CLL: The Latest in Treatment and Research
What Patients and Caregivers Need to Know

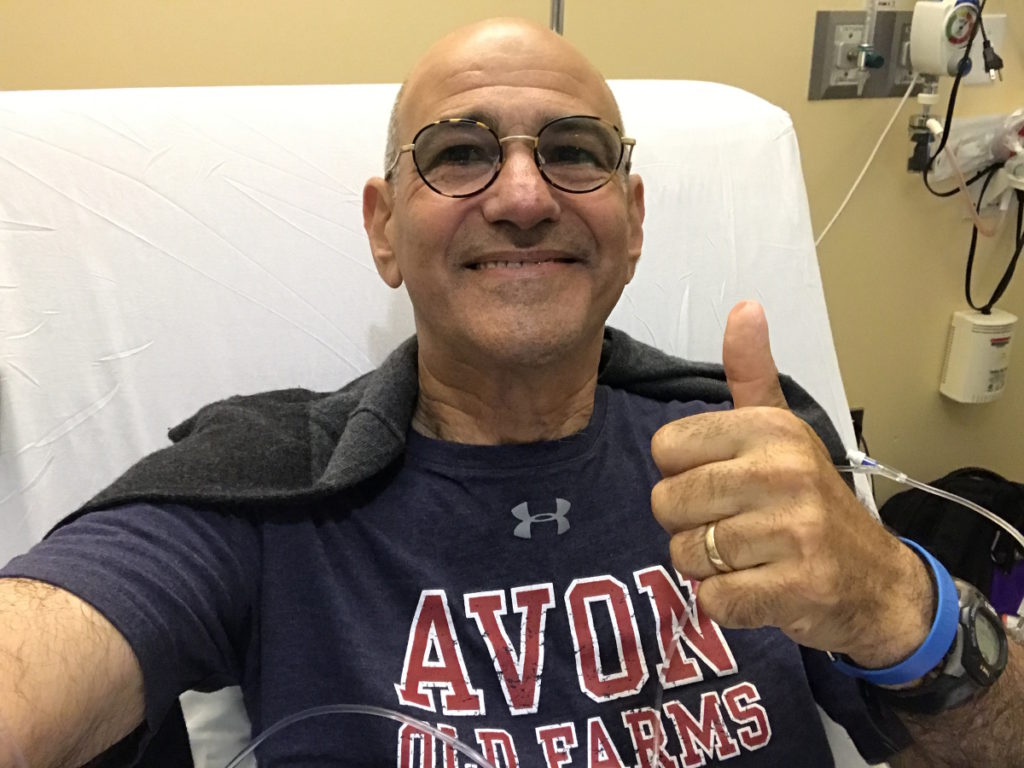
Chronic lymphocytic leukemia patient advocate Andrew Schorr has been living with CLL for 26 years.
In this conversation, he talks with hematologist-oncologist Dr. Nitin Jain from the MD Anderson Cancer Center who specializes in patients with CLL and ALL.
They discuss the latest treatment and developments in CLL coming out of ASH 2022, the annual meeting of the American Society of Hematology.

This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- BTK inhibitors: choosing the right drug for the right patient
- Ibrutinib
- Venetoclax + ibrutinib
- The importance of getting an infusion vs. oral medications
- What is the advantage of a third-generation BTK inhibitor?
- New data on Richter’s Transformation
- CAR T-cell therapy
- Chronic Lymphocytic Leukemia Patient Stories
BTK inhibitors: choosing the right drug for the right patient
Andrew Schorr: With us is one of my favorite CLL researchers and experts, Dr. Nitin Jain, from MD Anderson.
Patients like me have lots of questions. We hope we can live a long, full life with CLL. You have more options than ever before.
One of the areas is BTK, Bruton tyrosine kinase inhibitors. We have Imbruvica, acalabrutinib or Calquence, [and] zanubrutinib that may be approved in CLL before long but is used in some other conditions. These drugs have made a big difference for people. What [do] we know about them now and how [do] you choose which one is right for which patient?
Dr. Jain: BTK inhibitors are oral drugs. They target a specific protein called BTK on the CLL cells.
The first one was ibrutinib. The second-generation ones are acalabrutinib and zanubrutinib. Zanubrutinib is not yet approved for CLL, but we are expecting it to be approved pretty soon, maybe in the next couple of months.
There’s a third-generation BTK inhibitor called pirtobrutinib, which is not yet FDA-approved, but it’s on track and there’s a lot of data presented about this drug.
Currently, FDA approved for CLL are two BTK inhibitors: ibrutinib and acalabrutinib. In terms of deciding which drug to choose between these two, for my patients, I really look at the efficacy and safety profile of these drugs.
There are a couple of trials done in patients with relapsed CLL, [those] who had prior therapy for their CLL then their disease came back. Half of the patients were given acalabrutinib [while the other] half of the patients were given ibrutinib.
What those studies showed is that those drugs were equally effective but acalabrutinib [had] less toxicity. Based on that and some other data, I preferentially [use] acalabrutinib these days as the BTK enabler of choice for my patients.
Again, that argument may change a bit when zanubrutinib comes [into] the picture, and certainly down the line when we get pirtobrutinib. That would be another exciting addition to the field of BTK inhibitors.
Andrew: Okay, so that’s really going to be physician and patient choice, it seems. They’re all good drugs.
Dr. Jain: It will come down to the physician, how comfortable they are using a particular drug for their patients, and the medical data and how they look at it.
I present all these options to my patients, discuss some of the clinical trial data and big picture view, give my recommendations to the patients for the treatment, and follow what their wishes are.
Andrew: Then also in this discussion is what other conditions a patient might have, right? Do they have a heart condition or other things that would determine which medicine you might go with, correct?
Dr. Jain: You’re absolutely correct. One of the things we [are] concerned about is the side effect profile. Some side effects are bone aches, muscle aches, diarrhea, and skin rash. [They] certainly can be an issue and some patients require dose reductions, especially for ibrutinib.
Some things are somewhat less common but can be more serious, such as atrial fibrillation, which is an abnormal rhythm of the heart, hypertension, which can become a problem for some patients, or bleeding issues.
If a patient has some of those medical conditions ongoing — heart issues, recent heart attack, or heart rhythm issues — then many times, I try to stay away from BTK inhibitors and use venetoclax, which is a Bcl-2 inhibitor. Among the BTK inhibitors, that will really make the case for second-generation agents, which are less toxic in terms of cardiovascular side effects.
Andrew: There’s data coming out related to zanubrutinib, not yet approved, but whether there are [fewer] concerns related to that for some patients, am I right?
Dr. Jain: Yes, correct. Similar to acalabrutinib, zanubrutinib was also studied head to head [compared] to ibrutinib in relapsed CLL. In that study, they showed that there was less atrial fibrillation with zanubrutinib compared with ibrutinib. That’s the first time two BTK inhibitors were compared head to head and they’re also showing that one is more efficacious than the first.

Ibrutinib
Andrew: Let’s just talk about the one that’s been around a long time: ibrutinib. There are thousands and thousands of patients on it. If they’re doing well, there is not necessarily a reason to change, right?
Dr. Jain: I agree with you and I think that’s a very important question from a patient standpoint. I get asked this question all the time in the clinic because ibrutinib certainly was the first drug [on] the market. It really changed how we manage these patients and really dramatically improved the outcomes of our patients.
But now, we are seeing some side effects of these drugs. There are patients who have been on ibrutinib for years and years — five years, seven years, nine years — and they are tolerating the drug well, [with] no side effects, [and] disease is well controlled.
I’m not switching those patients to a different agent at this time. We continue to use ibrutinib. However, if they’re starting [to get] side effects, then we look into moving to a different agent.
Andrew: There’s a significant percentage of CLL patients who are on watch and wait for an extended time. Is there any new thinking about doing anything differently now or is that still the standard in CLL?
Dr. Jain: As a CLL research group, we are investigating whether you can treat certain patients with CLL who are [at] high risk for disease progression early on, for example, patients who have deletion 17p and high-risk disease unmutated IGHV gene.
These are patients [who] we expect to progress a bit faster. Their time to treatment after CLL diagnosis is probably shorter than other patients with CLL.
There are ongoing randomized studies in the United States where patients with CLL are randomized. Either [they are treated] right away with venetoclax-based therapy or we watch these patients and whenever the disease progresses, which could be several years down the line, at that time, they receive venetoclax-based therapy.
That’s an ongoing and very important trial in the field. We’ll have to wait to get that medical data.
The current standard remains the same. We should watch these patients until they meet our CLL treatment criteria, which is basically having low blood counts, low hemoglobin, low platelets, big spleen, big liver, big lymph nodes, or significant symptoms from the disease affecting [their] quality of life. If you meet those criteria, then we treat [you].
Venetoclax + ibrutinib
Andrew: We talked about single-agent therapy with BTKs primarily, but you gave a presentation with longer data on ibrutinib plus venetoclax. Tell us about that and whether that combo has promise for people.
Dr. Jain: Both ibrutinib and venetoclax are FDA-approved for patients with CLL. Back in 2014, our group and many other groups showed data that combining these two drugs together is actually [more] synergistic for the two in the lab. Based on that, we started this clinical trial of combining ibrutinib plus venetoclax, two oral drugs together, for patients with CLL.
We treated 120 patients at MD Anderson. These patients have never received treatment so this is the first treatment for CLL.
Almost 70% of patients achieved MRD-negative remission in the bone marrow after getting these two oral drugs. We saw very few relapses over the course of four years. Our four-year progression-free survival was 94%.
The importance of getting an infusion vs. oral medications
Andrew: How important is it to get that infusion versus these oral medicines?
Dr. Jain: That’s an unanswered question in the CLL field right now. We know that the CD20 antibody infusion, whether it’s rituximab or obinutuzumab, works very well when we combine it with chemotherapy [and] also works very well when you combine venetoclax.
There is some conflicting data when you combine rituximab with ibrutinib; it doesn’t really work that well with ibrutinib. However, obinutuzumab, which is second-generation rituximab, works a bit better when you combine [it] with acalabrutinib.
Now when we combine ibrutinib plus venetoclax together, the two most potent drugs we have for CLL, we are already seeing very high rates of remissions.
The question is: can you improve that further by adding an antibody? This is the question of doublet versus triplet. Two drugs versus three drugs.
When we designed the study, we did not elect to use the antibody because we thought [that] antibody would add more toxicity than benefit. However, there are other medical data with triplets, which [have] been reported as well.
Right now, it’s very difficult to say because all these drugs are very, very effective regimens. Doublets versus triplets, it’s really difficult to tease out if one is better than the other.
There are ongoing randomized controlled trials where they are evaluating doublets versus triplets. I’m hoping we’ll hear from some of these trials in one to two years. Then we can have a more informed decision [about] whether you really need to have CD20 antibody when you’re using these two older drugs together.
What is the advantage of a third-generation BTK inhibitor?
Andrew: You’ve mentioned pirtobrutinib, which is a third-generation BTK in trials. What would be the advantage of a third generation? How would that be different?
Dr. Jain: Pirtobrutinib, previously called LOXO-305, is a third-generation BTK inhibitor. The main advantage here is that, unlike the first two generations of BTK inhibitors, namely ibrutinib, acalabrutinib, and zanubrutinib, they bind to a very specific protein pocket.
They bind to a residue called cysteine 481S, which attaches to these drugs. These patients, when they relapse, develop resistance mutations and then these drugs cannot bind to that pocket.
However, pirtobrutinib is a non-covalent inhibitor. It does not need that residue to bind. It just blocks the pocket. That’s why it’s able to work for patients who have failed ibrutinib, acalabrutinib, or zanubrutinib. That’s one advantage that pirtobrutinib can work against patients who have failed previous BTK inhibitors.
The second advantage is safety. We have seen [an] excellent safety profile of this drug with very few patients having atrial fibrillation, bleeding complications, or any other major issues. What we know so far is that this drug works very well and it’s also very well tolerated.
New data on Richter’s Transformation
Andrew: A small percentage of CLL patients develop a much more aggressive condition called Richter’s Transformation. Is there progress being made there? Any news that gives hope in treatment for Richter’s?
Dr. Jain: Richter’s Transformation remains a tough disease. We are working on several clinical trials looking at new pathways to control the disease, including immune checkpoint inhibitors using venetoclax. One was actually pirtobrutinib.
When you use this drug as a single agent for patients who had Richter’s Transformation, almost half of the patients respond to the treatment and the response lasted for several months. That is one important agent for patients with Richter’s Transformation.
There’s also this new class of drugs called bispecifics, which on one hand bind to a protein called CD20, which is on the cancer cells, the CLL cells, or Richter cells, and then on the other hand, they bind to a protein called CD3, which is on the T cells.
What they do is bring the cancer cell and the T cells together. That has been shown in several trials to be very effective in diffuse large B-cell lymphoma. There is data presented [on] clinical activity for patients with Richter’s Transformation as well.
Those are two important classes of drugs being pursued [in] clinical trials.
The third one is CAR T-cell therapy that also several studies have started to evaluate for Richter’s Transformation, but no specific medical data was reported.
Andrew: Okay, let’s pull all this together. People are still in watch and wait, and that’s fine if their quality of life is not diminished, their blood counts are strong, etc. But when they move on to treatment now, it seems like there’s a discussion about which BTK might be right for them and whether or not they should consider BTK, still investigational, with a second drug like venetoclax. Is that correct?
Dr. Jain: Yes, correct. Absolutely.
Andrew: You have this whole line of tools that we haven’t had for that long and for people with aggressive transformation, there seems to be a glimmer of hope as well. If you had a new patient today, would you say that the likelihood is they can probably live a long and full life? You have medicines that may not cure the CLL — although sometimes you feel CLL is cured — but they can live long and live well.
Dr. Jain: Oh, absolutely. That’s exactly what I tell my patients these days, especially patients who are newly diagnosed. [When] they come for the first visit, obviously, [there are] a lot of questions in their mind. Hopefully, all patients with CLL can expect to live a normal lifespan with good quality of life.
We have excellent medicines for patients right now and the field is improving. [We have] other important, better medications, safer medications, immune therapies, [and] CAR T-cell therapies coming down the line.
I really, truly believe that we’ll be able to have patients with CLL have a normal lifespan. An important point is that you don’t need [a] cure to live a normal lifespan in the context of CLL.
You could have a small amount of disease present, but if it’s not interfering with your quality of life, your blood counts, your health, [and] what you do in your life, you can just continue to live with a very low level of the CLL.
Overall, we’re in very, very good shape in terms of the treatment paradigm for CLL patients. We’re all making really good progress.
CAR T-cell therapy
Andrew: I know CLL patients who’ve had CAR T-cell therapy. It is not yet approved. What is the future of chimeric antigen receptor T-cell therapy for CLL? It’s approved in some other blood cancers, but not yet in CLL.
Dr. Jain: I think this is one of the biggest advances in the last few years, I would say, in the context of blood cancers. It’s not approved for CLL, but [for] lymphomas, leukemias, [and] myeloma.
The field has somewhat lagged behind and we don’t have much clinical data yet. There are [a] few trials, which have been reported, but not very many.
There’s a lot of interest and discussion in general with investigators to develop CLL-specific clinical trials with some new constructs.
CAR T-cell therapy is very dependent on what kind of genes are inside of the CAR so it’s very technologically heavy where even small changes in what gene you insert can make big differences [in] how patients do. There’s a lot of effort happening [on] the lab side to draw up new constructs, which specifically could work for patients with CLL, also for patients with Richter’s Transformation.
That’s an area where I think many more clinical trials will come. In one to two years, I think we’ll have somewhat more clarity of the data in terms of CAR T-cell therapy for patients with CLL as well as for Richter’s Transformation.
Andrew: Okay. What you’re touching on is: can we get the immune system to fight the CLL and do it long term, correct?
Dr. Jain: Correct. From [the] chemoimmunotherapy era to target therapy era, now we are asking our immune system to dress [for] the job and take care of stuff.
Immune therapy works very well for melanoma, for solid tumors. So can we use our immune cells to help get rid of the CLL?
Andrew: It sounds like a great time of progress for those of us living with CLL. With the current therapies, some that may be approved even in the short-term, combinations, and then this work going on in immune therapy that’s happened in some other areas and where this pays off for us.
Dr. Jain, thank you so much for being with us on The Patient Story. We wish you well with your research and your clinical care of patients at MD Anderson.
Dr. Nitin Jain: Thank you.
Chronic Lymphocytic Leukemia Patient Stories
Lynn S., Chronic Lymphocytic Leukemia (CLL)
Symptom: Elevated white blood cell count
Treatments: Chemotherapy, targeted therapy (BTK inhibitor)
Serena V., Chronic Lymphocytic Leukemia (CLL)
Symptoms: Night sweats, extreme fatigue, severe leg cramps, ovarian cramps, appearance of knots on body, hormonal acne
Treatment: Surgery (lymphadenectomy)
Margie H., Chronic Lymphocytic Leukemia
Symptoms: Large lymph node in her neck, fatigue as the disease progressed
Treatment: Targeted therapy
Nicole B., Chronic Lymphocytic Leukemia
Symptoms: Extreme fatigue, night sweats, lumps on neck, rash, shortness of breath
Treatments: BCL-2 inhibitor, monoclonal antibody




3 replies on “CLL Highlights from ASH 2022”
Very good well written article. Helps reduce the initial fear and anxiety experienced by newly diagnosed patients.
Reading from the UK. Very informative with my recent diagnosis that needs treatment in the next few weeks.
Very informative read. I myself was treated with Obinutuzumb and Venetoclax, and now in remission.