Small Changes, Big Impact: Easing Myeloma Treatment Side Effects
Multiple myeloma advocate Valarie Traynham is joined by Donna Catamero, Associate Director of Myeloma Research at the Icahn School of Medicine at Mount Sinai and a nurse practitioner specializing in the treatment of multiple myeloma patients, and Abbey Reiser, a dietitian/nutritionist and board-certified specialist in oncology nutrition from the Ruttenberg Treatment Center The Tisch Cancer Institute, to share practical strategies for handling side effects, optimizing nutrition, and improving quality of life.
Interviewed by: Tiffany Drummond
Edited by: Katrina Villareal
- Introduction
- Difference Between Relapsed and Refractory Multiple Myeloma
- Common Symptoms of Relapsed/Refractory Multiple Myeloma
- Current Treatment Options for Relapsed/Refractory Multiple Myeloma
- Easing Multiple Myeloma Treatment Side Effects
- Eating the Rainbow
- The Role of Hydration in Managing Kidney Function and Oral Health
- Foods and Drinks That Multiple Myeloma Patients Should Avoid
- Avoiding Green Tea Supplements
- Managing Weight Changes
- Common Skin Conditions Multiple Myeloma Patients Experience
- Bispecific Antibodies for Relapsed/Refractory Multiple Myeloma
- Common Side Effects Associated with Newer, Targeted Therapies
- Specific Strategies for Managing Cytokine Release Syndrome and Neurological Side Effects
- Dietary Changes to Help Manage Loss of Taste
- Coping with the Emotional Challenges of Relapse
- Final Takeaways
- Conclusion
Introduction
Tiffany Drummond: I’m a patient advocate with over 20 years of experience in cancer research. My journey began as a caregiver when my mother was diagnosed with endometrial cancer in 2014. I quickly realized the challenges of finding resources, support, and shared experiences, and now I’m committed to helping others, no matter the condition.
At The Patient Story, we create programs to help you figure out what comes next. Think of us as your go-to guide for navigating not only the cancer journey but your overall health journey. From diagnosis to treatment, we’ve got you covered with real-life patient stories and educational programming with subject matter experts. I’m your personal cheerleader to help you and your loved ones best communicate with your healthcare team as you go from diagnosis through treatment and survivorship.

The Patient Story retains full editorial control over all content. We want to thank all of our promotional partners for their support. Because of them, our programming reaches the audience who needs it. I hope that you find this program helpful, but please keep in mind that while the information provided is encouraging, engaging, and insightful, it is not a substitute for medical advice.

ANP-BC, OCN, CCRC

MS, RDN, CDN, CSO

Patient Advocate
We are joined by two experts from The Tisch Cancer Institute at Mount Sinai in New York. First up is Donna Catamero, Associate Director of Myeloma Research at the Icahn School of Medicine at Mount Sinai and a nurse practitioner specializing in the treatment of multiple myeloma patients. We also have Abbey Reiser, who has a unique role as part of the multidisciplinary team at the cancer institute’s Ruttenberg Treatment Center. She is a dedicated dietitian/nutritionist and is also board-certified as a specialist in oncology nutrition. Valarie Traynham, a multiple myeloma survivor and thriver and an inspiration to many, will moderate this conversation. Your journey is one of inspiration. I’m excited about this engaging discussion.
Valarie Traynham: I’m a myeloma and breast cancer thriver. I’ve been on the myeloma journey for about nine years and the breast cancer journey for about five years. I can understand the issues when it comes to treatment side effects, so I am so excited to be here and have this conversation with these two ladies.
Difference Between Relapsed and Refractory Multiple Myeloma
Valarie: Donna, can you explain the difference between relapsed and refractory disease? I get this question a lot and it can be confusing to some of the patients.
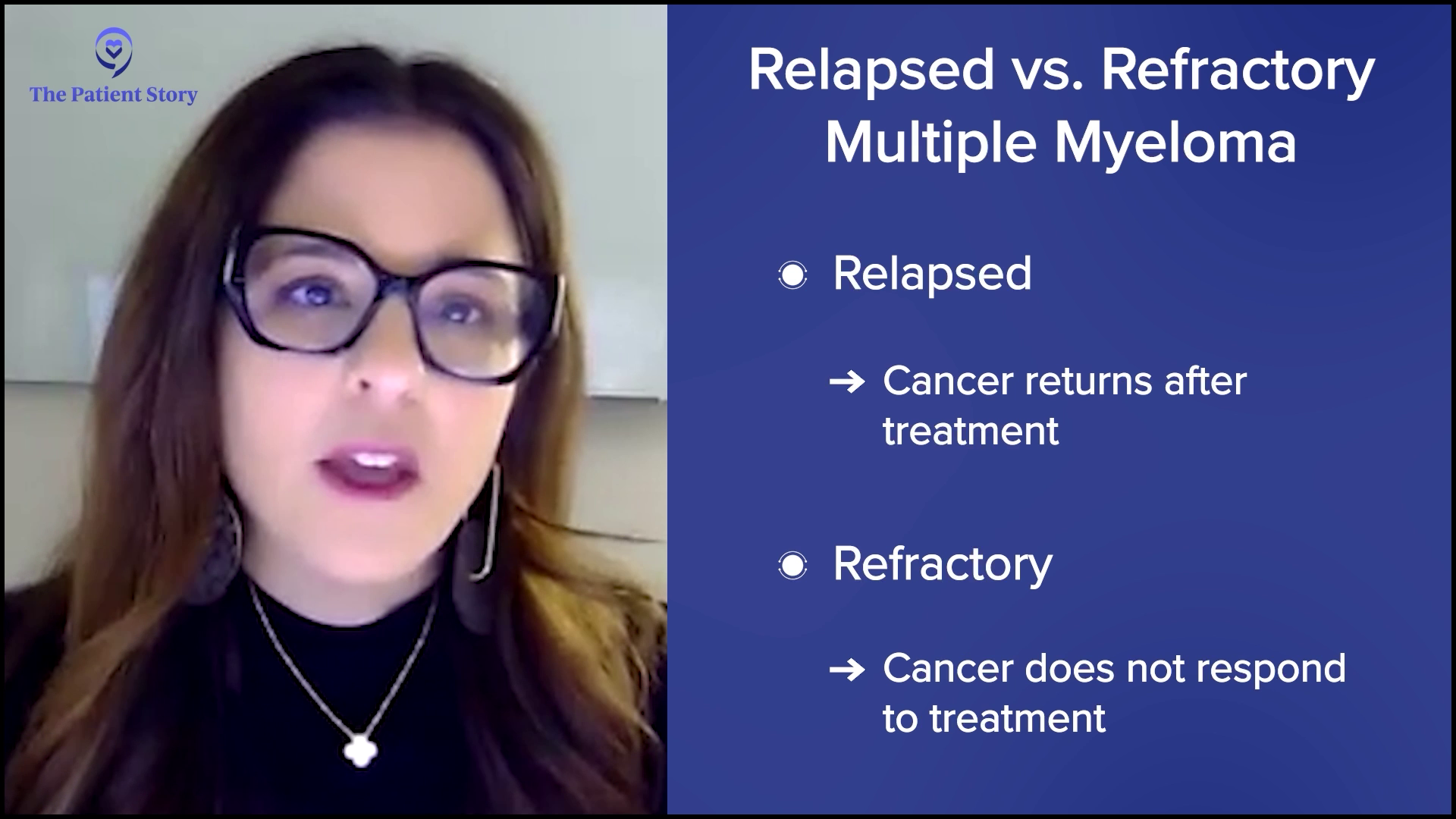
Donna Catamero: Most patients are both relapsed and refractory. Relapsed is when a patient has an initial response to therapy, so they’re either in complete remission, partial remission, or very good remission, and then their disease starts coming back, which means they’re relapsing from their response.
Refractory is when patients are on therapy and start to relapse, so that means they’re refractory to that therapy. Most myeloma patients are on continuous therapy, so when they start to relapse, they’re going to be a relapsed patient and then refractory to the current treatment thereon. Most patients past their first line of therapy are going to be relapsed/refractory.
Common Symptoms of Relapsed/Refractory Multiple Myeloma
Valarie: When we think of relapsed/refractory, what are some of the common symptoms? Is it just like when we are first diagnosed with myeloma? Is it some of those same symptoms or is it totally different when it comes to the relapsed/refractory setting?
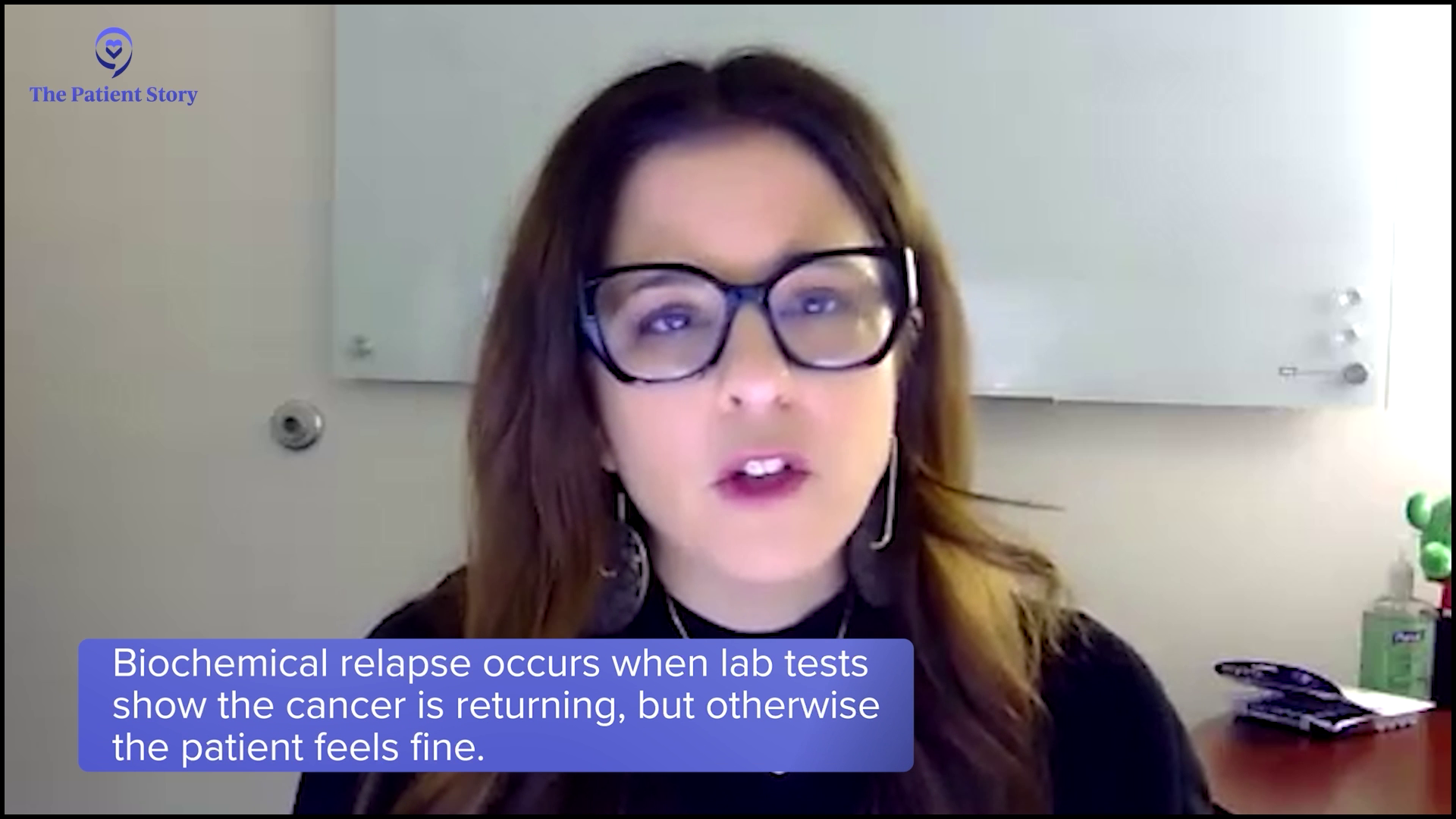
Donna: Patients fall into two categories. Some patients have a biochemical relapse, which means only their numbers are going up. We monitor myeloma patients through their labs. We look at their protein levels and see an increase, but otherwise, the patient feels fine. On paper, we see that their cancer is coming back.
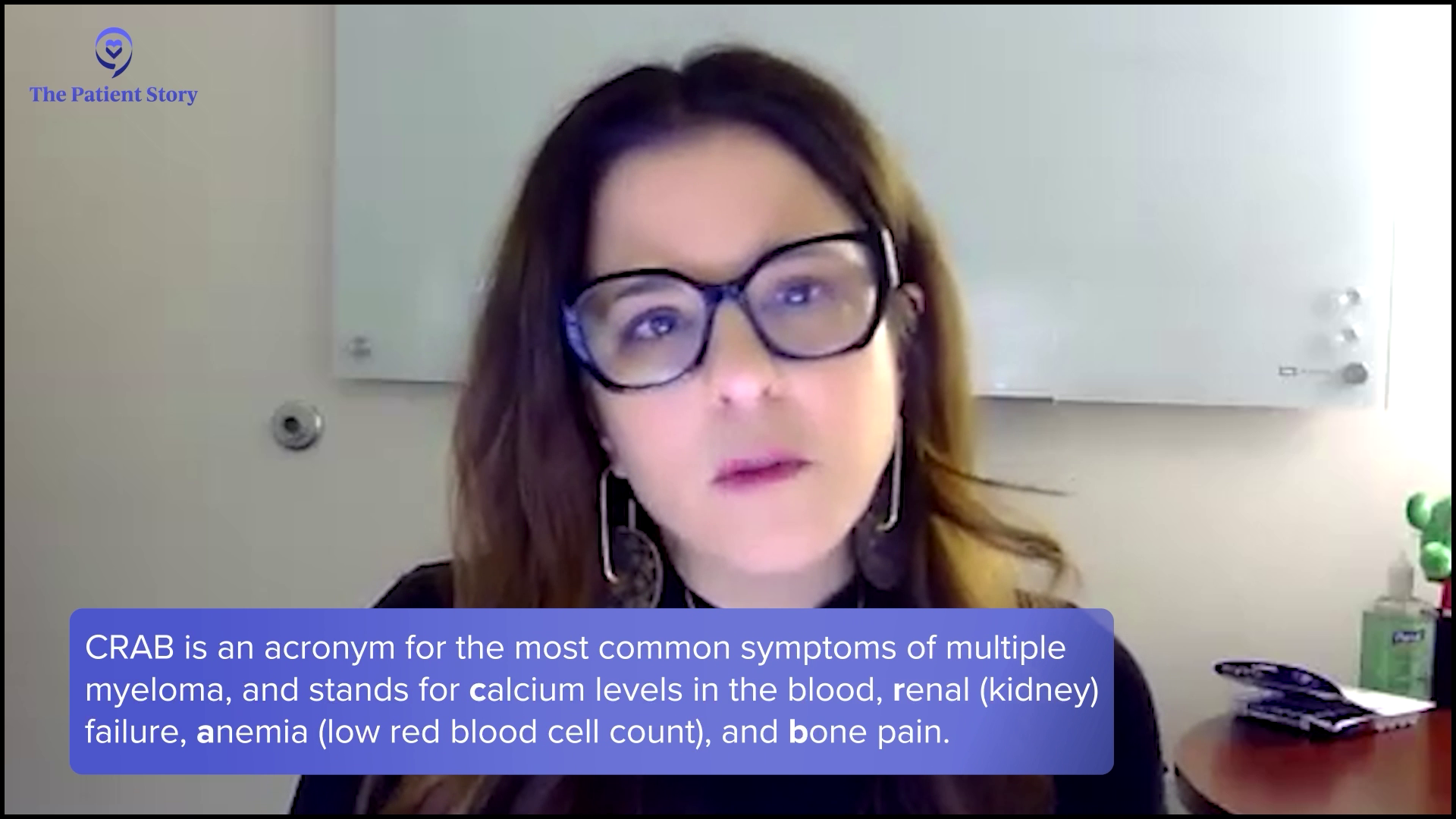
On the other hand, a patient can have a symptomatic relapse, so they’re either more anemic (A), have new bone disease (B), new renal (R) insufficiency or kidney disease, or elevated calcium (C) in their blood. These are the typical CRAB symptoms of myeloma, so they either have those or none at all and we’re seeing the cancer in their blood work.
Current Treatment Options for Relapsed/Refractory Multiple Myeloma
Valarie: What are some of the current treatment options for relapsed and refractory multiple myeloma?
Donna: The landscape of treating relapsed/refractory myeloma is so quickly evolving. We have so many new therapies. In the past five years, we’ve had so many approvals for multiple myeloma patients in the relapsed setting, so it’s a very exciting time.
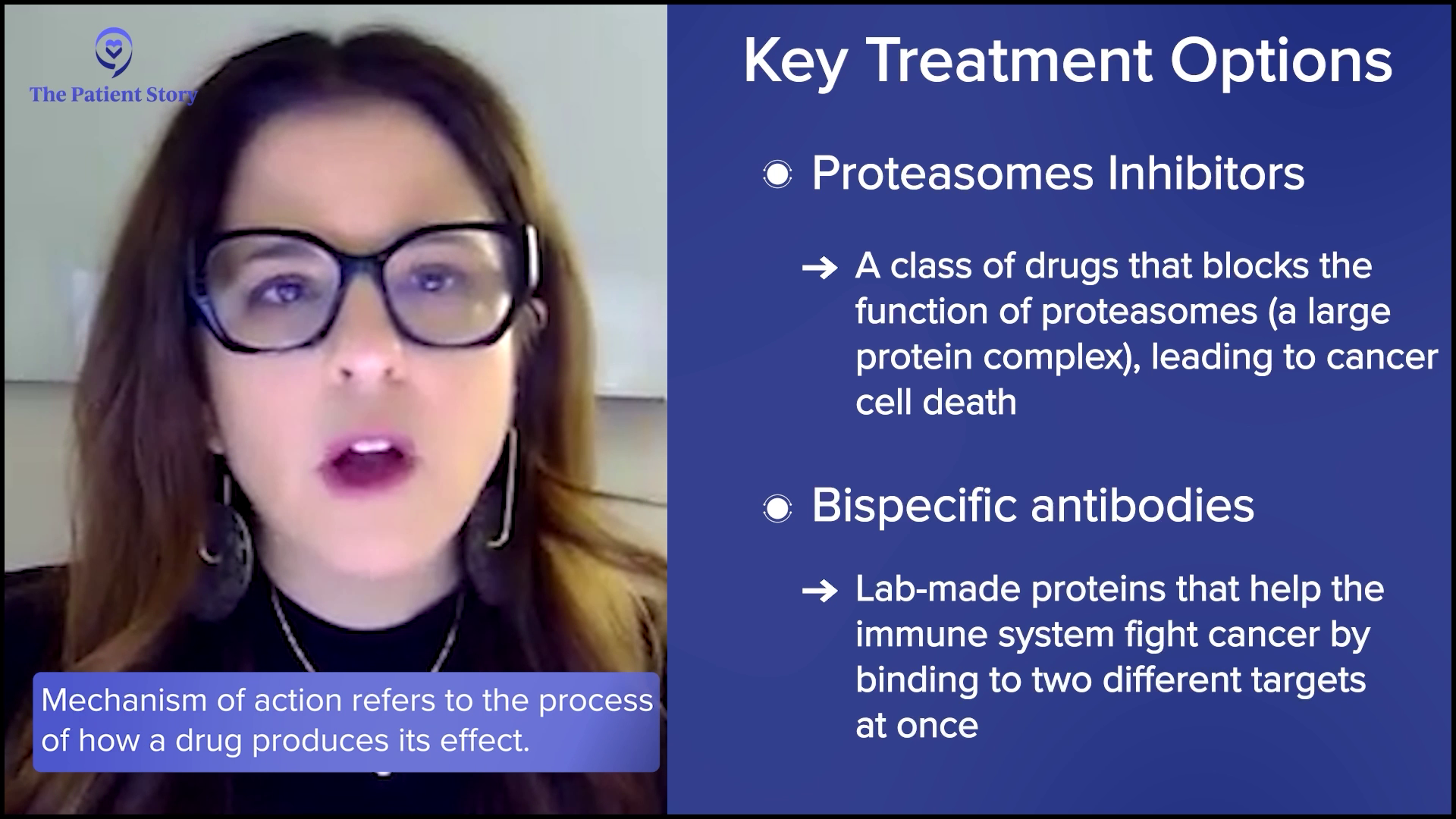
We have more targeted approaches with proteasome inhibitors, like kyprolis and bortezomib, that we can use in the relapse setting. We have more novel mechanisms of action, so more targeted towards the immune system, like bispecific antibodies for patients who’ve had four prior lines of therapy and then CAR T-cell therapy, another immunotherapy, which is very exciting for patients. It was initially approved for patients who had four prior lines of therapy, but now we can use CAR T-cell therapy in patients after one prior line of therapy.
Valarie: That’s awesome. I always get excited when I think of the therapies that we have since I’ve been diagnosed and even the therapies in the pipeline. It’s given us so much hope as patients.

Easing Multiple Myeloma Treatment Side Effects
Valarie: Abbey, how can a well-balanced diet specifically benefit multiple myeloma patients undergoing treatment?
Abbey Reiser: Diet recommendations often change throughout treatment based on how patients feel and if they experience any side effects that affect their appetite and/or their ability to eat. For multiple myeloma patients who are feeling an eating well, the nutrition recommendations are the same for most other cancers, which is also consistent with the recommendations for the general population.
Plant foods, like fruits, vegetables, whole grains, beans, nuts, and seeds, contain a variety of cancer fighters, including vitamins, minerals, fiber, and phytochemicals. Phytochemicals are naturally occurring compounds in plants that have the potential to stimulate the immune system, reduce inflammation, and fight infection, making these foods especially beneficial for patients to consume while undergoing treatment.

Protein can also help to boost the immune system, promote healing, and build cells, tissues, and muscles. We encourage choosing a variety of lean, animal-based and plant-based proteins, including chicken, fish, turkey, tofu, beans, and nuts. The current plant-based eating model recommends filling two-thirds or more of your plate with plant-based foods and one-third or less of your plate with animal protein to create a well-balanced meal.
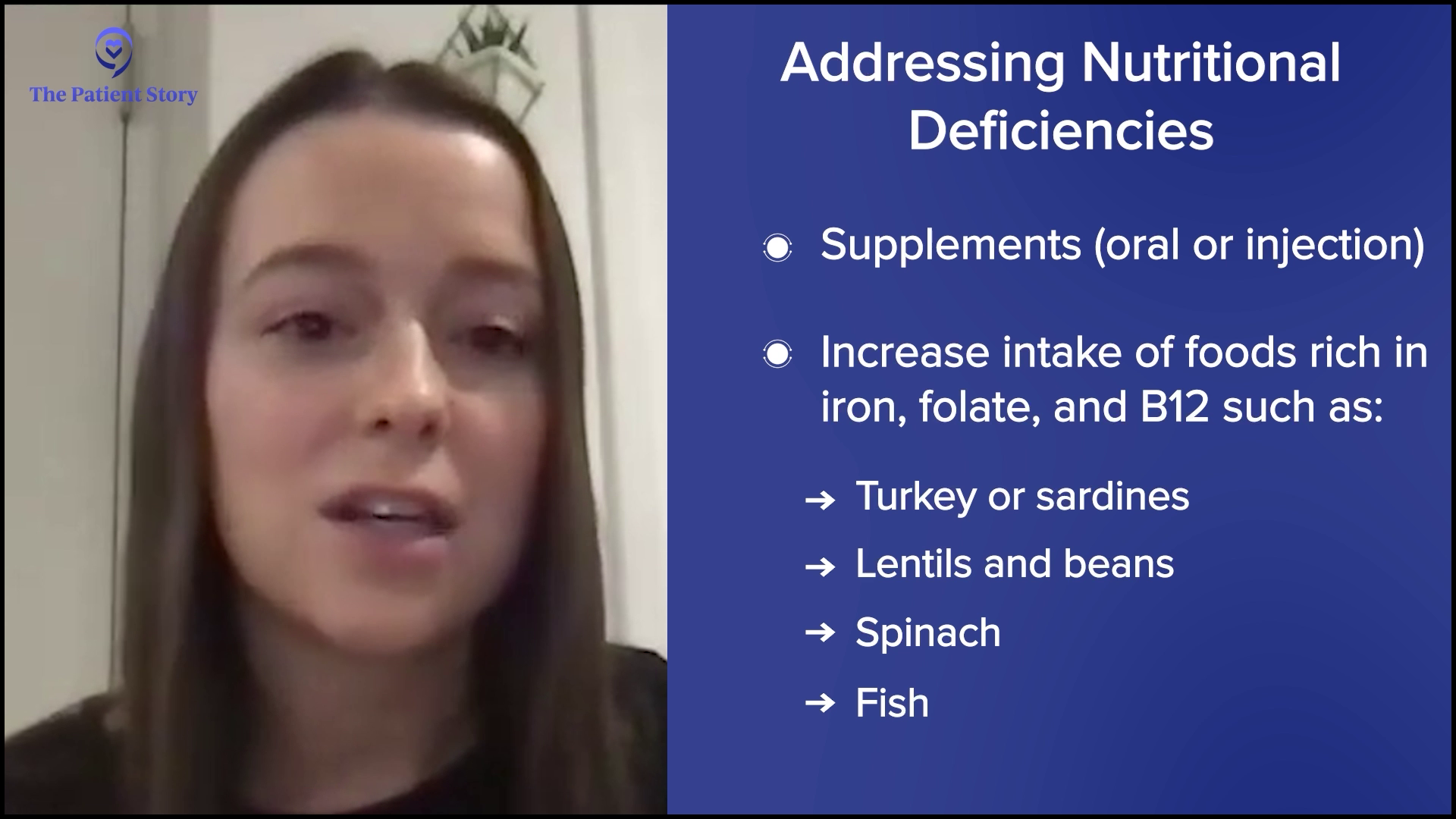
Valarie: Are there certain nutrients or dietary patterns that can help manage side effects like fatigue and anemia?
Abbey: Definitely. Patients who experience side effects from treatment may find it difficult to follow a plant-based diet to a tee. Fatigue is one of the most common symptoms among myeloma patients and one of the most common side effects of treatments. I typically recommend staying as active as you can, eating often, and adequately drinking plenty of fluids. Try planning ahead by asking for help with meal prep, trying meal delivery services, and keeping ready-to-eat snacks on hand, like nuts, granola bars, or pre-made protein shakes.

Anemia is commonly caused by the disease, treatments, or kidney dysfunction caused by multiple myeloma and cannot be improved by diet. However, nutritional deficiencies such as iron, B12, or folic acid can also be a cause, and this can be improved by supplementation either orally or by injection. It also couldn’t hurt for patients with these deficiencies to increase their intake of foods rich in these vitamins and minerals, such as turkey, sardines, lentils, and beans for iron, lentils, beans, and spinach for folate, and fish and dairy for B12.
Typically, I encourage patients to talk to their doctor about the cause of and plan of care for anemia before making any significant changes to the diet or starting a new supplement.
Eating the Rainbow
Valarie: As a patient, we’re often told to eat the rainbow. Is that something you recommend?
Abbey: Yes. If their appetite is good, they’re feeling well, and they can eat a variety of fruits and vegetables, I’m all for it because they’re going to get different nutrients from different colors. That’s definitely a recommendation that’s still staying strong to this day.
The Role of Hydration in Managing Kidney Function and Oral Health
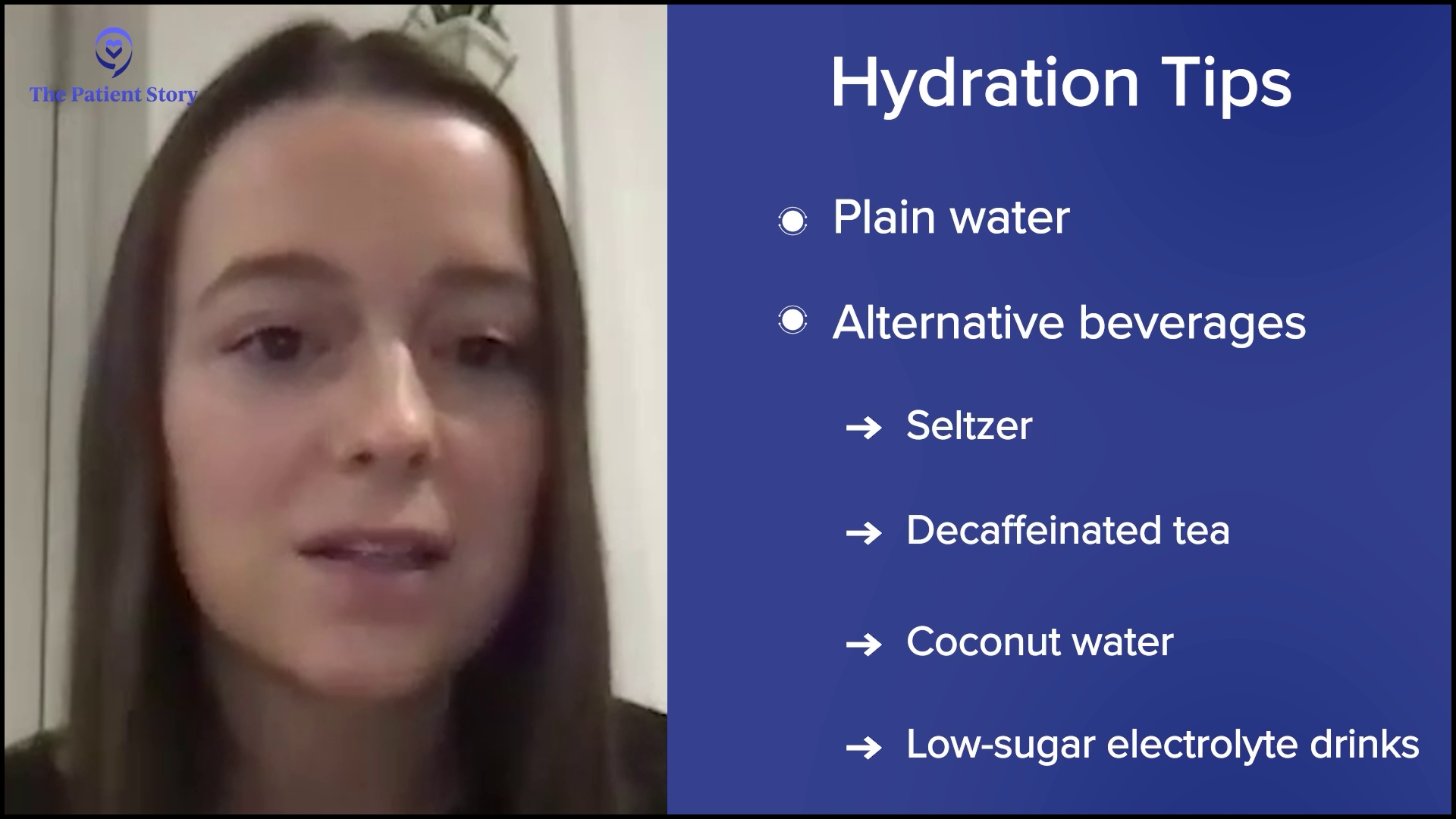
Valarie: We often hear about the role of hydration. Can you discuss that role in managing side effects of multiple myeloma treatment, such as kidney function and even oral health?
Abbey: Staying hydrated during myeloma treatment is essential, especially because dehydration can worsen kidney function, which is a common concern due to the disease’s impact on the kidneys. Drinking sufficient fluids helps to flush out waste products and manage potential complications, like high calcium levels, which can occur with myeloma. Bispecific treatments, like talquetamab, can cause oral toxicities including dry mouth, mucositis, and taste changes, and good fluid intake plays an important role in managing these side effects.
I recommend aiming for at least 8 to 10 8-ounce glasses of low-sugar fluids per day. Plain water is the gold standard and the preferred beverage for hydration, but other beverages such as seltzer, decaf tea, coconut water, and lower-sugar electrolyte drinks can also promote adequate hydration. Caffeinated beverages, like coffee, tea, and colas, as well as alcohol may worsen side effects like dry mouth, so I recommend limiting those.
Foods and Drinks That Multiple Myeloma Patients Should Avoid
Valarie: Are there any specific dietary considerations or restrictions that myeloma patients should be aware of? You mentioned alcohol and caffeine, but are there certain foods or drinks that they should strictly avoid?
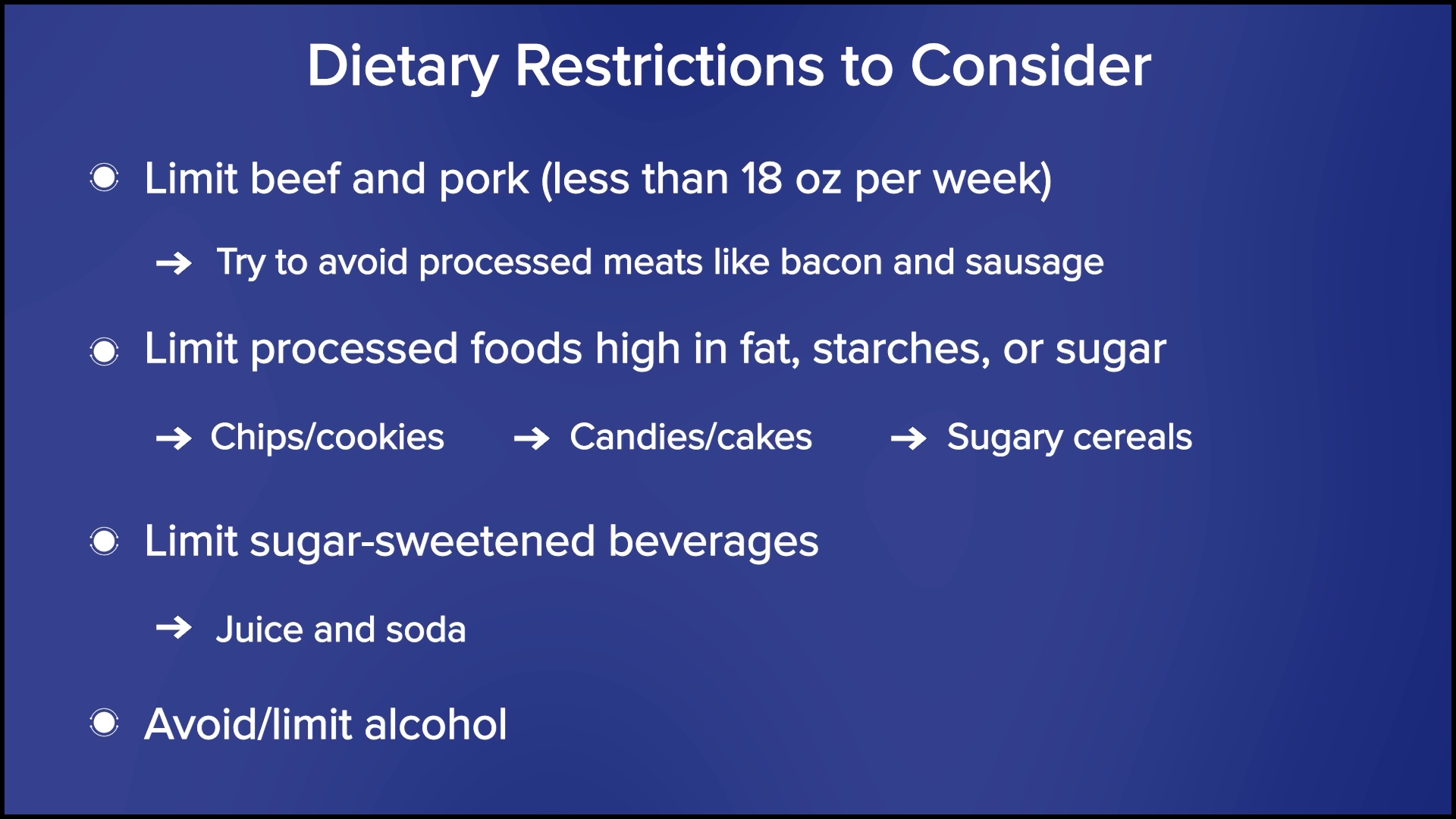
Abbey: A couple of limitations apply to every type of cancer. We recommend limiting red meat, such as beef and pork, to less than 18 ounces per week, and avoiding processed meats, like bacon and sausage, as much as possible.

I also recommend limiting processed foods that are high in fat, starches, or sugars, such as chips, cookies, candies, cakes, and sugary cereals. Patients should also limit sugar-sweetened beverages, like juice and soda, and avoid or limit alcohol. General guidelines recommend no more than two alcoholic beverages per day for men and one drink per day for women, but I typically defer questions regarding alcohol to the doctor.
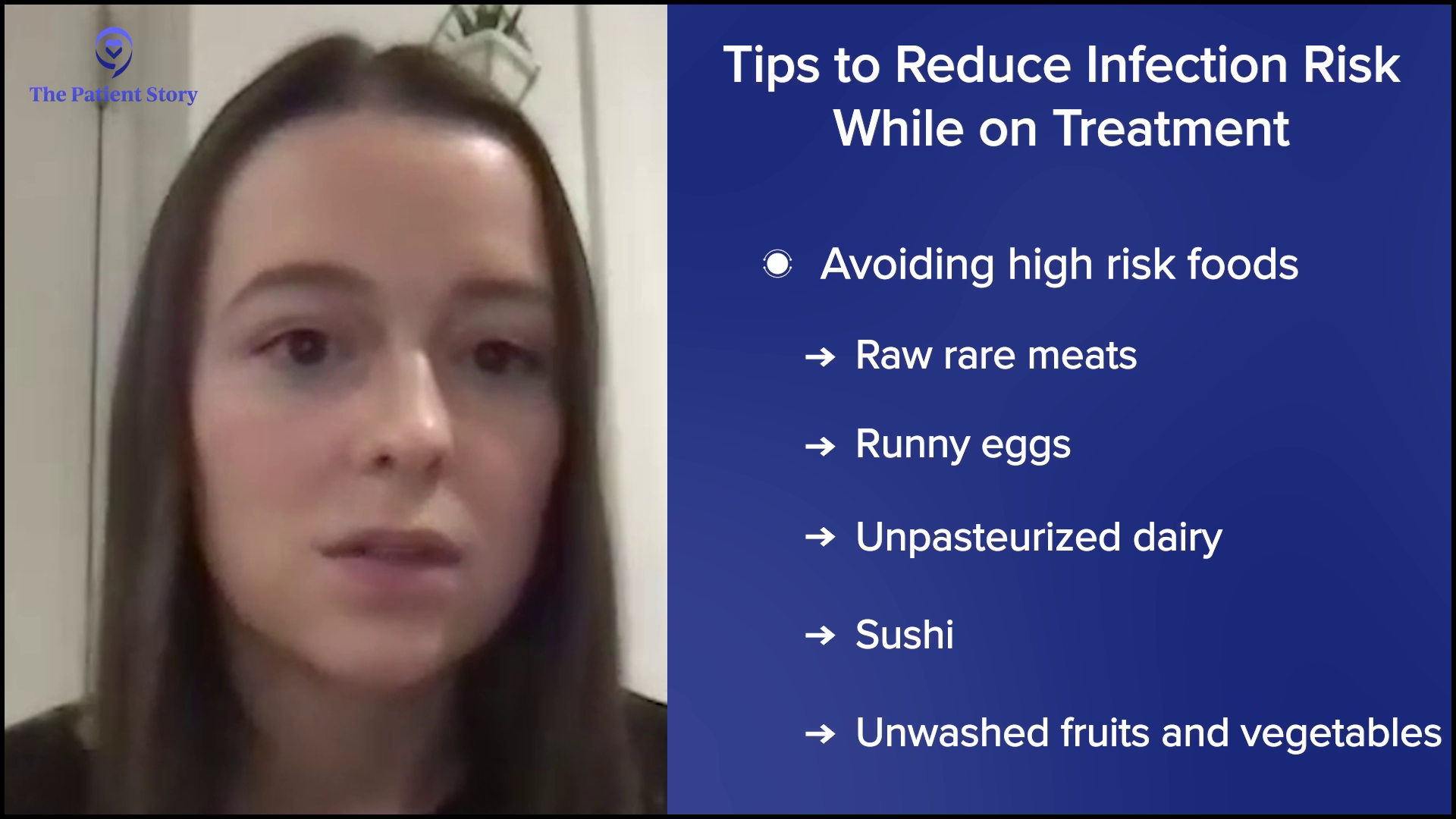
Multiple myeloma and its treatments can weaken the immune system and increase the risk of infection, which can make patients more susceptible to foodborne illness, which we often call food poisoning. Therefore, it’s important to follow food safety guidelines while on treatment in an effort to reduce infection risk. General tips include washing your hands well, separating ready-to-eat food and raw meats, checking expiration dates, refrigerating leftovers immediately, and avoiding high-risk places, like salad bars and buffets, and high-risk foods, like raw and rare meats, runny eggs, unpasteurized dairy, sushi, and unwashed fruits and vegetables.
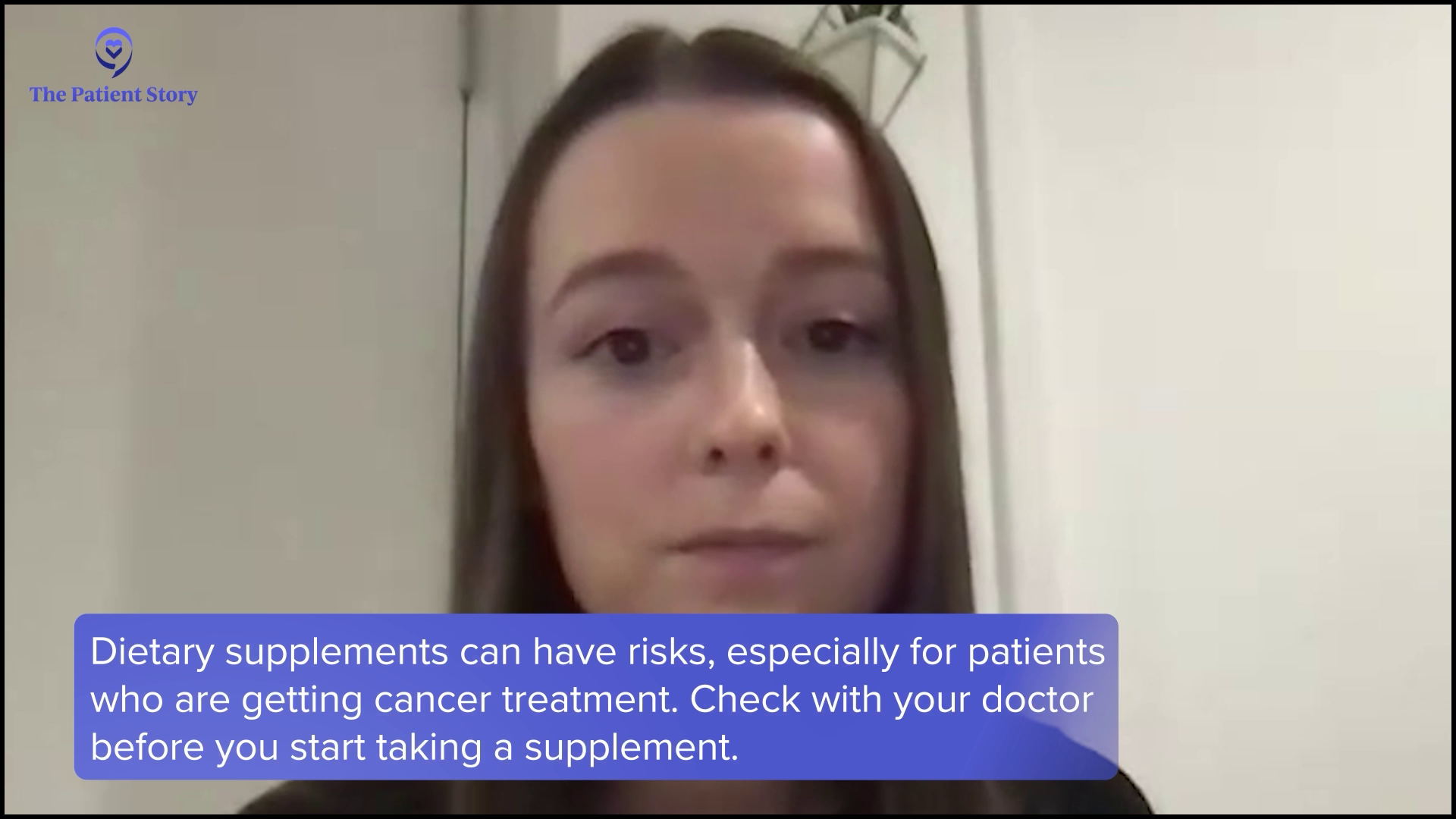
I also discourage the use of supplements, unless you have a deficiency or are told otherwise by your medical team. Supplements don’t offer the same benefits as eating whole foods. They’re typically not regulated by the FDA, and research tends to be limited in terms of how they may interact with treatment. For patients who are hoping to start taking a supplement, make sure to check with your doctor before doing so.
Avoiding Green Tea Supplements
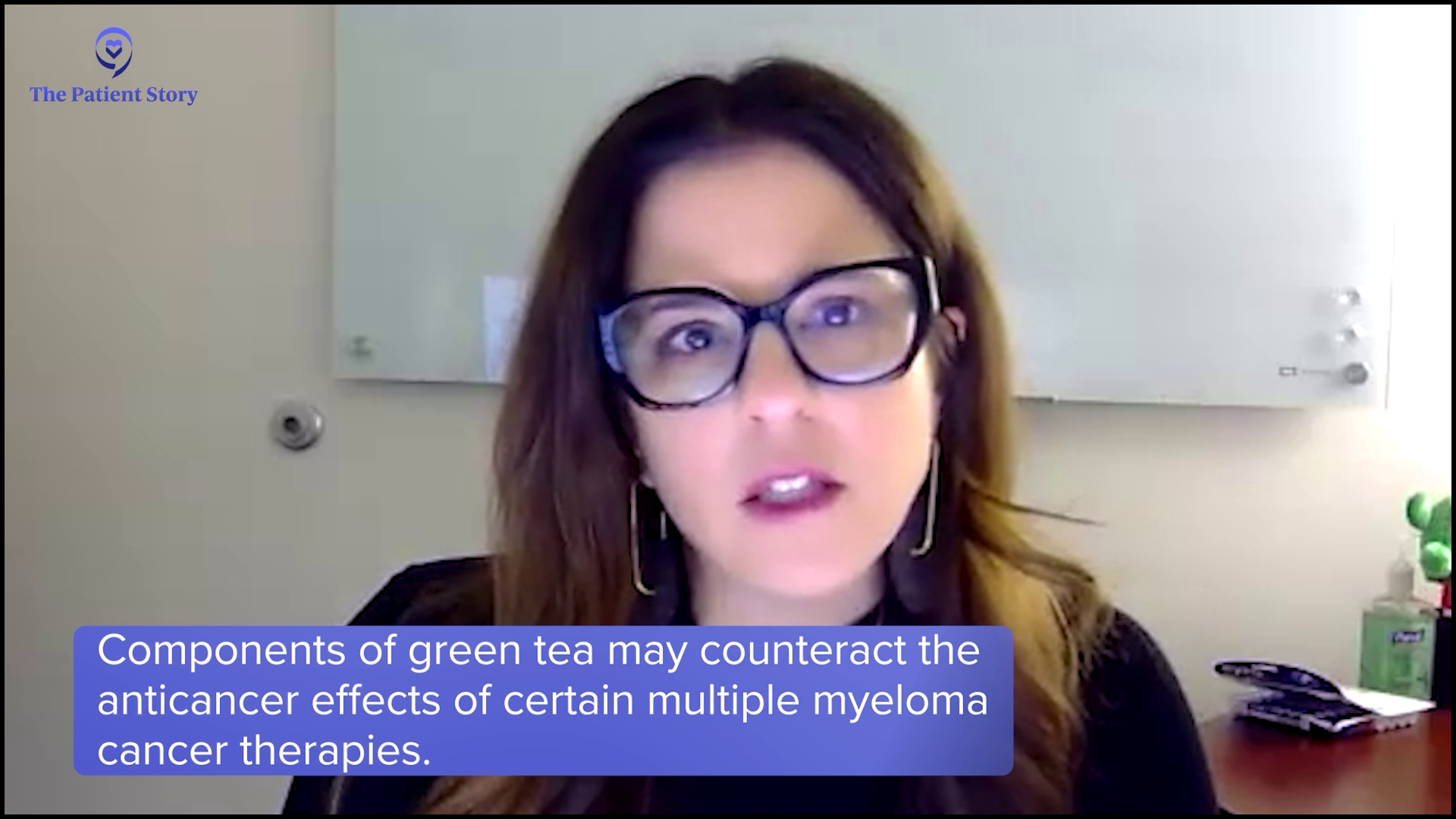
Valarie: What advice can you provide about green tea? With some treatments, they say to avoid green tea on the day that you’re getting treatment and a few days after. Is there anything you can say about that?
Abbey: That’s usually discussed if they’re on bortezomib. Donna, you and I talked about this before. I believe it’s the green tea supplement that they need to avoid entirely.
Donna: It’s the high-dose green tea extract that’s available as a supplement, which is contraindicated when on a regimen containing bortezomib. I advise patients who love green tea to not consume it on treatment days. The beverage itself is fine for patients. It’s the supplement that can get patients into trouble.
Managing Weight Changes
Valarie: How can a nutritionist help patients manage weight changes? I experienced a lot of weight gain taking steroids. Some patients deal with weight loss, which can be a common side effect of treatment. What can we do from a nutrition standpoint?
Abbey: Treatment side effects, especially oral toxicities, often lead to decreased appetite and weight loss. If a patient is experiencing unintentional weight loss, I recommend having small, frequent meals every 2 to 3 hours and choosing high-calorie foods as tolerated. I will emphasize healthy fat sources, like nuts and nut butters, avocado, and olive oil, because fat contains more calories per gram than proteins and carbs. I also encourage them to make homemade smoothies and shakes, and to drink oral nutrition supplements because sometimes it is easier to drink your calories than eat them when your appetite is low.
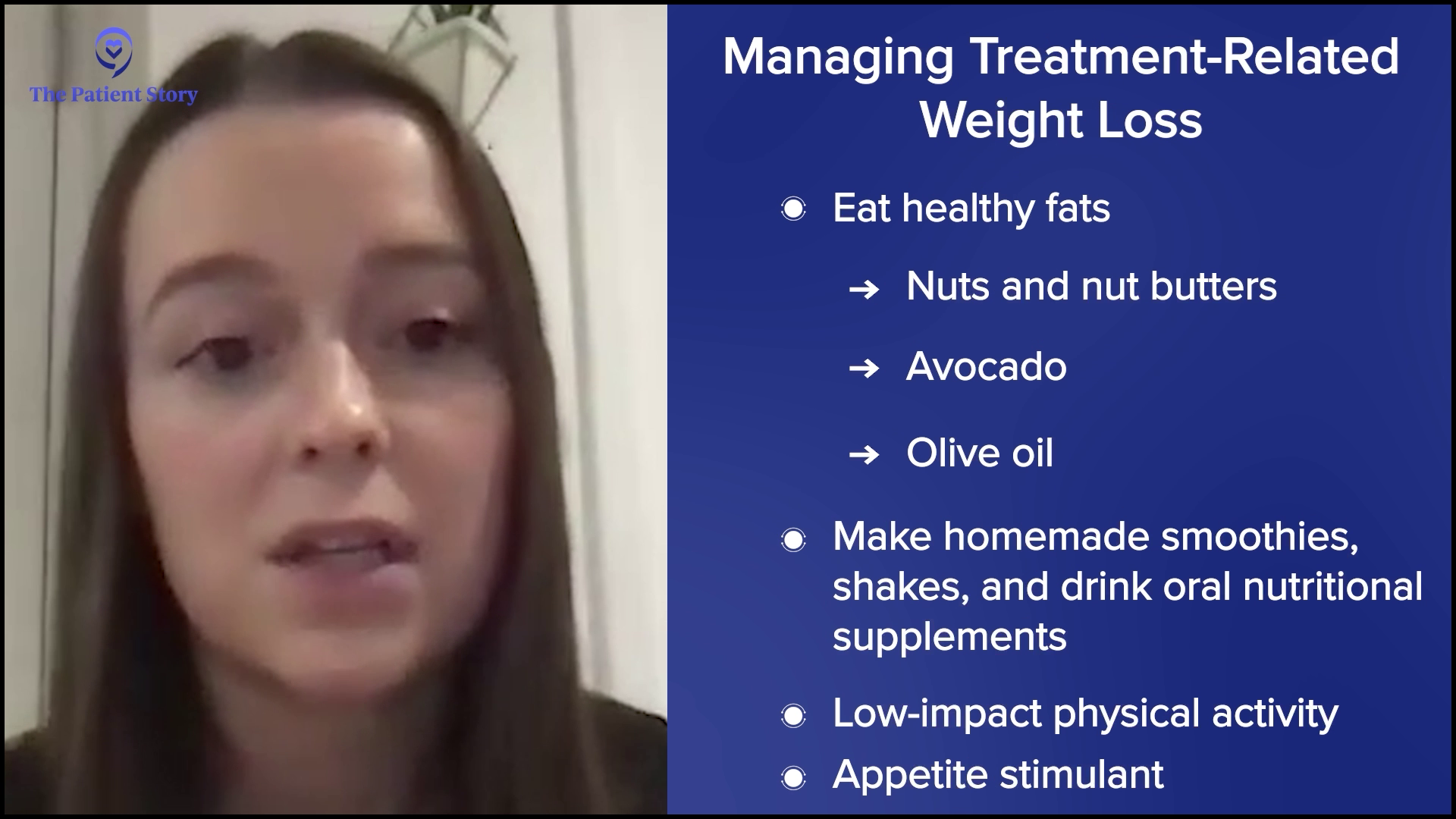
Low-impact physical activity as tolerated can also help to increase appetite and maintain muscle mass. For patients who are struggling to eat and whose appetite has been consistently low, it could be worth asking the doctor if starting an appetite stimulant is appropriate.

On the other hand, I also see patients experience weight gain while in treatment. Oftentimes, this is in part due to steroids or fluid retention. To maintain a healthy weight, we recommend following a Mediterranean-style, plant-based diet, which emphasizes having lots of fruits and vegetables, lean proteins, whole grains, and legumes. We also emphasize watching calorie intake, monitoring portion sizes, and eating slowly and mindfully. It takes 20 minutes for your brain to get the message that your body is getting food before you stop feeling hungry. The slower and more mindfully you eat, the sooner you should realize that you’re full.

I also recommend being physically active as tolerated, specifically to engage in at least 150 minutes of moderate-intensity physical activity per week, which can equate to 30 minutes, five days per week. Moderate-intensity physical activity could be a brisk walk or biking.
Common Skin Conditions Multiple Myeloma Patients Experience
Valarie: I’ve dealt with severe dry skin and hyperpigmentation. What are some of the common skin conditions that multiple myeloma patients experience as a result of treatments?
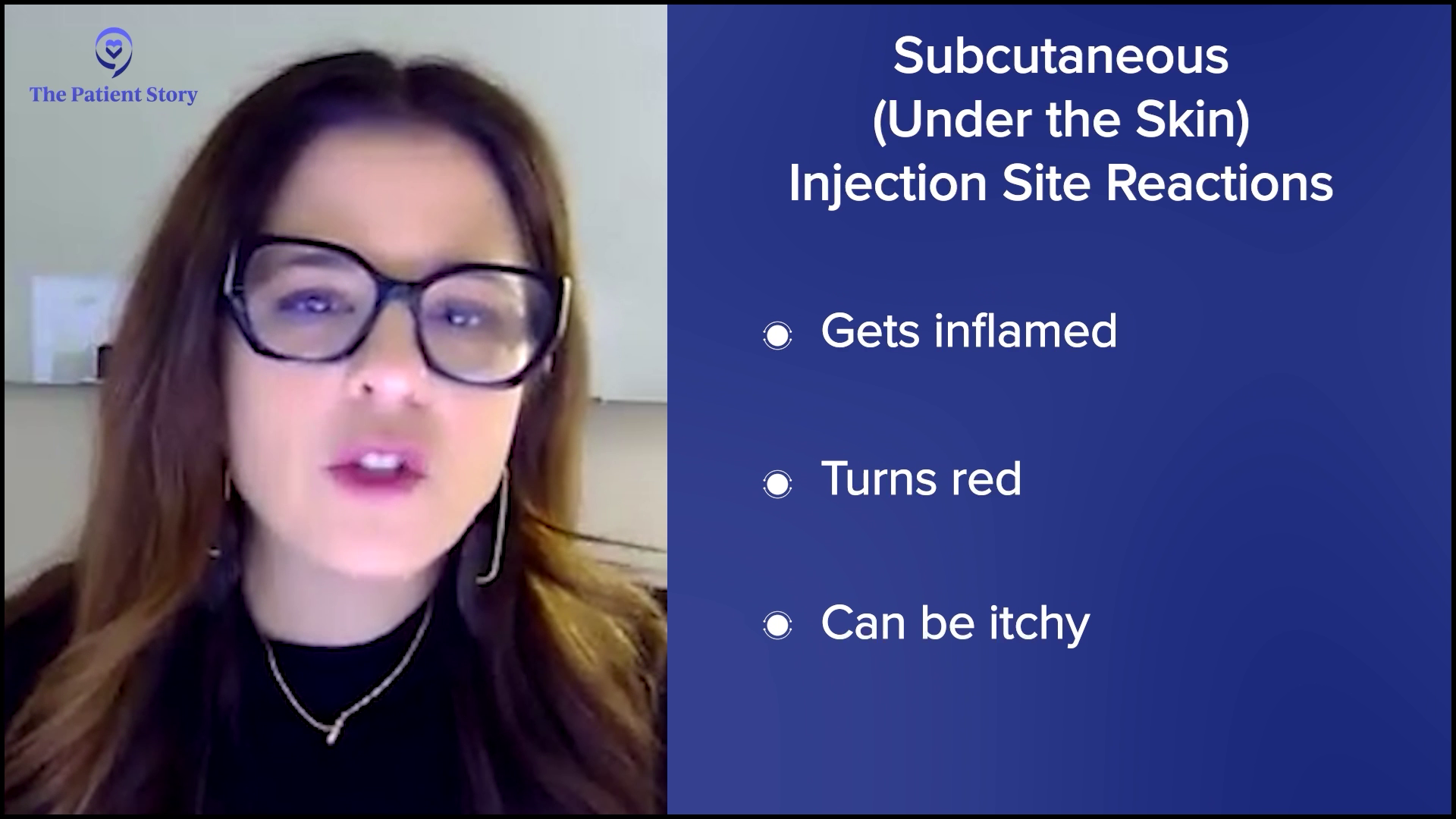
Donna: A lot of multiple myeloma treatments are subcutaneous injections, which means they go right underneath the skin, so we often will see injection site reactions. Around the area where we administered the medication, it gets inflamed, red, and itchy.
Another side effect we see is dry skin. For patients who experience this and if I know a regimen will cause dry skin, I tell patients to use heavy barrier moisturizing creams at the initiation of therapy, especially during long winter months. Our skin dries out fairly quickly with the heat. You want to use heavy barrier creams to help retain the moisture and start at the initiation of therapy.

When we see on-target, off-tumor side effects with talquetamab, for example, the skin on the palms of the hands and the soles of the feet start to peel. These side effects can be self-limiting and we can manage them well. We use lotions, like ammonia lactate, on the area. We’ll do that twice a day and this typically will resolve in 2 to 3 weeks for patients.
We also see nails that get brittle and peel. Unfortunately, there isn’t something we can give patients to eliminate brittle, peeling nails, but we can suggest nail polish hardener lacquers to make the nails stronger so they’re less likely to break. We recommend cuticle oil around the cuticle bed. We look for signs and symptoms of infection because we don’t want to have any nail infections.
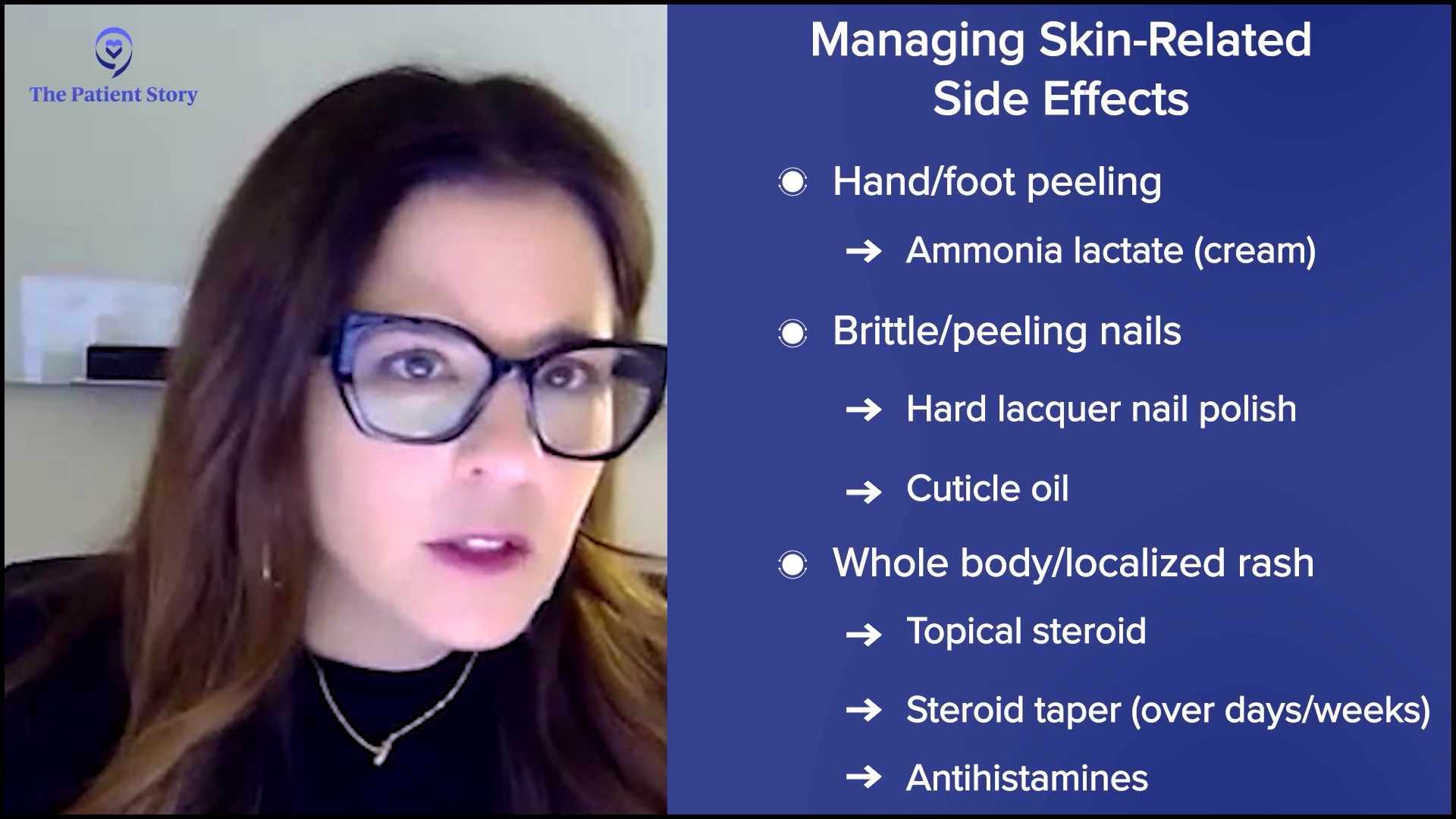
Another side effect that patients can experience is a whole-body rash or a localized rash. Depending on the size of the rash, we can manage it quite well with topical steroids or lotions. If a rash is more generalized, we’ll add a steroid taper. A course of steroids over several days will tamper down the whole-body rash, which will typically be resolved in several days.
A rash can be itchy or a patient could feel itchy in general, so we can use antihistamines for several days to help with any itchiness. If the itchiness is drug-induced and depending on the severity of the skin reaction, I’m going to hold off on the medication until these symptoms resolve before resuming therapy. If the rash is severe enough, I would consider either a dose reduction or a look at how frequently treatment is administered.

Valarie: Do you often refer to a dermatologist or treat them within your cancer center?
Donna: Early on, when we look at these new treatment modalities, we weren’t typically seeing these side effects. We work very closely with our dermatology colleagues, but we can manage these side effects quite well. I will definitely refer to our colleagues in dermatology, but for the most part, we can manage these symptoms quite well within our own practice.
Bispecific Antibodies for Relapsed/Refractory Multiple Myeloma
Valarie: Bispecific antibodies are emerging as a promising treatment option for relapsed/refractory myeloma. Donna, can you explain how these antibodies work? Have you seen an increase in this approach with patients?
Donna: This is a new and very exciting treatment modality. We had several drug approvals within the past few years with this new class of drugs. It’s similar to daratumumab where it will bind to a receptor on the myeloma cell. One arm of the bispecific antibody will grab the myeloma cell and the other arm will grab the receptor of a T cell.
Our T cells are little soldiers of our immune system. T cells will do surveillance and get rid of anything that looks bad in our system, so that includes infections and cancer cells. What a bispecific antibody does is grab onto the myeloma cell, grab onto the T cell, and bring that T cell close to the myeloma cell so that the T cell can recognize the myeloma cell and kill it
In essence, it mimics the mechanism of action of CAR T-cell therapy, but the benefit of a bispecific antibody is it’s off the shelf, so there’s no downtime unlike waiting for manufacturing CAR T cells. If I need to start a patient tomorrow, we can initiate therapy quickly. We’re harvesting the patient’s immune system to attack the myeloma cells. This is an exciting new treatment approach.
Common Side Effects Associated with Newer, Targeted Therapies
Valarie: As a patient, I’m very excited to hear about bispecific antibodies. What are some of the common side effects associated with these newer targeted therapies?
Donna: We’re activating that immune system, so the immune system gets revved up and what happens is it releases cytokines. Cytokines are little immune substances that can cause havoc. It can affect everybody’s system. Typically, when a patient gets a bispecific antibody, they’ll have a fever. This can progress to low blood pressure or difficulty with breathing, but these are so well-managed now.
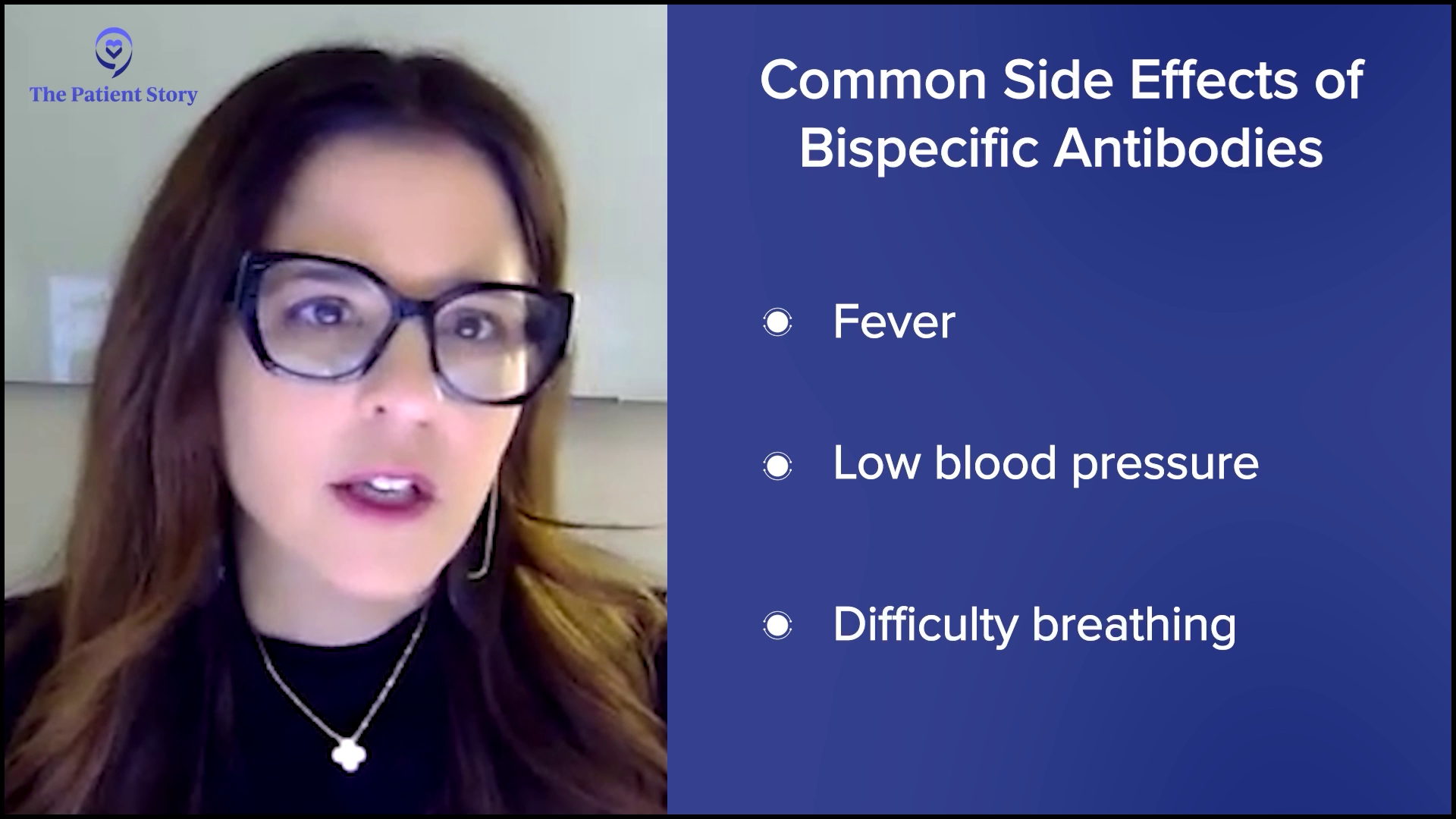
The patient will typically complain of a fever, almost like when we get our flu shots where we feel a little achy and get a low-grade fever. As a provider, I know this patient is probably having cytokine release syndrome (CRS). The immune system is getting revved up, so I will tap the brakes. We have treatments that will simmer down the immune system and within 24 to 48 hours, the patient’s symptoms will resolve and allow us to continue treatment.
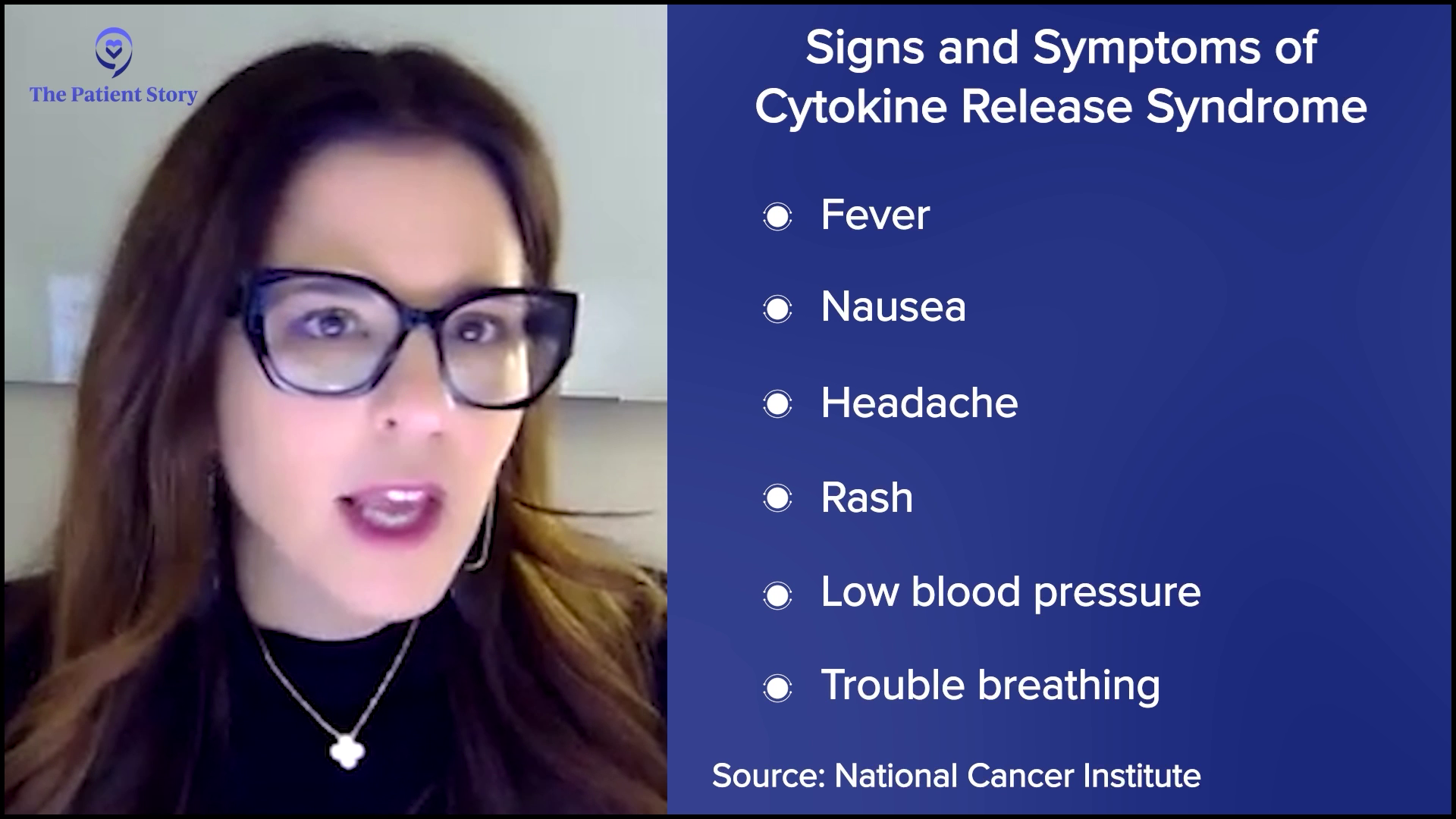
We try to mitigate this side effect by giving premedication, so we’ll give acetaminophen, diphenhydramine, and some steroids, but the majority of patients are going to experience CRS. Typically, we manage this inpatient, but more and more institutions are learning to manage these side effects as outpatients. We monitor patients very closely by checking their vital signs and intervening at the first sign of a fever. If a patient has a drop in their blood pressure or difficulty with breathing, we intervene very quickly.
The majority of patients will have cytokine release syndrome and to a much, much lesser extent, we see neurotoxicity. If patients have cytokine release syndrome, typically we see neurotoxicity immediately after. A patient might present with some confusion and maybe a little disoriented. They can name the hospital and their name, but instead of saying that it’s winter, they’ll tell you it’s spring.
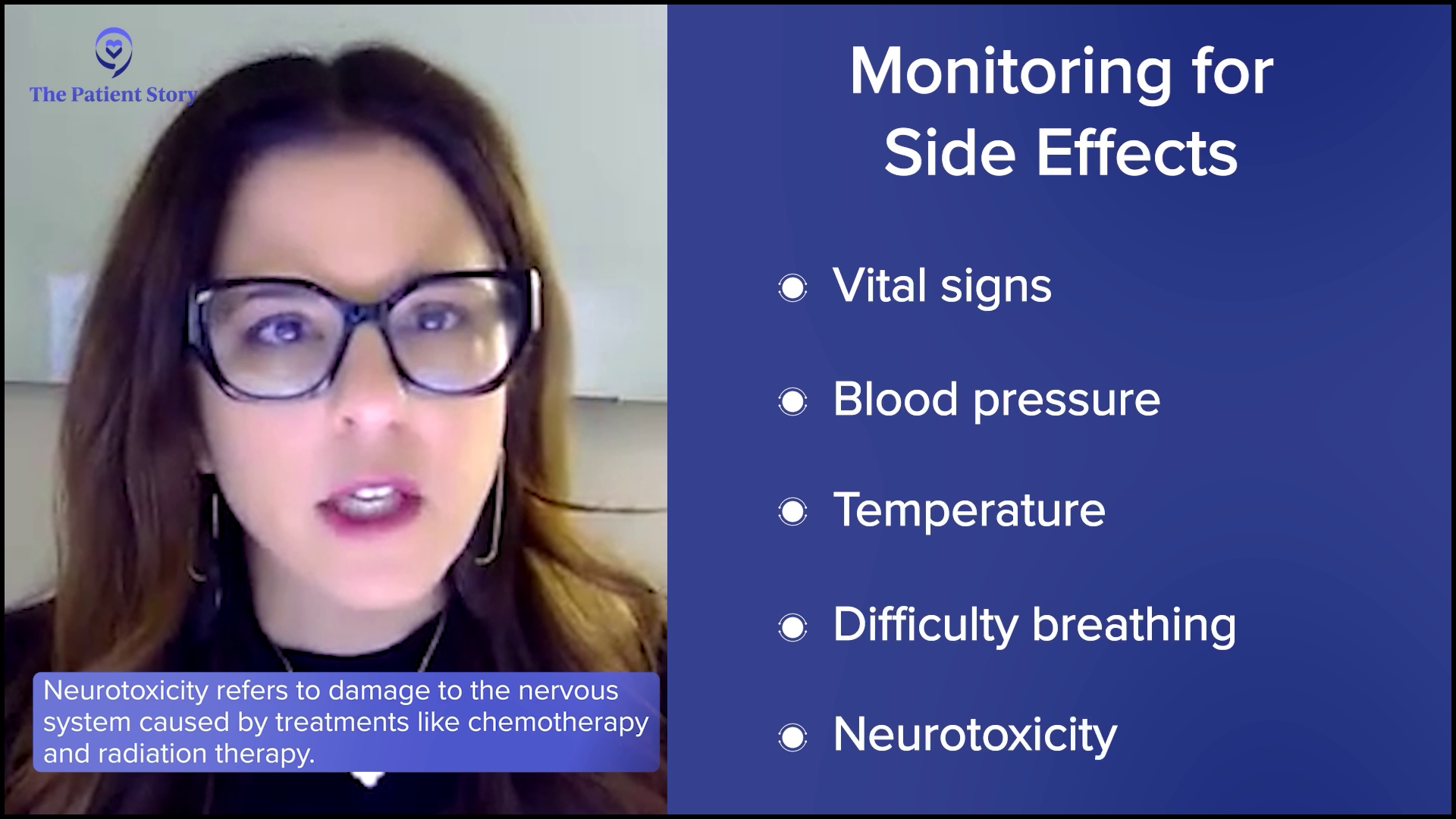
Also, we see patients with a change in their handwriting and this can be quite drastic. Before starting these therapies, we obtain a handwriting sample and monitor the handwriting sample throughout treatment. We’ll see a change from one 12-hour shift to the next where a patient will write a beautiful sentence and then a few hours later, will scribble across the paper. This patient is experiencing a neuro event. This can be scary, but this is reversible. We manage this very well. This is self-limiting, so it won’t reappear.
Care partners are very important when we give these types of treatment because if the patient is at home, they might not understand that they’re confused. It’s very important to have a care partner to monitor the patient to see if there’s any alteration in their mental status. We manage this quite well with steroids.
Specific Strategies for Managing Cytokine Release Syndrome and Neurological Side Effects
Valarie: Are there specific strategies for managing cytokine release syndrome and neurological side effects?
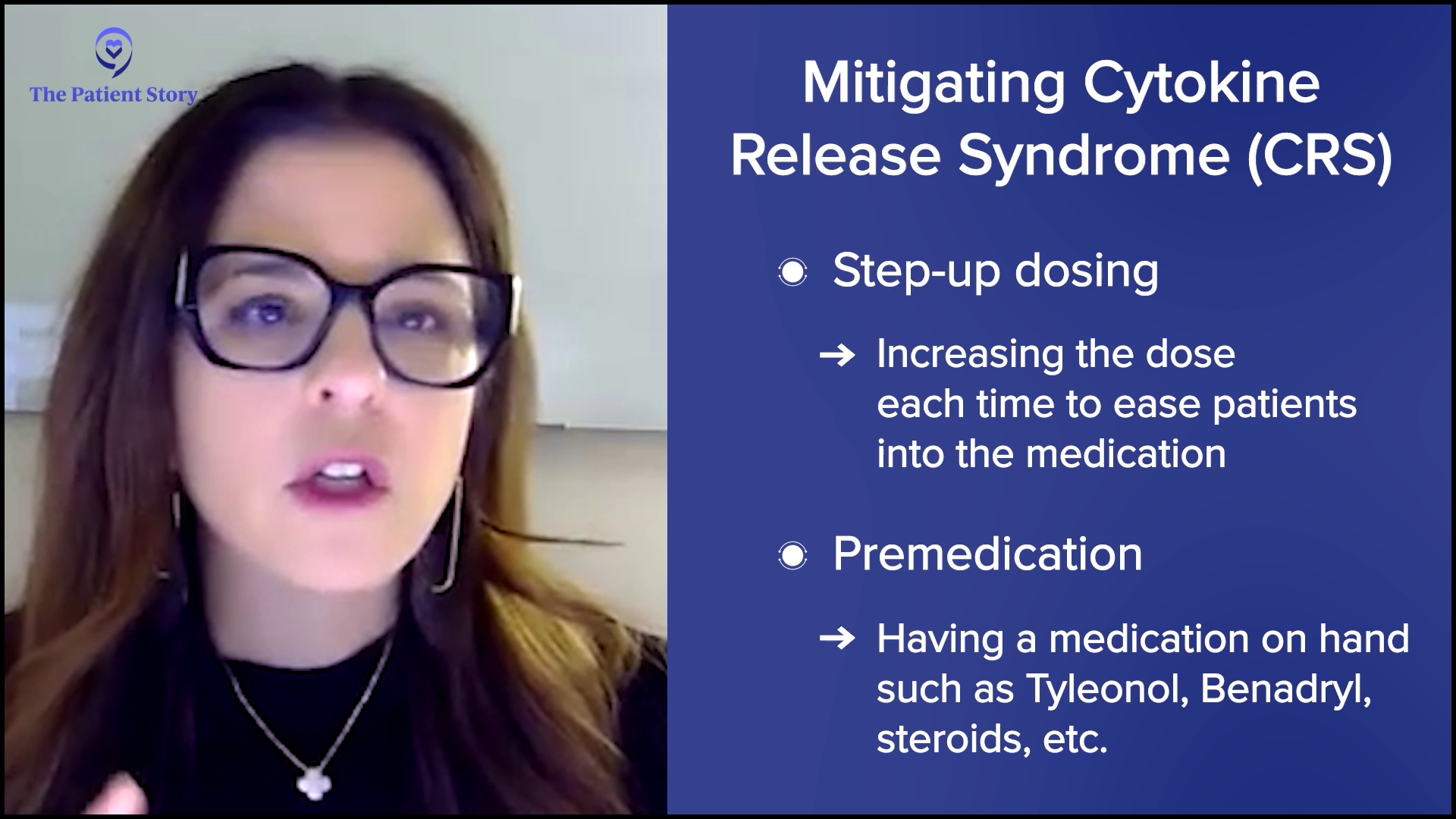
Donna: To mitigate some of these potential side effects, like cytokine release and neurotoxicity, we do two things. First, we’re going to do a step-up dosing approach. We’re going to give a small dose for that first dose, a slightly higher dose for that second dose, and then the full dose. We ease the patient into that medication.
The second thing we do is to have premedication on board to mitigate the severity. Most patients are going to have cytokine release syndrome, but it’s typically mild like a fever, which we can manage quite well. Neurotoxicity happens in a very low percentage. Less than 7% of patients will have this neurological event. Step-up dosing and medications can help, but that’s something we will manage when the symptoms arise.
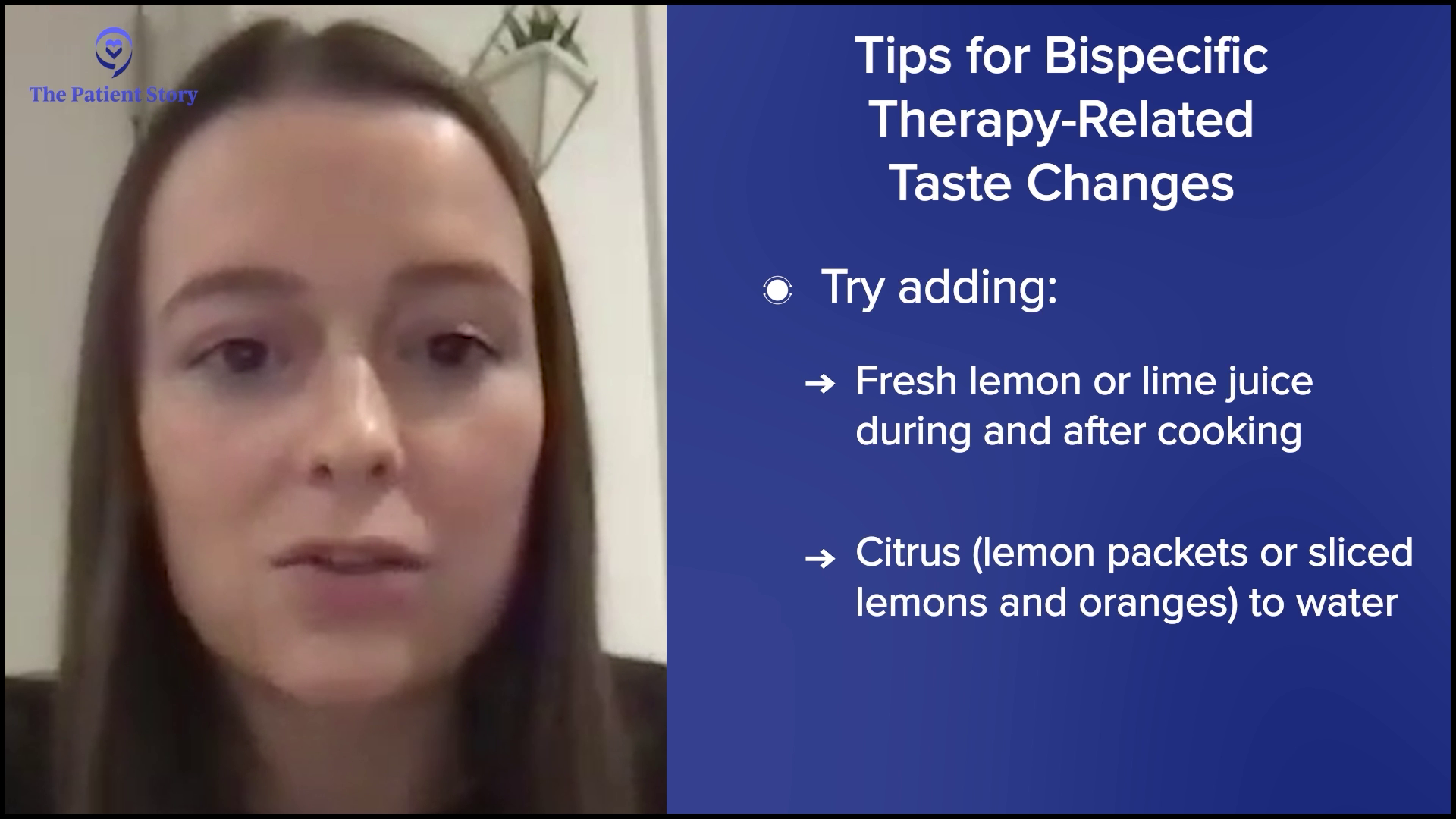
Dietary Changes to Help Manage Loss of Taste
Valarie: Abbey, we talked about diets and how having healthy snacks can help manage the side effects. For patients experiencing loss of taste, how can they change their diet to help manage that particular side effect?
Abbey: Taste change is one of the most common side effects that I talk about and it’s definitely one of the most difficult to manage. There’s no one-size-fits-all approach, not one miracle food that everyone enjoys, and no medication that provides total relief. It’s tough for patients to find foods they enjoy, let alone tolerate.
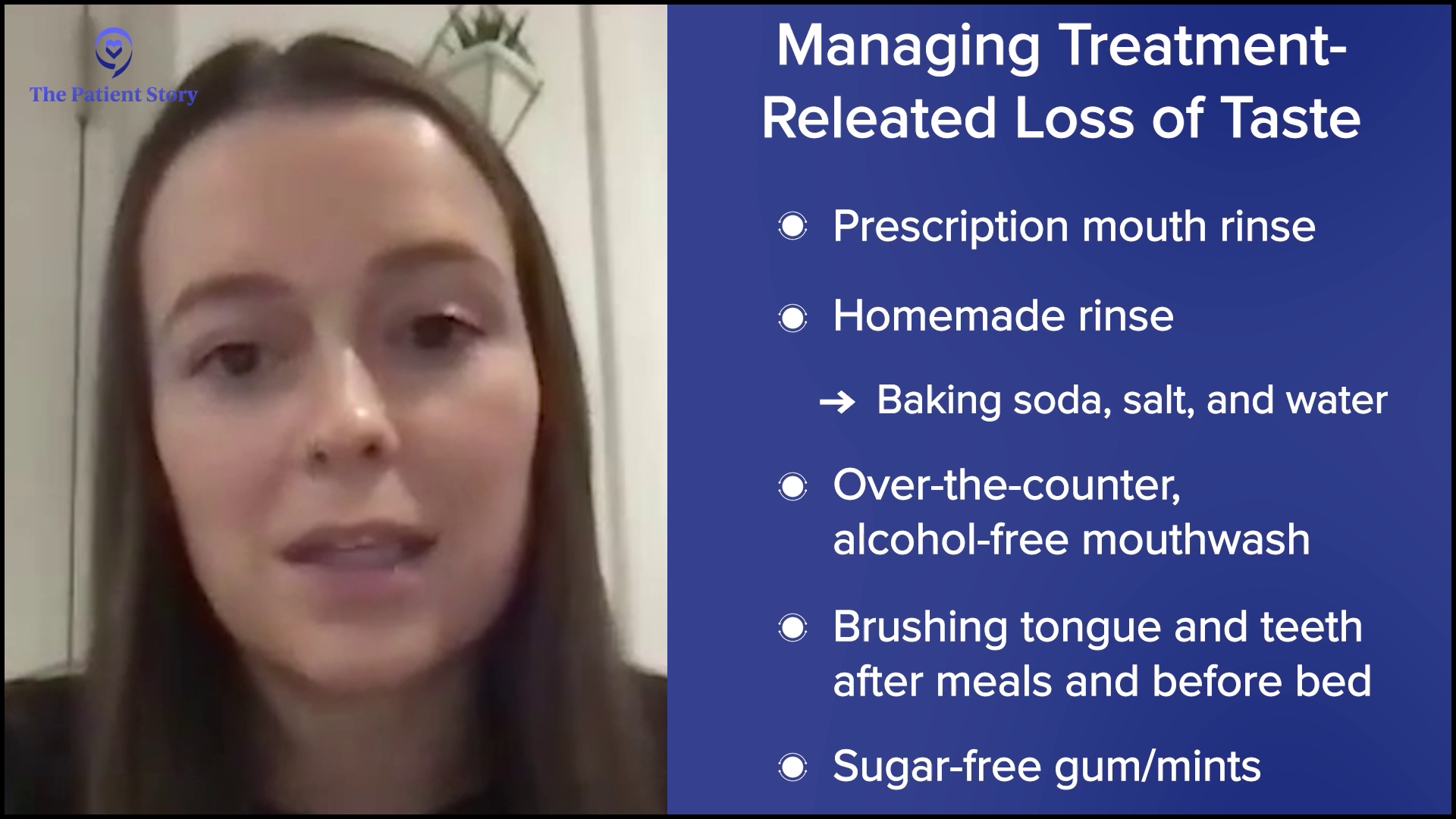
Something I emphasize to everyone, regardless of their experience, is good oral hygiene. Patients are often prescribed a mouth rinse, but if this doesn’t help, I recommend trying a homemade rinse made with baking soda, salt, and water, or an over-the-counter, alcohol-free mouthwash. Brushing the tongue and teeth after meals and before bed is also important to keep the mouth clean. It also doesn’t hurt to try sugar-free gums or mints to see if that improves any unpleasant taste in the mouth.

When patients describe taste changes, I hear a wide range of statements, including everything tastes too bitter, too sweet, too metallic, has no taste, tastes like cardboard, or everything tastes bad. If food tastes too bitter or too sour, I recommend adding something sweet to food, like honey or fruit. Or, if food tastes too sweet, try adding an acid, such as vinegar, lemon, or other tart, tangy, or acidic flavors. If everything tastes metallic, I recommend using nonmetal utensils and cookware, such as plastic, glass, or ceramic. Try fresh or frozen foods over canned and serving meat cold or at room temperature.

For bispecific therapies, the most common statement is everything tastes bad or has no taste. For this, I emphasize the importance of experimenting with different flavors, textures, temperatures, herbs, spices, seasonings, and sauces because you never know what might work for you. I often hear that adding acids like lemon, lime, vinegar, and tomato can make foods more enjoyable. I’ll often recommend adding fresh lemon or lime juice during and after cooking, and adding citrus to water, such as lemon packets or sliced lemons and oranges, if plain water tastes unpleasant.
Taste is the combination of not only the taste but also the smell and touch of food. If you can’t get any pleasure from taste, don’t underestimate the power of texture and smell. Soft, moist foods like oatmeal, soups, and mashed potatoes are usually more tolerable since they’re easier to chew and swallow, which means they spend less time in your mouth.
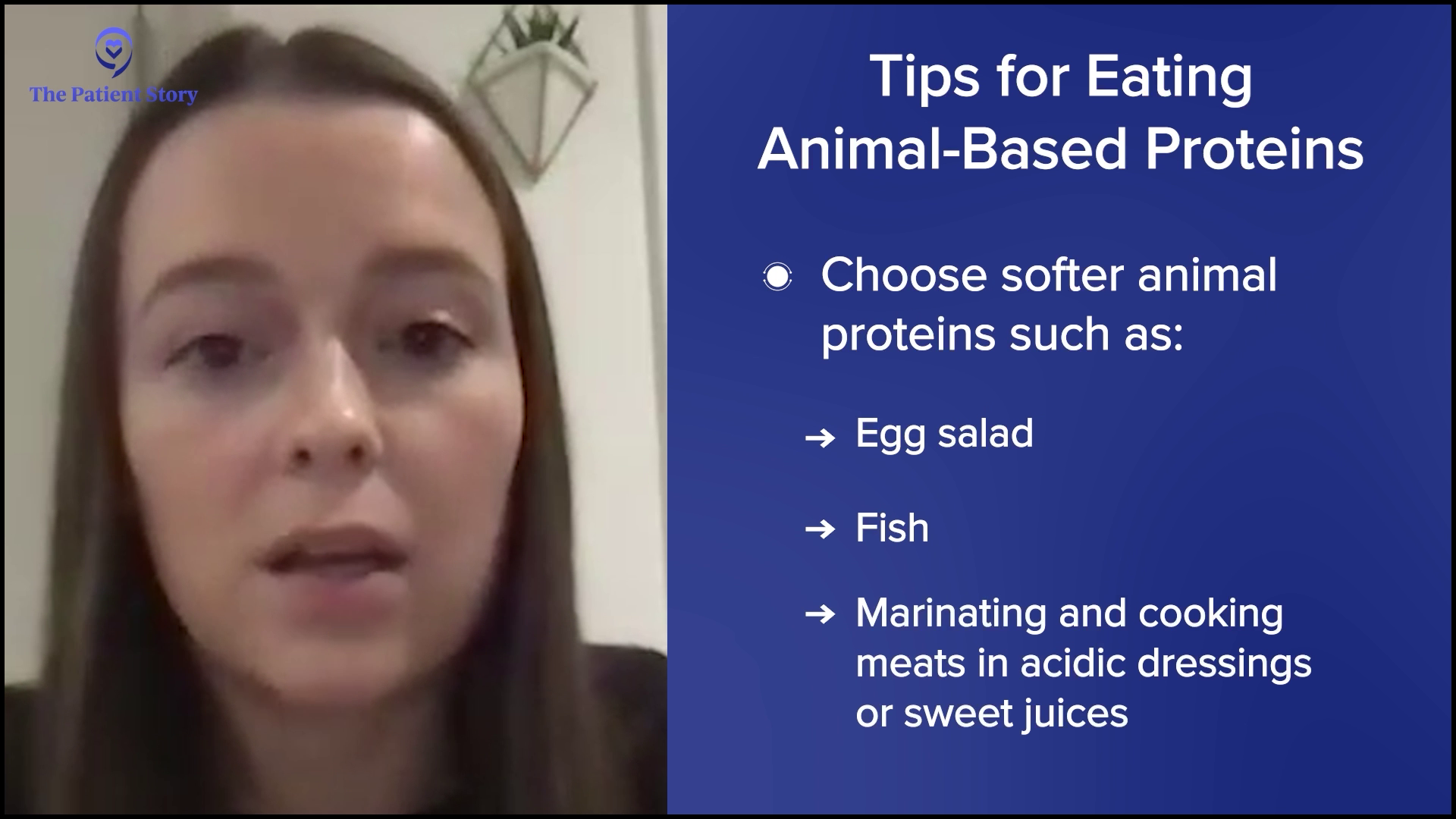
Smoothies and oral nutrition supplements are my go-to recommendations because they’re quick and easy ways to get in calories. Protein and smoothies allow a patient to experiment. Fruit is one of those foods that are often tolerable, so I recommend blending different fruits into smoothies to see if that makes them easier to get down. Animal proteins tend to be tough for patients to tolerate, so I typically recommend choosing softer animal proteins, like egg salad or fish, or marinating and cooking meats in acidic dressings or sweet juices.
Many patients report that they maintain their sense of smell despite losing their taste. I’ve had a patient say that certain foods, like cucumbers, cantaloupe, and coffee smelled good, which helped them taste good too, so it’s definitely worth experimenting in this way.
An important point that patients should take away when it comes to taste changes is that everyone is different. A recommendation that works for one person may not work for the other, so it’s important to keep trying and retrying foods because you never know what may end up working for you. Even though everyone is different, if patients are experiencing these side effects, they should know that they’re common and they’re not alone.
Coping with the Emotional Challenges of Relapse
Valarie: Let’s talk about the emotional side, such as anxiety and depression. Donna, how can patients cope with these types of challenges?
Donna: In the relapsed/refractory setting, every relapse causes a lot of anxiety and fear. When starting a new treatment, there’s a lot of fear, which can then increase anxiety and can lead to depression. Having a good support network is important for patients. We’re very fortunate in my institution to have a wonderful social work team that can help patients. We have support groups. Support groups work for some patients but not for others, so have care partners on your team to help patients through these challenging times. Each relapse becomes challenging for patients. The good news is that we do have great therapies for patients to provide support for patients to get through their therapies.
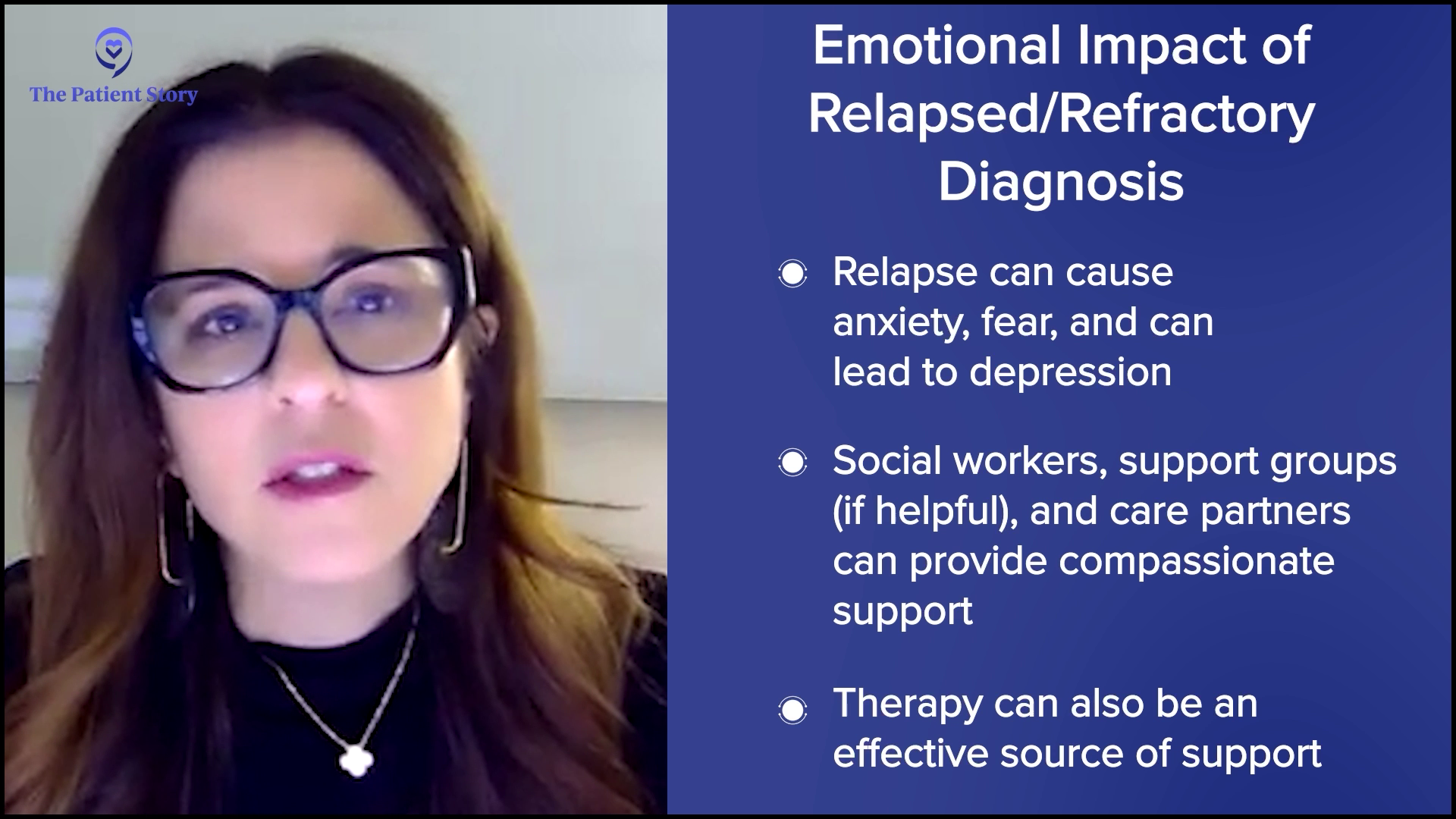
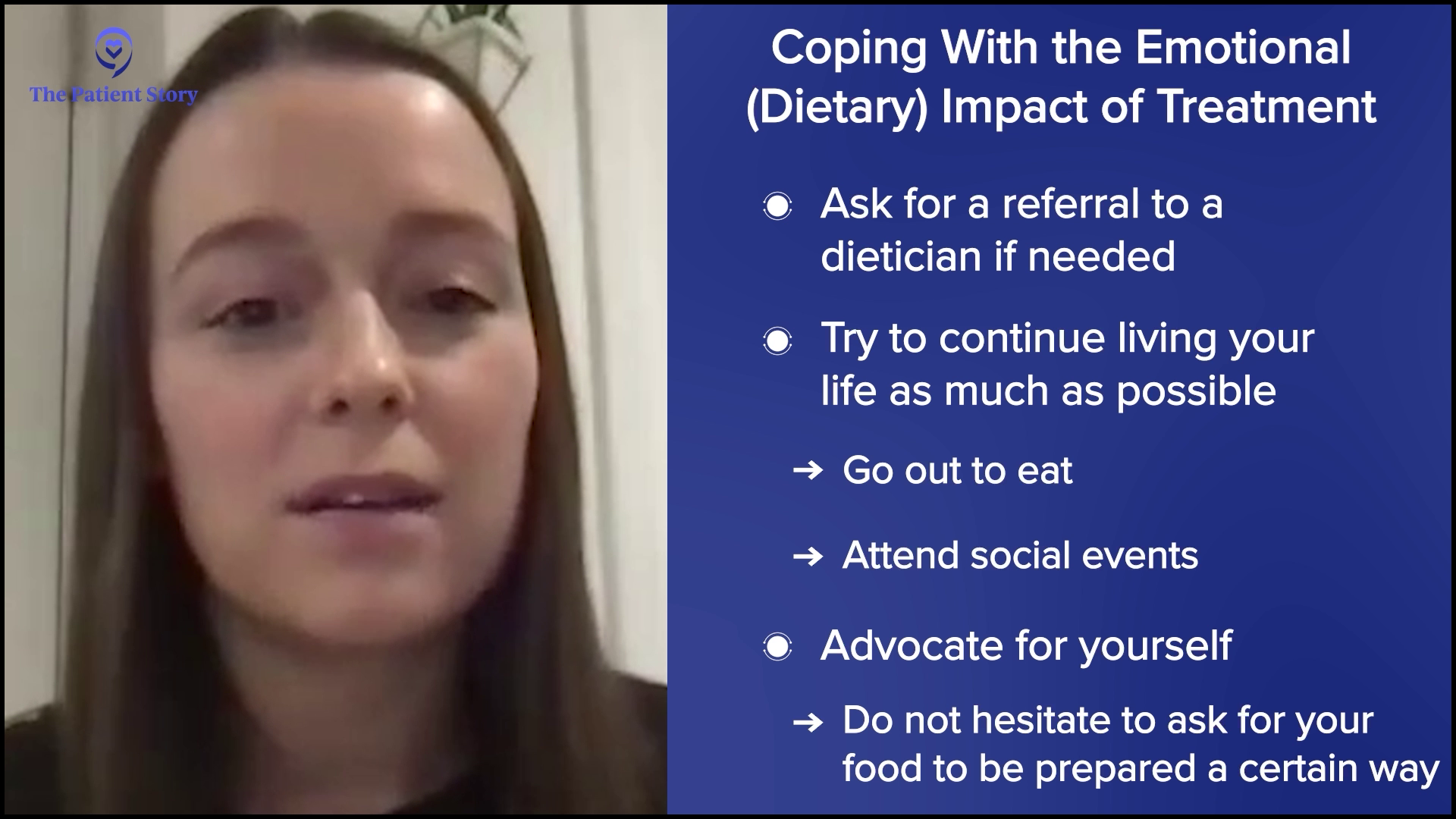
Abbey: From a nutrition standpoint, a patient experiencing side effects from treatment that affect their ability to eat can significantly impact a patient’s quality of life. It can cause patients to feel isolated because it’s hard for anyone to fully understand what they’re going through. On top of that, they might feel pressure from family and friends to eat more even when they don’t feel well and I’ve seen that cause resentment. Eating is such a social and cultural activity, and many patients feel like they don’t have a place at the table to help cope with these challenges.
I encourage patients to ask for a referral to a dietitian. Our job is to provide tips and tricks to help patients eat despite these side effects. I also encourage them to try to continue living their lives as much as possible, to go out to eat, and to attend social events when they have the energy and when it is safe for them to do so. When people are experiencing side effects and they go out to eat, they feel embarrassed or afraid to advocate for themselves. I encourage them not to hesitate to ask for their food to be prepared a certain way if it makes it easier for them to eat. If they want to bring their own food when they go out, that’s completely okay. I’m sure their friends and family would prefer to see them enjoying their meal and feeling supported, rather than feeling embarrassed or ashamed.
Valarie: As a patient and as somebody who’s been on that side of it, you have to look out for yourself. If that means taking something to a restaurant to spend time with your loved ones and be able to enjoy a meal, then do it.
Support groups are not for everyone, but there’s also one-to-one support available. You can talk with a myeloma coach or a mentor angel in various programs. Know that you’re not alone as you’re dealing with these side effects. Others are going through them as well and you always have someone to support you.

Final Takeaways
Valarie: Thank you, Donna and Abbey, for taking the time to speak with me and The Patient Story audience. Do you have any final remarks?
Donna: We have some great therapies we can offer patients. The important thing is getting patients through that therapy. There are side effects, but we’re going to help manage those so that patients can have the best possible outcomes.
Abbey: I encourage patients who are experiencing any side effects to speak up, advocate for themselves, and let their teams know. The sooner their team is aware, the sooner they can provide supportive care or treatment to help manage those side effects. If the side effects they experience make it difficult to eat, don’t hesitate to ask for a referral to a dietitian if their team has not referred them to one already.
Valarie: Yes, I agree with you wholeheartedly. Speak up and don’t suffer in silence. There’s no need for that.

Conclusion
Tiffany: Thank you again, Donna, Abbey, and our patient moderator and advocate Valarie, for taking the time to discuss mitigating side effects, especially to Valarie for sharing her myeloma experience. I am grateful that she shared her story with us. It takes a village and I know that your story, Valarie, will resonate.
It is important to be empowered so that you and your caregivers can make informed decisions about your care. That includes being educated on the latest on the side effects, mitigating those side effects, and getting the support that you need.
Part 2: Skin-Related Side Effects
Relapsed/Refractory Multiple Myeloma Patient Stories
Dr. Yvonne D., Relapsed/Refractory Multiple Myeloma
Symptoms: Severe hip pain, trouble walking due to a broken pelvis, extreme fatigue, bone pains
Treatments: Chemotherapy, stem cell transplant, radiation therapy, surgeries, CAR T-cell therapy
Michele J., Relapsed/Refractory Multiple Myeloma
Symptoms: Fatigue, anemia, persistent lower back pain, sharp leg pain during movement
Treatments: Surgery, chemotherapy, stem cell transplant
Theresa T., Relapsed/Refractory Multiple Myeloma, IgG kappa Light Chain
Symptom: Extreme pain in right hip
Treatments: Chemotherapy, CAR T-cell therapy, stem cell transplant, radiation
Laura E., Multiple Myeloma, IgG kappa
Symptom: Increasing back pain
Treatments: Chemotherapy, stem cell transplant, bispecific antibodies
Donna K., Refractory Multiple Myeloma
Symptom: None; found through blood tests
Treatments: Total Therapy Four, carfilzomib + pomalidomide, daratumumab + lenalidomide, CAR T-cell therapy, selinexor-carfilzomib