CLL 360°: It’s Time for Treatment – Making the Right Decision for Me
Edited by: Katrina Villareal
Learn how shared treatment decision-making—a collaborative process where patients and doctors work together to make healthcare decisions—can help you navigate the rapidly evolving landscape of CLL treatment options.
CLL patient advocate Michele Nadeem-Baker for an essential discussion on chronic lymphocytic leukemia (CLL) with Dr. Nicole Lamanna from Columbia University Medical Center and Dr. Charles Farber from the Atlantic Health System and Rutgers Cancer Institute of New Jersey.
Discover what shared decision-making means and how it can empower you in your treatment journey. Get insights into the latest advancements in CLL therapy and how to choose the best treatment plan for you. Learn how to weigh the potential benefits of treatment against its impact on your daily life. Gain strategies for discussing your preferences and concerns with your healthcare team.

We would also like to thank The Leukemia & Lymphoma Society and The CLL Support Group for their partnership.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Introduction
- Treatment Advances in CLL
- What is Shared Treatment Decision-Making?
- What Factors Guide Shared Decision-Making?
- Balancing Treatment and Quality of Life
- Approaches to Treatment
- Bridging the Gap: When Patients and Doctors Disagree on Treatment
- Beyond Initial (Frontline) Treatment
- The Role of Genetics in CLL
- Key Takeaways
- Conclusion
Introduction
Stephanie Chuang, The Patient Story Founder
Stephanie Chuang: The goal of our program is for patients and care partners to walk away with a better understanding of how to approach decision-making with their medical team with all these options. There’s so much rapid change happening with continuous therapy and time-limited treatment. The ultimate question is: what is the best for you and or your loved one?
My name is Stephanie Chuang. I’m also a blood cancer patient advocate. I was diagnosed with non-Hodgkin lymphoma and that experience is how I decided to start The Patient Story, a platform that aims to help people navigate life before and after diagnosis in human terms. We do this through in-depth patient stories as well as educational discussions, which we know is especially important for those who are dealing with CLL and SLL wanting to empower themselves continuously throughout treatment.

We want to thank The Leukemia & Lymphoma Society for its partnership in this program. The LLS offers incredible free resources, including their Information Specialists as well as their Clinical Trial Support Center, both of which provide one-on-one support in different areas for the blood cancer community.
We also want to give a shout-out to our friends over at The CLL Support Group on Facebook led by our friends, including our moderator Michele Nadeem-Baker. They offer ongoing virtual support for folks dealing with a CLL diagnosis.

Michele Nadeem-Baker, Patient Advocate
Michele Nadeem-Baker: I was diagnosed in 2012 and by the time I needed treatment, it was the end of 2015. I had a simple choice: standard of care or go on a clinical trial. I chose to join a clinical trial and luckily, it gave me part of the standard of care in combination with the future of treatment. I discussed all of this with my CLL specialist and we came to a shared decision for my treatment.
When I relapsed a few years ago, I had to make a decision once again. There were so many choices at that point, which was fantastic for patients but made it a little more difficult to make the decision.
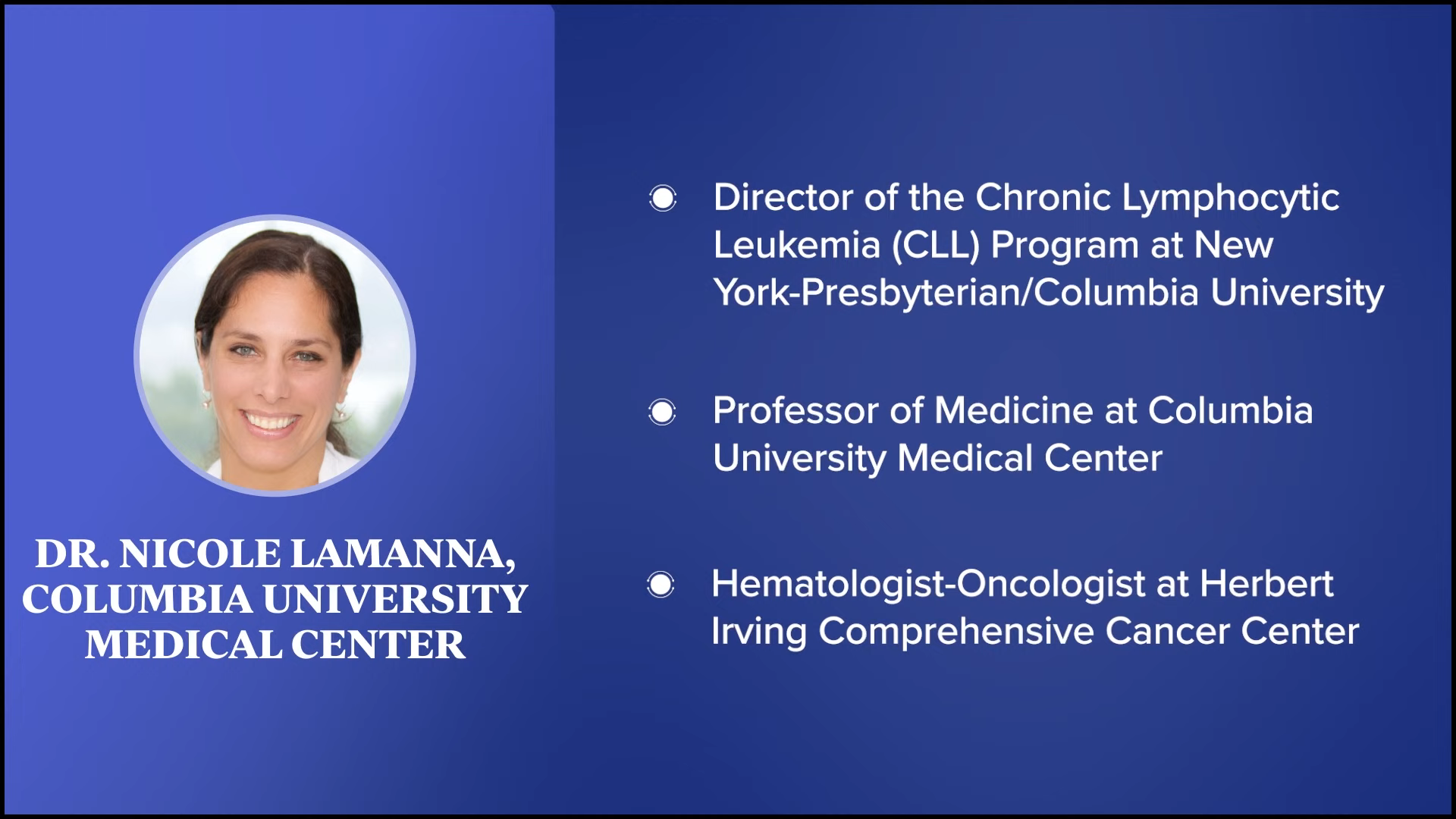
Dr. Nicole Lamanna, Hematologist-Oncologist
Michele: Dr. Nicole Lamanna is the director of chronic lymphocytic leukemia and professor of medicine at Columbia University Medical Center. Dr. Lamanna, what drew you to specializing in CLL?
Dr. Nicole Lamanna: When I was a resident at NYU at Bellevue, we used to rotate at Memorial Sloan Kettering for our oncology experience. As an intern and then as a resident, they put me on the leukemia service every year.
When I became a third year, one of the leukemia docs kept in touch with me and said, “Nicole, what are you thinking about doing?” I was into taking care of the whole patient, so I said, “I’m going to be an internist or a primary care physician. I love taking care of every part of the patient.” He said, “Didn’t we do that on leukemia when you were in the inpatient unit? Don’t you remember we took care of infection, kidney failure, and heart attacks?”
The more I thought about it, the more I thought about applying to an oncology fellowship. Sure enough, that little push and having good mentors did that for me. I decided to apply for a fellowship and went to Sloan Kettering. While I did my fellowship, I did my research with one of the leukemia guys, was taken under their wing, and started working with a CLL mentor. I wouldn’t be doing this if it wasn’t for them. I give them lots of credit.


Dr. Charles Farber, Hematologist-Oncologist
Michele: Dr. Charles Farber is a board-certified oncologist and medical director of oncology research network development for Atlantic Health System. He also serves as a clinical assistant professor at Rutgers Cancer Institute of New Jersey. Dr. Farber, what drew you to specializing in CLL?
Dr. Charles Farber: When I was a college student, I was working in a laboratory and doing structural activity relationships. I got into an MD/PhD program at NYU and was slated to go there and start research with Eric Simon who coined the term endorphin.
Right before I got there, he moved to Columbia, so I had to find someone with a research interest that would overlap with mine. I looked at the faculty at NYU and Robert Silber was doing cutting-edge work in CLL. I ended up joining his laboratory and I’ve kept up my interest in CLL throughout my career.
Treatment Advances in CLL
Michele: Doctors, the world of CLL has changed tremendously with so many more treatment options. Dr. Lamanna, can you give us a summarized update on the current CLL treatment landscape and how it’s changed, especially in the last couple of years?
Dr. Lamanna: To allude to what Michele was saying, back in the day, we had chemoimmunotherapy regimens like fludarabine, cyclophosphamide, and rituximab or FCR, or bendamustine-rituximab intravenous therapies. These were standard of care. We didn’t have as many choices.
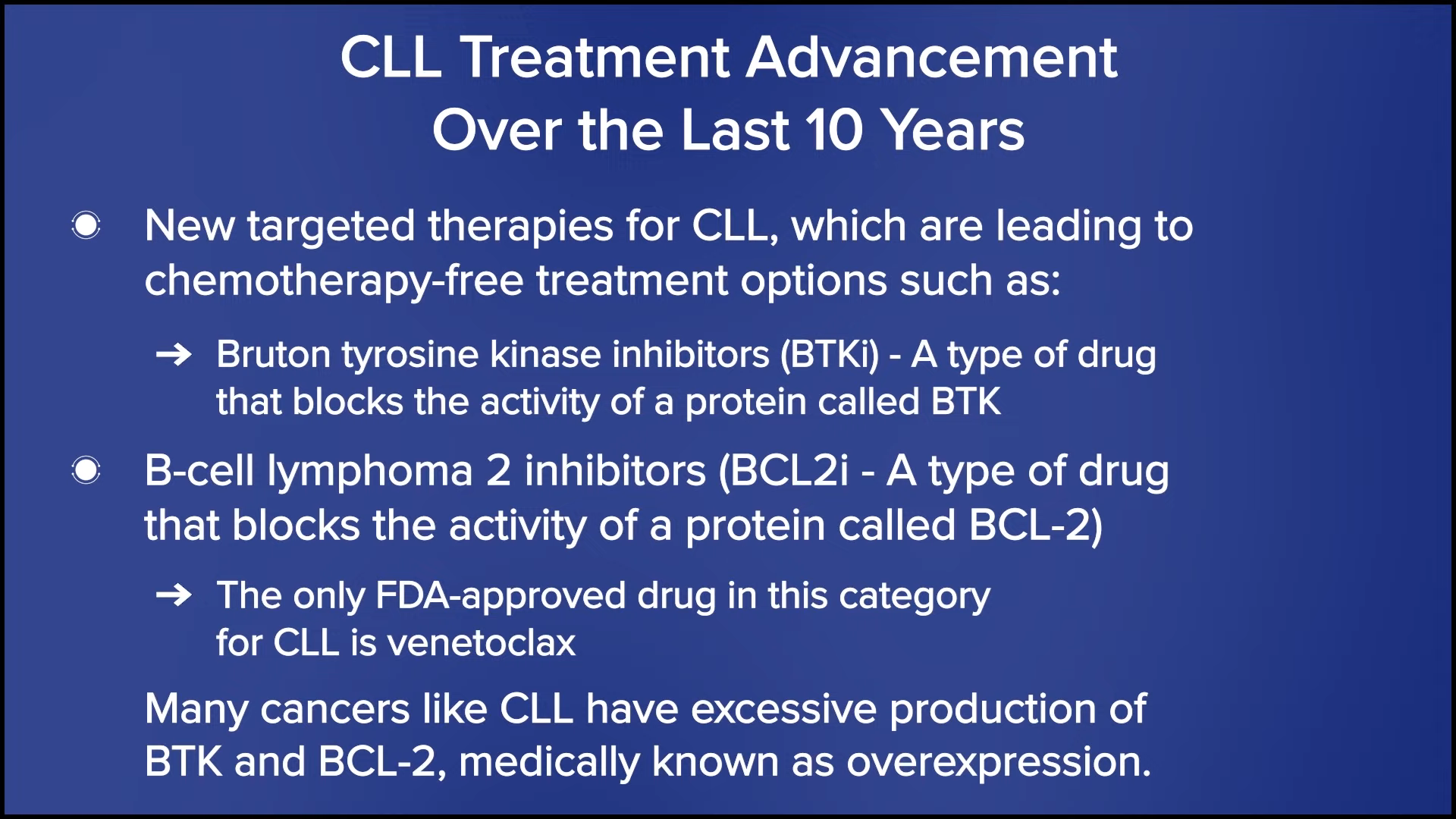
Now we have more of these targeted small molecule inhibitors. The two big classes we have are BTK or Bruton tyrosine kinase inhibitors and BCL2 inhibitors. These oral therapies have become the standard of care. Patients can either take a chronic therapy with one of these oral BTK inhibitors or you can get a time-limited approach with a BCL2 inhibitor.
The only one we have currently approved is venetoclax in combination with a CD20 monoclonal antibody, which is rituximab or obinutuzumab. We’ve moved away from chemotherapy and now people are on either BTK inhibitors or some sort of venetoclax-based therapy.
Shared decision-making is a collaborative process where patients—often with their family members—and their doctors sit down, communicate, and come up with a plan.
Dr. Charles Farber
What is Shared Treatment Decision-Making?
Michele: I’m extremely thankful for all of these new treatments, but this means choices, and choices mean decisions need to be made. Many patients are hearing the term shared decision-making. What does that mean?
It’s understood that doctors are the experts from a medical and clinical standpoint, and patients are the experts on themselves and what matters most. Dr. Farber, please explain in simple terms what shared decision-making means when it comes to treatment and what the process typically involves.
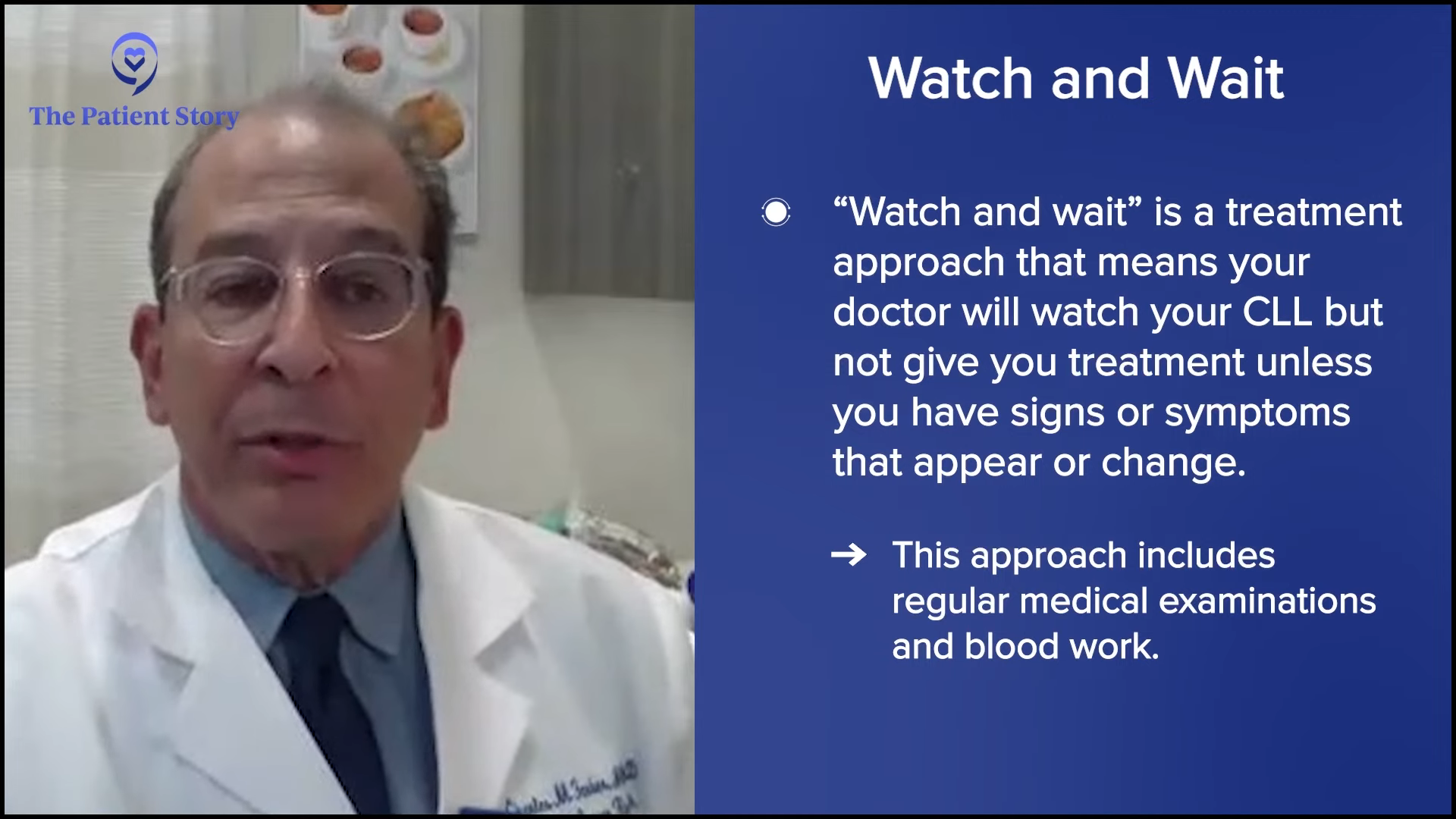
Dr. Farber: Shared decision-making is a collaborative process where patients—often with their family members—and their doctors sit down, communicate, and come up with a plan. It’s not limited to a choice of treatment or duration of treatment. With CLL in particular, most patients don’t need treatment, so we observe them. We do watchful waiting or as my patients refer to it, watchful worrying.
The first decision is what criteria need to be met before a treatment is offered. Then we discuss what treatment options are available, what are they, and what’s best for the particular patient. It’s individualized, so it relies on two-way communication where the doctor may have in mind what’s best for the patient, but the doctor doesn’t make the decisions for you.
We do share in the decision-making where it’s appropriate. It boils down to trying to communicate and impart important information to our patients and their loved ones to determine what’s best. It’s interactive. It’s a dialogue. The doctor with their experience and knowledge has to work with the patient with what they desire.
What Factors Guide Shared Decision-Making?
Michele: Dr. Lamanna, what factors guide you in making treatment decisions?
Dr. Lamanna: This has become more complicated and part of it is because shared decision-making has become more present because we have more options. When there was only one option, the choices were whether the patient was going to do treatment or not. With all these options, it becomes a conversation.
We do shared decision-making because these treatment options are slightly different… what may be relevant for them at this particular moment in their life may be different later on down the road.
Dr. Nicole Lamanna
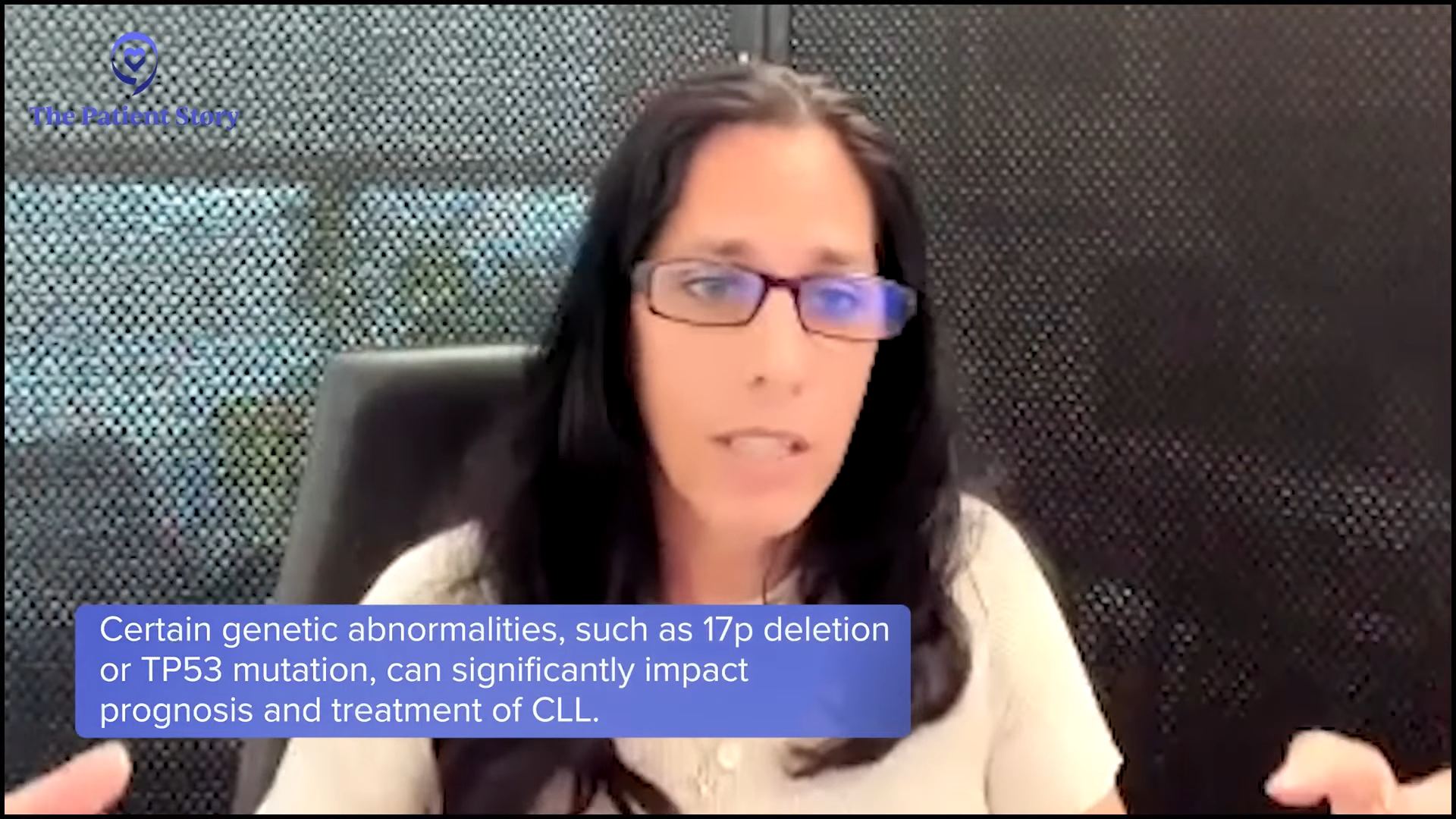
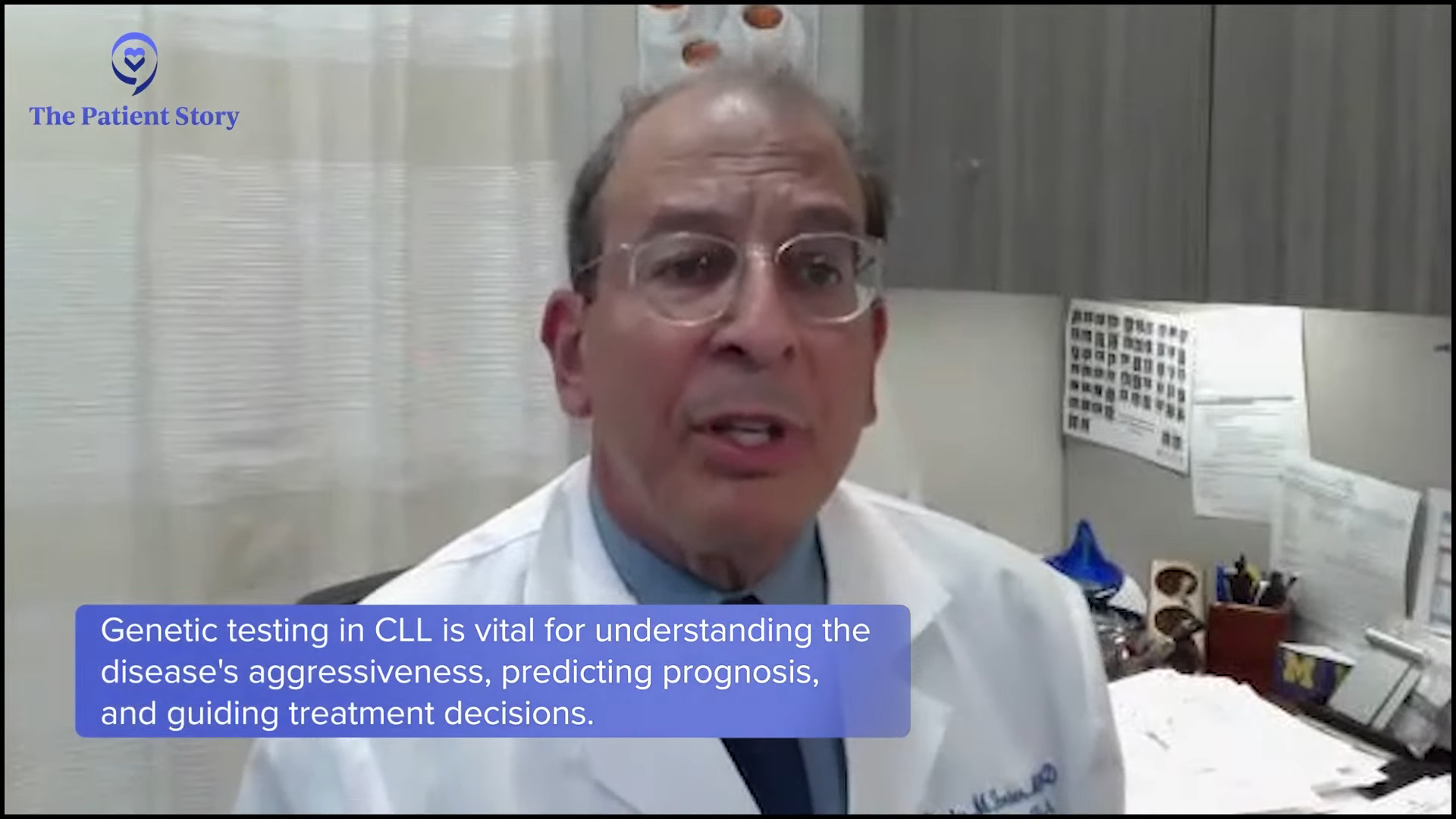
We think about the genetics and the disease itself. What is going on with the patient? What are the features of their disease? Are their blood counts bad? Do they have big bulky lymph nodes? Do they have genetic features? Do they have chromosomal abnormalities? Do they have high-risk disease? You might hear about 17p deletion, TP53 mutation, or even multiple chromosomal abnormalities.
What other medical problems does the patient have? What other comorbidities do they have? How is their kidney function? What are their social circumstances? Can they get back and forth to the clinic or the hospital frequently or not? Do they need extra support? Are we looking at therapies that might be easier for that patient?
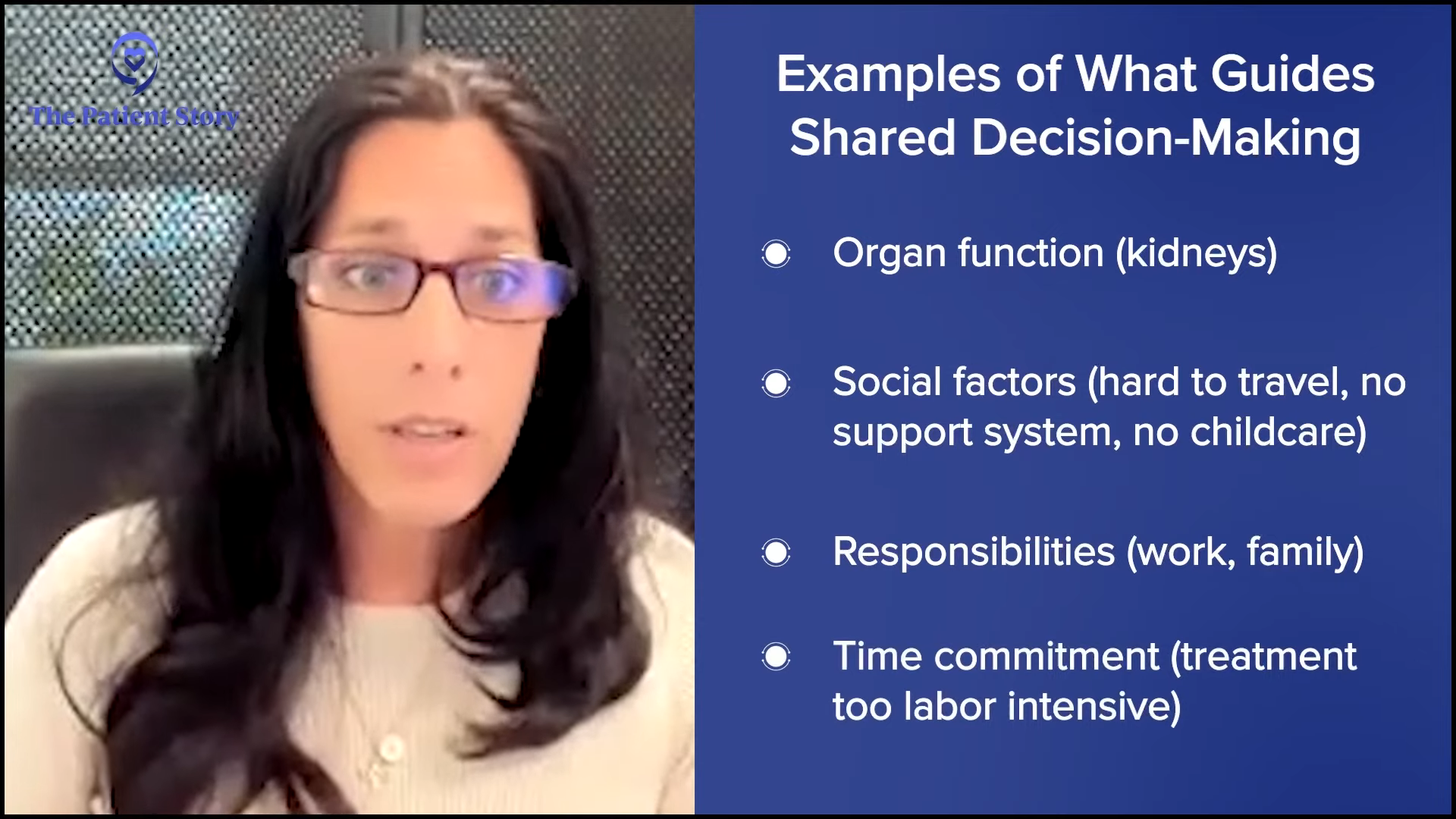
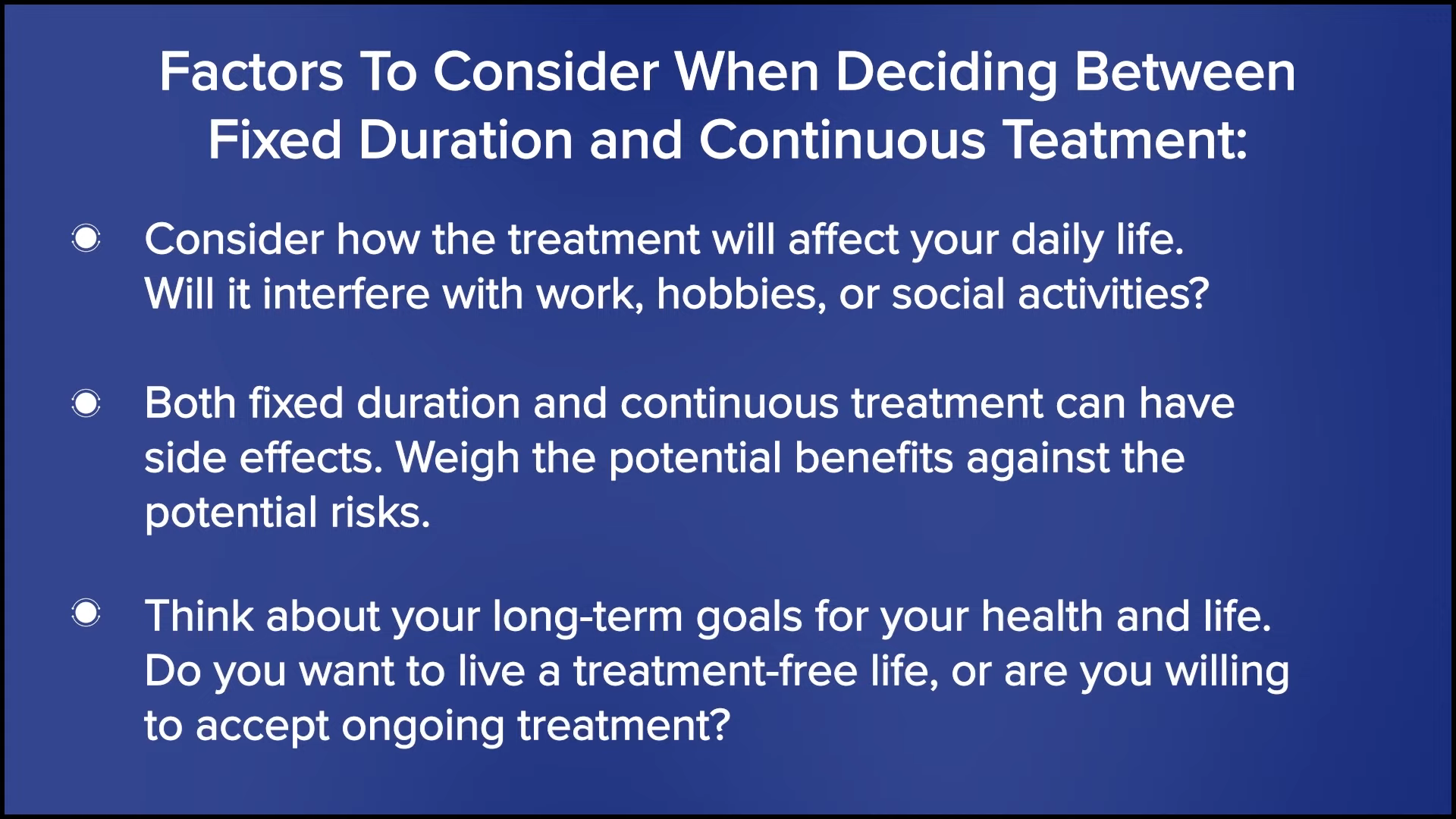
We take all of those into consideration and that’s where shared decision-making comes into play when we talk about either BTK inhibitors or venetoclax-based therapy. What are the choices in that person’s life at that particular time? Some people might have little kids and are busy and active, so they need something simple and not going to be too labor intensive. Other people may choose something different and go for more intensive therapy because they can put in the time.
We do shared decision-making because these treatment options are slightly different. They’re both great treatment options. Even though many people will wind up potentially using both of these options during their lifetime, what may be relevant for them at this particular moment in their life may be different later on down the road. That’ll come up again when you talk about relapse or needing more therapy.
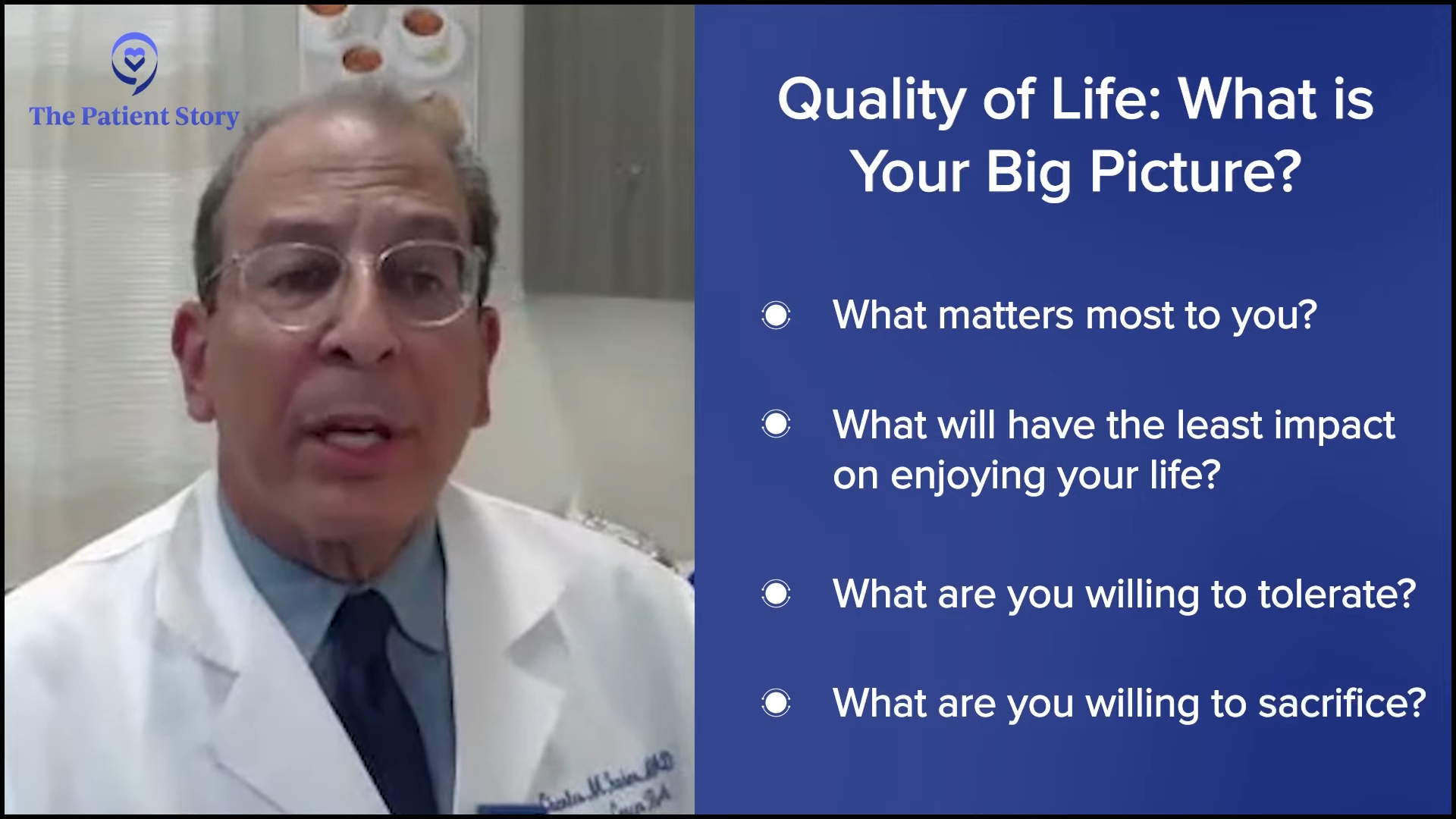
Balancing Treatment and Quality of Life
Michele: Dr. Farber, quality of life is an important factor for all patients when considering treatment options. How do you balance the potential benefits of treatment with the impact on a patient’s daily life?
Dr. Farber: It’s a very complex equation. I saw a physician newly diagnosed with a low-grade lymphoma. I asked him if he was retired, about his personal life, and what he enjoys doing. He was with his wife and family. The wife interrupted and asked, “Why are you asking these questions?”
I told her it’s very relevant in terms of the big picture. What are the goals of treatment? What’s the lifestyle of the patient? What are they willing to tolerate? How temporary is the initial treatment? Is it a phase? Some of the medicines require more intensive monitoring before things get better, so the questions are very important.
Quality of life is a very important issue and one of the more important variables in the treatment equation.
Dr. Charles Farber
Quality of life is life. Whether someone is willing to sacrifice, people want to live longer and better, and what they’re willing and able to tolerate and for how long has to be assessed. It’s a very complex equation and with these many variables, it needs to be explored.
What are the goals of therapy? Is it to make you live longer? Is it to make you live better? What are we trying to achieve? What are the treatment options? What are the side effects? Quality of life is a very important issue and one of the more important variables in the treatment equation. Shared decision-making is critical where you can’t do for the patient what you think is important. It has to be a dialogue.
Michele: All this is music to my ears because when I was on frontline treatment, my quality of life wasn’t so great, but at that point, there were no choices. We are so fortunate to have these choices now and that we can have a better quality of life as CLL patients.
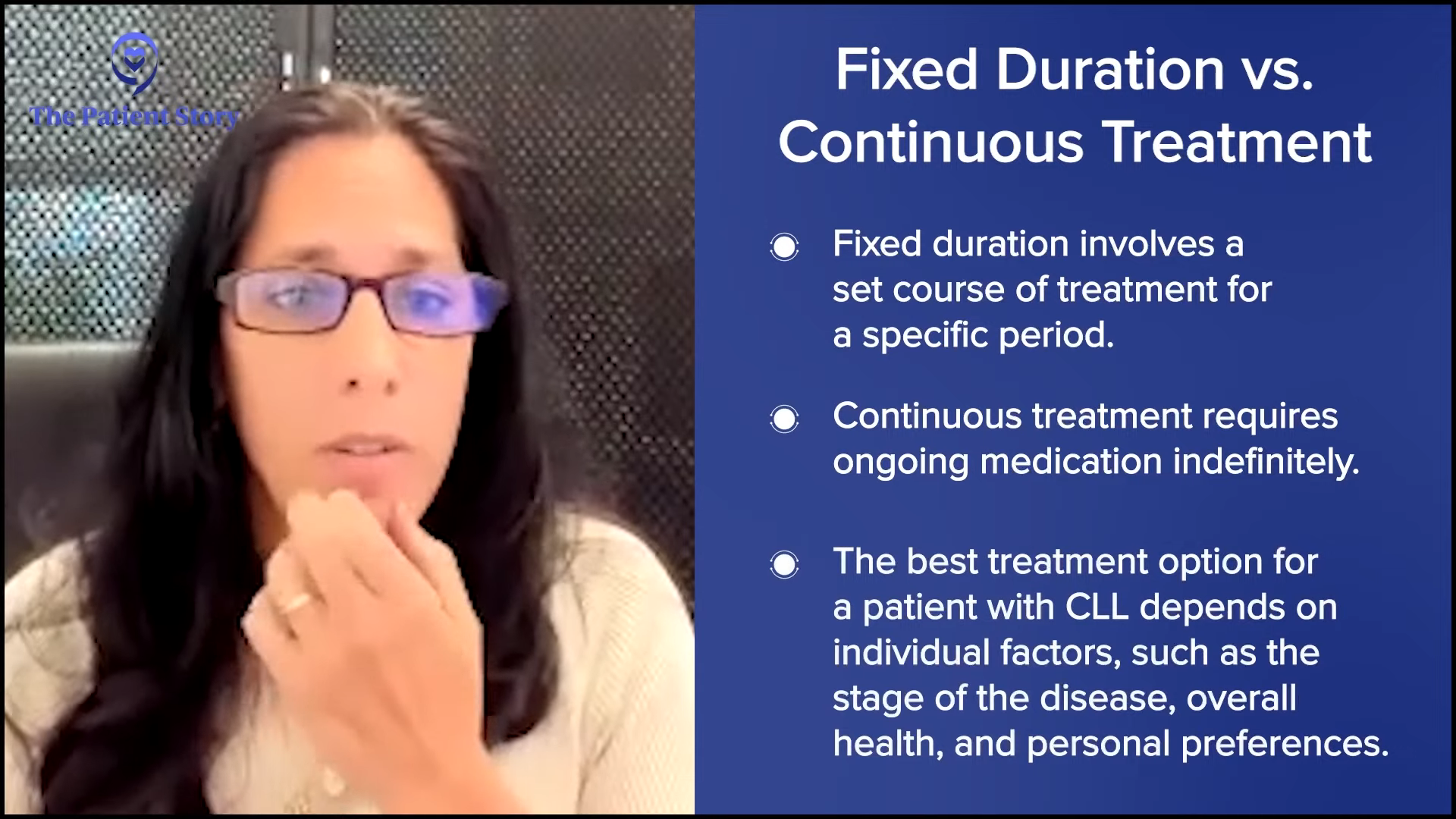
Approaches to Treatment
Michele: Dr. Lamanna, what are the potential advantages and disadvantages of a fixed-duration treatment versus a continuous treatment?
Dr. Lamanna: Both treatment options are great and because we have these excellent options, we talk about the logistics, the advantages and disadvantages of going for either approach, and then we align that with what’s going on with the patient at the time in their life.
Unless there’s something glaring, like a comorbidity or medical problem where I think one drug might be better than another, then I’ll still discuss both agents, but I’ll bring up my concerns and what I think they should do. You have these discussions and factor in what their wishes are.
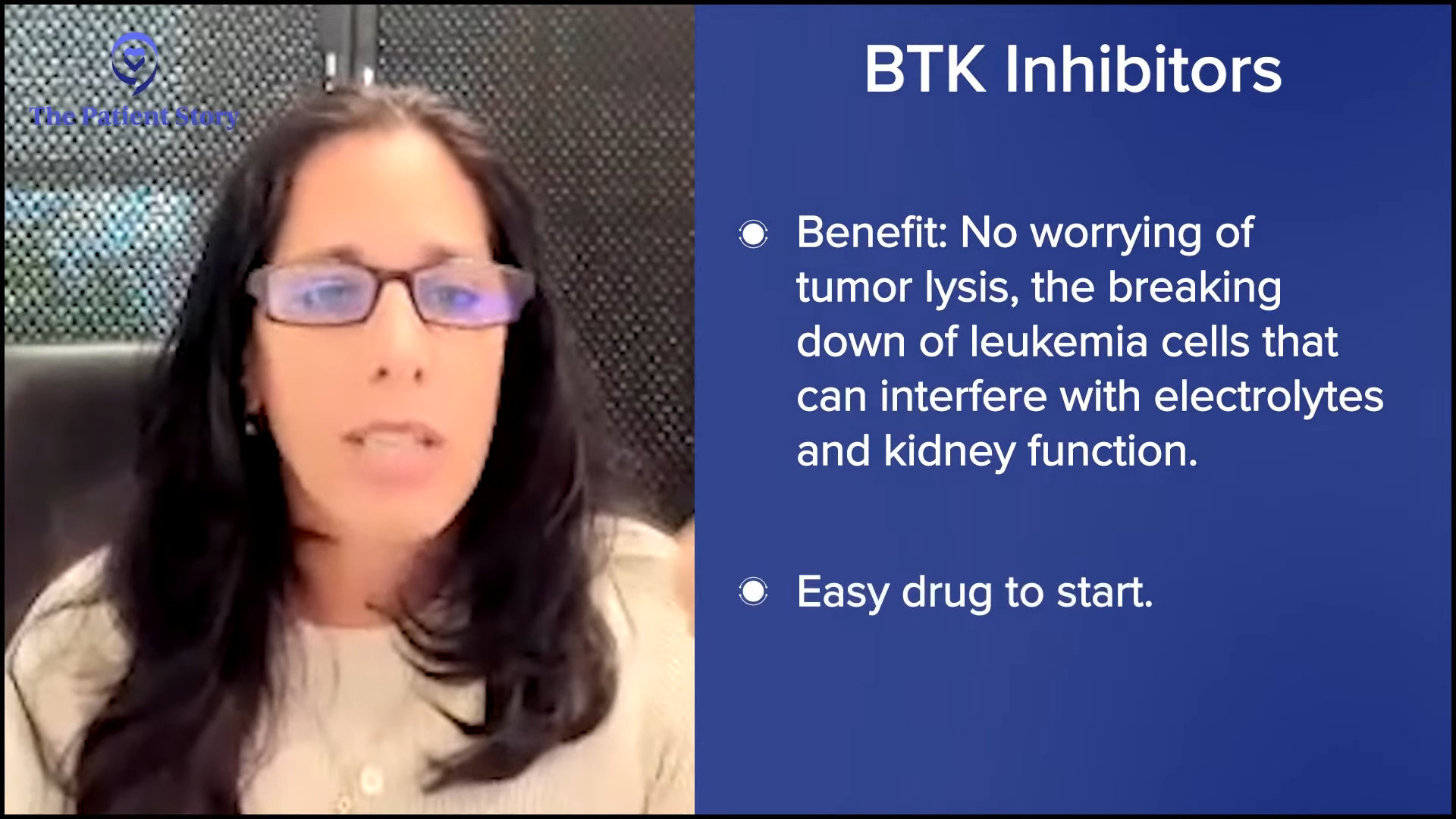
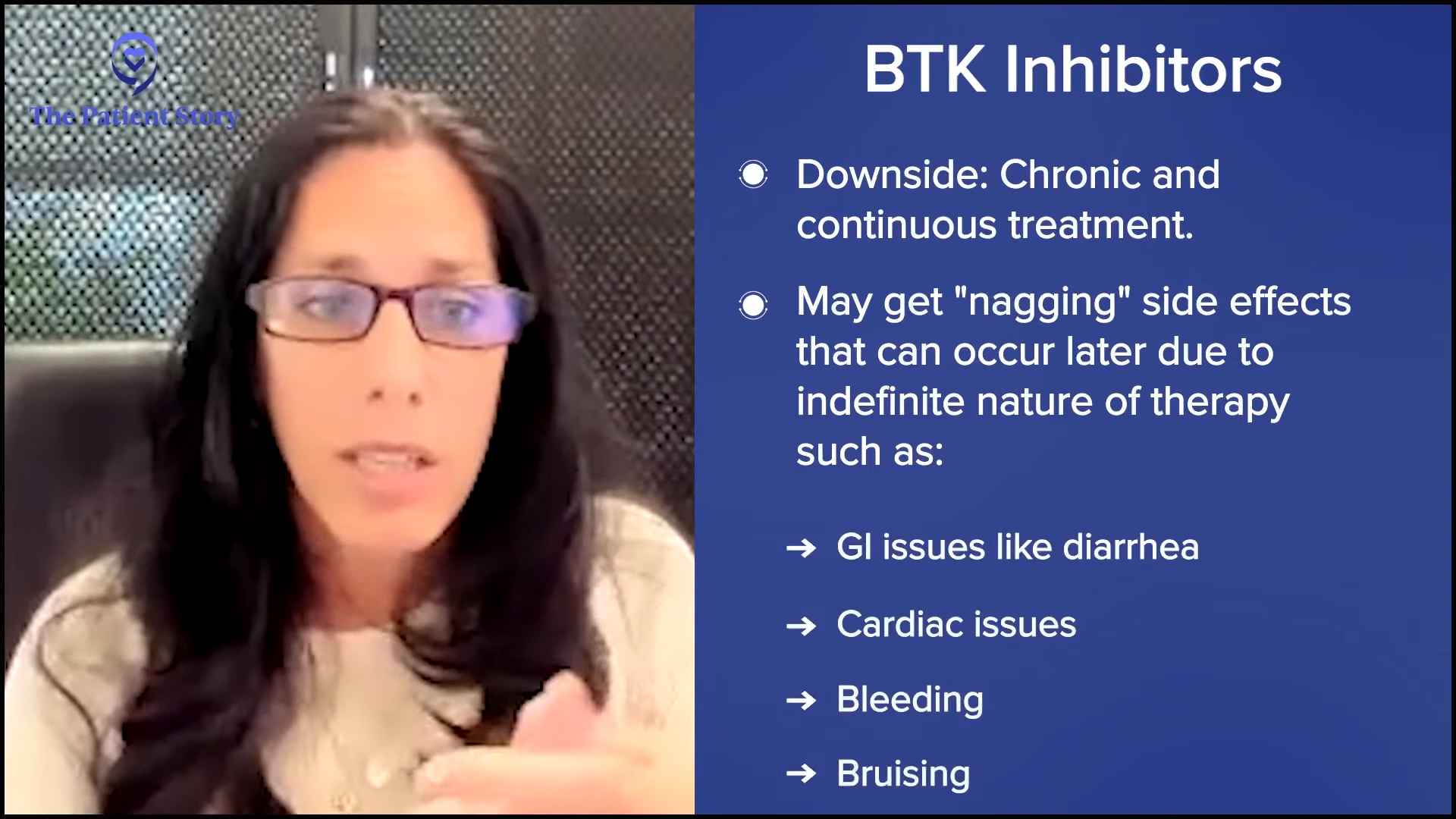
We teach everybody that if you’re taking BTK inhibitors continuously, some of these nagging side effects can occur later because you’re taking this indefinitely unless you have a side effect or your disease progresses. The downside is you could have some uncomfortable side effects, like diarrhea, GI issues, cardiac issues, bleeding, and bruising.
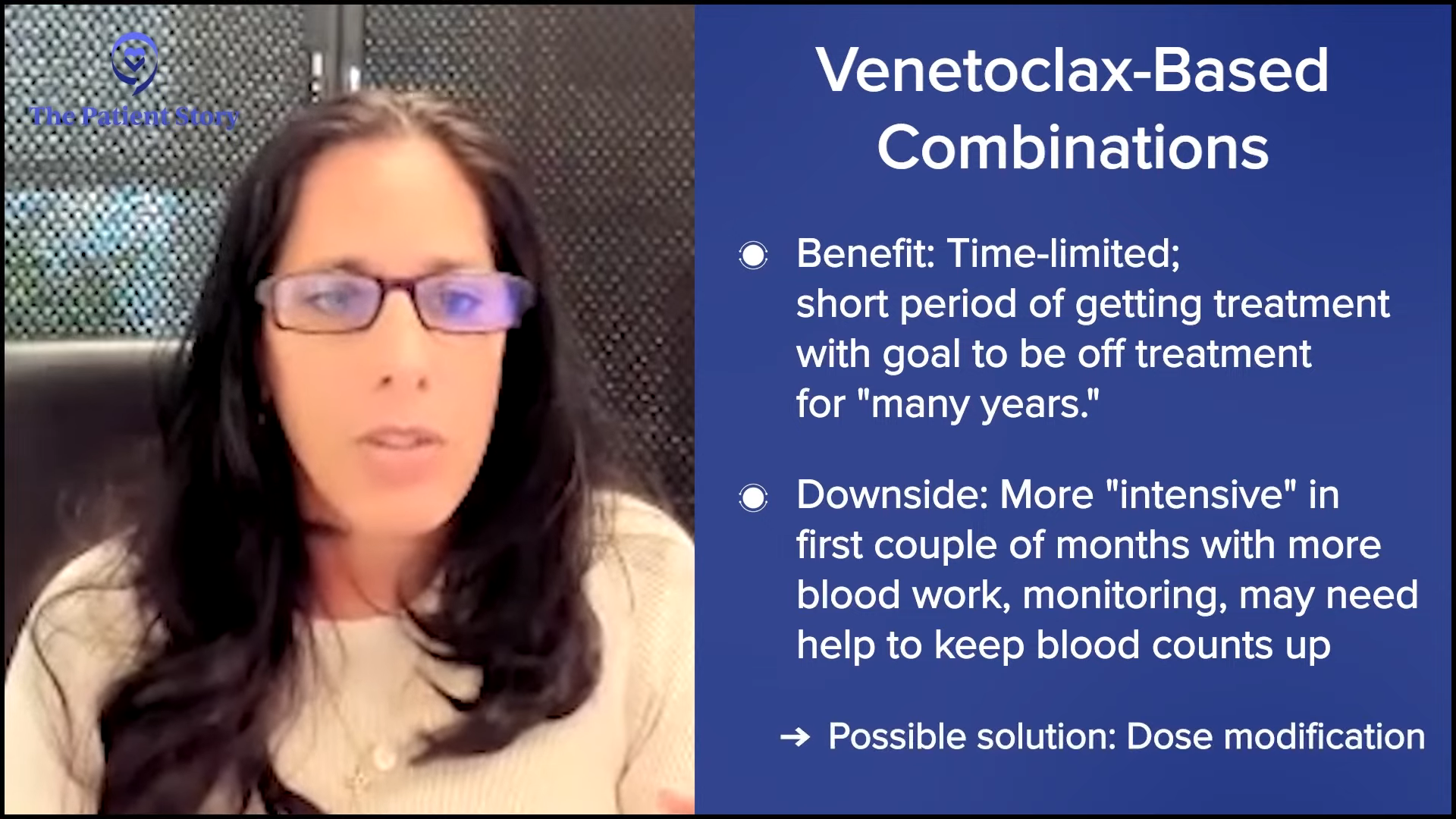
The benefit of venetoclax-based combinations is that it’s time-limited. It’s very similar to what we used to do with chemoimmunotherapy where you’re getting a short duration of therapy and hopefully won’t need to be on treatment until many years down the road.
The downside is that it’s more labor-intensive in the beginning. There’s a lot of monitoring because your blood counts can fluctuate a little bit more commonly with the combination. Sometimes you need extra help. They might have dose modifications. There are different logistics with a time-limited approach that people have to be willing to commit to, but the advantage is you get a break from therapy.
I have both of these conversations with patients because it is rare to say that somebody is precluded from one regimen versus another and that’s why most patients have an option. There might be some circumstances based on comorbidity, cytogenetics, or other issues that I’m concerned about with where I might recommend one approach versus another, but we have that dialogue.
Michele Baker: Dr. Farber, is your approach different and if so, how?
Dr. Farber: No, it’s very much in line with Dr. Lamanna’s. I would echo what she said that BTK inhibitors are very easy to start and hard to continue whereas the BCL2 inhibitor venetoclax is very cumbersome to start and requires a lot of initial monitoring. The patient has to come in very frequently for lab work and hydration as we’re ramping up, but it’s easy to continue.
Treatment has to be individualized. There may not be a perfect treatment, but one clearly may be better than another.
Dr. Charles Farber
With ongoing treatment versus finite treatment, the majority of people would like to be treated with finite therapy for one or two years, but that’s not for everyone. It’s a little counterintuitive, but some people feel very comfortable being treated with ongoing therapy because they feel like they’re proactively being monitored and treated.
A lot of people panic when it comes to the end of the year or two years on venetoclax and they become concerned about what we’re going to do next. It’s not broken. Why do we want to fix this? What’s wrong with continuing with venetoclax?
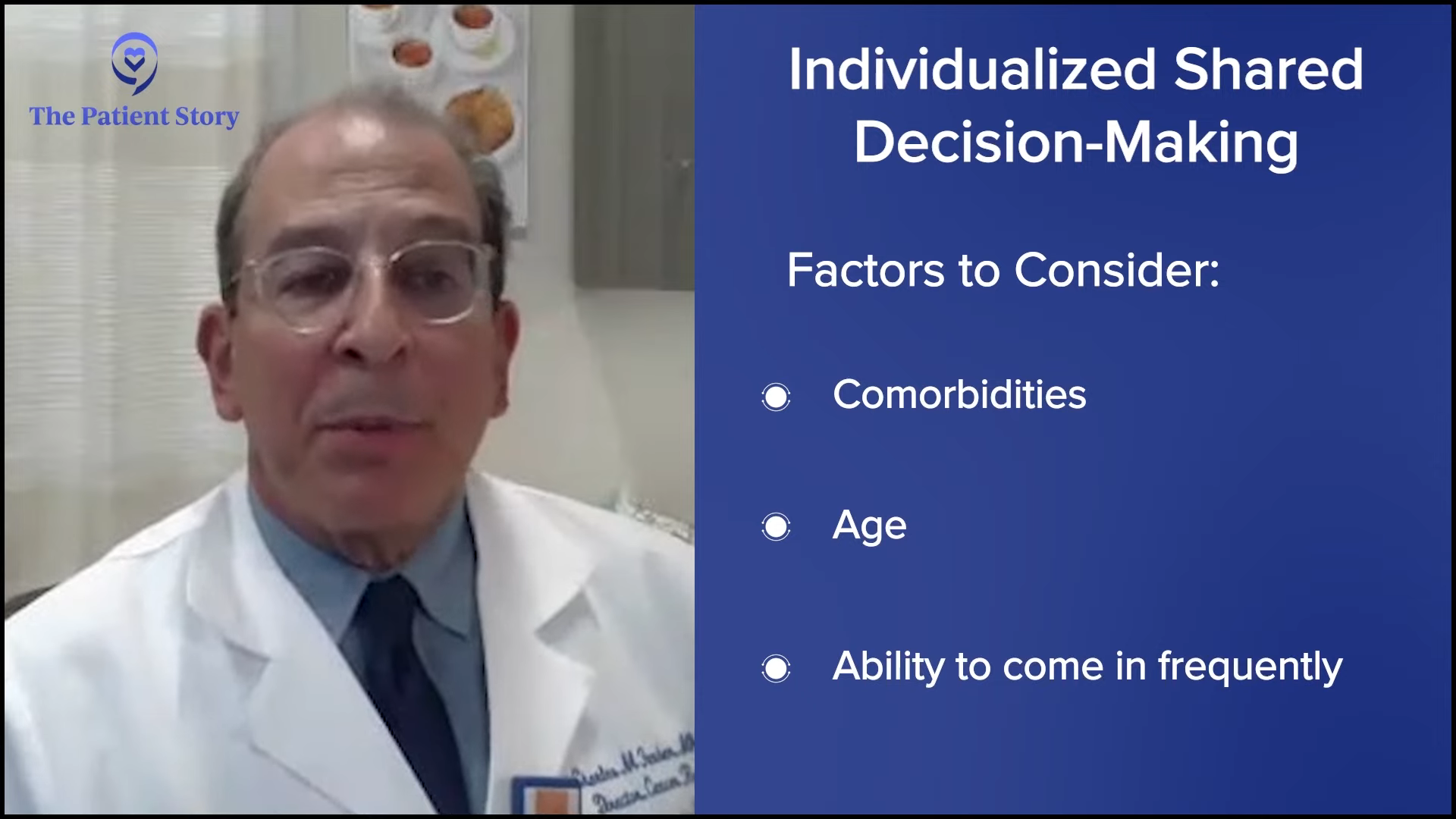
Shared treatment decision-making is individualized. Comorbidities, age, and ability to come in frequently in those first few weeks may dampen my enthusiasm for venetoclax in certain individuals. If they’re on an anticoagulant or blood thinner, I worry about that with BTK inhibitors.
It’s truly a situation where the treatment has to be individualized. There may not be a perfect treatment, but one clearly may be better than another. There’s a lot of information. CLL patients tend to be older and have comorbidities, so Michele, you are quite the exception. But you do the best you can. It requires a lot of patience, but it’s very gratifying.
We’ve had amazing treatments historically. If you look back 10 or 15 years ago, it was prehistoric, particularly for patients at higher risk with unmutated, immunoglobulin-heavy chains or TP53. We had no treatment until the advent of ibrutinib. It’s a very gratifying time to be in practice where we have options and we can talk to patients about what may be better for them.
Bridging the Gap: When Patients and Doctors Disagree on Treatment
Michele: What happens when a patient and their doctor have differing views on a treatment plan’s next steps? What do you do?
Dr. Farber: To some degree, the patient’s always right. If you feel they’re taking a misstep and if it’s not a horrible misstep, you voice your concern. If it’s something terrible to you, tell them you’re not willing to do it or perhaps they should seek an additional opinion. You try to resolve it.
The C in CLL is chronic. If they want to take ivermectin or something unproven, you try to educate them. You try to intellectualize. But it could be difficult because some patients get an idea and it may not be a good idea, but they feel very strongly about it.
If it’s something you’re uncomfortable doing, you can try to excuse yourself and offer a second opinion. It could be challenging and some patients get offended when you don’t do exactly what they’d like you to do. They could come at you with something from Dr. Google that isn’t necessarily appropriate. You have to be calm and try to explain the rationale for why you think it may not be a great idea.
Michele: What you would say to someone exactly if they brought up ivermectin?
Dr. Farber: I tell them that there have been anecdotal reports of patients doing well with various diseases, but that’s not scientific and doesn’t prove that ivermectin is effective in a given setting. I explain about randomized prospective trials. The best way that this is done scientifically is to take a group of patients and divide them into two or more groups. One group is treated with the test agent and the other is treated with standard therapy, placebo, or under observation. The true scientific way is if the group that gets ivermectin does better, lives longer, has a better quality of life, and has objective improvements in their labs or radiographs, that is scientific.
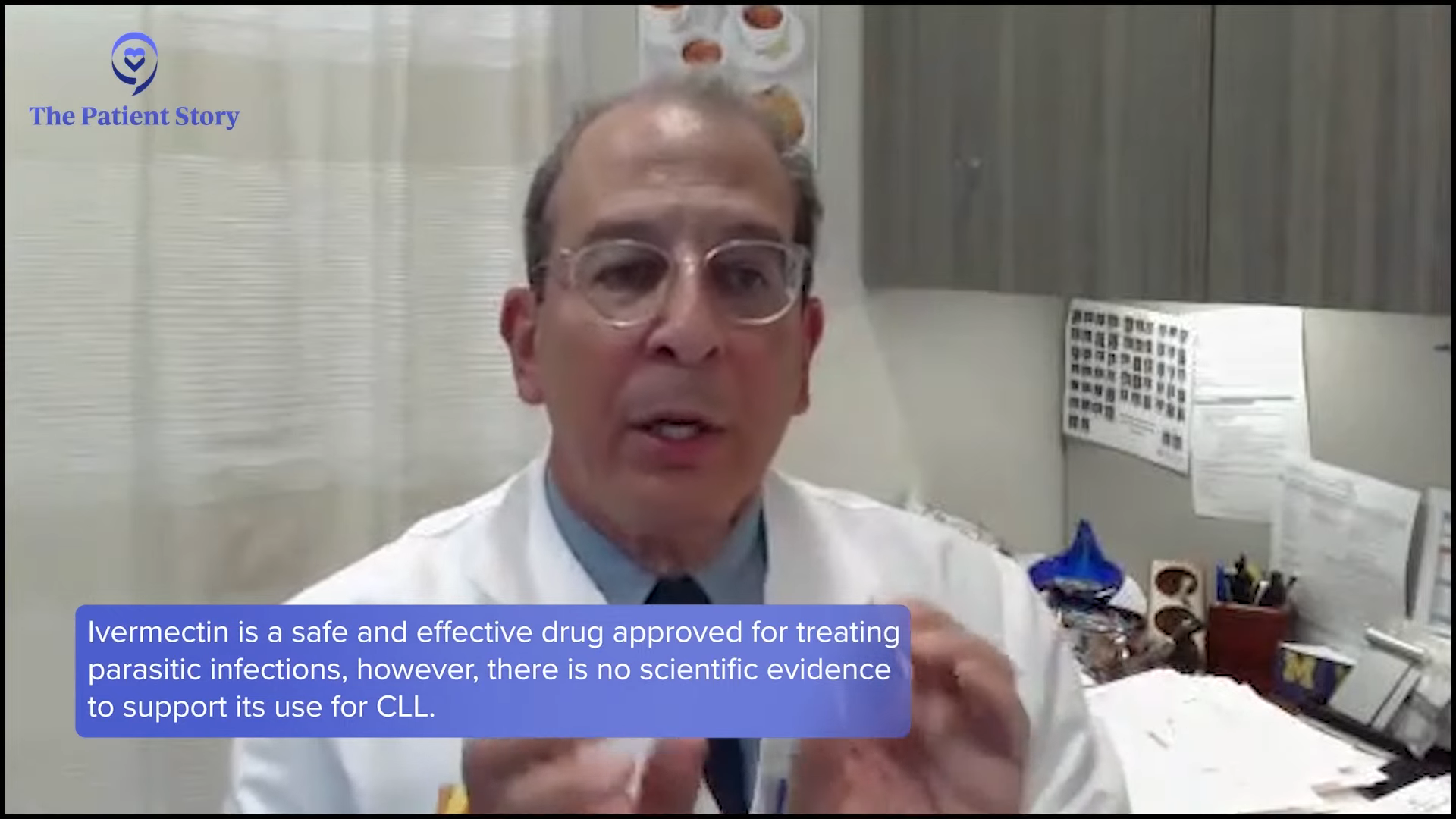
Sometimes in CLL and other diseases, there are spontaneous remission improvements. Single cases of patients getting better is akin to snake oil where someone comes up and endorses a treatment. That’s what I would I would try to explain. I try to explain that individuals getting better on ivermectin is not akin to a randomized prospective trial showing clinical benefit.
Michele: You’re very polite with your explanation and what you would say to someone about ivermectin. I appreciate that. Dr. Lamanna, what would you do if you and a patient disagree about what their treatment plan will be and their next steps?
Dr. Lamanna: To be fair, it is a dialogue. I’ve been fortunate that there aren’t many patients who I’ve had real troubles with. Thankfully, many patients either want to hear the whole discussion or read and bring up their questions with me and that helps the dialogue because you hear where they’re coming from.
If people bring up things that are completely not standard of care, then I have a discussion with them on the standard of care and about supplements or alternative medicines and how to integrate those into current practices or therapies that might be needed for their leukemia.
If somebody doesn’t want to take any standard of care treatment, then I’m probably the wrong person for them. It’s not difficult to have that conversation because either the patient is a right fit and doesn’t want to have anything, is afraid to take any kind of standard of care therapy for CLL, and that’s very easy to have the discussion and see where they want to take that.
Another conversation is when people get multiple opinions from different doctors. We see patients who talk about different therapies and they’re usually talking about all the standard of care therapies. The discussion now shifts to treatment sequencing. Should they do this one first or that one first?
Another discussion is talking about the different clinical trials and that’s great because that’s an open dialogue and right up my alley. I’m happy to talk about any of that, share my knowledge and expertise, and come to a mutual agreement if they want to do one or another, whether with me or someone else. I’ve never had too many difficulties where we’ve disagreed or where it’s been not approachable. It’s something that we have a conversation about.
You want to partner with a doctor and a team that fits you. I may not be the right person for that person all the time and that’s okay. I respect that.
Dr. Nicole Lamanna
I always say to patients that because CLL is a journey, you need to find somebody that you feel comfortable partnering with. That may not be me and that’s okay. It’s a long journey and they’re with you for a lifetime. You hope that they’re with you for 20-plus years or more. Hopefully, they will have a normal lifespan. That’s what we’re shooting for with all our research. You want to partner with a doctor and a team that fits you. I may not be the right person for that person all the time and that’s okay. I respect that.
Michele: It’s a long-term relationship and it’s important that you and your doctor gel. I always say it’s almost like dating, trying to figure out who’s right. My relationship with my CLL specialist is probably one of the longest I’ve had; not quite as long as with my husband but almost.
Beyond Initial (Frontline) Treatment
Michele: Let’s move forward to second-line and third-line therapy. Dr. Lamanna, what factors do you consider? Are they different when selecting a second-line therapy and planning for future treatment options?
Dr. Lamanna: This is a journey. Although most patients are focused on their first treatment and what they’re getting at that moment, I’m always thinking about their next lines. The goal is to try to think ahead.
What they got in the frontline and what their response duration was to that therapy will play a role in what they’re going to be recommended in the second or third line.
Dr. Nicole Lamanna
In the second or third line, you consider several factors. What did they get in the frontline? Have the genetics of their disease changed? Were they once a favorable risk and now changed to 17p deletion or TP53 mutation? How did they tolerate their first regimen? Do they have new comorbidities or new medications that we have to be concerned about? What they got in the frontline and what their response duration was to that therapy will play a role in what they’re going to be recommended in the second or third line.
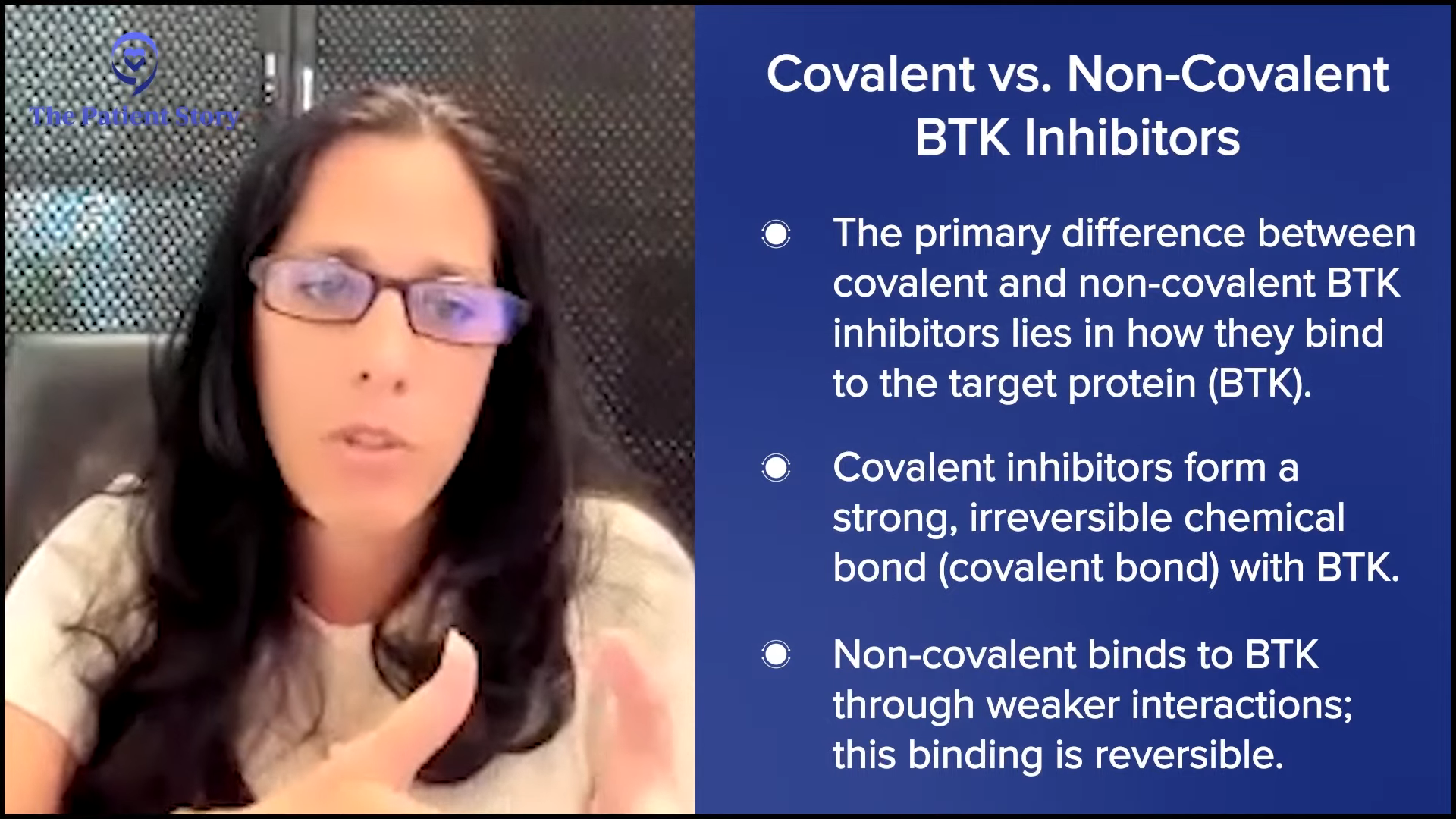
If they got a time-limited approach with a venetoclax-based regimen, like venetoclax-obinutuzumab, how long did that last? Was it short? Was it long? Did they tolerate the regimen? Is that something we can reconsider? If they were on a BTK inhibitor for their frontline treatment, then we’re not going to offer them another covalent because most people at this point have gotten covalent BTK inhibitors in the frontline.
How to sequence these drugs is still being evaluated. The point is it’s important to know what they had for frontline therapy.
Dr. Nicole Lamanna
If they’re continuously taking a medicine, you’re not going to switch them to the same class of covalent BTK inhibitor. You’ll likely go to a venetoclax-based regimen. We have a non-covalent BTK inhibitor, pirtobrutinib, which recently got approved. How to sequence these drugs is still being evaluated.
The point is it’s important to know what had for frontline therapy, whether their genetics changed, if they have any new comorbidity, what their response was, and if they had any major side effects. All of those play a role in determining second and third-line therapy.
The Role of Genetics in CLL
Michele: Dr. Farber, this is something that CLL patients are always asking. I had my test when I was first diagnosed and this is what it showed, but now they’re showing something else. What happens to our genetics? Is it from treatment?
Dr. Farber: Yes, genetics can change. If you look at newly diagnosed patients who’ve never been treated, perhaps 5% or 7% will have a TP53 mutation or 17p deletion whereas if you look at populations of patients who were very heavily treated, particularly with chemotherapy drugs, up to 50% of those patients will have the dreaded TP53 mutation or 17p deletion.
If a patient needs a new line of treatment or is having progressive disease, if they haven’t had genetic testing, they should be checked
Dr. Charles Farber
By treating, you do one of several things. You can introduce new mutations or at least select a population of cells that have that mutation. What’s very important is if a patient needs a new line of treatment or is having progressive disease, if they haven’t had genetic testing, they should be checked again because there may be something emerging that was not there or not recognized earlier. There are a variety of different assays used, like FISH and next-generation sequencing.
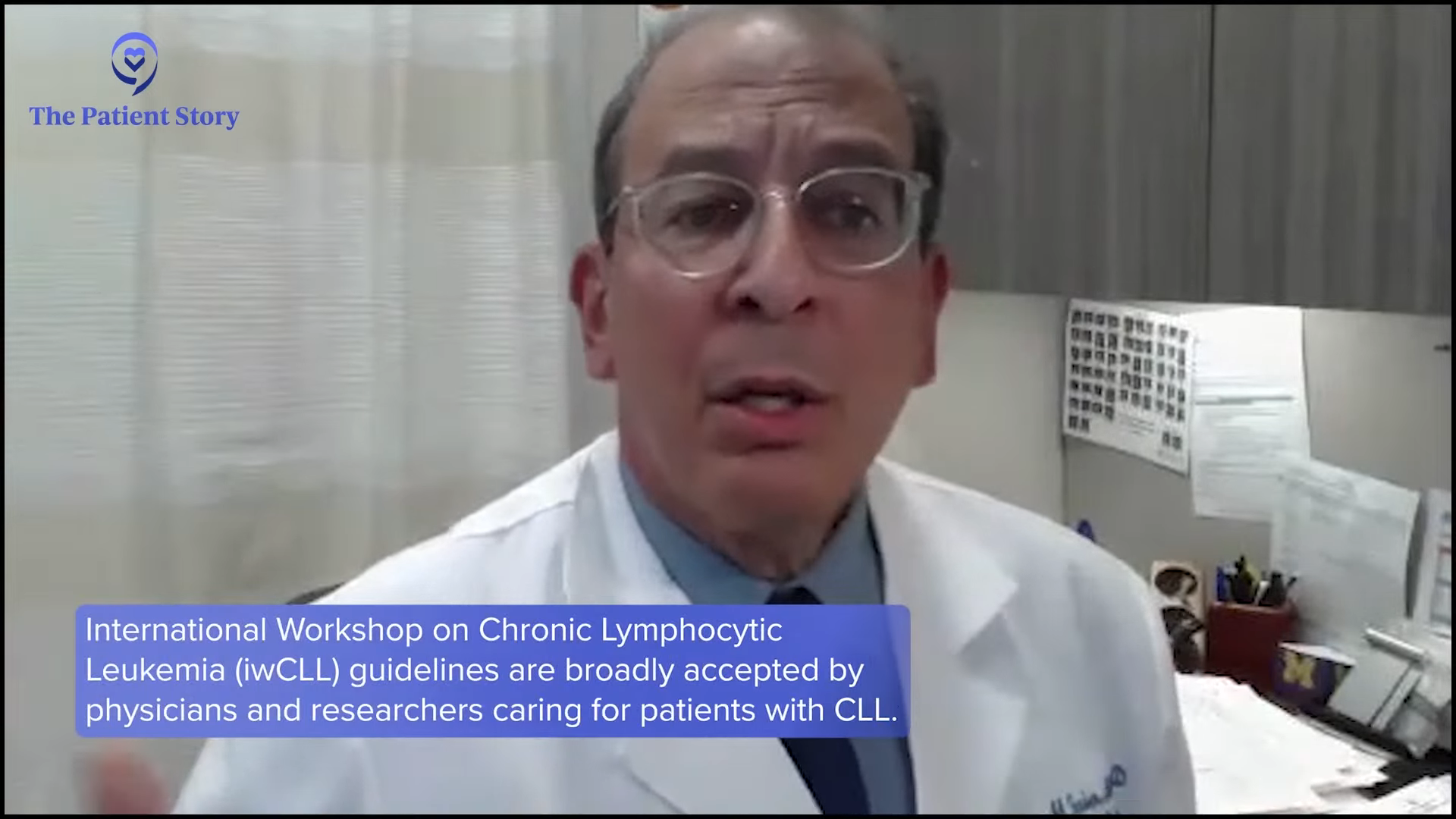
It’s not the same biology through the course of the disease in a given patient. It can sincerely change in part through treatment and that’s one of the reasons in general that we tend to try not to treat patients until they need treatment. The International Workshop on Chronic Lymphocytic Leukemia (iwCLL) has criteria for who needs treatment and not everyone needs treatment.
They say there’s no benefit to treating early. I would take it a step further. There may be a detriment to treating a patient before they need treatment. It’s like shooting off your ammunition before the war begins. Some are seldom accused of starting treatment before an individual needs treatment. If a patient hasn’t had a genetic profile of their disease done in recent times and they progress, they should be checked out again.
Key Takeaways
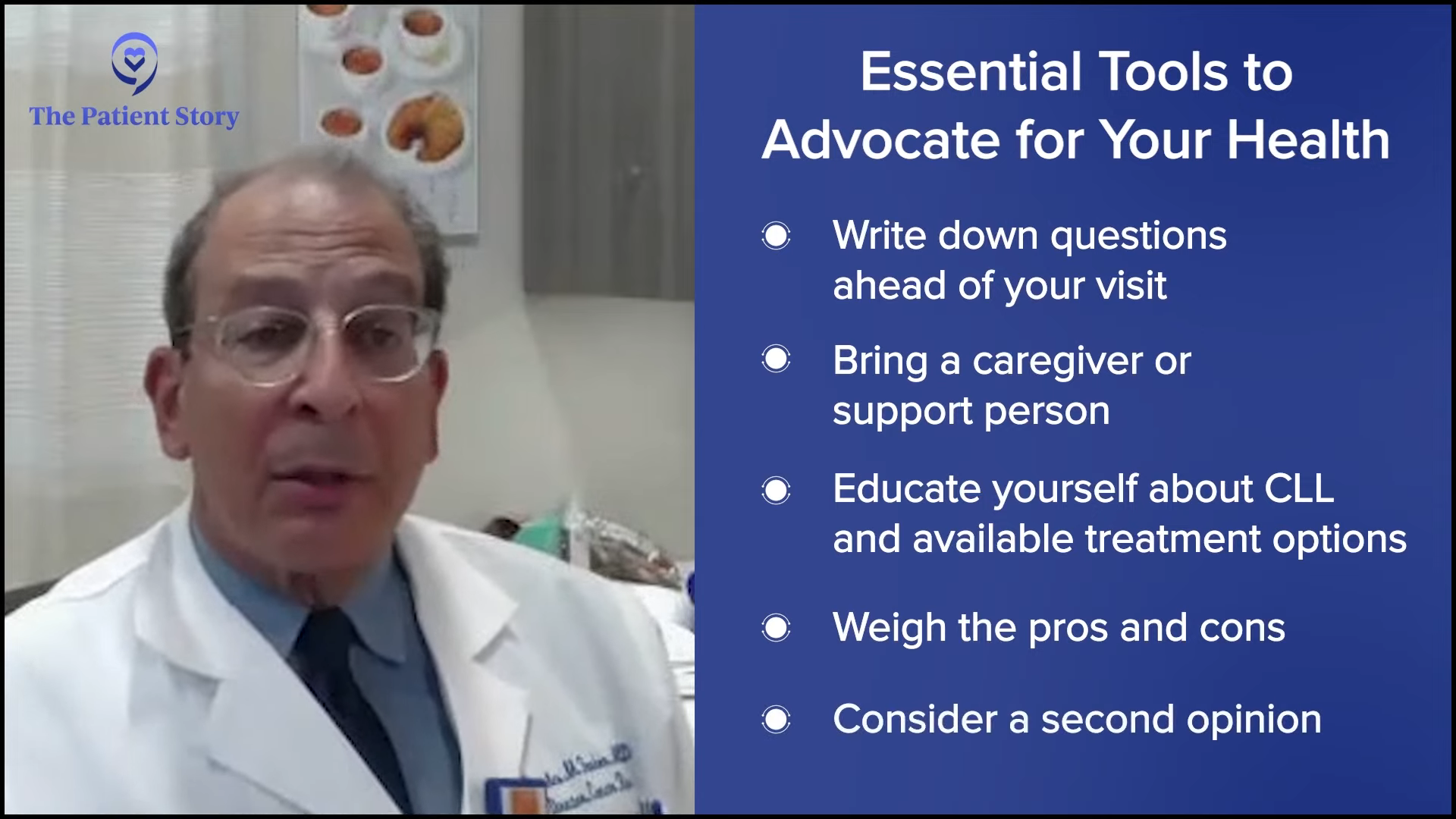
Michele: What is your advice to patients? How can they most effectively advocate for themselves and have shared treatment decision-making conversations with their doctors, especially when they’re so overwhelmed with the amount of information they’re getting? How can they advocate for themselves when their doctor is not looking at newer therapies, like if they’re in a rural community and don’t have that advantage?
Dr. Farber: The patient needs to bring their spouse, a relative, or a loved one to review what the doctor’s saying at one of these critical junctures. It’s important to write things down.
When all is said and done, the patient can come up with a little chart where they can see the pros and cons of a treatment. You might have one for each different treatment being offered to you. Listen carefully to the doctor.
Come up with very focused questions. Write things down before you go in rather than having a free-for-all discussion.
Dr. Charles Farber
Ask their opinion. What do you think? Do you think one is better than the other? Do you think they’re equivalent? What aspects of one treatment would be better than another treatment? What aspects would be inferior? Are there any nuances to my current medical state that might make one treatment better than another? Come up with very focused questions.
Write things down before you go in rather than having a free-for-all discussion. Back in the day, we didn’t have options. There was one best treatment and we could change the dosing and the schedule to try and finesse it, but now we have different options. We have different agents within a given class. The doctor and the patient must come up with a good plan for the individual.

Dr. Lamanna: It’s often good for patients to bring somebody to their appointments because it’s hard to hear everything with one set of ears. Sometimes what the patient might be focusing on is different from what their loved one or friend might be. They may hear other aspects of the conversation.
The beauty of CLL compared to other cancers is we can have multiple conversations when we’re gearing somebody up for treatment. I often encourage them to write down questions and bring them to their next visit or message us. Thankfully, we have the leeway and flexibility of doing this at multiple sessions to try to answer their questions more thoroughly. That’s very rare. That’s not to say it never happens in CLL because sometimes it happens, but often, you have that luxury of time.
Thankfully, we have the leeway and flexibility of doing this at multiple sessions to try to answer their questions more thoroughly.
Dr. Nicole Lamanna
We also try to set up educational visits to go over the drugs and their side effects. There are a lot of good support groups for CLL where they can go over questions. I hook patients up early when I first meet them. I give them a book from The LLS talking about CLL and then I give them websites that they can visit. I say to patients that not everybody’s ready to go online and look at their disease. Dr. Google can be a problem, but for those who want to, I want them to go to reputable sites that talk about the disease.

Conclusion
Michele: This has been wonderful. I’ve learned so much from you. Thank you, doctors, for your devotion and dedication to helping CLL and SLL patients. We all better understand shared treatment decision-making and how important it is in our journeys.
Stephanie: Thank you so much, Michele. Thank you to Dr. Lamanna and Dr. Farber for all the work that you are doing with your patients and patients everywhere in CLL and SLL. It’s so important to be empowered again, especially in the space of this disease, which requires a lot of engagement and understanding because there’s so much rapid development happening with different therapies.
We want to thank our partners, The Leukemia & Lymphoma Society and The CLL Support Group.
I hope that you learned something from the program, that it spurred some thoughts, and that you can walk away with some actionable items on your list of things to do. We hope to see you at a future program. Take good care.

Special thanks The Leukemia & Lymphoma Society and The CLL Support Group for their partnership.
CLL Patient Stories
Lynn S., Chronic Lymphocytic Leukemia (CLL)
Symptom: Elevated white blood cell count
Treatments: Chemotherapy, targeted therapy (BTK inhibitor)
Serena V., Chronic Lymphocytic Leukemia (CLL)
Symptoms: Night sweats, extreme fatigue, severe leg cramps, ovarian cramps, appearance of knots on body, hormonal acne
Treatment: Surgery (lymphadenectomy)
Margie H., Chronic Lymphocytic Leukemia
Symptoms: Large lymph node in her neck, fatigue as the disease progressed
Treatment: Targeted therapy
Nicole B., Chronic Lymphocytic Leukemia
Symptoms: Extreme fatigue, night sweats, lumps on neck, rash, shortness of breath
Treatments: BCL-2 inhibitor, monoclonal antibody




