Building a CLL Game Plan
Strategies for Treatment, Trials, and Team Building
Chronic lymphocytic leukemia (CLL) care is getting more personalized than ever.
CLL patient advocate Jeff Folloder and expert hematologist-oncologist Dr. Nicole Lamanna (Columbia University Irving Medical Center) explain how today’s innovative targeted therapies, time-limited treatment options, and emerging clinical trials can help patients craft a care strategy that truly fits their needs. The conversation dives into how to assemble a strong, collaborative medical team, at both local hospitals and major centers, so patients and families feel empowered at every step.


Thank you again to Blood Cancer United and the CLL Society for their partnerships.

Thank you again to AbbVie for its support of our independent patient education program. The Patient Story retains full editorial control over all content.
- Introduction
- Newest Treatments for CLL
- Continuous Therapy vs. Treatment for a Set Time
- Treatment Options: Newly Diagnosed vs. When CLL Comes Back
- Will CLL Treatment Affect My Fertility?
- Building the Best Medical Team
- How Can Patients Facilitate Communication Between Their Community Doctor & A CLL Specialist?
- Understanding the Roles of Your Team and Patient Advocacy Groups
- Clinical Trial Options for CLL
- Addressing Concerns About Clinical Trials
- Exciting Areas of CLL Research
- Quality of Life and Treatment Decisions
- How Do I Talk to My Doctor About Symptoms and Side Effects?
- Why Isn’t My Doctor Starting Treatment Right Away?
- Conclusion
Edited by: Katrina Villareal
Introduction
Jeff Folloder: Hello and welcome to “Building a CLL Game Plan: Strategies for Treatment, Trials, and Team Building.” My name is Jeff Folloder. I’m a long-time passionate patient advocate. I’ve been on the chronic lymphocytic leukemia (CLL) journey for over 15 years. Because of all the wonderful things that have happened over those years, I am living an excellent life, and it’s my mission to make sure that everyone with CLL has the opportunity to live a great life.
In this discussion, we’ll talk about the latest treatment options for CLL, how to build the right medical team, how to access clinical trials even in community settings, and most importantly, how to make shared decisions that keep quality of life at the center.
This discussion is brought to you by The Patient Story, which is on a mission to humanize cancer. We do that through educational programs like this one, but also hundreds of videos of patients telling their personal stories to help others. You can find those stories at ThePatientStory.com.

Tremendous thanks to our sponsor, AbbVie. Without them, we can’t do programs like this, so their support is important, helping us host these educational programs for free. We want to note that The Patient Story does maintain full editorial control.
We hope that you find this helpful. Remember, this is not a substitute for medical advice. We hope it will inspire better discussions with your medical team.
We want to hear from you, so we can make these discussions even better. What did you enjoy? How can we improve? Please take the time to let us know. It’s how we get better.
It’s my pleasure to introduce my friend, Dr. Nicole Lamanna. She is the Judy Horrigan Professor of Medicine for the Leukemia Service and the director of the Chronic Lymphocytic Leukemia Program. She’s at the NewYork-Presbyterian/Columbia University Irving Medical Center. I have a very direct question for you, Dr. Lamanna. What drives you to show up to work every day?

Dr. Nicole Lamanna: It’s a pleasure to be here. I’ve been doing this for a long time, too. As he’s been an advocate for 15 years or so, I’ve been doing this for over 20 years. And I love what I do. I’m also a very staunch patient advocate and he knows this very well, which is why I do these kinds of programs. I love taking care of patients with this disease and trying to figure out therapies that will improve the quality of their lives and the efficacy of the treatments to deal with this disease.
Hopefully, at some point, we’ll have curative therapies. I think that we’re getting close with what we’re doing with all the great treatments we have now. It’s been a big change for somebody like me who started in the era of chemoimmunotherapy and to see this transition over 20 years is phenomenal.
That’s what drives me to come to work every day. You build long-lasting bonds with your patients. This is, in part, why I love dealing with this disease, because I get to make wonderful relationships with my patients, so it’s a lot of fun.
Newest Treatments for CLL
Jeff: You mentioned the old-school treatment programs, like chemoimmunotherapy. I’d like to think that for most of us, that’s pretty much in the rear-view mirror. What new treatments are available for CLL today, and how are they different from older treatments that patients used to get?
Dr. Lamanna: Some of you may have even received some of those older treatments, right? Twenty years ago, we used chemoimmunotherapy, which included drugs like fludarabine (Fludara), bendamustine (Treanda, Bendeka), cyclophosphamide (Cytoxan), all intravenous treatments.
Don’t get me wrong — they were great treatments. In fact, some of you might have had them and have done well on them, but they had a lot of side effects, so they were harder to give to older individuals. Remember, the median age for this disease is the 70s, although we have lots of younger people, too. But sometimes, chemotherapy can be rougher if you have lots of medical problems and are older, so it became prohibitive for many older folks.
As we started to understand the biology of this disease, how these abnormal B cells grow and live, and what supports them, understanding the pathway of their development led to a lot of targets. Over the last 10 to 12 years, we’ve had a slew of targeted therapies, so they’re not that new anymore.
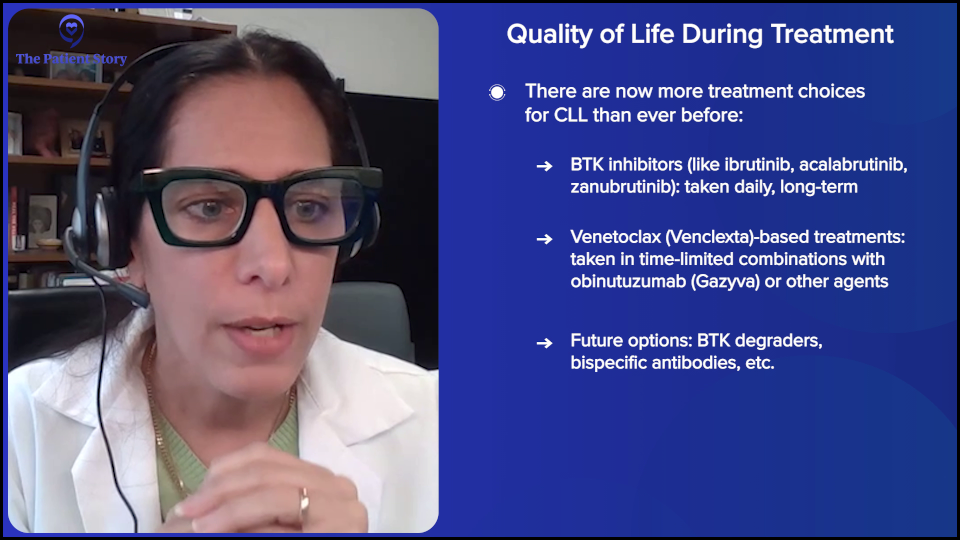
We have two major classes. One is called Bruton tyrosine kinase (BTK) inhibitors, which many might be familiar with. They’re oral agents, and we now have three FDA-approved BTK inhibitors — ibrutinib (Imbruvica), acalabrutinib (Calquence), and zanubrutinib (Brukinsa) — which have dramatically transformed the landscape of treating this disease.
They’re much more tolerable therapies with great efficacy. In many randomized trials against the older forms of chemotherapy, they showed an improvement. In a way, what Jeff mentioned about moving away from chemotherapy is due to both toxicity as well as proven improvement in efficacy. We’ve moved away and pushed chemoimmunotherapy down the road for these targeted therapies.
The other big class is what they call BCL-2 inhibitors, which are agents that help with the killing and allow the CLL cells to die. There’s one that’s FDA-approved, which many of you might be familiar with. It’s an oral agent called venetoclax (Venclexta) and is often given in combination with other therapies, which also dramatically changed the way we treat this disease.
Now there are newer agents, Jeff. I don’t know if you want me to speak about all the exciting stuff in clinical trials now, but we can get to that later. But these are the ones that have removed chemoimmunotherapy and have moved patients into the newer era of targeted agents with improvement in disease control and better side effects.
Jeff: That’s fantastic to hear.
Continuous Therapy vs. Treatment for a Set Time
Jeff: I know a lot about BTK inhibitors and venetoclax (Venclexta), but I have also been hearing from our communities that these treatments don’t have to go on forever. It used to be that you had to take them for the rest of your life. What happened? What changed? And how do doctors decide who gets to do it short-term and who gets to do it for the rest of their life?
Dr. Lamanna: When we first started with targeted therapies, BTK inhibitors were given as a daily medication that you would take indefinitely. Unless you were having a side effect to the medicine or it was no longer working, people can be on these for years.
Then, when venetoclax (Venclexta), the BCL-2 inhibitor, became available, we started partnering it with a monoclonal antibody called rituximab (Rituxan), which is an intravenous but more targeted therapy than the older chemos. What we noticed is that people could get very deep remissions quicker than with just the BTK inhibitor that we were giving chronically.
Through clinical trials, it became a time-limited combination that people could take. This was for patients who had prior treatments and was given for two years. We knew it had deep responses that people could get off of treatment and take a break. It’s like what we do with chemotherapy, where people would get six cycles of a regimen and be done, but it was limited more so because of toxicity issues. You can’t continue chemo indefinitely, but you’d get treatment and get off treatment until you needed treatment again, maybe years down the road. Venetoclax (Venclexta) in combination with rituximab (Rituxan) became the first time-limited combination.
When we saw that, we moved it to the frontline with a different monoclonal antibody called obinutuzumab (Gazyva), which is a little bit more potent. Then it became a shorter duration in the frontline setting, meaning people who have never had treatment for their CLL. It was a year of therapy, and there were great responses.
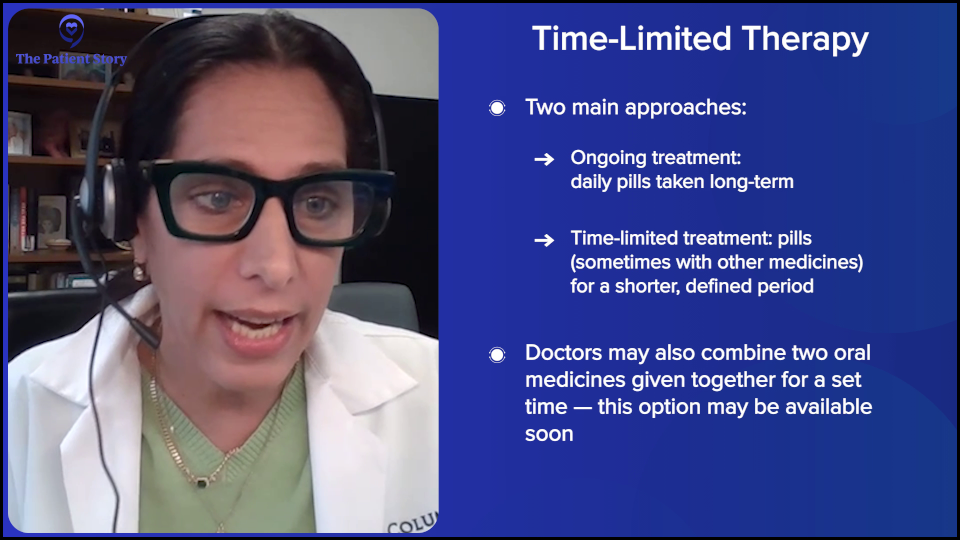
Now we have good options for patients. Some patients, if they want, can take continuous therapy, and some people can take time-limited therapy.
Fast forward to more recent data — so it’s going to get a little bit busier — studies were saying, “Why don’t we combine BTK and BCL-2 and also do a time-limited approach with our two best therapies?” This oral-oral combination is not yet FDA-approved, but it’s in the NCCN Guidelines from a study that was conducted for several years and reported at one of our big meetings in 2024, looking at acalabrutinib (Calquence) and venetoclax (Venclexta). We have an oral-oral combination that will hopefully get approved by the FDA soon, but treatment is also time-limited. How do we choose?
This becomes a discussion between you and your provider. The good news is that both of these are great treatment options. For some patients, it depends on their other medical problems, or particularly if they’re frail. It depends on social circumstances. Do they have good support at home? Can they go back and forth to the medical center frequently?
There are two different treatment paradigms of continuous therapy with an oral drug versus combination therapy. They have different side effects and different monitoring schedules, so we have to take those into account with each patient that we see and have an open dialogue about preferences, side effects, and medical problems, so we can help guide you in making an informed decision.
There are some patients for whom a pill every day is an easy thing to do. Depending on their circumstance or how busy they are, like maybe they can’t go back and forth to have labs done frequently, then the medical center might choose a pill every day.
Some people want to be done with therapy. There’s an advantage to getting a break from treatment. They might say this works for them. They want to get a good response and hopefully have years off of treatment, so they don’t take medicine continuously that could have potentially chronic side effects.
We have a much longer discussion now in the clinic about treatment options because the good news is we now have these treatment options. We didn’t have them before. One of the important things that patients need to know is that they can switch. They can go from one drug to another. Choosing one treatment doesn’t preclude them from changing therapies in the future if they need them, which is important because patients ask what the better choice is. The answer is we don’t have one.
Randomized trials are looking to see if one treatment option is better if we start that first versus the other, but that will take years in follow-up to get data to say if one is truly better to start with before another or not. In general, we haven’t said that that’s the case because they’re both good options, and we haven’t shown that one is necessarily better than the other. It’s more of a discussion between the provider and the patient, taking into account all these other factors, like medical problems, other medicines that the patient might be on, and so on, to make an informed decision about which option might be better at that particular time.
Treatment Options: Newly Diagnosed vs. When CLL Comes Back
Jeff: Let me complicate the matrix a little bit. It sounds like there are an awful lot of options and components that you’re crunching with your patients to get to the treatment route. Is there a difference between someone who’s brand new to the CLL game versus someone who’s relapsed or refractory? Does that add even more complication to this process?
Dr. Lamanna: For someone who might be getting treatment for the first time, the discussion may be a little easier in the sense that they’re a clean slate since they haven’t had any other therapy yet.
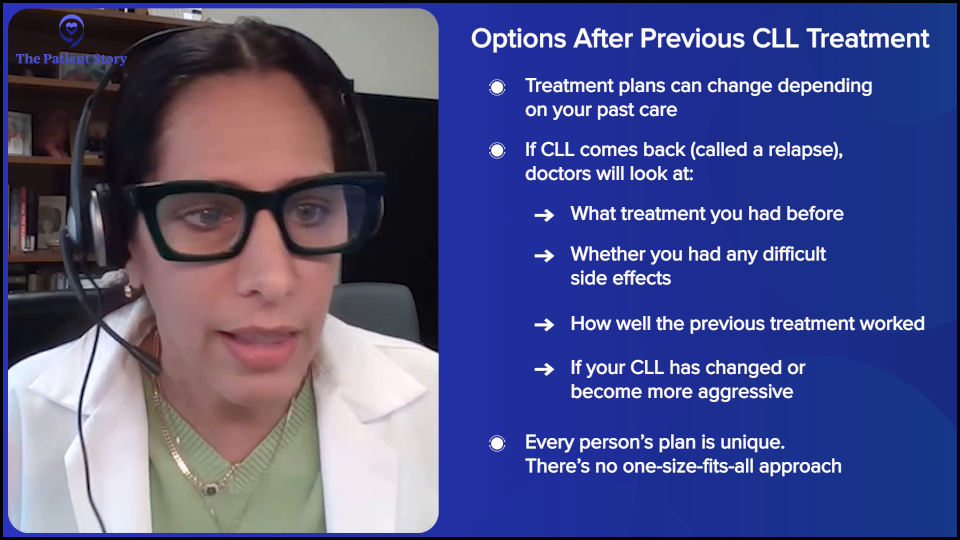
Relapse absolutely is different because partly what you do next will also hinge on what you did prior. Did you have any particular side effects from said treatment that you might have gotten as your frontline treatment? Has your disease changed? Have the genetics of your disease changed? Are there any more aggressive features that might change what we’re thinking about what to treat you with?
In the relapse setting or for somebody who’s had multiple therapies, there’s no doubt that we’re thinking about the kinetics of their disease, the patient themselves, their newer medical problems, side effects from what they got before, and how well their previous treatment did. All of these play a role when we talk about subsequent lines of therapy.
It’s an individualized approach to therapy. I’m not sure we’ll get a one-size-fits-all. I think that would be impossible because even with a good regimen, people can encounter side effects, so you always have to adapt according to the person in front of you. Relapse can be a little bit more complicated because we’re thinking about what that person has gotten before and how well they did.
Will CLL Treatment Affect My Fertility?
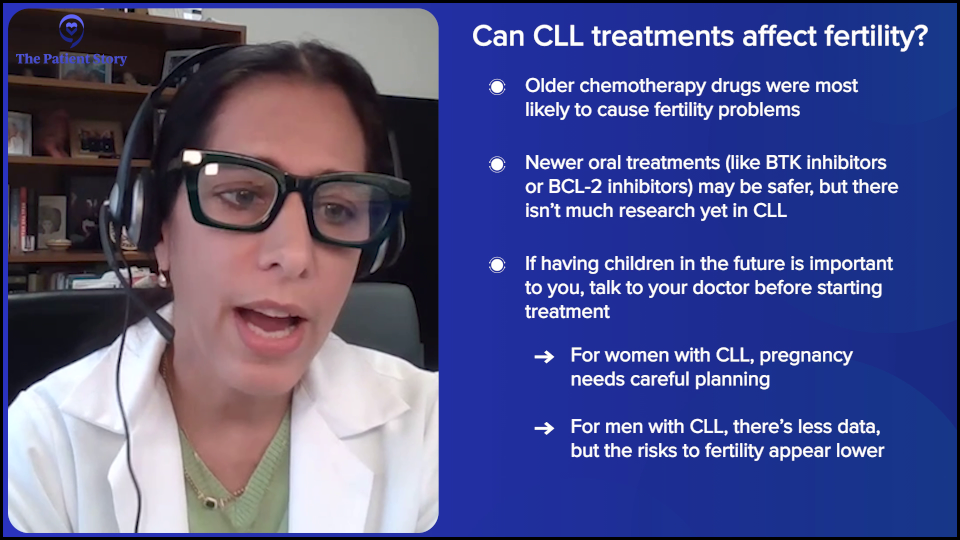
Jeff: Paul has a great question, which I wish would get asked more often because it’s important. “Do different CLL treatments affect fertility for those of childbearing age?”
Dr. Lamanna: There’s no doubt that a lot of the treatments may impact fertility. Chemotherapy was probably the biggest offender when we talked about that, but the TKIs, not so much. There’s a paucity of data in CLL only because the median age is older, but we have tyrosine kinase inhibitors for another chronic leukemia called chronic myeloid leukemia (CML) that have been used, and we’ve shown that, over time, pregnancy is safe.
Now it does depend on the drugs that you’re getting, so we do talk about that. People of childbearing age with CLL who are on therapy need to talk to their provider. Obviously, our ideal preference would be not to be in therapy if they’re pregnant. If the childbearing person who has the CLL is the woman, it would ideally be nice not to be on therapy while they’re pregnant. If it’s a male CLL patient, I don’t think we have data. There’s probably insufficient data to say if it impacts sperm and their ability to impregnate a non-CLL person.
When I think about counseling some of my patients, I have not had that as a barrier for them to impregnate as a male CLL patient. With women, I have more of a discussion. We talk about the risks of having CLL and the impact on blood counts, which will happen as a pregnant female with CLL, because they often become anemic, and it can change the white blood cell count. We talk about the timing of therapy as well. For a woman, it’s a longer discussion and we try to see if we can plan a little bit.
There’s animal data and we have anecdotal data of these therapies. I’ve had several younger CLL women patients who have had successful pregnancies and deliveries. That’s the good news, but there’s a paucity of data in this regard only because the disease impacts older patients and most aren’t having children later in life. You need to talk to your provider, but you can plan for families.
Building the Best Medical Team
Jeff: When we were doing the introduction, one of the things that we mentioned was team building. The National Football League (NFL), for all intents and purposes, is one of the best team sports out there. Even more important than that, as far as I’m concerned, is team building for CLL. The reason why I say that is that I help manage a Facebook community that has over 18,000 patients and caregivers.
Dr. Lamanna: That’s a lot.
Jeff: That’s a lot of folks impacted with CLL. Invariably, when they join us, the first question they ask is, “Do I really need to see a CLL specialist?” And everybody, almost in unison — very rarely on the same pitch — will say, “You don’t have to go to one; you just have to see one once. You’ve got to get a CLL specialist on your team.” You’re a CLL specialist.
Dr. Lamanna: It’s a biased question.
Jeff: It is a biased question. How can a CLL patient go about putting together the right team? Not everyone has access to a major metropolitan CLL center with CLL specialists. Is there a difference between being treated at a local community hospital versus a big cancer center? How do we put all this stuff together?
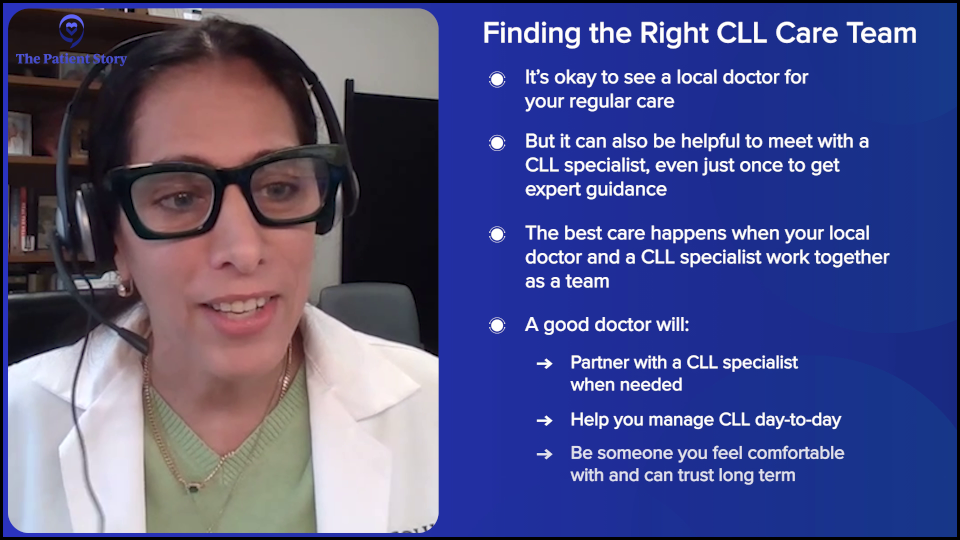
Dr. Lamanna: I’m a CLL specialist, so, of course, I’m going to be biased. I work with lots of patients who aren’t able to come to big academic centers or to the city, which makes sense. You should feel very comfortable with your local physician. If your physician is a community physician, you want to be able to have an open dialogue and be able to ask questions.
I agree that you should see a CLL specialist. No doubt, this is a rare disease, so most of the doctors in the community — and I am not knocking the community docs; they work hard — might see a variety of different diseases, so they may not know the most up-to-date information about CLL per se if they’re treating many diseases. I think that it’s good to see somebody once or at critical times, perhaps if you’re requiring therapy or getting therapy again. It’s always good to touch base with a CLL specialist and have them part of your team because they can be helpful. They can bring up treatment ideas that maybe the local physician hasn’t thought of or can partner with the local physician. I think that’s important.
For my patients who come from afar, if they’re in another state and they have an emergency, I need to make sure that they can get care very quickly, so I want them to have a local physician. If their physician is comfortable with me, where I can talk to them and they can talk to me, then that’s a good sign. If they’re intimidated and have a problem with me, then that’s a problem. I don’t have a big ego. Jeff, do I have a big ego?
Jeff: You do not have a big ego.
Dr. Lamanna: I am just a humble CLL doc who wants to take good care of my patients. That’s my drive. Not all the other stuff. If you can have a meaningful conversation with your physician and they’re willing to work with a CLL specialist at critical times, that’s important. There might be aspects of your case that are complicated or new treatment options.
It’s great to have a CLL specialist on your team and to know that your local physician is the one managing you on a day-to-day basis. You should feel comfortable with that. You need to have a good rapport.
Remember, CLL is a journey. As Jeff noted, he’s had this for years. You’re going to have your physician, hopefully for years, so you want to have a good relationship with them and their team because that’s the one that you’re going to go to all the time. It’s great to have them like a primary care physician in a way. They’re there with you for years. You get to know them and they know all about you and your other medical problems. You form this long-term bond.
It’s always important to include a CLL specialist. If you’re able to do that, that’s great because they can be important at critical junctures during your journey, like treatment discussions, unusual side effects, or complications. Sometimes patients can be very complicated. The community physician will be there for you all the time, so you need to have a good relationship with them. If they’re comfortable working with a specialist if and when needed, then that’s a good sign. That’s a great sign.
How Can Patients Facilitate Communication Between Their Community Doctor & A CLL Specialist?
Jeff: Keeping the NFL metaphor going, having a CLL specialist as your quarterback seems to work out pretty well. It’s been my experience that in this day and age, most doctors have absolutely no problem cooperating with other doctors. We’re not in the ‘60s and ‘70s, where the doctor was the center of the universe and there was absolutely no room for anyone else. It’s a relationship.
As you said, CLL is long-term. There are so many wonderful choices available now and many more coming in the near future. You have to have that long-term relationship. Let’s talk about what the patient can do to facilitate the quarterback and the local team player. What questions should the patients be asking? What should they be taking note of and keeping track of? What’s the best way for them to share test results and treatments with all the doctors? How do we put everything on one plate?
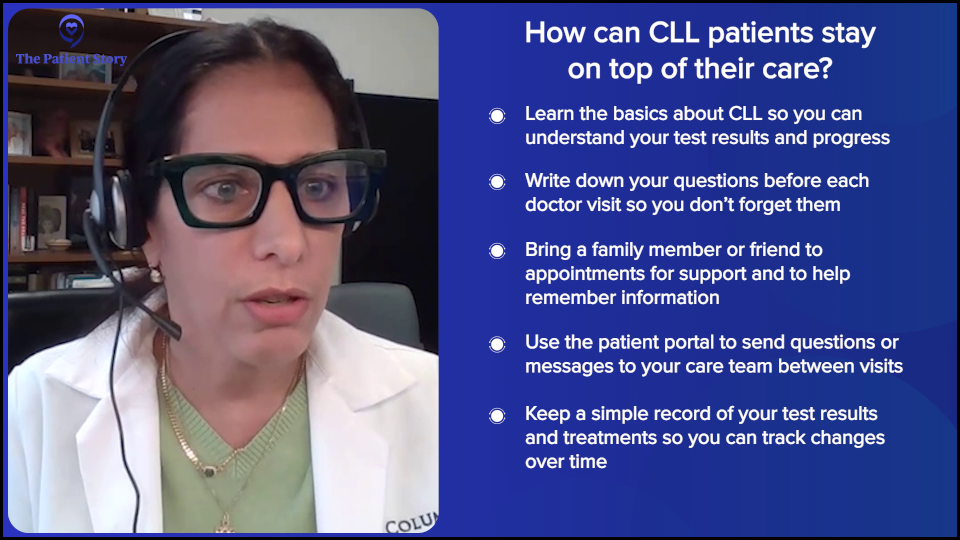
Dr. Lamanna: Forums like this and online communities, like the one Jeff manages, are very helpful to have a basic understanding of your disease. Try to understand what it is to have CLL and how to look at your blood counts. You don’t have to be a scientist or a professional. It’s all about having an understanding, so that if you want to look at your blood counts, you know how to interpret a little bit about what they could potentially mean. That will help when doctors are talking to you about where you are on your journey. Are you progressing? Are you stable? Are things fine? What’s going on? Understanding your disease is important.
When you go to a doctor’s visit, it’s good to bring somebody if you can because you may not hear everything. Your helper will also hear things so that later, if you’re wondering about whether a doctor said something, you have somebody else as another set of ears. I always tell patients that if they have questions, they should write them down and bring them in, so we can go over them. They can also send messages through the patient portal. Many hospitals and centers have portals, so you can message your questions to your team.
It’s always important to write them down because you won’t always remember when you go to the office. Maybe you just had your blood drawn, so you’re anxious, which is totally normal during a visit, but you might forget things. Always bring a list of questions.
Spend some time getting a general education about your disease with your team. There are some patients who don’t want to do a lot of reading online and that’s okay.
Jeff: It’s okay.
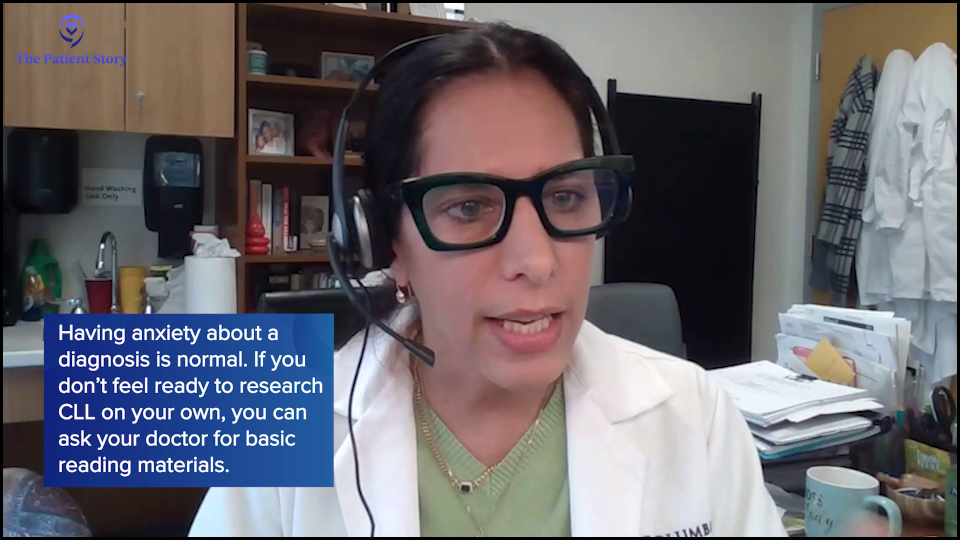
Dr. Lamanna: There are some patients who, for them, it could be very anxiety-provoking. If you’re not at the point where you want to hear other people talk about their CLL or their treatments, then don’t. The internet can be good, but it could also be bad because you can Google things, and it just spits stuff out. Because CLL is a very heterogeneous disease, patients may be at a different point in their journey than you are, so that could be very anxiety-provoking, too. If you’re not ready for all that, then pull back and keep it very simple with your doctor.
Usually, when I first meet a patient with CLL, I spend a good amount of time educating them about their disease, and I hope they feel that way. I also give them some general reading material and guidelines. I give them a printout about healthcare maintenance, vaccines, and other things that they may not remember, so they can go home with a little package after they first meet me.
It takes many visits to understand the disease itself, what it means to look at your blood counts and the lymph nodes, and things like that. I would advise people to write things down, bring questions, and bring somebody with them, so you have an extra pair of ears. Write other questions. After the visit, if something comes up and you’re not sure, you can ask your provider or team.
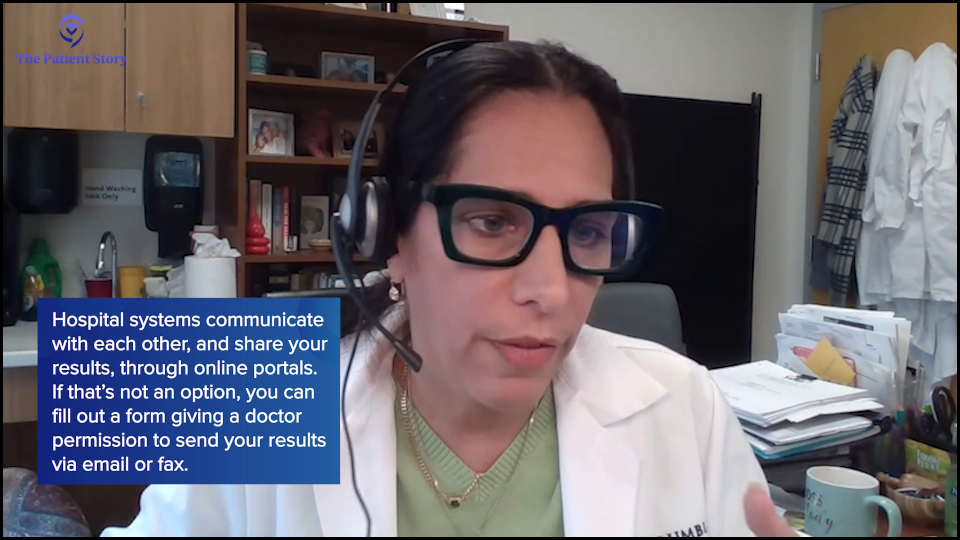
Now, let’s say you have multiple people involved. Jeff, you asked about how to share information with other providers or with the CLL specialist. Most hospital systems nowadays are doing well with working through systems. Many hospitals even cross-communicate. You can ask your physician, “Do you partner? Are you online? Can my CLL specialist see this through one of these hospital systems or not?”
They’ll know because they’ll say, “Oh, yeah, they can see me and I can see them,” so then that’s easy. You can message the team and say, “Hey, I had a CT scan and the results are online,” or “I had blood work done.” If they don’t, then it’s still the old-fashioned way of uploading or sending by fax. That works, too.
Jeff: They still exist.
Dr. Lamanna: It still exists. And that’s okay too, right? It depends on where you are, what kind of system they have, and if they integrate with other systems, so that information can be shared between the physicians.
That goes not just for your CLL, but for other medical problems. This is common. I was in the clinic yesterday and my patient had a CT scan for a completely different reason. I said, “Hey, can I have access to that CT scan? I’d like to look at it. I’d like to see how your lymph nodes are doing, too.” It provides another opportunity. They weren’t linked in, but I said, “Don’t worry. We’re going to have you sign a release, so I can have my secretary work on getting that scan.”
There are different ways to communicate with the teams. You just need to ask your doctor. “Can my doctor see this through your system or not? If not, can we make sure that they get a copy of it?” Or you can upload yourself. A lot of my patients are very tech savvy, so they upload the lab results and reports into their own portal, so I can see them, but you don’t have to do that. You can have the physician’s office do that, too, if you’re not so savvy or can’t do that. You just need to request and then everybody can see the information.
Jeff: As far as what the medical teams need to know, I’m going to have to underline one particular plan of action for all male CLL patients. When you walk into the doctor’s office and the provider asks how you’re doing and you say, “Fine,” please bring your significant other, because “fine” is not the correct response. Your significant other will absolutely underline that you’re not fine. X, Y, and Z are going on along with ABC and one, two, three. We need to get this information in the hands of our medical providers so that they can be responsive to our CLL.
Dr. Lamanna: If you’re a non-talker, it’s always good to bring a partner if you’re not going to talk, as they know what’s going on with you. We always joke around because then the partner or spouse will start bringing up other stuff. They say, “You see? I’m in trouble. They’re talking about everything.” That happens.
Jeff: You just have to go with it.
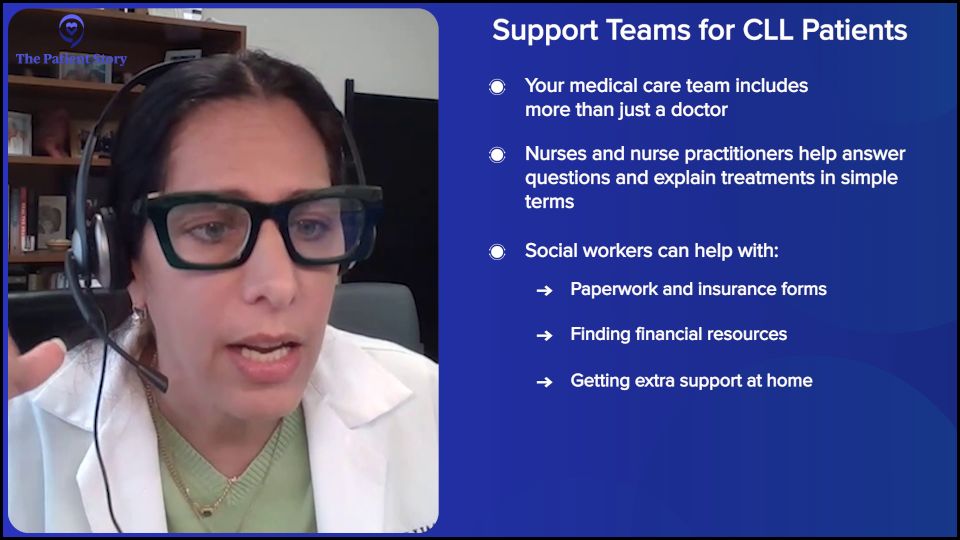
Understanding the Roles of Your Team and Patient Advocacy Groups
Jeff: We talked a little bit about medical providers. What role do social workers, patient advocacy groups, and other support systems play? How does that work with the CLL care team? I mentioned 18,000 people on the CLL Support Group on Facebook. There are dozens of CLL groups on Facebook and throughout the country. How do these support roles fit into this program?
Dr. Lamanna: Let’s first talk about your medical team and then about the outside support. Besides the physician, many of you have probably already interacted with a nurse, a nurse practitioner, or a physician assistant. They’re part of the medical team, per se. They’re also very good at handling and putting out fires.
My NP is great at education. She’ll do educational sessions before somebody starts treatment. They do a whole video visit to educate about the drugs and side effects. They’re part of your medical team, too, and often may respond for the physician, depending on what’s going on.
We also have social workers who can get involved, depending on the person’s needs. Not everybody needs a social worker, but some people do. They have questions that are not necessarily medical but are tied in. I get them involved if I think that the patient needs extra resources. Sometimes that could have to do with financial resources or other social resources that they might need. The social worker can be very helpful with paperwork or facilitating other means that might help the patient if they’re on treatment, where they may need other support besides medical. Most practices, whether it’s academic or community, have a social worker.
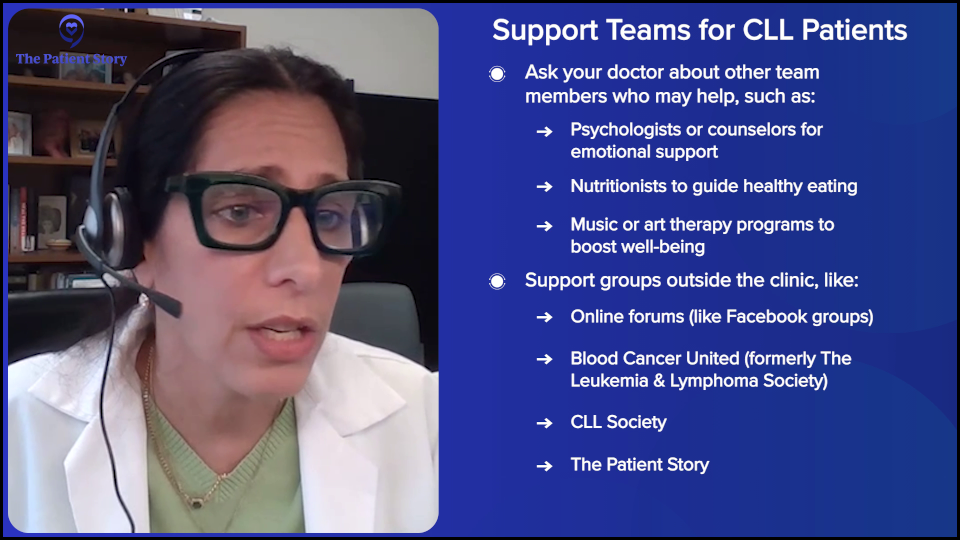
Before we get outside the medical team, other things could be available to the practice, so it’s something you should ask your physician team. There are psychologists and psychiatrists. There might be other services in the medical practice, like nutritionists, art therapy, or music therapy. That’s something that you can ask during the first visit. You may not need those services right away, but maybe it’s something to think about.
Ask the practice what other internal resources you could take advantage of, so that if you need them, they’re available to you and the physician can get them involved as well. It’s important to know that there are internal groups. Sometimes people need psychiatric or psychological counseling to help them initially with their new diagnosis, besides talking with their physician or provider. Or maybe you feel uncomfortable dealing with just your partner because it feels too stressful, so you want someone else who can hear you out. There’s nothing wrong with any of these.
Then, as Jeff noted, there are external resources, like organizations and groups that have these forums. But also, we have the Lymphoma Research Foundation, Blood Cancer United (formerly The Leukemia & Lymphoma Society), and many online groups with resources available to patients that they could take advantage of, depending on their needs.
I give a list to my patients, even if they don’t need them right away, so that they have them already. These are things to bring up to your physician. If there’s something that you think you’re not getting assistance with, your physician can tap in or tell you where to go to help make your life a little easier. There are internal and external resources for CLL patients and for cancer patients in general, and patients may not know how to take advantage of them. If there’s something that you feel isn’t medical and you’re not sure if you could ask your doctor, bring it up with your physician. There are a lot of untapped resources for leukemia patients.
Clinical Trial Options for CLL
Jeff: At the beginning of this presentation, we talked about the exciting treatment options available and in the works. We’re now going to talk about what I think is the most important part of CLL: clinical trials. The reason why I think that is because without them, we wouldn’t have any of this new cool stuff to use for our CLL journeys.
I participated in a clinical trial more than a dozen years ago and I got great results from it, even though I’m currently relapsed. Without the knowledge that was gained from that clinical trial, we wouldn’t be able to build on the new stuff. What clinical trial options are available for CLL patients today and how do they fit into their personal treatment landscape?
Dr. Lamanna: I want to thank you, Jeff, for participating in a clinical trial; kudos and thank you. There’s a big misconception out there about clinical trials and, as Jeff noted, we can only move the field forward and bring new agents to patients through clinical trials. Patients get very fearful about clinical trials because they think they’re experimental and they’ll become a guinea pig.
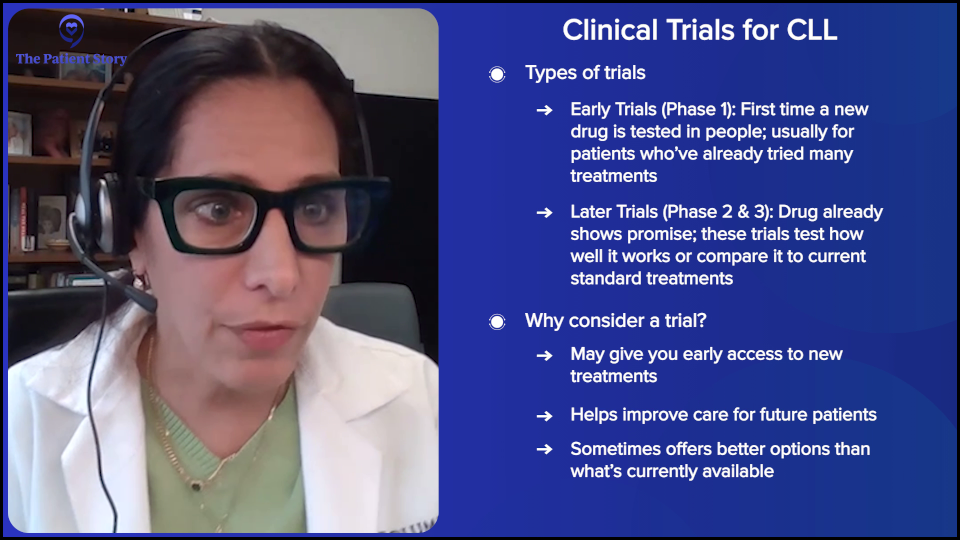
There are different types of clinical trials, which are very important to note. There are trials where the drug hasn’t been studied, meaning it’s the first time it’s going to be in a patient, so we don’t know the dose yet or the potential side effects; that’s a phase 1 clinical trial. Usually, the patients who participate are those who have received all forms of standard care and other agents, so somebody who’s very relapsed and we’re looking for newer options for them.
Then some trials are further along in development, meaning we know the dose and side effects, they’re looking promising, and we’re moving them up in development. They’re expanding to see how well it works, what the results are, or compared to a standard of care treatment. Is this better than our current treatment? These are usually done on patients who are less heavily pretreated or newly diagnosed, where we’re comparing it against a standard of care and we think it might be better.
There are different types of clinical trial options. As a patient, how do you figure that out? Do you have access to clinical trials? Depending on where you’re at, your team may or may not have access to clinical trials or run clinical trials, so that’s one question. If so, can they partner with other places? Are you interested? This is where a CLL specialist is important because there might be a good option for you, depending on what you’ve had and where you are in your CLL journey, that perhaps a clinical trial could be a good option for you. You won’t know unless you inquire.
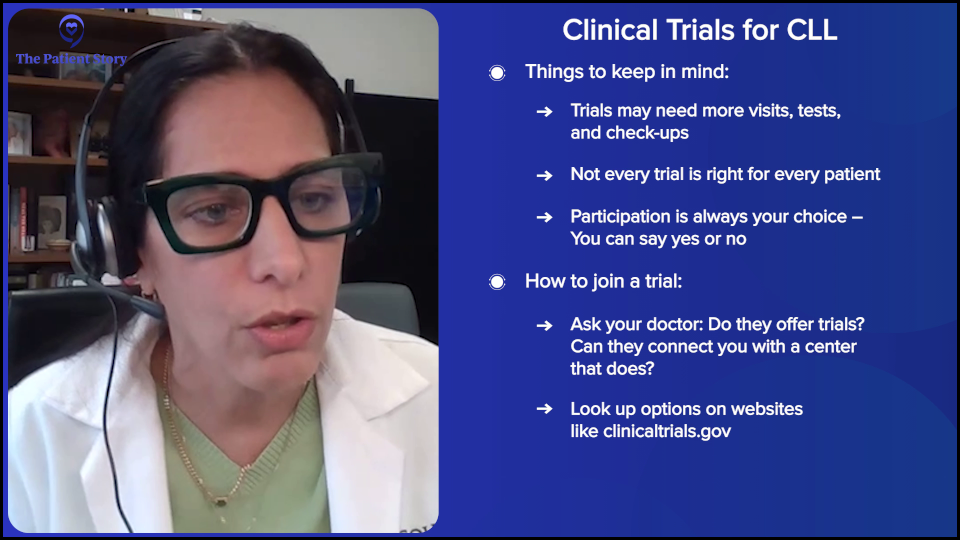
Now, clinical trials aren’t for everybody. Being in a clinical trial means you’re going to commit to more than you would normally. Jeff can probably tell you this better. Many clinical trials will do more blood work, more imaging, and more checking in because they’re following patients very closely to look at responses and side effects. They’re going to do more than they would usually as standard of care, so you have to be comfortable with that.
The first question is what clinical trials are available to you, so you want to talk to your provider about access to clinical trials if and when available… and if you need it. There are also ways that you could do online research. There are websites that talk about clinical trials, like ClinicalTrials.gov. Clinical trials change all the time. We open and close studies all the time, so what might be running at one point in time may no longer be open. We might be done with that trial and have moved on, so that’s important, too.
If you need treatment, whether it’s your first or subsequent lines, do you have any access and what are those clinical trials? It’s a good time to talk to a CLL specialist about that and your provider. If your provider has access to trials, then you could sit down and talk about them.
Usually, the provider is trying to make sense of each individual. Not every trial is right for every patient, which is very important. Some trials are very appropriate for a patient, depending on where they are with their disease, but not for another person. Your provider is supposed to help guide you based on where you are with your disease, what the best options of treatment are, and how a clinical trial might enhance that aspect or not.
It’s an important and critical time to talk to somebody if you’re interested in clinical trials because it might provide you with the next best therapy. I think that was what Jeff was getting at. It might provide a lifeline. If you’ve had all these other treatments, where do you go next?
Jeff: I love the way the clinical trial was presented to me. I was told that my participation would get me earlier access to the best stuff. We know that this is going to be great and this will get you quicker access to it, and I liked that approach.
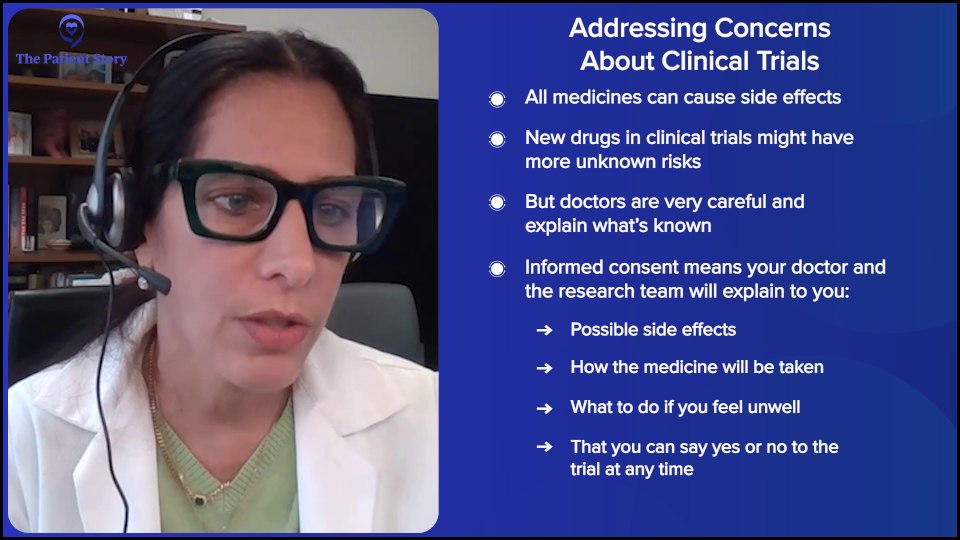
Addressing Concerns About Clinical Trials
Jeff: Earlier, you mentioned phase 1 and phase 2 clinical trials. Some clinical trials have risks. How do you address the risks of clinical trials with your patients?
Dr. Lamanna: Absolutely. Even the drugs we now consider standard of care were in clinical trials at one time.
We have to talk about the side effects or potential side effects. This is necessary whether the treatment is a new drug or part of a trial that compares a standard of care with a newer drug whose side effects we already know. We have to talk about all potential side effects, regardless of whether you’re on a clinical trial or not.
Obviously, with earlier phase studies, we may not know all the potential side effects of a newer treatment, especially if something has never been used in humans. But usually with more advanced clinical trials, we pretty much know a lot about the side effects and we need to talk about that. That’s what informed consent is all about. You might have other medical problems, so how does the treatment fit with your medical problems and other medications? You need to have an open dialogue about whether it’s right for you.
Again, whether it’s a part of a trial or not, we should be having that discussion. That’s informed consent, even if you’re not on a clinical trial. We need to talk about the side effects, so you’re aware. “If I have a side effect, who do I call? What’s the dialogue going to be when I’m on treatment, so that I can get access to you and your team and they can help me with my side effects? Should I stop the drug? Am I going to amend?” Whether you’re on a trial or not, it’s important to understand the potential side effects when you’re on treatment.
Remember, those commercials on TV where they talk about a drug and you hear all the side effects? Even with taking aspirin, there could be a bad outcome. Somebody could have died from taking something as simple as an aspirin. Informed consent is important, but the doctor needs to tell you the frequency and commonality of those side effects, so you can make sense of them and not panic. Otherwise, nobody would ever take treatment. Ever. You have to make sense of them, work with the team, and talk to them.
The clinical trial process is lengthier for sure. There’s more work to be involved in one because you’re going to be seeing the team much more often and doing much more. You’ll have more blood work and potentially more imaging, so you need to be comfortable with that.
Exciting Areas of CLL Research
Jeff: We’ve laid out clinical trials and I know you do a lot of work with clinical trials. I’m going to ask you to pull back the curtain a little bit. Tell me what’s exciting. What’s the coolest stuff that you’re working with in clinical trials right now?
Dr. Lamanna: As I noted, we have BTK inhibitors and a BCL-2 inhibitor, venetoclax (Venclexta). There are newer classes or newer mechanisms of action that we’re very excited about, which I hope will lead to newer FDA approvals in the near future.
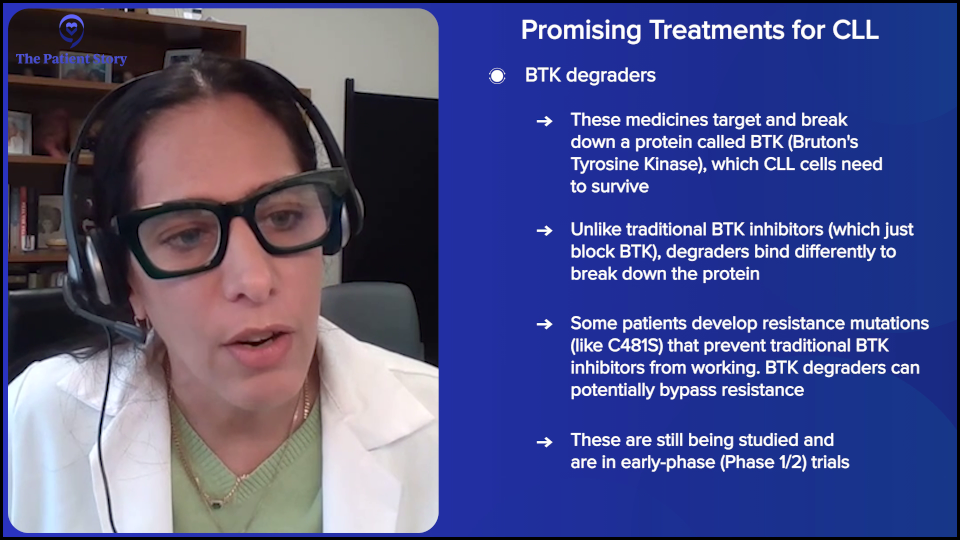
BTK inhibitors bind to the Bruton tyrosine kinase protein. These are ibrutinib (Imbruvica), acalabrutinib (Calquence), and zanubrutinib (Brukinsa). We even have a newer one called pirtobrutinib (Jaypirca), which binds a little bit differently to BTK.
What does that mean? Unfortunately, these drugs are not curative, so patients can develop resistance to the site where they bind to BTK, all of these drugs. Eventually, people may develop resistance to their therapy. BTK degraders bind very differently to BTK, which is very important in the survival of CLL cells. It binds the whole complex and it degrades and gets rid of the whole complex differently. Theoretically, it could get around the resistant mutations that are on some of these BTK inhibitors, where they bind to one site and then the protein changes, so they no longer are effective because now they’ve developed a mutation at the site that they can’t bind to anymore.
The BTK degraders will bind as a complex and they’re looking very promising in clinical trials. There are several of them that are in development. Again, we usually start new drugs in patients who have received prior treatments that are working well for them. These trials are being done in patients who have had relapse or multiple lines of pretreated CLL.
The responses are looking encouraging. Trials are looking at them by themselves, but there are also going to be trials that will look at them in combination with other agents or in less heavily pretreated patients. I’m hoping that’s a different mechanism of a drug that will be available at some point in the future. We still need some time. It’s very early. That’s one very exciting group of agents being looked at.
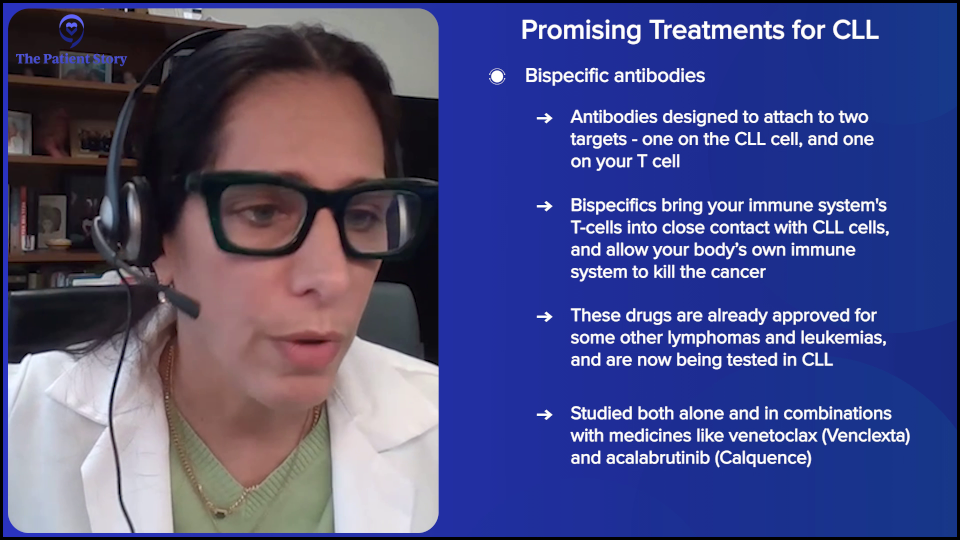
Another group of agents that is very exciting is called bispecific monoclonal antibodies. Like rituximab (Rituxan), which I told you guys about earlier, or obinutuzumab (Gazyva), which binds to CD20 on your CLL cells, the bispecific antibody binds to one of the markers on your CLL cells and that could be CD20 or CD19, but it also binds to your T cells, so that’s why it’s called “bi.” The goal is to bring your T cells in close proximity to your B cells and try to target and kill these CLL cells.
They are also very encouraging in clinical trial development for CLL. They’re approved for use in other lymphomas, but show encouraging results in CLL. There are many clinical trials looking at these bispecifics either as a single agent or in combination with other drugs that are already approved for CLL.
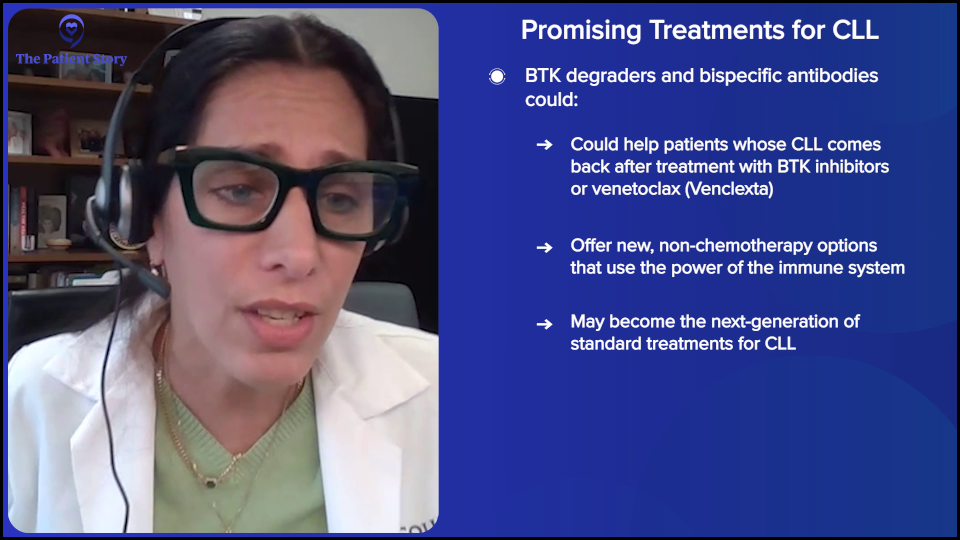
These are going to further enhance what we can do for patients who get current standard of care drugs, like BTK inhibitors and venetoclax (Venclexta). If they relapse and need more therapy, they’ll hopefully have newer agents to choose from through the development of these clinical trials with BTK degraders and bispecifics. It’s very exciting.
There’s more I can talk about. I can go on and on and on. But those are some of the more promising ones in development that I’m very excited about. There are a lot of clinical trials surrounding those mechanisms that are going to be very important.
Jeff: Very cool. There are so many options available to us. When I first started this, there was plan A and plan B, and that was it. You were going to get either/or. Now we have to use up the entire alphabet.
Quality of Life and Treatment Decisions
Jeff: From what I’ve seen over the past few years, quality of life has become one of the most important components in this decision-making matrix. How do you personally help your patients navigate through this complex matrix? Let’s talk about how quality of life impacts decision-making.
Dr. Lamanna: Let’s talk about people who aren’t on treatment. We talk about the quality of life when they’re off treatment. It doesn’t mean that you may not have any symptoms from your disease. Sometimes these are harder to quantify, like fatigue and other things like that. It may be difficult to say this is just your CLL, CLL and other things, or a combination of CLL and other things that are going on in your life. We talk about patients who aren’t on treatment, getting exercise, going out, enjoying life, having a quality of life, and looking at it as a chronic disease that you currently don’t need treatment for.
I don’t like the term “watch and worry.” I think it’s a terrible term. We need to get rid of that because, yes, there’s anxiety and we’re not taking away that component. But if you don’t need treatment for your disease, it’s good to be on the sidelines because you get to see the development of all these treatments that may replace current treatments and potentially have fewer side effects. You might get different options that might be better.
Remember, all treatment has potential side effects. If you don’t need treatment, why get treatment? It’d be different if we had a treatment that cured everybody and then we wouldn’t be having this conversation. But until that occurs, until we prove that starting somebody on treatment earlier is going to do better for the group as a whole, or that it extends survival, we wouldn’t do that. We haven’t shown that yet in clinical trials, so this is why not everybody needs therapy and may not need therapy for years
The goal is to talk about their quality of life when they’re off therapy and if they need help with some of those issues. When you’re first diagnosed, there’s a lot of anxiety, so that’s understandable. Quality of life is one piece.
For people who are in therapy, it’s another discussion about quality of life. We talk about therapies, the side effects of those therapies, and how they relate to what’s going on in their lives at the time. We have great options and you can go from one to another in the future. You can go from a BTK inhibitor to venetoclax (Venclexta) or the other way around.
We talk about how a particular treatment option at the time may impact their life, depending on where they are in their life. Are they having kids? Do they have a young family? Are they working and traveling a lot? Those are important. You need to talk with your provider because these factor into what treatment option you might choose at the time.
Fifteen years ago, I had a very young patient who had a young family and was constantly working, so he chose to do a BTK inhibitor because doing other therapies was more complicated at the time. He said, “It’s easy for me to take a pill. I’m going to do that.” Believe it or not, he’s still on a BTK inhibitor and doing great. Those are some of the discussions you have with your provider because where you are currently in your life may feed into the side effect profile of the drugs and what you may choose, so that’s important.
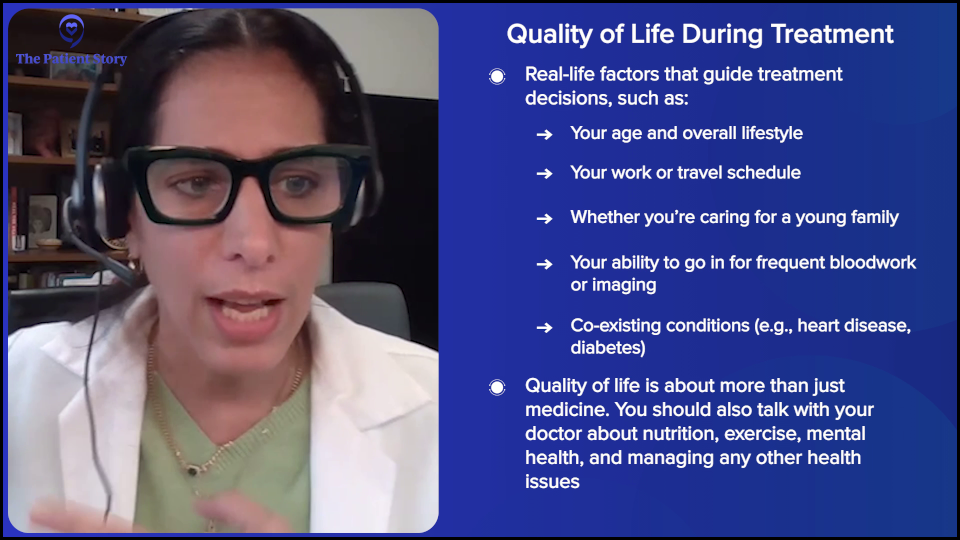
In general, for all patients with CLL, we talk about the other stuff. We talk about diet, exercise, and even psychological counseling and support, if needed. People ask a lot of questions about food and healthy diets.
Other medical problems feed into this, so we talk about their other medical problems and how to manage them if they have other chronic health problems. CLL is chronic, like other medical problems, which is why you need to think about it. Like people with diabetes, heart disease, and high blood pressure, CLL is a chronic condition. That should give you hope because people are living very good quality of lives with their other medical problems, but they need to be well-managed, so sometimes, we need to partner with your other healthcare providers.
I do think, Jeff, it’s an important concern, particularly because we’re getting better at this. We have a long way to go, but it’s important to talk about it since there isn’t one option now. Survival continues to improve and gets better. There’s no single choice where this is your only choice and what you have to do, so discussions on quality of life become important.
How Do I Talk to My Doctor About Symptoms and Side Effects?
Jeff: I want to focus on quality of life a little bit more, if you’ll indulge me. This is part of the communication process that patients need to be hyper-aware of. Medical professionals can’t help you if they don’t know what’s going on. If you’re feeling tired all the time, don’t just deal with it. Let your medical providers know that you’re tired and that it’s more than just being tired after a workout. I’m tired all the time. If you’re getting sick all the time, you need to let your medical professionals know about this.
At the same time, if this is weighing heavily upon you and you’re dealing with stress to the point where it is making life difficult, you need to communicate that to your medical professionals because they can help you. This is part of the treatment matrix and part of deciding how to treat your CLL.
I know that you deal with this with your patients on a very regular basis. I want the patients and their caregivers to know that it’s okay to talk about this. This is part of the shared decision-making that must go on. Would you agree with that?
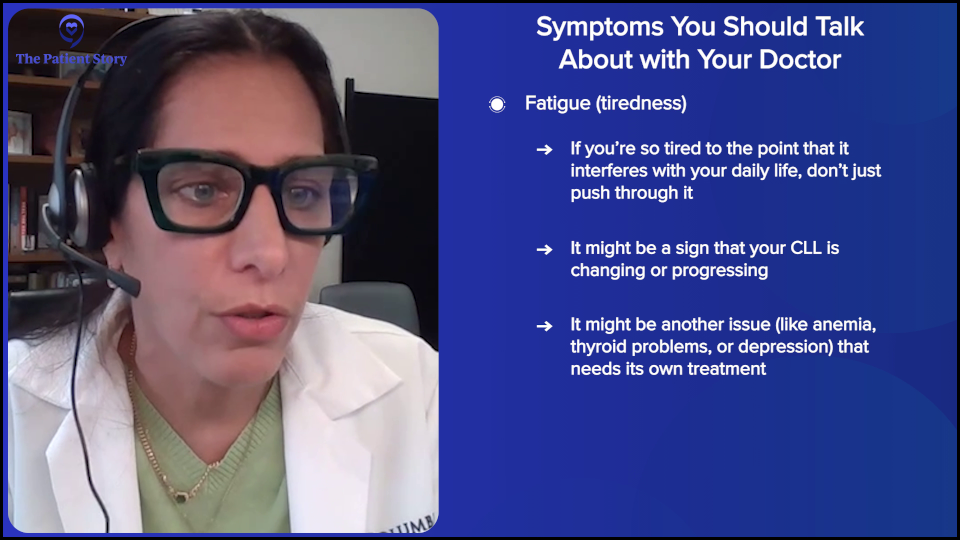
Dr. Lamanna: Oh, absolutely. Importantly, sometimes some of the symptoms, even though you think there’s nothing you can do about them, may be more than that. There may be something. If somebody tells me that they’re tired to the point that it’s inhibiting their daily activities and quality of life, then I will work that up because maybe there’s another reason that they’re tired. Maybe it is related to their CLL. Even if their numbers are okay, I might have to factor that in if they are debilitated, then we do have to talk about whether or not that means embarking on therapy earlier. Because somebody’s not textbook and their counts aren’t terrible, is there something else going on?
There’s a medical intervention potentially that needs to be worked up, or maybe there are other things going on and there’s a different diagnosis or support needed because of whatever symptom. Jeff’s absolutely right. It’s important to tell your provider and healthcare team what’s going on because it could potentially have some ramifications for your treatment or your medical care that you’re not even aware of. They need to work it up and say, “Okay, this is this, and this is why you’re feeling this or not.” They need to make sure that there’s nothing related and there’s an intervention potentially that could help you.
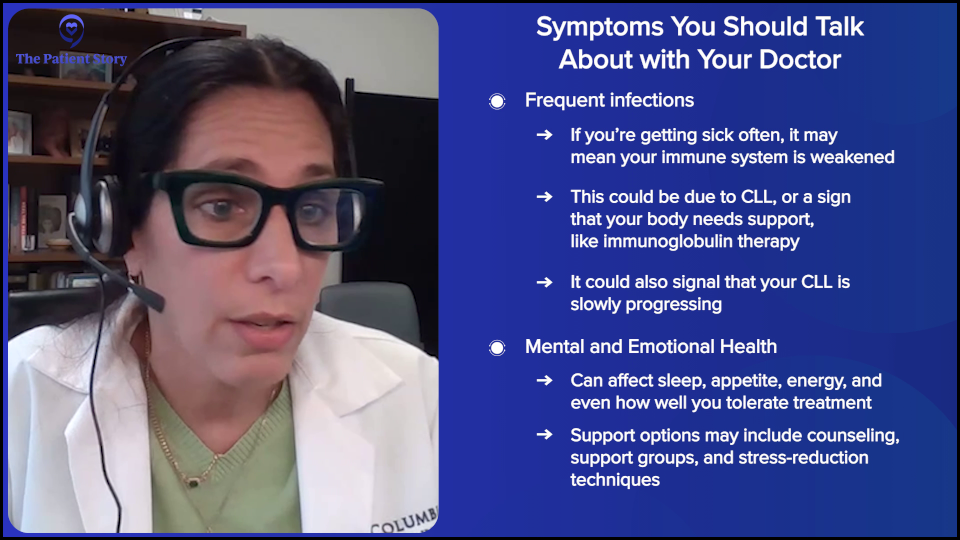
Infections are a big thing. I want to talk about this. Some providers want to know if you’re constantly sick and some providers might say, “I want you to call your internist.” This is a unique thing. I have my people call me because if somebody’s always sick all the time, is it because their immune system is run down? Do I need to factor that in with where they are with their CLL?
Patients who are always sick may need extra assistance, whether they need gammaglobulin or help. Maybe they’re getting sick all the time because their disease is slowly progressing, so maybe we should be treating them sooner. It’s important to share what’s going on with your providers and healthcare teams, so they can help navigate and see if it’s medical or not. Is there another diagnosis? What can we do to help support you through the issues that you’re going through?
Why Isn’t My Doctor Starting Treatment Right Away?
Jeff: I’m going to deliberately avoid the W words for what we do with CLL patients and use the totally stilted phrase “mindful surveillance.”
Dr. Lamanna: I say active observation and monitoring, but active surveillance is great. I use active surveillance too.
Jeff: Just justice tilted, in my opinion. Lee’s got a great question. “Is it a good idea or should I talk to my doctor about other options? Why do we have to wait? Why can’t we just go knock it out now?”
Dr. Lamanna: You’re referring specifically to why I can’t treat it right now, as soon as I’m diagnosed.
Jeff: Exactly.
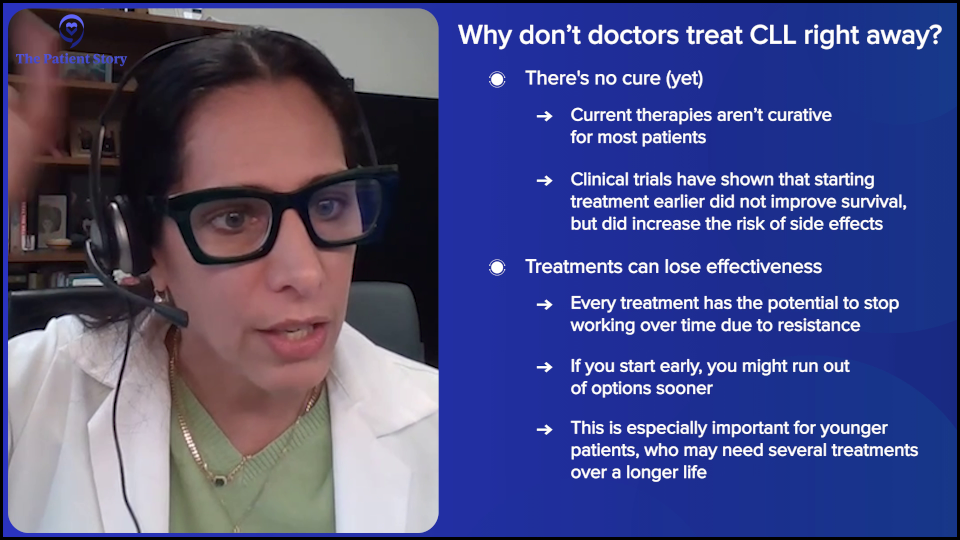
Dr. Lamanna: As I alluded to earlier, we don’t have curative therapy yet. What we have shown, or at least run several clinical trials on, is that starting earlier treatment in CLL didn’t benefit the patient. There were increased side effects from the therapy and it ultimately didn’t improve survival. If we start therapy, we’re giving you treatment with potential side effects and not improving the outcome. That was one of the major takeaways.
But the other major takeaway is if you’re younger — this may have less relevance for older patients — we also know that when you start treatment, there’s always the potential of developing resistance to therapy.
Most of my patients are extremely nervous about their first treatment and all that goes with the first treatment, like the side effects. I’m thinking of not just your first treatment, but also your next treatment, the treatment after that, and the treatment after that.
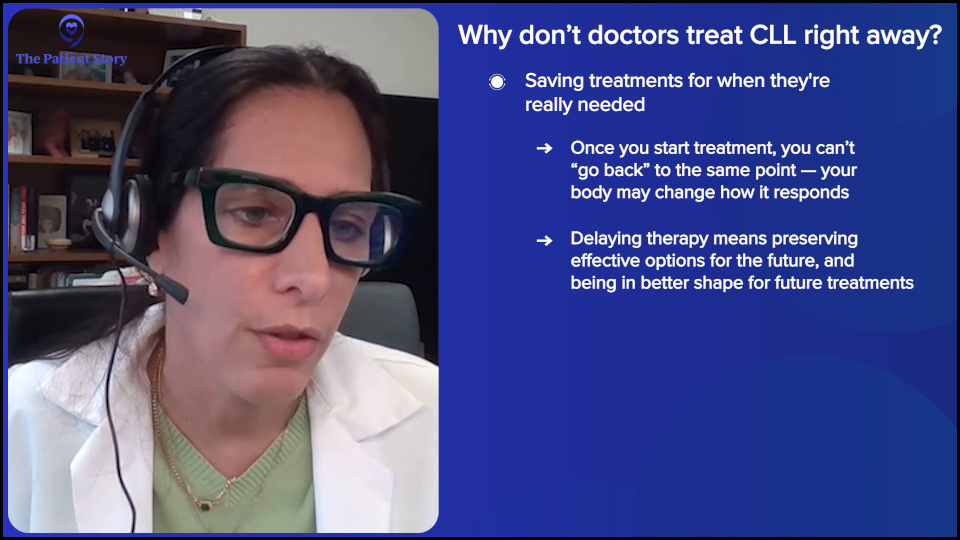
I’m forecasting as your CLL doc in the future. When I look at you, this particular person with CLL, how do I get you to have a normal lifespan? How do I forecast the drugs in the pipeline, the drugs that I need to know, and how to get you there so you can enjoy all the life stuff? We know that if you don’t need therapy, we can potentially start the clock with resistance. I worry about resistance patterns and the ability to use those therapies later on down the road.
Until we prove that starting treatment earlier would benefit you, we will not change that paradigm. The one other cancer I can liken this to is prostate cancer, because many patients with prostate cancer also don’t need treatment if they have low-risk disease and are monitored for similar issues. It’s unusual because when we think about cancer, everybody thinks about how to get rid of it and be done with it.
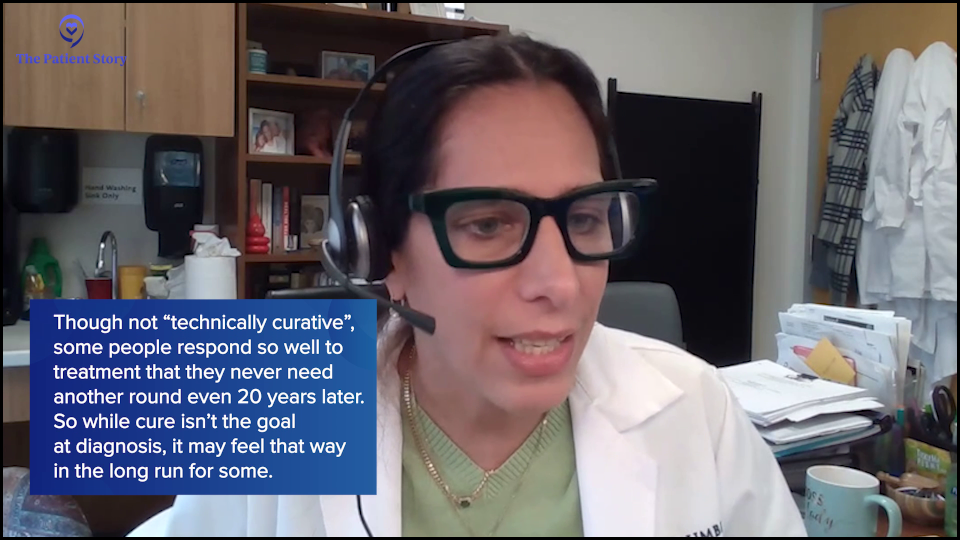
We don’t have that yet in CLL because it’s technically not curative, although that’s also a very loaded term. There are patients whom I have treated 20 years ago and have never needed treatment, and for all intents and purposes, they may be cured of their CLL.
In general, we know that CLL is a chronic disease and can come back, so we think about that and about issues of resistance when we talk about treatment and somebody starting treatment. That’s why we don’t start everybody on treatment as soon as they get diagnosed, because we haven’t shown a benefit yet. We don’t want to take out potential agents that we need later on when you do need treatment.
Jeff: It does. Dr. Lamanna is always thinking three and four moves down the range.
Dr. Lamanna: I have to.
Jeff: Note to self: don’t ever play chess with her. Not a problem.

Conclusion
Jeff: I loved having this conversation with you. When I have these types of conversations, I do get excited. All of these choices that are in front of us right now are here because of clinical trials and because CLL specialists have made the deliberate effort to learn more about CLL. We have more choices today and we’re going to have even more choices tomorrow because we keep on researching.
I find comfort in the fact that as long as I’m on active monitoring, the longer I wait, the more likely it is that a drug that’s going to be developed will be the right one for me and that it could cure me… and that would be very cool.
Dr. Lamanna, I want to thank you for sharing your expertise with us. I love having these conversations with you. You’re a ray of sunshine in literally what can be a very depressing journey for a lot of people. I’m glad that you are so dedicated to making sure that people with CLL live great lives.
I want to thank AbbVie for its generous support of this program. The support helps us to host these educational programs for free. The Patient Story maintains full editorial control of these programs.
We hope that you find this helpful. Remember that this program is not a substitute for medical advice. We hope that it will inspire you to make better decisions and have better discussions with your medical team.
We want to hear from you to make these discussions even better. What would you like? What can we improve?
No matter where you’re treated, your voice matters. Ask the questions. Explore the options and remember that you’re a key member of your CLL care team.


Thank you again to Blood Cancer United and the CLL Society for their partnerships.

Thank you again to AbbVie for its support of our independent patient education program. The Patient Story retains full editorial control over all content.