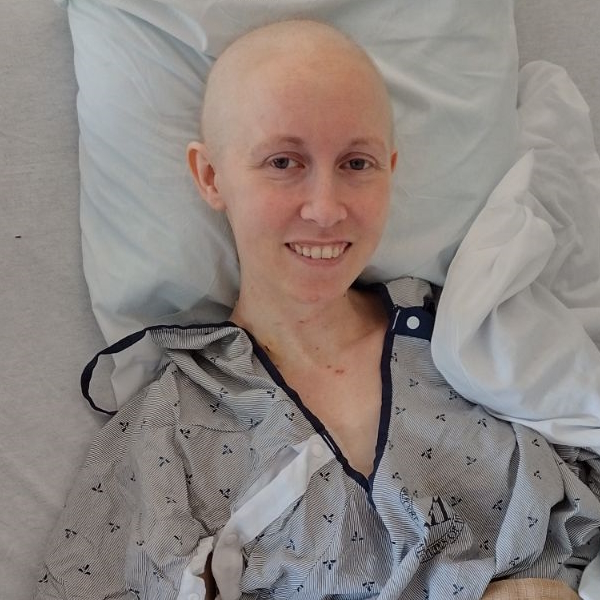
Ashley’s Stage 4 Rare Adrenal Cancer Story
Interviewed by: Taylor Scheib
Edited by: Katrina Villareal

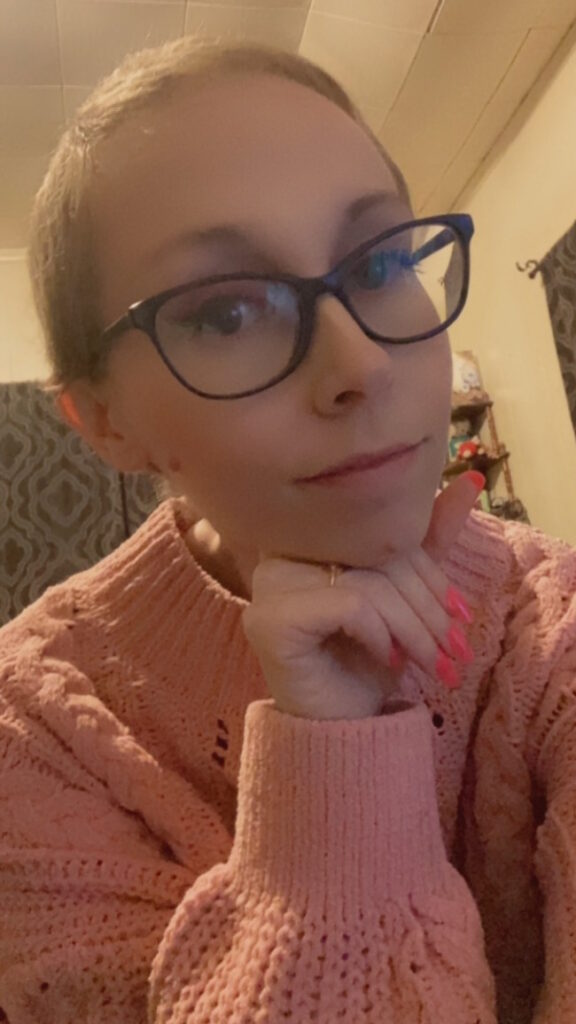
Ashley’s symptoms began with mild back pain in October 2022, which escalated to severe discomfort by January 2023. After a series of tests, a CT scan revealed an 11 cm tumor on her adrenal gland and she was eventually diagnosed with stage 4 adrenocortical carcinoma (ACC), a rare cancer affecting about 300 to 400 people annually in the U.S. Despite facing numerous challenges, including a delayed diagnosis due to lack of insurance, she educated herself on her condition, sought out specialists, and joined support groups.
Her treatment journey began with EDP (etoposide, doxorubicin, and cisplatin) chemotherapy and mitotane, which caused severe side effects, including hypothyroidism. Despite the challenges, the tumor showed signs of shrinkage and she underwent surgery to remove it. When chemotherapy became ineffective, she switched to targeted therapy with lenvatinib, which showed promising results.
Throughout her journey, Ashley also struggled with mental health issues and adjusting to the need for help, but she found support through therapy and counseling. Ashley emphasizes the importance of self-advocacy in medical treatment, seeking second opinions, and the value of support groups in navigating her rare diagnosis.
- Name: Ashley P.
- Diagnosis:
- Adrenocortical carcinoma (adrenal cancer)
- Staging:
- 4
- Symptom:
- Mild back pain on her left side that escalated in severity
- Treatment:
- Chemotherapy: EDP (etoposide, doxorubicin, and cisplatin) & mitotane
- Surgery
- TKI inhibitor: lenvatinib
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
I was having some mild back pain on the left side, which was eventually where the tumor was discovered.
Introduction
I live in Beaumont, Texas, about an hour and a half away from MD Anderson.
In October 2022, I first started showing symptoms of my cancer, but I wasn’t diagnosed until March 2023 and I’ve been living with stage 4 cancer since then. It’s extremely rare. It affects 300 to 400 people in the US every year, which is about one in a million people.
Pre-diagnosis
Initial Symptoms
When I first started having symptoms, they were very mild and pain-related. I was having some mild back pain on the left side, which was eventually where the tumor was discovered. I would rate the pain at a 3 out of 10. It would always happen after long car rides, so I chalked it up to bad posture.
The pain was on and off throughout the next several months until about January. Then I had severe back pain that manifested at a friend’s house. I was sitting on the floor and it overtook my whole body. It was probably a 7 or 8 out of 10. Within a couple of days, it eventually settled down and then went away. I still thought it was my posture.


Come February, I started to feel a pinching pain around my rib cage. I had never had that. It was persistent throughout the day in a specific spot and that’s what got me worried. I couldn’t figure out what it could be, so it scared me a little bit. Some family members told me it could be this or that, it might be something serious, and that I should get it checked out.
I went to our local hospital where they ran a bunch of tests, including blood work and X-ray. I came in with high blood pressure of around 190/105, if I remember correctly. I wasn’t aware that I had high blood pressure, but I think it has been ongoing and I hadn’t been checking it. I was also anxious, so I’m sure that was playing a part.
CT Scan Revealed Tumor
They saw something in my X-ray, which they said could be an infection in one of my lungs but I had no respiratory symptoms. They gave me a COVID test and it came back negative. Everything they checked came back negative, so they sent me in for a CT scan because they couldn’t figure out what was going on. It was a good thing they did that because that’s when they discovered the tumor coming off of my adrenal gland, which I believe was around 11 cm at the time.
She gave me the news of this enormous tumor coming off of my adrenal gland and the very last thing she said was, ‘It has metastasized to your lung.’
Getting the Scan Results
The doctor comes in with a look on her face and I knew she was about to give me bad news. My stomach dropped when I saw the way she looked at me. The whole mood in the room changed. My fiance came with me to the hospital, but because it had gotten so late and the chairs were so uncomfortable, he was sleeping in the car in the parking lot when she told me.
She gave me the news of this enormous tumor coming off of my adrenal gland and the very last thing she said was, “It has metastasized to your lung.” I could tell she didn’t want to say that part because that meant stage 4. At that point, I didn’t quite understand anything about what she was saying. She said it was 95% sure I had cancer because they can’t tell you 100% until they biopsy.
She ended with, “We don’t think we can handle this here, so we’re going to have to transfer you to an ICU.” They treated my blood pressure because that was all they could do for me.
I called my fiance, told him where he needed to go, and gave him all the information I could. We didn’t know much, so I was relaying what little information I had. He was sitting there crying and I was comforting him more than I was comforting myself. I was completely disassociated. I went into shock a little bit. It was a surreal experience.


Transferring to Another Hospital
I had to be transported to another hospital’s ICU about an hour and a half away, but I had to wait until the next morning for an ambulance to transfer me.
The oncologist came in and said, “I don’t think it’s ethical to treat you without insurance.” They sent in a social worker who handed me his phone to talk to an insurance agent. They sent me home after three days. I had to wait a full month for the insurance to kick in.
When I went home, I hadn’t had a biopsy yet, so I didn’t even know my diagnosis. I couldn’t look anything up because I didn’t know what it was. All I knew was there was a tumor and something in my lungs.
I had something serious going on and all I was doing was waiting. I had no idea how fast things needed to be moving.
Waiting for Insurance
I didn’t have any coping skills because medical issues weren’t something I had ever dealt with, so it all hit me like a train. I went into a state of almost paralysis. All of a sudden, it was almost as if I could feel the tumor and it made me afraid to move and get out of my bed. I thought, Am I going to make it worse? Is it going to rupture? These types of tumors are very, very fragile. They’re like an egg. At the time, I didn’t know, but that was still a thought because I knew how big it was.
I was at my heaviest, but I started losing weight because I wasn’t eating well. I was so paralyzed by fear, worry, and not knowing anything. While at the hospital, I even asked the nurse if I was going to die soon and she changed her demeanor a little bit. She said, “Oh no, no, but this is very, very serious,” and that stuck with me.
I had something serious going on and all I was doing was waiting. I had no idea how fast things needed to be moving. Each day, I would try to get through the day and after another day’s done, move on to the next day. I was looking at my calendar every day, compulsively checking the days off until I could get my insurance.


Diagnosis
Getting the Biopsy Results
Once I got the biopsy results and knew what I had for sure, I started digging. I put all of my anxious energy into finding out more about my type of cancer. I joined adrenal cancer Facebook support groups and started talking to people and watching YouTube videos. There are a few conferences that have a few of the experts that exist in the United States. There’s only a handful of them and they put together this conference with all of this educational information.
One time, I stayed up all night because I was so anxious and freaked out because I didn’t know what my future was going to look like. I wanted to know what my options were. I couldn’t get my mind to separate from what I was going through, so that was a difficult time for me. That beginning stage was probably one of the most difficult experiences I’ve dealt with so far, even after everything I’ve been through.
What helped was educating myself and talking to people with the same diagnosis. There aren’t a lot of us because it’s so rare, but there are support groups. I don’t know anyone in my city who has my diagnosis. I’ve been to urgent care centers and some of them have never even heard of what I have.
At a certain point, I couldn’t work anymore. The symptoms had worsened to where I would get very high blood pressure and resting heart rate, so I didn’t feel like it was safe for me to work.
Finding a Specialist
When I joined support groups on Facebook, they were recommending certain doctors who were doing research on my type of cancer, but they’re located in Maryland at the National Institutes of Health. A girl in the support group called me and gave me all this information. She even put me on a three-way call with someone from the NIH about getting set up. Eventually, someone gave me the direct phone number and email address of the specialist, Dr. Jaydira Del Rivero.
I wanted to get recommendations and second opinions, and see what a true expert would say. The support group led me in that direction and I kept seeing her name over and over again in these groups. I emailed my scans to Dr. Del Rivero and they gave their recommendations.
What helped was this was all government-funded, so it’s all covered. For me, it was perfect because, at a certain point, I couldn’t work anymore. The symptoms had worsened to where I would get very high blood pressure and resting heart rate, so I didn’t feel like it was safe for me to work. I was afraid to even get up and use the restroom because my heart would start pounding like crazy.

Treatment
Discussing the Treatment Plan
I had a very skilled expert team collaborating with a local hospital that I knew would work with them. We put together a game plan for the first steps.
At my oncology appointment, we had a full discussion of where I stood and what things were looking like. I knew a lot about it because I read and listened to experts talk about it, so it didn’t come as a shock to me.
I had to get set up with an endocrinologist as well. The day after my appointment, I had a port put in and then the next day, I had chemo. That’s how quickly things started moving.
When I got to the hospital, they told me I was going to be there for a few days. It’s very intensive. It’s four days of infusions.
EDP Chemotherapy
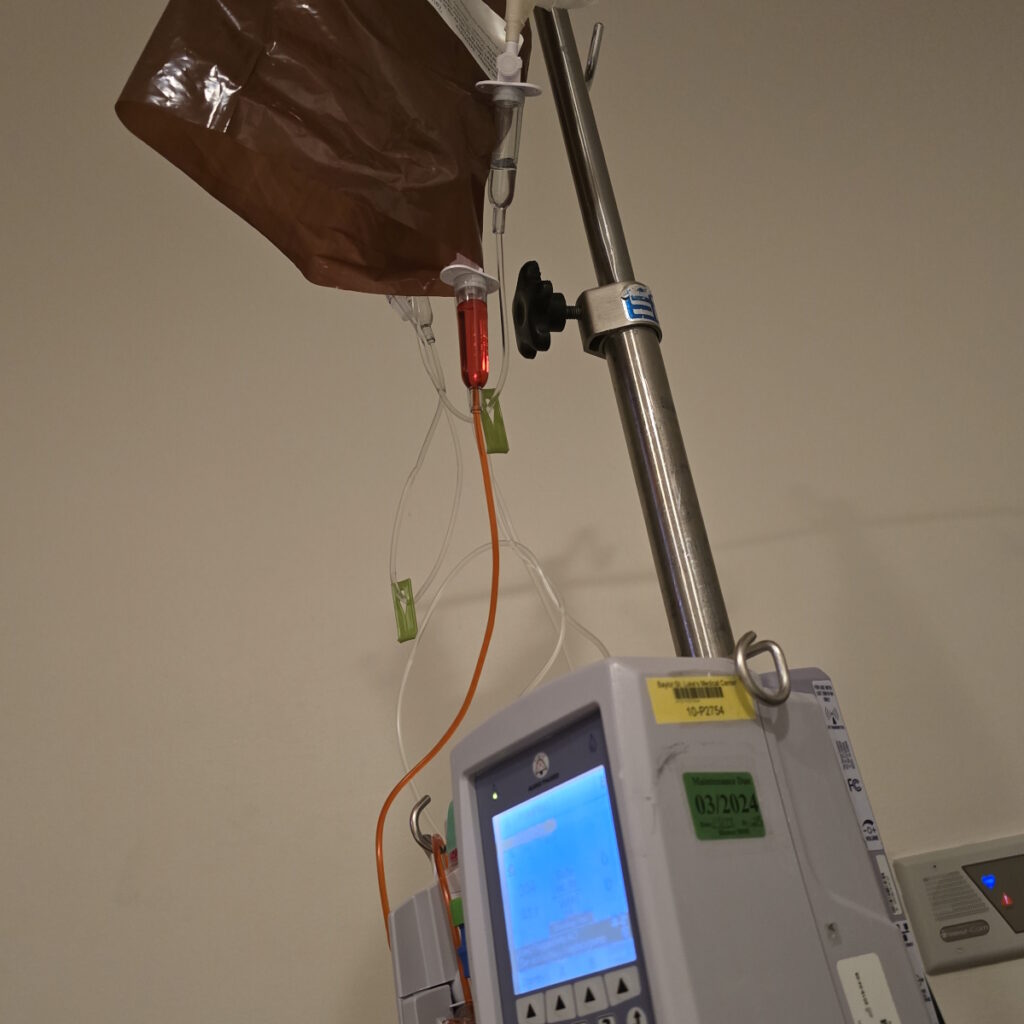
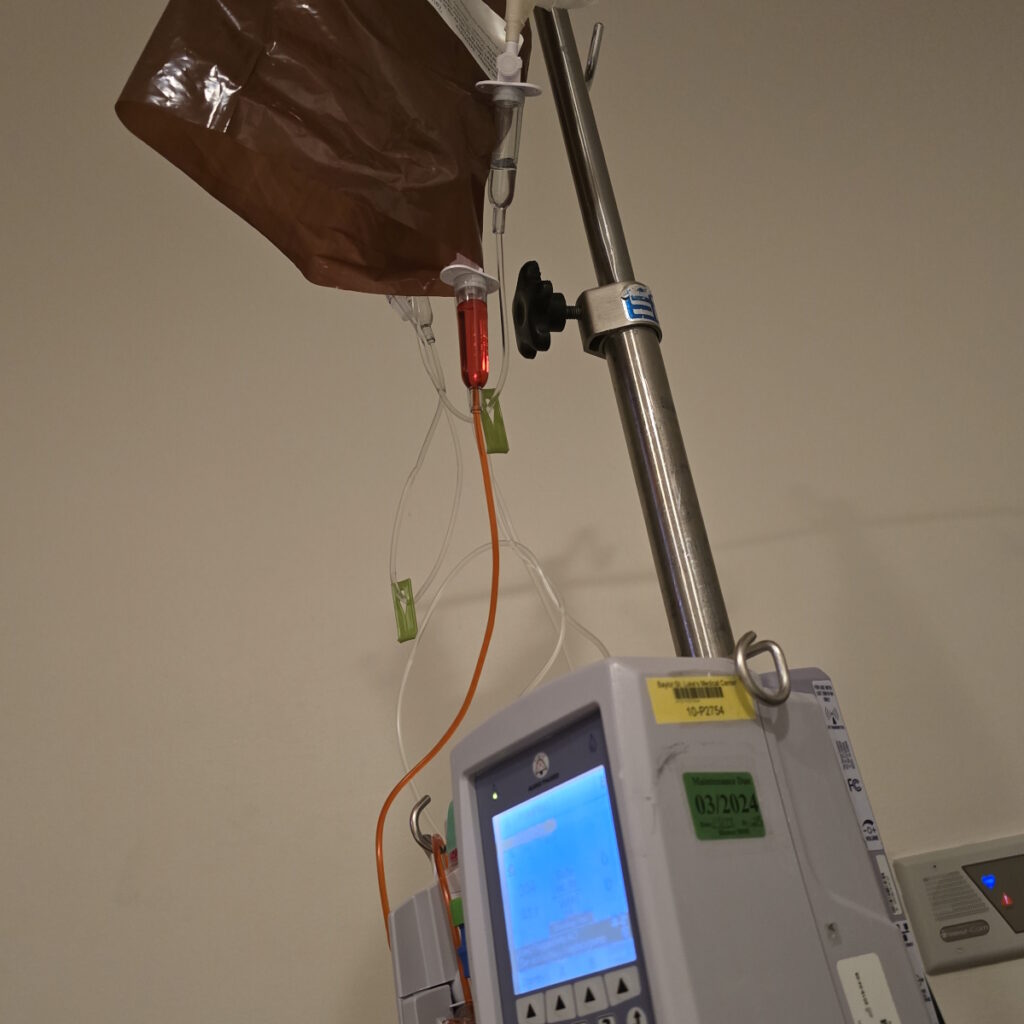
Unfortunately, ACC patients don’t have a lot of FDA-approved treatment options. We only have one line of chemo, EDP (etoposide, doxorubicin, and cisplatin), and that’s done inpatient.
I showed up to my first chemotherapy session thinking I was going to go home after an infusion. But when I got to the hospital, they told me I was going to be there for a few days. It’s very intensive. It’s four days of infusions and the first day is doxorubicin, which is otherwise known as the Red Devil.
Before they start chemo, they have to do all sorts of tests to make sure your heart’s okay and I didn’t have any issues there. On the second day, I had etoposide and then on the third and fourth days, I had a combination of etoposide and cisplatin. Usually, I’d be in the hospital for five or six days.
Side Effects of EDP Chemotherapy
The first and second cycles were the worst by far. My body didn’t know what hit it and by day two, I was hugging the toilet. I remember thinking, This should be temporary. This is what happens. This is what you think of when you think of chemo. I almost felt so bad that I didn’t care. It was strange.
My blood counts were low too and made me feel so out of it. By the end, I needed a blood transfusion because I was right on the cusp of my counts being too low. They wanted to be on the safe side. I had a lot of fatigue for about a week.
There was a lot of vomiting. I’m already a small person, so I didn’t have a lot of weight to lose to begin with. My heaviest before my diagnosis was 108 lbs and I’m only 5 feet tall. I learned how to cope over time. I figured out that I could tolerate mac and cheese and that’s all I would eat. I made it through.
I had to wear a medical bracelet everywhere I went because if I got stressed out, sick, or developed a lot of pain, I could go into an adrenal crisis.
Mitotane
While doing chemo, I was taking mitotane, the only FDA-approved medication for adrenocortical carcinoma that’s been used since the 60s. What it does is shut down adrenal function and supposedly help shrink things, but more often than not, it slows things down. They use it in conjunction with chemo.
By my second round of chemo, I was taking nine pills per day. They would make me gag because they were enormous and very chalky, which would cause more throwing up.

Side Effects of Mitotane
I developed hypothyroidism due to that medication. It does a lot of damage to the body. It shuts down your adrenal glands so they don’t produce cortisol anymore. Then you have to take hydrocortisone, which is like synthetic cortisol. You have to have cortisol or things get very bad and you could end up in an adrenal crisis.
I had to wear a medical bracelet everywhere I went because if I got stressed out, sick, or developed a lot of pain, I could go into an adrenal crisis because my body wasn’t producing cortisol, which is a stress hormone. I didn’t know a lot about it before all of this started.
I have to have emergency injections now. It’s almost the same concept as an EpiPen, but it’s more difficult to administer because you have to draw up the medication. If I’m ever on the verge of an adrenal crisis, I have to inject myself and then go to the ER, but we don’t think that’s going to happen.
I’m off of that medication now, but my adrenal gland is still not producing enough cortisol to not take hydrocortisone, so I have to give myself thyroid hormones and synthetic stress hormones. These are all side effects of the treatment and not because of the cancer.
We saw shrinkage. They recommended for me to do a third round of chemo because we were trying to get to surgery so I could get the tumor removed.
Mid-Treatment Scan
By the time I was going to start chemo, the tumor had grown to 16 cm and it was so painful. The pain went away almost immediately after the first cycle. I was going to get two rounds of EDP and get a scan to see if it was responding. Thankfully, we saw shrinkage. They recommended for me to do a third round of chemo because we were trying to get to surgery so I could get the tumor removed.
I was going to NIH to get that done by one of their amazing surgeons, Dr. Hernandez. They typically keep the tumors and do different treatments to see what might work.

I was getting my third round in the hospital when I got the call saying they had approved my surgery, so that helped me push through. I was so happy. Initially, I didn’t know if we were going to get surgery or not. I’ve seen people not make it through the beginning stages of chemo and even have their tumors removed before things got bad. The ultimate goal is to get the tumor out. The faster you can do it, the better.
Other than my port insertion, I have never had surgery in my life. We started preparing for a trip up north for a massive surgery.
I eventually had to do more chemo after surgery, but it ended up not working anymore during my fourth and fifth rounds. I had my last cycle in February 2024.
Things are trending in the right direction, so I’m hopeful that this new treatment is working.
Targeted Therapy
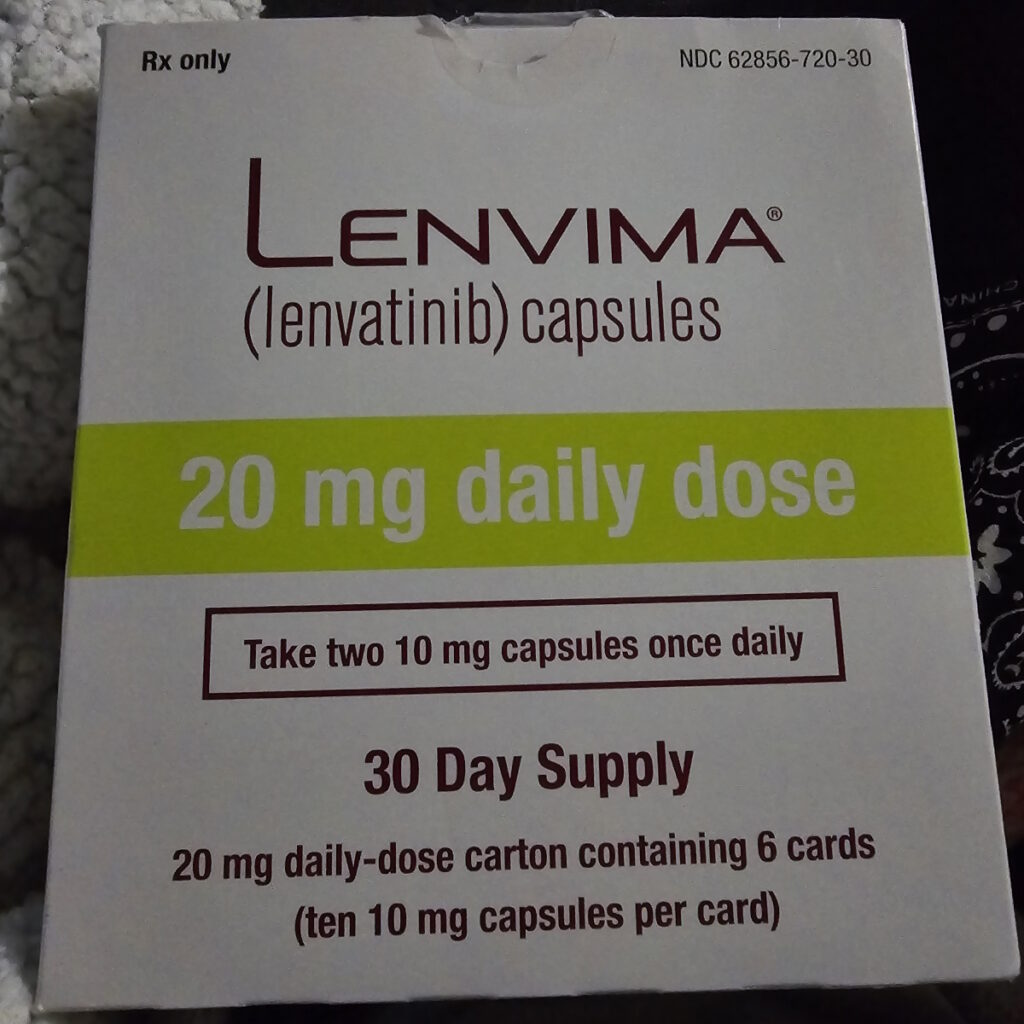
They pulled me off mitotane and put me on lenvatinib, a TKI inhibitor. I don’t have many side effects from it. They use that in combination. It’s better than Keytruda (pembrolizumab) alone.
I only have to take two pills a day now. Symptom-wise, as far as the cancer goes, I feel way better. There are some indicators, like some tumor markers, that have significantly gone down. My team is seeing that things are trending in the right direction, so I’m hopeful that this new treatment is working.
I know some people in my support group who are on the same combination and they’re having amazing results. They’re stage 4 like me with no evidence of disease.

Mental Health Care
It feels like I’m making two steps forward and one step back, but now I feel like I’m moving forward at a steadier pace. It was difficult in the beginning because I didn’t have many coping mechanisms. I had never gotten therapy in my life. I thought I was so healthy—and I—was until cancer came into my life.
I didn’t expect cancer. If I was going to have any health problems, cancer was not what I thought it could be. It doesn’t run in my family. I’ve done genetic testing and I tested negative for everything they tested me for.
When I was trying to wrap my head around this, I thought, Why me? And why such a rare cancer? I don’t fit in the age bracket for the age that this affects people. It’s usually middle-aged women, young children, and some middle-aged men. More often, it’s women between their 40s and 60s. I’ve met some friends through the support group who are around my age, but it’s much more rare.
I struggled with why. I wanted to know. I felt like I would get some sort of closure if I knew that, but I don’t know if I’m ever going to get the answer.
I’m getting a lot of help in areas I’ve never had help in, so in a way, I’m rebuilding myself and enriching my life.
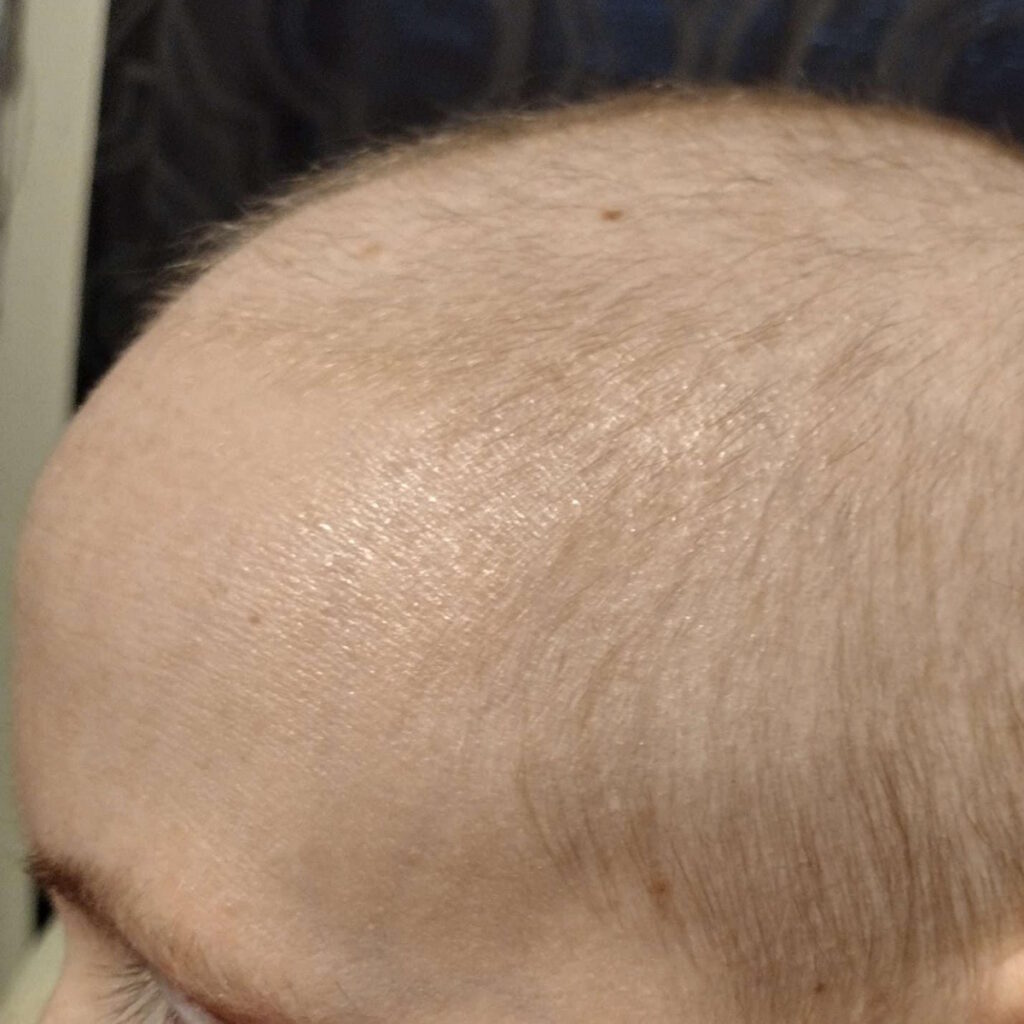
I struggled with body image because after my surgery, I was down to 82 lbs and that played a part in my mental health. I felt helpless because I realized there were so many things I couldn’t do, mostly due to the side effects of the medications I was on.
I would be wiped out and I wasn’t used to that. It hit me out of nowhere. I went from being a fixer or a helper to somebody who needed help. I didn’t know how to do that. It was painful for me to adjust.
For a long time, it was one of the most difficult parts for me mentally, especially after surgery because I was in horrible pain. It was an open surgery, so I have a scar from right under my rib cage to past my belly button. It’s probably 10 to 11 inches long.
After surgery, I had to get a lot of help with doing basic tasks. I felt awful for the people having to take care of me because this wasn’t who I was and that was a huge adjustment. I didn’t know how to cope.
I wasn’t getting therapy at the time, but I am now through MD Anderson, which is amazing. I see a counselor and I feel like my mental health is the best it has ever been despite my diagnosis. I’m getting a lot of help in areas I’ve never had help in, so in a way, I’m rebuilding myself and enriching my life. It’s amazing how these resources have been helping me.


I’m using the time that I have now to get my mental health where it needs to be, which in my opinion should be better than it was even before I was diagnosed. I’m working on myself. I see it as an opportunity.
I’ll never be happy that any of this happened, but I have the time and resources now and I’m seeing some benefits. I’m learning a lot of coping mechanisms in how to deal with things in the future.
If the treatment’s working and I don’t have that many side effects, that’s a win-win. I’ve seen nothing but improvement since going to MD Anderson.
There’s no telling where I would be right now if I hadn’t made those choices to focus on what I needed to do to get myself where I needed to be.
Words of Advice
Don’t let the doctors dictate what happens to you. If you have a gut feeling, act on it. Don’t be afraid to get second opinions. Seek out experts. There are usually other routes that you can take. There are so many resources out there. It was difficult for me in the beginning, but once I got everything set up and figured out, I told myself I may have saved my life with these changes.
There’s no telling where I would be right now if I hadn’t made those choices to focus on what I needed to do to get myself where I needed to be. One thing that they would always repeat in my support groups is don’t let location dictate your treatment, who you see, or who you get your recommendations from. If that’s a problem, then start looking into things. You’d be surprised at how many resources are available out there.
Don’t idly sit back and let things happen if things don’t feel right. Talk to multiple people. Join support groups. Not only do they provide great advice, especially in my case when there’s not a lot of information, but the sense of community that you get from it is priceless. I have made so many amazing friends in the ACC community.
There are usually support groups for every diagnosis that you can think of. Mine is so rare and there are three that I’m on. If I find someone with my diagnosis, the first thing I always think of is to try to plug them into the support groups. It helps in so many different ways that it might change the whole trajectory.


Inspired by Ashley's story?
Share your story, too!
More Rare Cancer Stories
Regina J., Lung Neuroendocrine Tumor
Symptoms: Wheezing, back pain, coughing that sometimes produced blood
Treatment: Surgery (partial lung resection)
...
Tabbie V., Pancreatic Neuroendocrine Tumor (pNET)
Symptoms: Abdominal pain, unusual organ "inflammation" feeling when walking, fatigue
Treatments: Chemotherapy (oral and IV), surgeries (Whipple procedure or pancreaticoduodenectomy, liver resection or partial hepatectomy)
...
Hayley O., Pancreatic Neuroendocrine Tumor (pNET)
Symptoms: Severe right-sided pelvic pain, nausea, diarrhea
Treatment: Surgery (pancreaticoduodenectomy or Whipple procedure)
...
Drea E., Gastric Neuroendocrine Tumor (gNET), Stage 3, Grade 1
Symptoms: Fainting spells, fatigue, dizziness, anemia, shortness of breath, absence of menstruation, unexplained weight loss, night sweats
Treatment: Surgery (total gastrectomy with a Roux-en-Y reconstruction)
...
Caroline C., Gestational Trophoblastic Neoplasia & Placental Cancer, Stage 3
Symptoms: Morning sickness & an unusually high beta hCG
Treatment: EMACO chemotherapy
...
Shannon W., Choriocarcinoma
Symptoms: Molar pregnancy, vaginal bleeding, overall feeling of unwell, cramping, weight loss, elevated HCG level, feeling bloated
Treatments: Chemotherapy, surgeries (D&C, total hysterectomy)
...





