Kelsey’s Acute Lymphoblastic Leukemia Caregiver Story

Kelsey was 30 weeks pregnant when her husband, Seth, was diagnosed with acute lymphoblastic leukemia. She stepped into the role of caregiver during what should be an exciting time in her life.
As a dentist, Seth had some medical expertise but the diagnosis was still a major shock. Kelsey had to navigate the medical system and cancer care while planning for their baby’s arrival.
Kelsey shares processing the diagnosis, becoming new parents, and navigating the recovery process.
On a day where you feel like you can’t do it anymore, you just say, ‘One more day.’
Kelsey K.
This interview has been edited for clarity. This is not medical advice. Please consult your healthcare provider for treatment decisions.
- Leukemia Symptoms
- Diagnosis and Treatment
- The diagnosis
- Changing cancer care hospitals
- How far along were you when he was diagnosed?
- How did you process your husband’s diagnosis while also being pregnant?
- Being strong for each other
- How did you get through those challenging times?
- Feeling like you’re always doing the wrong thing
- What advice do you have for caregivers feeling guilt?
- Becoming Parents
- The Recovery Process
- Reflections

Leukemia Symptoms
Introduction to Kelsey
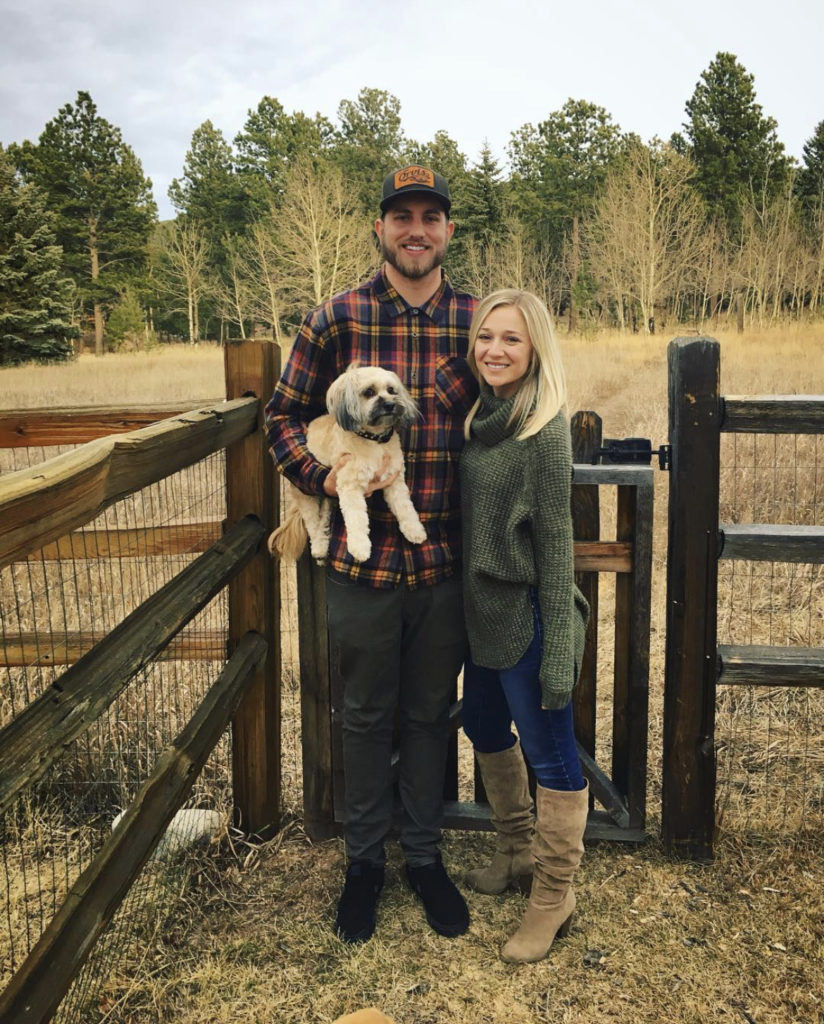
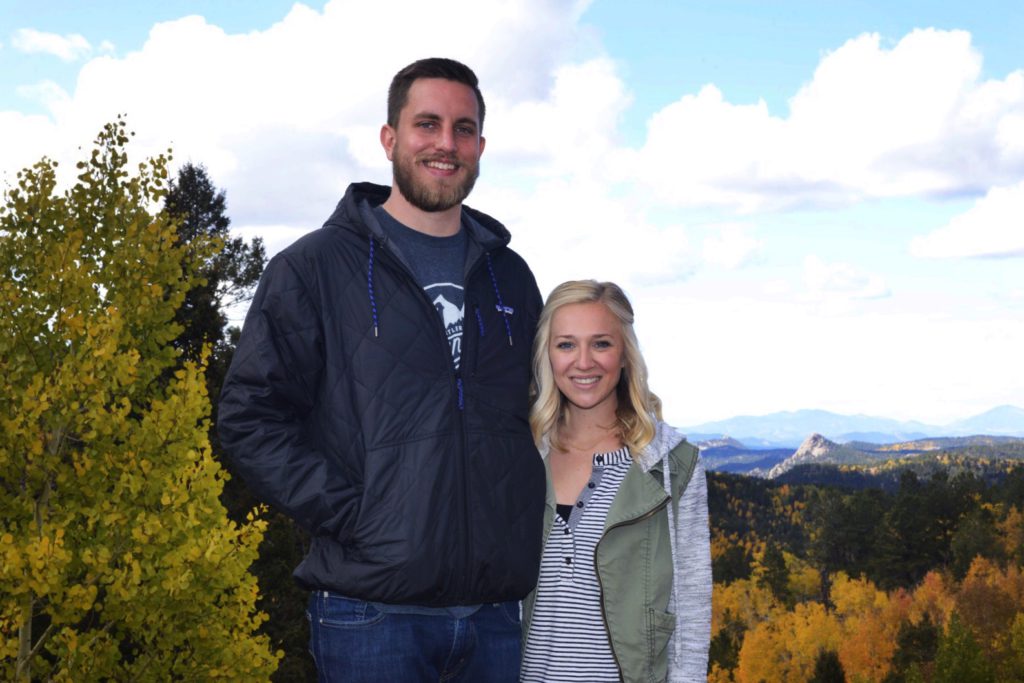
I’m Kelsey Klasko. Hobbies and things we enjoy probably changed a lot, especially since having our daughter.
[I] absolutely love being outside, even if it’s just eating lunch outside, playing in the grass, hiking, camping, fishing. Anything outdoors makes me happy.
I don’t think I’ve ever, especially in the last few years, had a really strict exercise regimen but I like to keep moving. Having a toddler definitely helps me do that.
Seth’s 1st symptoms
[My husband] started feeling really crummy. He went camping with one of his friends, and I was going to go, but I was pregnant. My doctor said off-roading, and high elevations are not good for you right now.
He went with one of his buddies, and he took one of our dogs. Just knowing my husband and how similar we are and loving to be outside, I just know when he’s gone for the weekend that I’m not going to hear from him until it is sundown the night he’s supposed to be home because you won’t have phone service.


He called me the day after he left and said, “I’m on my way home. I feel terrible, just my whole upper body, even breathing.”
He was driving home on a dirt road, and it was bumpy. [He] was just feeling everything. That was really weird.
We’re young and healthy, so I thought, “All right, buddy, how much whiskey did you guys have last night?” High mountain elevation sickness — people get that, too, and you were sleeping on the ground, and we’re 30 now. We chalked it up to all that kind of stuff.
He felt crummy the rest of the weekend, took it easy, and then he was having several more painful episodes that were concerning. More fatigue.
First hospital visits
We started going to the doctor. His blood work came back normal. They did a chest X-ray. They chalked initially his symptoms up to a strained muscle under his ribs and told him to take it easy.
In the night or late early morning, he was just having these [episodes] where he was just waking up in pain. His upper body was just painful. It got to a point where he just kept going back to the doctor.
They prescribed him muscle relaxers and anti-inflammatories, and that wasn’t helping. We are not really medication people. I mean, we take Advil or Tylenol if we need it. He’s a doctor himself, and he just really wanted to make sure they knew, like, “I don’t want opioids; [I’m] not trying to get pain medication.”
But the concern became greater when the muscle relaxers weren’t working because we’re sitting here like, “Okay, it’s not muscular. What’s going on?” Again, just a few more weeks go by.

He had gotten the Johnson & Johnson vaccine. I wondered, “If I go into labor and he hasn’t been vaccinated, will they not let him be there with me?”
He got the Johnson & Johnson vaccine and had a pretty moderate reaction. I wanted to take him to the ER, and he’s like, “No, they’re just going to tell me it’s the side effects from the vaccine.” And so he didn’t go.


Irregular blood work
Then the baby shower came and went. [For] the baby shower, normally he would go get out of the house and go fishing for a day or something, not be surrounded by a bunch of women in a house having girl time.
But he stayed home. He didn’t leave. He wasn’t feeling well. You could just kind of see his pallor; his color was not right. His dad had actually ended up flying out to come and visit with us because he could even tell his son [was] not behaving normally.

We were reading the ER doctor’s notes, and he has a differential diagnosis. One of them was lymphoma.
He went to the doctor on a Thursday. He was supposed to go to work with me because we work together, and he ended up going into the doctor that day. He just was feeling terrible. I had to tell him, “You’re staying home. You can’t function like this.”
He went to the doctor. They actually repeated blood work. This was like three weeks apart. Then I got home from work that day, and he was on the phone with her.
She said, “Your blood work’s totally irregular, and I want you to get a CT scan. I ordered one for you tomorrow, but I really think you should just go to the emergency room because you can get one faster.”
ER visit
So we did that. They repeated the blood work because they wanted to make sure it wasn’t a lab error or anything. They did do a CT scan. I’m not going to say all ERs are this way, but I think a lot of emergency rooms, it’s not really their job necessarily to diagnose in these situations.
It’s more of, “Let’s get you to the right people.” So the only thing that the ER doctor could tell us is that “your spleen’s enlarged, your platelets are extremely low, and I’ve had a hematologist review your blood work. He really wants to see you as soon as possible.”

This was a Thursday night. My husband and I have medical backgrounds — We’re in dentistry, but we’re educated to a degree. I wondered, “What do all these symptoms mean?”
We were reading the ER doctor’s notes, and he has a differential diagnosis. One of them was lymphoma. I wondered which one was the worst one, and what do we do. Again, no one had diagnosed him with anything.
Trying to set up a hematologist visit
Friday morning, I called the hematologist that the ER doctor gave us, and it was a bit frustrating because it was a central scheduling phone number. It’s not the doctor’s office. When I finally got ahold of them, I said, “He needs to see him as soon as possible.”
It was the first week of September and they told me they didn’t have any openings until the end of the month.


I told them, “No, [not] the end of the month. He needs to be seen today. If not, Monday. It needs to happen.” I asked, “Is there someone else I can talk to?
I got connected to the office, but again, it was a woman who works at the front desk, not a nurse, not anyone. I explained, “This is an emergency. The end of the month isn’t going to work.”
The earliest they could do, the best they could do, was that following Friday, so a week. I said, “Okay, I guess, schedule it.”
Symptom escalation
Over the weekend, his condition plummeted. He started having bruises everywhere. They weren’t going away. Petechiae all over his body. Again, the color of his skin. He just was sweating, and his gums started bleeding. He’s a dentist. His gums don’t bleed.
I called on Monday, and I kept making phone calls. I honestly don’t even know how I ended up getting on the phone with the triage nurse, and she was over at MD Anderson in Greeley, which is probably 40 minutes from our home. She just said, “Bring him in. Just bring him in.”
I didn’t realize at that time his primary care doctor who had done the blood work, who told him to go to the emergency room, had actually sent some of the blood work off to a pathologist already. There were things going on in the background that we just didn’t know yet.

Diagnosis and Treatment
The diagnosis
We got to MD Anderson in Greeley, and they sent us to the infusion center, where people do outpatient chemotherapy. We’re just kind of sitting there. Again, we don’t know what’s happening, but we thought, “Is it a mistake that we’re here? Part of me feels like you don’t get here unless you have cancer, but we don’t know anything.”
One of the nurses actually brings us back to a hematologist oncologist’s office, and says, “Hey, based on some of the blood work we have here and talking with your doctors and then the ER, we’re pretty positive that you do not have lymphoma.”
And I was relieved. I was like, “Yes!”



But then she said, “I’m almost positive you have leukemia.” I started crying right away. I think Seth, my husband, was just sort of sitting there. You’re hearing what they’re saying, but you’re not really hearing what they’re saying.
I’m just thinking, “I’m almost 30 weeks pregnant, and how does this…?” I just started spinning. I asked the doctor, “Is he going to be able to be with me when our daughter is born? What’s going on?”
She said, “Yes. Absolutely.” Very reassuring at the time. She said, “We still have to get more information.” He had to get scheduled for a PET scan. He had a PET scan, I think, the next day or two days later. More and more blood work. I mean, so much blood work going on.
»MORE: 3 Things To Remember If Your Spouse/Partner Is Diagnosed With Cancer

Changing cancer care hospitals
The doctor that was there was like a traveling doctor. She let us know, “If it is the type of leukemia we think he has, it can’t be treated here. We’re going to be in contact with some doctors in Denver to see if we can get him admitted.”
Seth had to get more and more bloodwork and bone marrow biopsy. They didn’t really want to send him home, but they didn’t know how soon they could get him admitted down in Denver.
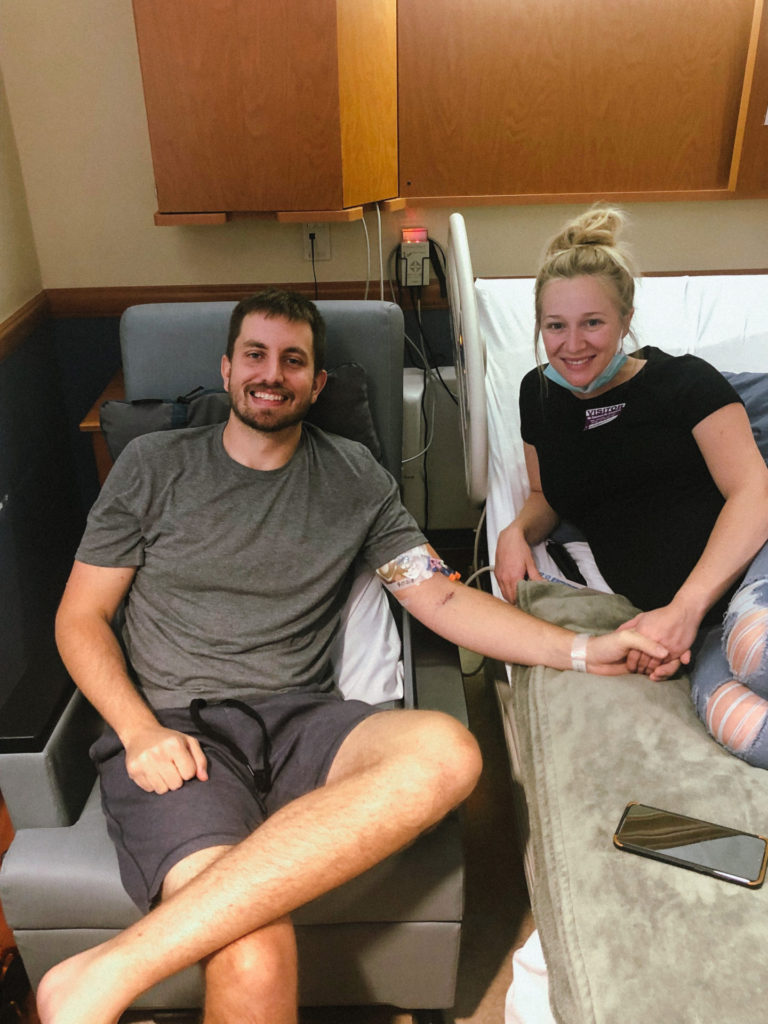
They wanted to get as much information as they could and at least start doing something for him in the interim. Thursday when he was at the ER, his platelets were 20,000, which is very low. By Monday when things were significantly worse, they were like 8,000.
The center is not very equipped to deliver blood products, especially the amount that he needed. Just for one bag of platelets, he was sitting around for like seven or eight hours.
His body at that time was so sick. He’s not retaining them. So they’re just kind of dying and flushing away. He got his first bone marrow biopsy on a Thursday, and then that same day, Colorado Blood Cancer Institute in Denver contacted us and said, “We have room for him; we’ll take him.”
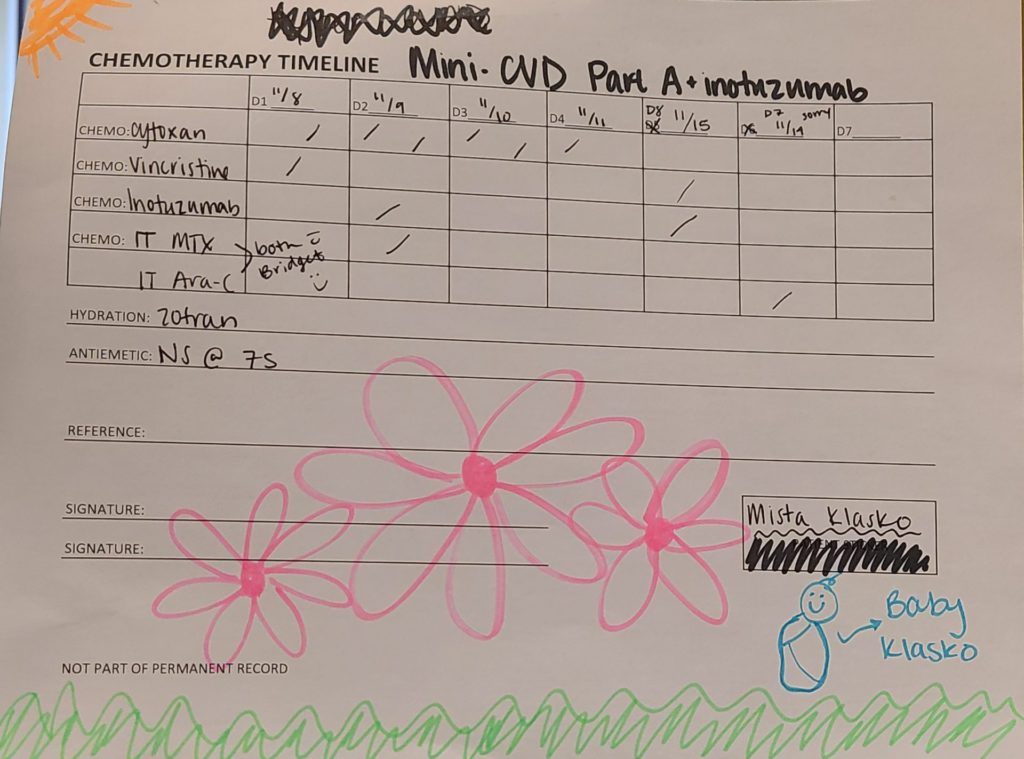
They basically sent us home that night to pack because they said, “You’re not coming home right away. You’re going to be there for at least a few weeks.” We headed down to Denver, and so September 17th was his first day of treatment for acute lymphoblastic leukemia.
How far along were you when he was diagnosed?
His actual date of admission in Denver was my 30-week checkup and I canceled it. The family kind of fought me on that. I was healthy. I felt good. I’d gone to all my other doctors’ visits.
The first trimester of my pregnancy was weird. I ended up having bleeding, which can happen, but I think mine was a little bit higher risk. I actually wasn’t allowed to do any real physical activity or anything in my first trimester. There was a heavy chance that I would miscarry, but I didn’t.
This is a moment — a long moment, but it’s not forever. It’s not our life. It’s just for now.
That part was scary, but by the time I was at 30 weeks, everything was going really well. To me, it was a no-brainer. I thought, “I’m not going to miss my husband getting admitted into the hospital. I’ll go to a checkup a few days later. We’ll figure it out.”

How did you process your husband’s diagnosis while also being pregnant?
I think I still am. Initially, I thought there was going to be a lot to worry about when she was born. For now, I don’t want to say it’s easy because it wasn’t, but I was like, “She’s with me. She’s here.”
They always say, “The baby can hear you, the parents. They feel what you’re feeling.”
I thought, “She’s going to be around us and hear us both as much as possible. So we’re all going to stay together, and I’m going to be as calm, cool, and collected as I can while she’s still cooking. I don’t want that to be anything additional for us to all worry and stress about.”
I thought back to how I was raised and observed my parents. Then I put myself into my husband’s parents’ shoes and then, of course, my husband’s shoes.



I just always thought, “What example do I want to be for my kid, and how do I want to remember this time and how I carried myself?” Whether it was for her or for him or for the rest of our family.
I think I always use that as a little bit of motivation. I think just always be hopeful and optimistic. I’m going to hope the best and think the best until someone tells me I can’t. That’s always been my mindset.
Being strong for each other
To a fault in some ways, I think my husband and I both tried to be strong for each other. I think he wanted to display strength so that I wasn’t worried about him and stay healthy through my pregnancy.
I wanted to be as strong as I could for him because I wanted him to know I have total confidence that we’re going to get through it, and we’re going to be fine. This is a moment — a long moment, but it’s not forever. It’s not our life. It’s just for now.

How did you get through those challenging times?
We have such great support. His parents, my parents, and even his aunts. It’s almost like the caregivers need caregivers. It never ends. We all needed each other. I think that was so helpful for me.
I wouldn’t leave the hospital. I stayed there with him. It was almost a solidarity thing.
Family [would] tell me, “Look, go for a walk, get out, and we’ll be here.” It was almost reassuring knowing if I wasn’t with him, someone else was with him. And the same with our daughter.
Feeling like you’re always doing the wrong thing
I knew the challenge would be much greater once she was actually born because she wasn’t allowed to be at the hospital with him. There would be times when I had to be with her, and it was very difficult because I felt like I was always doing the wrong thing.
I felt like if I was with her, I needed to be with him, and if I was with him, I should be with her. No one ever made me feel that way but me.



Seth and I talk about it all the time. There are people that do this alone and people that don’t have caregivers or caregivers that don’t have caregivers.
We’re so grateful that we’ve faced so many worst-case scenarios in our early lives together, but of every worst-case scenario, we’ve had the best possible outcome you could get from that. Remembering that is important.
What advice do you have for caregivers feeling guilt?
You’re not doing yourself or anyone you’re with any justice by not being present with them at that moment. I just had to tell myself that if you’re going to be with Charlotte, give her all the attention and love that she deserves right now.
You’re not helping Seth by worrying constantly and not being present with her, and you’re not helping her by not giving her all of the love and attention.
In a way, I kind of felt like, you know what? Your daddy can’t be here with you right now, so I’m giving you all the love from both of us. And kind of the same with him. When I was with him, I’m giving him all the love from her.



I kept a blanket of hers with him in the hospital, so I would kind of have his scent or whatever on it. Then every few days I’d swap some blankets out and then take that blanket back to her.
Just knowing, like I said, when I wasn’t with Charlotte, she was getting the best care from her grandparents and aunts, and the same with Seth. There’s just no shortage of love.
The nurses were phenomenal because there were moments when he was alone, give or take, for a few hours or whatnot. They were a great source of relief, knowing that he was in good hands when there were moments when there was maybe a lapse of family being there with him.
Becoming Parents
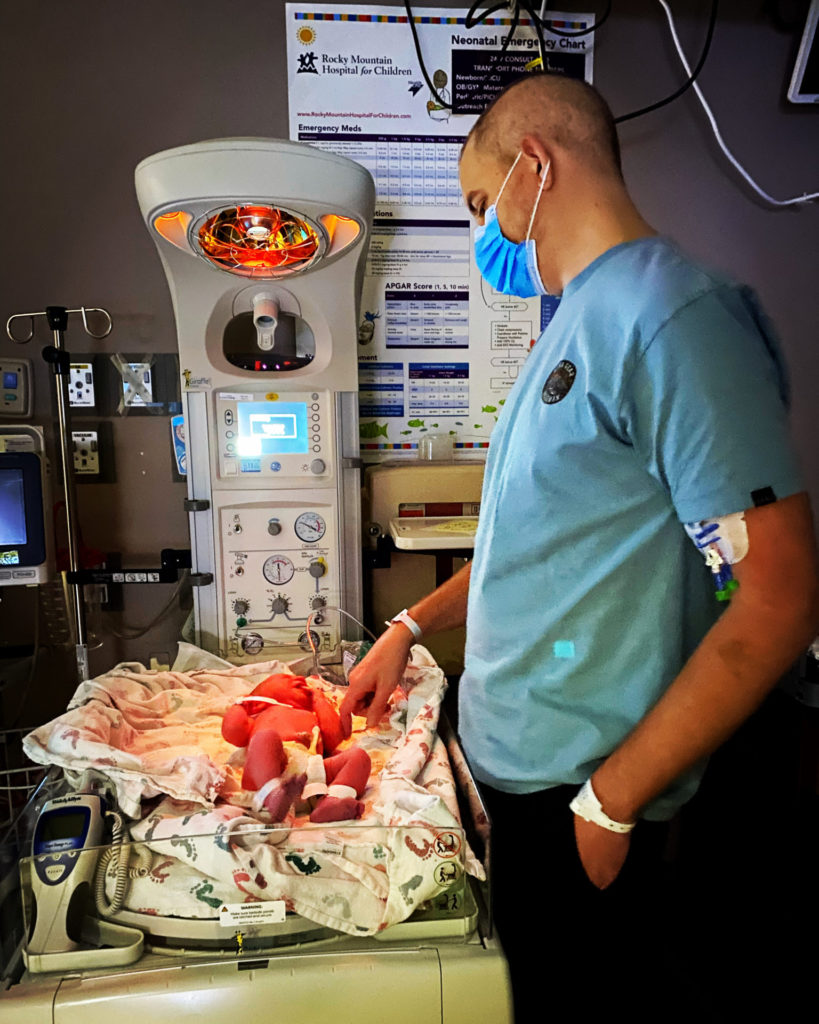
Was he there when you delivered your daughter?
Yeah. With just the fortunate schedule he had. We told his medical team from day one. Of course, they knew our situation. It was so obvious because I was super pregnant. He was home for almost every major event holiday.
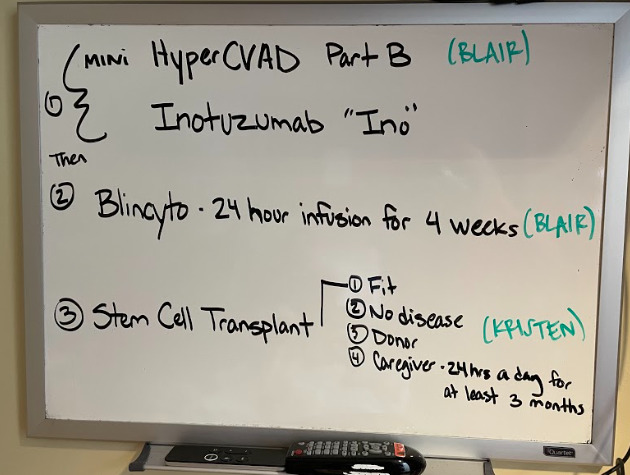
The way it worked out, his initial inpatient stay was six weeks. It was supposed to be shorter, but his first round of chemotherapy didn’t work. He was supposed to be on the pediatric treatment plan, which is strictly chemo. But it’s long. It’s a few years.
Initially, we thought he was getting out after about three weeks, and then we got his bone marrow results back, and it hadn’t worked. That’s when they told us, “Hey, we’ve got to start over with this chemo plan, and we’re going to do the adult plan.”
On top of that, that’s when we found out he was going to need a transplant. So that was a really hard day. I had everything packed. I was ready to go home. I was like, “I’m getting this guy out of here. Jailbreak.”
The doctor made his rounds and told us that we weren’t leaving that day. So it was another three weeks.
Getting induced
He was discharged on October 29th, and my due date was November 10th. By the time he had gotten out, I was 39 weeks. At that point, women are allowed to do elective inductions.
Prior to him being sick, I told him, “I don’t really have a pregnancy plan or a birthing plan. I just really don’t ever want to get induced. I just want to kind of let it all happen.” But he was actually scheduled to go back in for more chemo on November 8th, so we knew we had a window.



Again, it’s a control thing, right? It’s almost like so much has happened outside of our control, and if I can control him being able to be there for our daughter to be born, I’m not going to miss that.
We made the decision I would get induced, and he was there. We were, again, fortunate. Because of COVID, they had strict rules about who could be your support person in the hospital for your delivery.
I talked to them, and I said, “My husband just spent six weeks getting chemo in a different hospital. I don’t know how long this labor is going to take, and I don’t know if he’s going to be able to be here the whole time.”
They worked with us. They allowed my mom to stay and be with me the whole time, and he was allowed to come and go and be there for the most important parts. Again, it all worked out.
Recovering after giving birth
She was born on November 5th, and we got to leave the hospital on the 6th. He was home for a couple of days before [going] back to Denver for chemo. We live about 45 minutes away.
From a recovery standpoint, I thought, “I want to recover as fast as I can because I want to get back down to Denver and visit with him.”
My husband, of course, was always very supportive. The family was always there. For most of the first year, we were never alone. Someone was always with us, which was amazing.

How did you manage life as both a new mom and a caregiver?
You just have to. I don’t know. I try to write things down, make notes, [and] have a schedule as best as I can. I made it a priority to try and breastfeed our daughter, which got a little complicated with being with my husband, being home, and back and forth.
I was almost scared in a sense. One of the things I read online about breastfeeding [is] it helps prevent childhood cancers like leukemia. For me, I was like, “She’s getting all the breastmilk. All of it!”
I think it’s a control thing. I can control that she gets this and that she’s getting fed the best. No matter what, I’m doing what I can to support her in that way. No matter what.
I know I carried a degree of stress and anxiety with me that I probably tried to push down again purely from the fact that I’m like, “They say that the baby feels what the mother feels.” I just was trying to control so much of that.
I don’t think I was fooling anyone but myself. I probably should have had more moments to cry or get it all out. And I had my times, but I thought, “I can do that later. You can cry later.” Then later comes, and then I had about 50 other things to do.
Caregiving as a full-time job
We used to work together full-time as a couple, and both of us, our lives completely stopped. I stopped working as well and didn’t go back to work until the end of August this last year.
For me, it felt like my new job. It is the most important job I’m ever going to have, whether it’s being a caregiver for my husband or daughter.
That just became my blinders-on focus that no matter what, I’m going to just give everything I have to them. I always told myself, “You can do this another day. You can do this for one more day.”
Then the next day comes, and you say, “I can do this for one more day.” There were times when it was really difficult.
I do think finding the good, even in the smallest moments. It can be hard. I get really greedy with my husband’s recovery and where I want it to be versus where it is.
I had to stop doing that and start celebrating those little wins and be excited for them, even when they may seem small. Celebrate them because you need to, because it gives you hope for the future.

The Recovery Process
Processing your emotions
It’s kind of strange when you go through something traumatic. You compartmentalize parts of your emotions and your life. During the treatment process, when he was in the hospital, and even the first 100 days after his transplant, you have such a schedule.
I was so busy that my primary focus was, “What am I doing now? What do I have to do in an hour?”



Now we’re in a place probably since [the] end of summer, early fall, where my husband became a lot more independent and helpful with our daughter, and we were kind of alone as our family unit.
I think you have this delayed processing. We both started therapy. He and I both see a therapist, and I’m not saying you go once and it’s magic, poof. But she’s been helpful. Honestly, I wish we could do more therapy.
Letting yourself feel your emotions
For me and for Seth, I think our processing is probably a little different, what I need versus what he needs. I’m at a point where talking with other caregivers is helpful because you can try and explain to people what’s happening or what you’ve been through.
It’s no one’s fault, but if you haven’t lived it, it’s just a very difficult thing for someone to understand — and then add all of the extra circumstances we had on top of it. It’s complicated.

I do think kind of starting to let myself feel however I should feel. I think there’s a lot of me feeling guilty for wanting to cry or be sad because it’s like things are — I don’t want to say things are perfect now because they’re not. But there is so much to be grateful for and happy for.
But there is a mourning of experiences you thought you may have had. Usually, you picture the birth of your child or the first few months or a year in a certain way, just like you imagine your wedding, right? You kind of have this picture, and it’s changed. It’s not that way.
You can be sad for that, but then you have those moments where you’re like, “Yeah, but I’m also grateful because, without everything we’ve been through, he’d be dead.” It’s a continuous process, and I don’t think you’re ever done processing it or feeling it.
Recognizing triggers from the leukemia experience
I think a lot of patients and caregivers will go through phases of times where they’re maybe triggered by something. We went to Phoenix back in November to go see family. That was kind of the first thing we’ve done since before COVID and him getting sick.
I was packing his bag for him, and it was the same bag that I packed for him to go to the hospital every time. I cry every time I pack a bag for him. It’s weird because it’s not something I expected to happen.



I told him that after the fact, and he said, “Well, maybe I just need to get a new bag then.” And I said, “Yes, please, let’s get a new bag!”
We’re still in recovery. That may be lost on people outside of this community. People assume you’re in remission or you had your transplant or, oh, my gosh, Kelsey is back to work. Wow, your life, boom, everything’s better.
This is just another chapter that’s probably a lot harder than either of us expected. Our therapist has reassured us it’s actually very normal what we’re experiencing right now, which is validating.
I don’t think I expected this phase to be so hard on my mental health. But I’m happy that both of us are working on it. Some days and weeks are better than others, but we’re a work in progress.
What advice do you have for taking care of your mental health during recovery?
Well, I’ll say something our therapist had told us or me. She said it’s not uncommon at this point in recovery where the caregiver and the patient actually start to progress at different rates.
She said, even in your relationship, it can be challenging. I was so used to doing absolutely everything for him because he needed it, and now he doesn’t necessarily, and I still want to do everything.
[It’s] almost like stretching that muscle of knowing when is it right for me to maybe push a little to encourage him to have some more independence versus when do I need to pick up that extra slack in any facet of life?
I think that advice would be no matter what you’re feeling, it’s normal. We’re not all going to feel the same way, and our responses are not going to be the same. Accepting that is okay.

Being open about your feelings
I do wonder sometimes if I’d cried more in front of my husband, maybe if it would have made him feel comfortable to do the same. Because I do wonder sometimes if both of us are trying so hard to be strong for each other that we almost don’t allow each other to express ourselves in a way that both of us are craving in the moment.
I do think having a little bit more openness about your own feelings is important as well. We’re so concerned about how everyone else is feeling and doing that sometimes you forget I’m still really important, too.
In order for me to be the best I can be for them, I need to recharge or reset or just do something. It doesn’t have to be anything big, but just finding something small you can do for yourself that makes you feel better.

Again, it’s probably different for each person. It is important. So I would just say feel however you feel. It’s okay, and you’re important, too, even if you sometimes don’t feel like it.
Look forward. I think constantly being positive and hopeful. It’s so easy to dread the worst. “Cancer” is a trigger word. It’s a terrible word.
Waiting for results
There are times that are really difficult, especially when we’re waiting on results. His one-year transplant anniversary is two months away, and so he’ll have another biopsy in April.
I don’t even think about it or worry about it until he gets it, and then you’re just waiting, waiting, waiting, waiting. You don’t get results usually for one to two weeks.
I’ve always noticed this kind of anxiety we both have but almost don’t talk about when we’re on edge a little more when you’re waiting for results. Like I said, sometimes just address the elephant in the room.
»MORE: Patients describe dealing with scanxiety and waiting for results
Reflections
Remembering others’ intentions
It can be hard when you talk to friends and family or other people. Again, outside of this, I think that so many people want to find a way to relate to you by saying, “Oh, I totally get that.”
It’s hard because, of course, their experience is totally not relatable at all, but they’re doing the best they can. I think that sometimes you can be a little annoyed, because you’re like, “You don’t get it.”
But remembering intention, people are intentionally trying to connect with you with something they just do not comprehend. Take it with a grain of salt and just remember people’s intentions are generally good when they’re trying to relate to you. So be patient with them.



What is the right thing for friends and family to say to someone with cancer?
Usually saying something is better than saying nothing. I think sometimes you may have friends or people — maybe they’re not your best friends, but people you’re close with in life or that you see on a regular basis.
Some people just don’t know what to say because it’s a hard thing to approach. Say something. It could be as simple as, “I’m really sorry. That sucks.” Sometimes just say, “You know, that really does suck.”
Instead of sometimes trying so hard to relate, just empathize. You don’t need to necessarily try and relate so hard, but just having that empathy is really helpful.
So much of what was good for Seth in the hospital was when friends visit or family visited and they talked about normal parts of life. Sometimes it’s almost refreshing to hear about other people’s problems because it takes me away from mine for a minute.
Change in perception of real problems
There’s the duality of that. Seth and I are forever changed in the sense that our perspective of what true problems are versus menial things seem like are real issues, and then you find out they’re really not.
Something we’re both working on, too, is recognizing when people talk to us about their problems, those used to be our problems before everything happened. Not necessarily having hostility against anyone for that because that’s what is normal for them.
But it is hard sometimes when you listen to someone talking about their issues, and you just sit there like [nodding]. You take it one of two ways. You can be annoyed and angry and like, “Oh, they’re so insensitive.” Or you can just be like, “Wow, I miss when that’s all I cared about.”


Staying optimistic
The progress isn’t always linear, which can be frustrating. We expect from day zero and then counting back up after the transplant, that it will always improve. Thinking every day is better than the last, and it’s not, which again is difficult.
But even if it’s not better every single day — you may have a week or a month where things are great, and then maybe they’re not, and you stay there for a month, and then they get better again. It does get better. It does.
I think just staying hopeful, staying optimistic. On a day when you feel like you can’t do it anymore, you just say, “One more day.” And then every day, that’s what we say: “One more day.”
But it does get better. Even if it may not feel like it or there are times that are really hard, you do get through them. Medicine’s improving, research is improving, and I’m just so grateful for that. And be a donor.

Inspired by Kelsey's story?
Share your story, too!
More Spouse Caregiver Stories
David Garrigues Ronda, Spouse of Laurent Gemenick, Bladder Cancer Patient
“Talk to family, talk to friends. Ask for help. Don't be alone. And above all, don’t miss any doctor's appointments.”
...
Lung Cancer Caregiver Series Episode 2: Stephen and Emily Huff's Candid Conversation
"We talked, and I remember saying, "What if we have kids and what if I die?" And you were like, "What if you live?"
...
Emily Huff, Spouse of Stephen, Lung Cancer Patient
“Emily's the reason why I’m alive today. The treatments have kept the cancer at bay, but she's the one who’s kept me living, breathing, and enjoying life.”
...
Blair D., Spouse of Brain Cancer Patient
“Find other people who are going through the same thing you are. This journey is very isolating and very lonely.”
...
Nat G., Spouse of Bladder Cancer Patient
“You have to become selfless as a caregiver. You have to assure that person that you are there for them.”
...
Kyle Appleford, Spouse of Lung Cancer Patient (Metastatic) with No History of Smoking
“Ask for help. Don’t be too prideful to accept the help. I wouldn’t be here without all the support from family and friends.”
...






