom, I just open it up. It’s all sterile. I can touch it on the outside and feed it in. I stand there, pee, take it out, throw it in the trash, and I’m on my way. It takes less than 10 minutes.
Had I waited, the cancer may have been to a point where that wouldn’t have been an option. It could have gotten bladder-invasive in the wall. These things grow fast. You need to have it out within 90 days.
When I made the decision to have my bladder out, I knew that I had 90 days to have my surgery because that might be a regrowth period and I didn’t want anything to grow back before I had my procedure. My husband and I had a trip to the Dominican Republic. I said, “As long as I can go on my trip, I’ll be ready to have my bladder out when I come back.” And that’s what I did. Five days later, I had my bladder removed.
When you’re having surgery, you never know what’s going to happen. What if something just didn’t go right? I told my husband, “We’re going to go on this trip. We’re going to enjoy and have the time of our lives because what if we don’t get a chance to do this anymore? I want to make sure that we have a good time.” And we did.
Fortunately, everything turned out well. I had a few little setbacks during my recovery period, but I would not change anything. I’m just so glad that I made this decision, other than having to go to the bathroom on a schedule. Every 4 to 6 hours, I have to empty my bladder.

Choosing the best urinary diversion option for yourself
I thought about this. I didn’t want the bag so that was not going to be an option for me. I knew that if my other diversion failed, I could always go to the bag. You could always go to the bag later but you can’t go back once you decide you want the bag.
The other thing was if I have retention or bladder leaking, what [a] hassle that’s going to be. This is for the rest of my life. Who’s going to cath me when I can’t see down there? My husband? He won’t be able to see either. Who’s going to do it? But if I have the Indiana Pouch, if someone’s taking care of me, it’s really easy for them to take care of me. Someone else could do it [really] easily. It’s not difficult. They don’t have to go down there and try to find where to cath me.
I thought about a variety of things. I thought about the right now. I thought about the future. I thought about the things that I like to do. My husband and I love to go to concerts, outdoor venues, [and] festivals. Usually, there [are] porta potties involved. Is that going to be conducive to my lifestyle? What about when we travel? We like to travel. We like to go overseas. Is that going to be a problem? All of these things are manageable with my diversion.
It’s not just about living. It’s living your life abundantly and having the best life that you can possibly have.
Impact on intimacy and relationship
This is another reason why support groups are really important.
When they do a surgery of this nature, it’s major. They not only remove your bladder, but they remove your ovaries [and] part of your vagina because your bladder sits right on top of your vagina so there’s part of it that has to be removed. In some cases, they remove most of the vagina, especially if they think there’s a possibility that cancer has gotten through that. They [also] take out your appendix and lots of lymph nodes.
When you’re thinking about being married, young, and not having a vagina, that could be traumatic to your relationship. I never would have thought to ask but somebody in my support group brought it up. I talked to her and she became one of my close friends, too. When she had her bladder removal surgery, they removed all of her vagina except for maybe two inches, which [meant] that she would have to come back later and have a reconstruction of her vagina. I was like, “Oh no, that is what I’m not doing. I don’t have [a] muscle-invasive disease so it’s not out of my bladder. I do not want to have no vagina.”
I talked to my doctor ahead of time and said, “If I wake up and I don’t have a vagina, all hell’s going to break loose so we need to make sure that I wake up with a vagina.” She said, “We’ll do vagina sparing.” I said, “Yes. I want to make sure I have a working vagina.”

It was very nice that I was able to consult with the plastic surgeon. Another reason to go to these big cancer centers is [that] all these doctors are there. The plastic surgeon was there and he went through the procedure. I said, “If they get in there and there’s a problem, I expect to wake up and still have a vagina.” He said, “If they get in there and they have to remove everything, then I’ll either take part of your muscle from your thigh or from your abdomen and I will make you a vagina. You’re not going to wake up and not have a vagina no matter what.” I said, “You promise I’m not going to wake up with no vagina?” He said, “No. I will fix it.”
It seems like something small when you have cancer, but it’s not. It’s still quality of life. It’s living your life and living your life abundantly. I want it all. If I have to go through all this, I want to make sure that I’m going to have what I need to be happy and all those things.
One of the things I was able to tell Ebony because she was coming behind me was, “Make sure you talk to them about vaginal sparing [so] you don’t wake up like another friend [who] only [has] a two-inch vagina and nobody told you anything.”
There [have] been a lot of people on the site whose partners left them. They have cancer and their partners leave. Because mentally, they can’t handle it or this situation. They can’t wrap their head around the fact that their sex life is going to be very different.
This is important. This is quality of life. It’s not just about living. It’s living your life abundantly and having the best life that you can possibly have.
Having my own community of support outside of my own friends and family also took the pressure off of them.

Support
Connecting with people through cancer support groups
Around the time that I transferred to City of Hope, I joined a bladder cancer support group on Facebook. I found a couple of groups: one was women and bladder cancer [and] the other one was just bladder cancer itself. Connecting with people — that were going through the same things that I had gone through, that had gone through what I had gone through, so I could ask questions that could offer me support — was invaluable while I was going through my process. I’ve met some lifelong friends since I joined a group.
The first person I met was a woman in New Jersey. She was diagnosed with the same cancer that I have. However, hers was caught at an earlier stage so she did maybe one round of BCG, but she hasn’t had to do anything else. They’re just scoping her.
My son is a dancer and we went to New York for him to do an intensive. I also have another son and son-in-law who live there. We went to visit them and I was able to have lunch with my bladder cancer wife. I got to meet her for the first time. We had lunch together. You think we’ve known each other for years. It’s the best thing ever. I think we both cried. We got diagnosed weeks apart and we have been going through this journey together, supporting each other.
We exchanged numbers after meeting on Facebook and we just started texting each other back and forth. We became really fast friends and we’ve been friends ever since. Sometimes I find myself calling her before I call my husband. That’s why I said she’s my cancer wife. Before the scan, she’d call me. I call her before her scans. We comfort each other. It’s so funny. This black lady and this little Jewish lady and we’re just a year apart in age. We have just bonded and she is truly my sister.
Then, also Ebony. When Ebony came on to the bladder cancer support group, she posted something and there was something in the background of her picture that let me know that she was in the same sorority that I was in. I got so excited, especially because there [were] not very many black people at all in the support group. There’s just not a high percentage of black people that have bladder cancer.
I [sent her a message] and said, “You know, I think you’re in my sorority.” We started talking and then we exchanged numbers. We started texting each other and supporting each other across the country. She was at the beginning of her journey so it was really nice that I was able to talk to her, encourage her, and let her know what the surgery was like when I was going through the process. When I got to meet my friend, that really just solidified our relationship more.
You never know why people come into your life.
Importance of finding & connecting with someone in your cancer community
It’s very important. It keeps you going. It empowers you.
I call my nursing students baby birds and they call me mama bird. Some students have graduated [and] have gone on to have their own careers. One of which I became very close to and she ended up having breast cancer. I was really supportive of her during her breast cancer journey, which was before I had bladder cancer.
You never know why people come into your life. I really believe that our relationship was orchestrated by God so when I got ready to go through my experience, I was going through it with someone who had already been through cancer before.
When she was going through her cancer, we used to talk about [how] I was going to help her write a book. The book was going to be, “You’re Not Helping,” and the things that people say to people that have cancer. “You’re going to beat this,” little things like that. It’s like, “You’re not helping.” There [are] a lot of things that people say and they think that they’re helping, but they’re not helping.
There are things that you can say that would be helpful. That’s why when people pass away, a lot of people say, “I’m sorry for your loss.” And that’s not helpful. What can you say? “I’m praying that God will support you and will send you peace and understanding.” “Is there anything I can do?” There [are] the superficial things that people just naturally say and then there [are] things that people say that have meaning that really go there.

Some people don’t know what to say. I have a lot of friends [who] I didn’t even hear from when they first found out. I understand that it’s hard for you to wrap your head around my experience and what I’m going through but, at the same time, this is the time that I need you the most. Don’t disappear on me.
Having my own community of support outside of my own friends and family also took the pressure off of them. The things that I felt that they should have been doing to support me, I really didn’t need that because I had my community already that was there to support me and they were there to talk. They didn’t care about me talking about cancer for an hour.

The power of connecting with someone within your own circle
I felt a real sisterhood. I felt a special bond with her (Ebony, pictured left) outside of cancer, which was nice. In my sorority, we have a very small chapter where I live. Off the top of my head, we have lost maybe six sorority sisters over the last 15 years to cancer of various kinds: cervical, breast, liver, [and] pancreatic. It’s just so strange that so many people from one small sorority have all these cancers that take place. It’s really been rough.
One of my sorority sisters was diagnosed with stage 4 cervical cancer and she passed away. I started treatment in January, she passed away in September. [She] and I had been really, really close. I had taken her to the hospital before her initial diagnosis. To be going through that and have someone you love [and] close to pass away from that experience, it’s a lot. That’s why the mental health side is even more important.
Through this journey, I’ve lost a lot of people to cancer. In 18 months, four people close to me have died of cancer. One of breast cancer, one [of] cervical cancer — both my sorority sisters from the same chapter — and two first cousins that died seven months apart. One we buried last month, stage 4 colon cancer. He’s a year younger than me and then his brother died six months before that. Pancreatic cancer, weeks from diagnosis to death. These are my first cousins. We took baths together as babies. That was painful.
My cousin that passed away [from colon cancer], he and I are very close. We were only 13 months apart and we got diagnosed a week apart. We’ve been walking together through this, too. We’re both encouraging each other on a regular basis, talking to each other every week.
You can’t put 100% of your life into your healthcare provider’s hands all the time. Don’t have expectations that somebody else cares about you more than you do.
Words of advice
Listen to your body. If you feel like something’s not right, it’s not right. It doesn’t matter if they say, “Oh, everything’s okay.” You have to remember these things. If you die, they’re going to get another patient. The only people that are going to be affected by my death are the people who love me. And I love myself. If I feel like something is not right, I’m going to get a second opinion. Why? Because I’m entitled to one. And that’s what I’m going to get.
I’m entitled to do research and I’m going to do whatever research I need. Again, going back to, “The Lord helps those who help themselves.” Sometimes we ought to go out and help ourselves. As a provider, I care about all of my patients. I do the best I can do for them. But I am a human being as well and I don’t know everything. You can’t put 100% of your life into your healthcare provider’s hands all the time.
Every situation is different. If something doesn’t feel right to you, something’s probably not right. You’re obligated to find out so that you do feel right about whatever it is. Don’t always listen to what everybody else does. You have to do what’s right for you. Get all the information that you possibly can and then decide what’s best for you. You’re the one that’s going to have to live with your decision.
I couldn’t let anybody else make this decision for me as to what type of diversion I was going to have because it was my life and I’m the one that’s going to have to deal with it. No one else. No one else cares how I pee. They may have an opinion about it, but they’re not the ones cathing. They’re not the ones getting up in the middle of the night. They’re not the ones that have to see if they have an infection or not. They’re not. It’s me. I’m the one.
Put yourself first, whatever it is that you feel. If you feel that something’s wrong, then usually it is wrong. Don’t have expectations that somebody else cares about you more than you do.

Follow-up regimen
Now that the bladder is gone, I don’t have to worry about bladder cancer but I’m going to be monitored for the next five years. Every three to six months, they’ll scope my pouch.
After five years, I’ll be monitored every year for the rest of my life. Scoped and probably CAT scan to make sure that there’s no recurrence there or anywhere else. And that’s a blessing to me.
Do what’s right for you. Get all the information that you possibly can and then decide what’s best for you. You’re the one that’s going to have to live with your decision.

Inspired by LaSonya's story?
Share your story, too!
Bladder Cancer Stories
Laurent Gemenick, Bladder Cancer
Symptom: Presence of blood in urine
Treatment: Surgery: transurethral resection of bladder tumor or TURBT
Jon T., Locally Advanced Muscle-Invasive Bladder Cancer
Symptom: Darkening urine, blood in urine, dull right flank pain
Treatments: Surgery(transurethral resection of bladder tumor or TURBT), antibody-drug conjugate, chemotherapy
Michael V., Bladder Cancer (Non-Invasive High-Grade Papillary Urothelial Carcinoma), Stage 1
Symptoms: Frequent urination, burning sensation when urinating
Treatments: Surgery (transurethral resection of bladder tumor or TURBT), immunotherapy (Bacillus Calmette-Guérin or BCG treatment)
Dorinda G., Bladder Cancer
Symptom: A significant amount of blood in the urine
Treatments: Surgery (transurethral resection of bladder tumor/TURBT, surgery for papillary lesion), immunotherapy (BCG), chemotherapy
Healing Together: A Mother and Daughter Navigate High-Grade Bladder Cancer
Mary Beth’s story about caregiving starts with an important awareness message about female bladder cancer symptoms.
Danny G., Non-Muscle Invasive Bladder Cancer
Symptoms: Fatigue, back pain, erectile dysfunction, nausea
Treatments: Surgery (transurethral resection of bladder tumor or TURBT), chemotherapy, immunotherapy