Cheyenne’s Stage 3B Melanoma Taught Her the Power of Self-Advocacy
When Cheyenne was diagnosed with stage 3B melanoma in December 2024, everything in her life shifted. At first, doctors thought it was stage 2, but after surgery in January, the diagnosis became clearer. As a photographer and storyteller, she’s spent decades documenting the world around her, but suddenly she had to turn that lens inward and focus on her own health.
Interviewed by: Taylor Scheib
Edited by: Katrina Villareal
Her first warning sign was a mole on her back that itched. Even though her gut told her something was wrong, the first doctor told her it was cosmetic. Thankfully, a physician assistant took her concerns seriously and ordered a biopsy. That persistence saved her life. From that moment on, Cheyenne learned the importance of advocating for oneself and trusting one’s intuition. She emphasizes that when something doesn’t feel right, asking questions is essential.

After surgery revealed cancer in her lymph nodes, she was officially diagnosed with stage 3B melanoma. She describes the wide local excision as far more invasive than she expected. Recovery was rough, but she leaned on her husband, friends, and a strong medical team. Even though she feared asking for a second opinion, she eventually welcomed it and found reassurance knowing she had access to comprehensive care.
Immunotherapy became her next step, but it hasn’t been easy. Side effects like colitis, thyroid problems, and adrenal issues forced her to pause treatment. Despite setbacks, she has shifted her focus toward what she can control, by supporting her body with meditation, yoga, organic foods, and daily juicing. Instead of filling every day with endless work and projects, she’s learning how to slow down, listen to her body, and celebrate small victories.
Cheyenne also reflects on the emotional side of stage 3B melanoma. Losing her beloved dog BamBam, who went through treatment at the same time as her, deepened her understanding of presence and grief. She’s found comfort in rituals, from nightly tea to morning breath work, and discovered the power of community, whether through friends dropping off books or her husband sitting by her side at tough appointments.
Above all, Cheyenne stresses the importance of education. She believes that knowledge is power, and being informed about treatment options, staging, and side effects helps patients make decisions with confidence. Sharing her story makes her feel seen, and she hopes it encourages others to speak up, ask for help, and feel safe in their vulnerability.
Watch Cheyenne’s video or read her interview transcript to find out more about her story:
- She learned the hard way why trusting your gut is non-negotiable
- What her dog’s cancer taught her about slowing down and living fully
- The unexpected ways diet and meditation became her lifeline
- How she found her voice and learned to ask for a second opinion
- Name: Cheyenne E.
- Age at Diagnosis:
- 45
- Diagnosis:
- Melanoma
- Staging:
- Stage 3B
- Symptom:
- Itchy mole on her back that changed in appearance
- Treatments:
- Surgeries: Wide local excision, sentinel lymph node biopsy, lymph node removal
- Immunotherapy
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
- My name is Cheyenne
- The first red flag – my initial melanoma symptom: an itchy mole
- The moment everything changed
- How I found my care team
- How surgery went
- The cancer spread
- What the mole looked like
- My reason behind getting a second opinion
- Treatment side effects forced a break
- How my life has shifted
- Navigating my diagnosis with my partner
- What I want people to know
- How I’ve supported my body
My name is Cheyenne
I got diagnosed with stage 3B melanoma in December 2024. I was first diagnosed with stage 2 and then post-op in January, we discovered I was stage 3. I’m from Malibu, California, but currently reside in Santa Cruz.
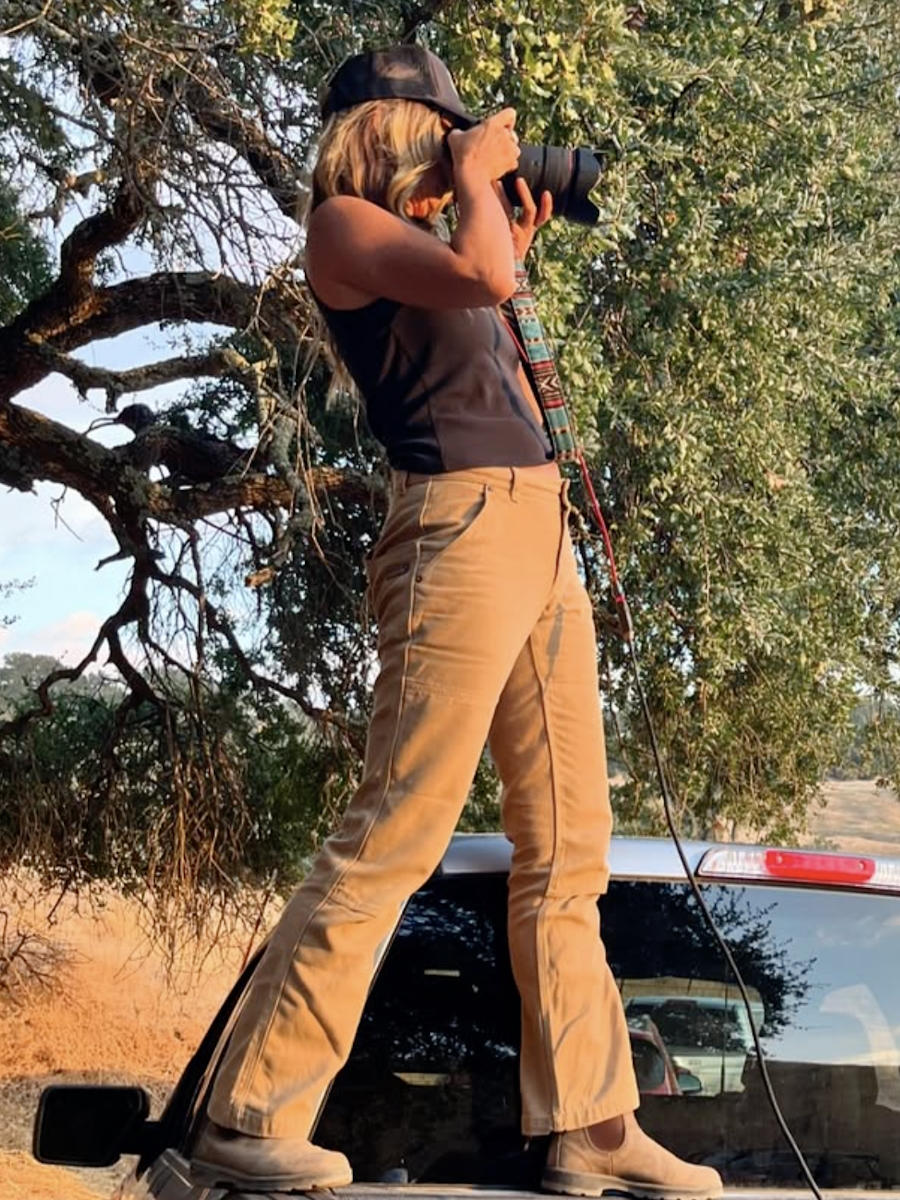
I’m a photographer, traveler, and a lover of dogs, kids, and all things. I work in the commercial advertising space. I photograph a lot of women’s health, women’s fashion, kids, sports, recreation, and travel. I’ve been doing that for about 25 years.
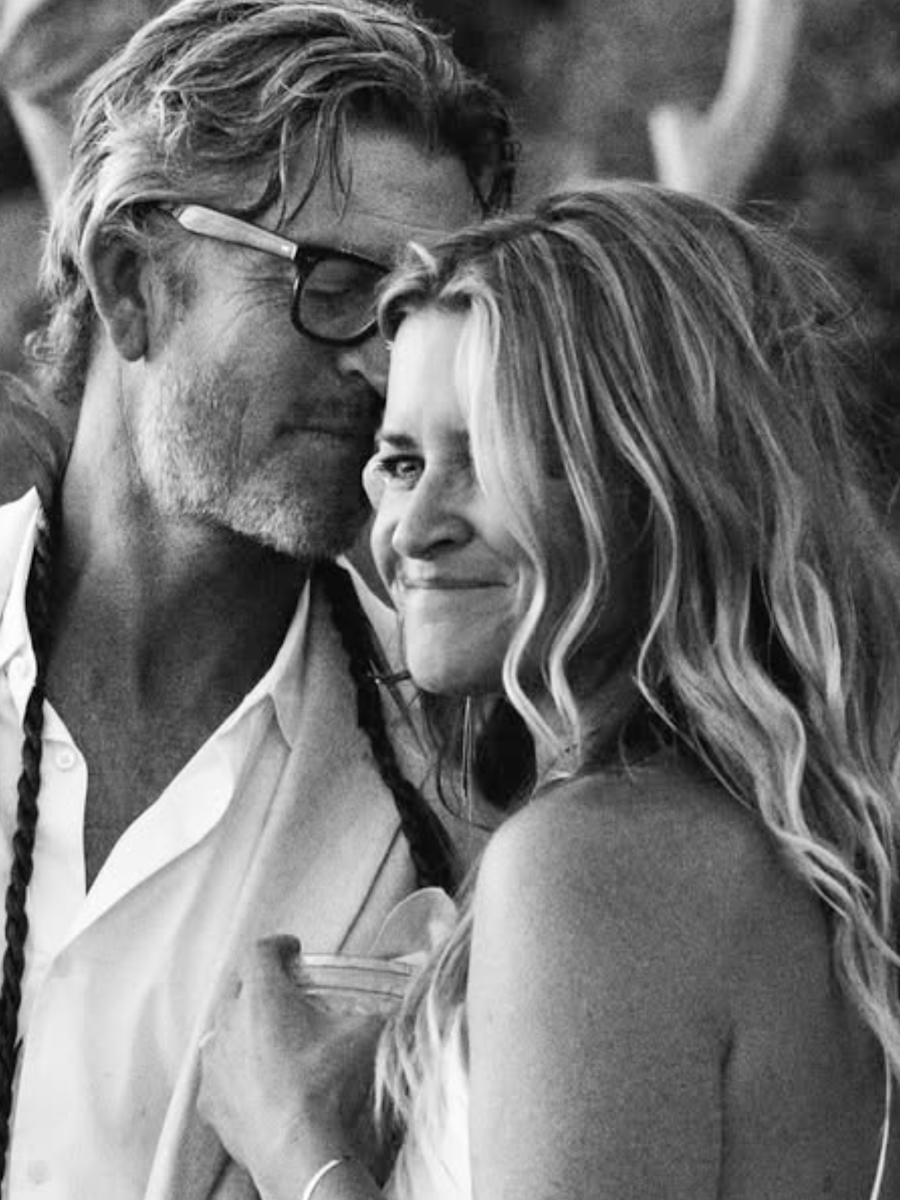
I’m married to a very handsome man who is an avid surfer and a geologist. We love living in Northern California. We’re very outdoorsy people. We live in a little town just above the ocean. It’s super beautiful, and it’s been a great place for me to work on this healing journey, for sure. I left LA about five years ago. I was there my whole life. I got my diagnosis when the fires were happening.
I’m not working at the moment. I’m taking a little break to focus on treatment and doctor’s appointments, but I still go outside for little walks, hikes, and days at the beach.
My parents grew up in the film industry. They were both stunt people. I grew up in a family of stunt people, including my mom, dad, aunts, uncles, cousins, and my sister’s husband. I grew up in that industry and loved image-making. I got into stunts as well in my 20s. I did that for a while and then realized the longevity was not there for your body, so I turned to the other side of the camera.
I picked up a camera and fell in love with it. I could tell stories, travel, and make a job out of it. I studied under a photographer in New York and then started my career. I feel lucky that I had creative parents who encouraged that process and it took flight. I signed with my first agent at 28 and went down the path of shooting lifestyle. I never got heavy into fashion. That parlayed into doing a lot of campaigns with kids and athletes. It’s been an incredible career and I plan to keep going for a while.
I talk to my best friend every day, so I hope I do her justice. She would describe me as a planner, a very hard worker, sensitive, and a good friend. I work hard. I probably work too hard sometimes, but I love my job, so it’s a combination of always having creative ideas that I want to get out of my head and loving to be busy. I’m learning to slow down, so not filling every moment with something to do is my true challenge right now. I definitely get described by most people as a very hard worker, very sensitive, and someone who loves to organize and plan things.
I realize it’s become a coping mechanism for me. I’ve had a lot of loss in my life. I’ve lost my parents at a young age, a couple of friends, and a couple of ex-boyfriends. We lost our dog to cancer last month, which was the hardest thing in the world. Learning to slow down has been a gift. He got diagnosed two to three months after me. We went through treatment together for months. I would go to his and then go to mine.
I don’t often have pictures of myself. It took me a while to dig deep and find some. I have a million pictures of everybody in my life and all the things I do, just not of me. There’s a photo of my dog and my arms after treatment one day, and there’s a tattoo on my arm that says, “Love you, Daddy-O.” It was the last note my dad left me before he passed away, and I got it tattooed on my arm.
I ended up naming my dog BamBam, which was my dad’s nickname. There was a day when I was lying on the ground with BamBam, my arm was wrapped from an infusion and his arm was wrapped from an infusion, and my tattoo was in the picture.
The first red flag – my initial melanoma symptom: an itchy mole
I noticed a mole on my back, which had been there for some time. I’ve learned now that moles on the back are very hard to watch because you can’t see them, but it was something that I was concerned about. I asked my general practitioner about it, not long before we ended up getting it biopsied. Unfortunately, the first doctor I shared it with told me that she thought it was cosmetic. I pushed and said, “Are you sure?” I let her know that it itched and found out later on that it was a telltale sign. I’ve learned that when in doubt, biopsy. I didn’t know enough at the time.
About two months later, I came down with pneumonia in December 2024, so I went in for a chest X-ray. The physician’s assistant asked me about the mole and he said, “Have you had this checked out?” I said I did a couple of months ago. He asked if we had biopsied it and I said no. He said, “I can’t do it right now, but can you come back tomorrow? I’d love to shave this off.” I said absolutely because my prior doctor made me feel like it was cosmetic and it wouldn’t be covered by insurance, so thank God for him. We shaved it off.
I got a call from him two days after Christmas and he let me know the news. I truly feel that man saved my life. I ended up finding out how aggressive it was and how a few months later would have made a big difference. Everything changed on December 27th and within three days, I had a surgeon, a plastic surgeon, and dermatology. I had four or five appointments and was scheduled for wide excision surgery in two weeks. Everything got put on hold. He told me that this needed to be the most important thing to focus on and I took him very seriously. Recently, my husband also got his skin checked by him, so I got to shake his hand and thank him.
The first doctor I saw spent five minutes with me. The second physician assistant that I saw spends 20 to 30 minutes with me. He even said to me, “You can’t give good care in seven minutes,” which apparently is the average they spend with you in the room. It was a doctor I had seen for the first time, so I hoped for a bit of a longer of a visit. I was pretty upset.
I feel very in tune with my body. I trust my intuition a lot. I had a mom who erred on the side of hypochondria, so I have always erred on the opposite side and never worried about little things in medical stuff, but I truly feel when I know something’s wrong, something’s wrong. I trust my gut wholeheartedly now.
I was upset and it took me a few months, but I eventually wrote that doctor a letter and let her know my case. She wrote back a very kind letter, apologizing and thanking me for letting her know, and let me know that she would pay more attention and be more careful in the future. It felt good to get that off my chest. It felt nice and her response was nice. There were no excuses. She just apologized and I appreciate an apology that is heartfelt, so it was nice.
The moment everything changed
I will never forget it. It was a Friday and I was trying to watch a movie with my family. The phone rang and I remember thinking to myself, “Stay present. Don’t answer the phone.” Then it rang again. It was a number I didn’t know. I have a little trigger response from the losses I’ve experienced when the phone rings repeatedly. I talked myself out of answering. Then I noticed the time and day. It was a Friday at 5 o’clock, which is when doctors tend to call.
I didn’t remember the biopsy, but when it rang a third time, I decided to check the message. I paused the movie and told my husband I needed to make a phone call. Sure enough, it was the doctor. He was incredibly kind and sweet. I put him on speakerphone, so he delivered the news to my husband and me. We didn’t know any staging, but we knew that it was serious.
My brain fast-forwarded to all the things I had coming up and all the things I needed to do. “I’m leaving in 10 days for a job in Mexico. Can I go?” He said, “I don’t think so.” His exact words were, “This needs to be the most important thing for you right now.” Of course, I somehow figured out how to still do my job in Mexico, but it went from a calm two days after Christmas to we need to go home and go to the doctor every day this week. Everything changed.
I had had a basal cell carcinoma removed from my face about 10 years prior, which was treated with a little bit of chemo cream. I had learned a little bit. I knew that melanoma was the scary one, but I didn’t know how scary and serious it could be and how much it could spread.
I started a deep dive. My sister-in-law sent me a book that I immediately read. My favorite book is called Radical Remission and it was an inspiring book to read. There are a lot of scary books out there. In this book, there were a lot of positive stories and different stories, so it was a good introduction to cancer. I went down the Google rabbit hole. I wanted to educate myself, so I started listening to audiobooks and podcasts, trying to learn as much as I could.
How I found my care team
I was given a team. Friends immediately said I needed a second opinion. I felt comfortable with my team. I didn’t know any different. I’m a part of an organization in Santa Cruz that I’m happy with. It felt comprehensive and personal. It felt good, so at that time, I didn’t feel any need for a second opinion.
We’re also very close to Stanford. I felt like I was in a good teaching hospital. If and when I need to go there, I will. I have established care over there since then. I feel like I have a very good team.
How surgery went
At the time, I was T2. They explained that it was hard to tell for certain because my biopsy was done by a shave, so they didn’t know the true depth until they went in. They explained to me how the surgery would go, that they were going to do a sentinel lymph node biopsy, and remove some of my sentinel lymph nodes in my right arm. My mole was right behind my right arm.
They explained it pretty well to me and then I followed up with some research. I would say I didn’t grasp how big the excision and how intense the surgery were going to be. The year prior, I had a hysterectomy and it felt invasive. The recovery is as bad as removing an organ and I didn’t expect that. In my mind, I thought they were going to cut and dig it out. It was a good chunk. I had armpit numbness and inability to use that arm.
They ended up finding cancer in one of my lymph nodes, which they removed, and there were still some things lighting up in that area, but it was more invasive than I realized. My husband saw me post-surgery and got very lightheaded. It was more than I expected, for sure.
I heard wide excision and I knew I had a plastic surgeon and a surgeon on the case, but I didn’t realize how big a surgery it was going to be. I saw him yesterday. They had to go all the way down to my muscle and underneath my breastbone. For the lymph nodes, they were in there more so than they had hoped, so he didn’t realize that either.
The cancer spread
January 15th was a bummer. They called us to talk about it in person. We didn’t even know that the staging could go up from there at that time. They explained the depth of mine. On a scale of 1 to 4, it was a 3.5. It was about as deep as it could go. It wasn’t ulcerated, but it was the nodular type, which was the most aggressive.
Later on, when I went to Stanford, I learned of the mitotic rate. The rate at which it multiplied was 10, so I was very high risk and very advanced. They explained my treatment plan. I would start immunotherapy in March. I would do 13 rounds spaced out by about three weeks, so it was supposed to take me a year. It’s going to take me a lot longer than we had planned.
I started in March. I did about four rounds and I’ve been on pause for the last nine weeks because of side effects.
What the mole looked like
It wasn’t that big. It was dark and raised, which you would notice for sure. I have freckles everywhere and covered moles. I’m a tough case. I wasn’t staring at it because it was on my back, so it’s not like I was watching it. I have others I look at and ask about, and they are wildly different from everything else on my body for sure.
At Stanford, they have a mole mapping program. They do full-body photography at some of these hospitals. For people who have a lot of moles, they scan your entire body and simulate it next time you come in, so they can see the growth in size and keep track. How can you keep an eye on several moles? I’m grateful for that technology, for sure.
My reason behind getting a second opinion
When you first get diagnosed, everyone has a lot of ideas, opinions, and suggestions. Everybody wants you to get the best possible care. I’m in a smaller town and I wasn’t sure how great the care was here. I thought that as soon as I had a bad feeling or if I had questions or doubts, I’ll go for a second opinion.
In the beginning, I felt on track, and then my dermatologist in Santa Cruz suggested it. She said, “Your skin is hard to keep track of. You’ll be in here every three months, but it might not hurt for you to go to Stanford.” As soon as she said the words, I said, “I would love that. I’d love to go over there.”
I feared asking for a second opinion, even though I know it’s very normal. Your doctors aren’t supposed to take it offensively, but I didn’t ask outright. She referred me to their melanoma center and got me established. I’m going every six months. I’m in there so that if I need further care, I can get it from them. It feels safe. I appreciate it.
I have a dear friend who has stage 4 cancer who’s also established over there. He has been my cancer guru. He’s communicated with his doctors about my doctors. He said, “It sounds like you’re in great hands.” He’s helped me navigate some of the systems as well.
I’m still going every day. I’m not doing treatment, but that doesn’t mean I’m not doing anything. I’m currently getting steroid infusions and IV hydration for all my side effects. I feel like I go to the doctor every day, so I’m very grateful that they’re close to home. It’s only a 20-minute drive for me. Stanford’s about an hour and a half, so it’s not too bad, but I’m grateful that I’m not there as often as the cancer center in Santa Cruz.
Treatment side effects forced a break
I developed colitis from the immunotherapy right away, as well as a full-body rash, extreme fatigue, thyroid issues, adrenal issues, and pre-diabetes. I learned that I had autoimmune issues coming into this. I’ve had Hashimoto’s and thyroiditis that were underactive my whole life, so I’ve been on synthetic medication. I’ve been told that there’s a tendency for people who have autoimmune disease to develop it that once you start immunotherapy, you have a higher chance of getting other autoimmune diseases. Apparently, about 25% of people get one of these side effects from my treatment and 4% get all five. I’m in that four percent.
They all came crashing down pretty fast. It was tolerable for a moment, but the colitis got so bad that I lost a lot of weight and wasn’t able to eat or do anything. I was going to the bathroom so many times a day. We did two rounds of steroids orally, but that didn’t work. I was doing daily infusions of steroids and I was very dehydrated from that. The IV hydration has been helpful.
We’re in a holding pattern of trying to get me down to a dosage where I can resume treatment. We got a second opinion and the conversation has been about whether we can stop treatment if we need to. The general consensus is no. We’re going to try and push through, but we have to get my body to a place where I can tolerate it.
How my life has shifted
I have a great support system. I have incredible friends who have shown up and sent me messages, photos, books, and things. I have started meditating in the mornings, which has been a game-changer for me as it allows me to focus on breath-work and calming my nervous system. My nervous system is so wound up from this year and the loss of my dog, so I’m trying to be calmer so that every experience is not as jarring to my body as it has been.
My days are pretty slow. I try to do yoga every day. What I used to do before 8 a.m. is about all I can do for the entire day. Now it’s like going to yoga, the grocery store, and getting my infusion, and then going home, which is a very successful day and is hilarious. I used to do that, go to work, and do other social things. If I have an infusion and go to yoga, there’s nothing I can do after 5 p.m.
It’s been a gift. It’s been a huge learning lesson. I won’t lie, the first six months of this year, I kept working. I didn’t stop. I figured out how to work in between treatments and pretended like everything was fine. I kept operating at my highly efficient level. When they told me that I had adrenal insufficiency and borderline adrenal crisis, I finally started listening. My body’s not handling this well and is mad at me, so I need to stop.
I was proud of how much I could do. If I wore it like a badge, I was like, “Oh, I can do 100 things in a day and then come home and still do all these things.” Now I’m just like, “Why did I feel like I had to do that all the time?” So I’m slowing down, which I have truly only done in the last two months and even more so in the last couple of weeks.
It took my dog getting sick for me to realize, when they told me he had about 2 to 4 months to live, that I don’t want to miss any of those moments and that made me start turning down work and staying home. I know that was his gift to me, getting me to a place where, once he was gone, I have to do this myself and focus on this.
Navigating my diagnosis with my partner
It’s changed us a lot. He’s been incredible. I feel like he’s been there with open arms. Fortunately, he works from home, so when there are appointments that I need him to go to with me, he will take the time and come with me. He has been supportive financially. He was working part-time very comfortably and took a full-time position as soon as I decided to go on disability. He stepped up and offered to take the brunt of all the things, so I didn’t have to worry financially.
He always checks in with me after appointments and asks how they went. When it comes to going to appointments with me, I battle with that because when in the beginning, I thought I could do it by myself. Then I started to realize that some of them were hard. You don’t always know when they’re going to be hard, so I had to share that with him. He was like, “Tell me when you want me to come.” I would go to these appointments and come out of them sobbing, and he would be like, “Why didn’t you ask me to come?” I’m like, “I had no idea that was going to go that way.” That has been a lesson for us both where I pick and choose.
If I have a funny feeling, then I ask him. I felt bad about it in the beginning because he was missing a lot of work, but now I say, “This one’s important,” and that’s it. He shows up. Sometimes we get him on video if we need to or something. He’ll be there at the drop of a dime for me.
Our whole life has obviously changed in terms of travel and commitments. We had to have some big talks about what our expectations were. We try to look at some of it as short-term and some of it as long-term, like not going anywhere for the next month. For us, it was the whole year. This is the year where we stay at home and focus on this. We can do weekend getaways. We love to travel. We’re both little adrenaline junkies with sports and things, so not skiing, surfing, or doing all those things is hard for us.
But we live in a beautiful place and we’re getting to spend more time at home and with friends. The quality of our time and where we spend it are very different. We have a wedding coming up in October and almost everybody is very understanding. We say we will be there, but my schedule could change. I want to make it to my nephew’s wedding more than anything in the world and I’m sure I will, but I’m nervous because I don’t have my treatment schedule and I don’t know what’s going to happen. We have that flexibility between the two of us and allows him to do things on his own. I have a lot of girlfriends who will show up and spend time with me. If a girlfriend comes to town, I tell him to go do something.
I love to have something to look forward to. Fortunately, my husband is not a planner. He’s very go with the flow and a last-minute Larry. I joke that he’s the Zen master Buddha because he’ll just do whatever. It’s been a huge lesson for me because I don’t operate that way. Meeting somewhere in the middle is probably the healthy approach.
But the way I’ve been looking at the future has been in shorter chunks. With work, I used to look one year ahead, five years ahead, and have all these big goals and plans that I’m not doing at the moment. Now, I’m staring at my feet, trying to get one foot in front of the other. I’m readjusting my brain and learning how to take one day at a time, but still allowing myself to have little things.
We went to Tahoe this past weekend. We saw some friends and having that on the calendar for two months, I thought, “If we make it, we make it.” The day before, we almost didn’t make it because I had infusions that day and didn’t get scheduled until the day before. I thought I might feel horrible. Friends who understand have been wonderful, but we made it and I had a great time.
Now we have nothing on the calendar until the wedding in October. I still allow myself little things to look forward to, but the month of September is for me to focus. I’m probably getting a port in the next couple of weeks, so I know I have that surgery coming up. I take it day by day. I wake up and try to get to yoga.
I didn’t know how difficult I would be. They did a vein check on me, looked at me, and said, “You’re great,” even though the phlebotomist hates me. I average 3 to 5 sticks every single time. I’m covered in bruises, with the hydration and the steroids. The nurses have been telling me for months to do it and I kept thinking, “I don’t want to do another surgery.” But now that my treatments are pushed until February, I’m nowhere near done, so I might as well. I’ve asked a lot of people and they have said they were grateful. I haven’t heard anything negative about it, so I can still have my life and do all the things.
What I want people to know
What has stuck out for me is to trust your gut and your intuition. Our intuition is so spot on when you’re in tune with your body, whether you’re not feeling well or something doesn’t feel right. I’ve gotten a lot better at advocating for myself.
Knowledge is power. I know I’m not a doctor and I don’t know the specifics, but understanding your type of cancer, type of treatment, and your options is huge. We go into these appointments and get fed so much information so fast that we take it as the Holy Grail. We don’t always know what our options are. Always go in with a list of questions and write down answers to questions. Try to have a very comprehensive understanding of what’s going on.
I was told to tell my story to the doctors at Stanford, so I reiterated my case and they were like, “Wow.” Even my husband was like, “Wow, that was impressive.” They said, “You’ve done your homework.” It feels good because then I can understand when they send numbers, names, and details. Fighting for myself is something I’ve learned a lot.
How I’ve supported my body
I have radically changed my diet and focused on things at home that can help heal myself. I’m dealing with cancer, but at the same time, I feel like I’m healing my body in a way that it’s always wanted, even outside of cancer. I was trying to reduce the inflammation in my body already and this was a catalyst. Weirdly, I feel like the things I’ve been doing have been so supportive and integrative that my body’s oddly happy. I can tell my body is like, “Oh, thank you. This is the care and concern that I’ve always wanted.”
There were things I always wanted to do, but it felt so hard to make big changes in my diet. Do simple things, like getting rid of processed foods. None of us should be eating crap, but it’s so easy and accessible. I’m feeding and nourishing my body well. It has been something that has felt so good and something that I felt so proud of, that I wish we all did, regardless of cancer. Getting slapped with the C-word is a bigger incentive, but I am proud of the healthy changes I’ve made in my life, which has been the silver lining in all of this for me.
I’ve taken certain foods out of my diet. I have stopped drinking and stopped eating all processed foods. I’ve stopped eating red meat. I don’t do any cow products. I’ll do some goat and sheep, some game occasionally, because I’m pretty deficient in iron. I’ve switched to completely organic. I juice every day.
I take a lot of supplements that I’m deficient in. I’m bad at taking vitamins, so my supplements are little droppers of vitamin D, B12, iron, folate, and all those kinds of things. I put them straight in my green juice in the morning and I drink that. I’ve enjoyed juicing, as nerdy as it sounds, but it’s become meditative. It’s my thing. Every Sunday, I get all my veggies ready.
I have a garden. I don’t grow all of it, but we get vegetables from a local community supported agriculture (CSA) box and that feels great, that all my veggies are coming from close by. I try to get my food as close to home as possible. The meat and vegetables all come from local regenerative farms. I’ve decided that the money I’m saving on alcohol and all the other crap gets to go into good food, fruits, vegetables, and meat, and keeping that close to home.
I’m off sugar. I’m doing honey and maple syrup, and that was the hardest for me. Alcohol was no problem. Processed meat was hard because I loved sausages, but when I took out sugar, I felt like a crazy person. It took me months, but now I’m here. Once a month, if I go out to dinner and someone gets dessert, I’ll have a bite or two. It tastes delicious and wonderful, but it tastes too sweet.
I freeze bananas and cover them in a sugar-free non-dairy chocolate. My sweet tooth is completely gone, which is amazing. Now I have a bite of a real dessert and I’m like, “Whoa!”
Getting rid of all the artificial sweeteners and caffeine is a new one. I was doing caffeine for the first six months and when my adrenals got shot and I stopped working, I was like, “Why do I even need caffeine?” It’s a habit that I had to break. Occasionally, I’ll have a chai tea, but for the most part, I’m off caffeine.
Drinking tea every night has become an awesome ritual that I love. I was never a big tea drinker, but the practice of making it, drinking it, and going to sleep after has been nice. All those things have felt supportive. I feel like I’m helping my body through this process. It’s hard on my body and if there was anything else inflammatory going on in my body, if I was trying to fight it with all that crap, you’re adding insult to injury and making it harder on yourself.
I feel like I have this very clean vessel to soak in the medicine and help myself heal, which has been my favorite part. I got a lot of cancer-fighting and anti-inflammatory cookbooks and found new ways to make dinner for my husband and myself. I’m sure there are things he misses that I’m not making. But fortunately, we were both already gluten-free and have gone dairy-free as well. He’s been on board with that, but I still make a steak every now and then.

Inspired by Cheyenne's story?
Share your story, too!
More Melanoma Stories
Brittanny G., Skin Cancer (Melanoma), Stage 3A
Symptoms: Mole that enlarged, changed shape, and became dry, patchy, and flaky, fatigue
Treatments: Surgeries (wide local excision, lymphadenectomy), immunotherapy
...
Teresa B., Recurrent Breast Cancer (Hormone-Positive), Oral Cancer (Lip Cancer), and Skin Cancer (Melanoma)
Symptoms: Lip cancer: chapped lips & a pimple-like growth on lip, breast cancer: enlarged left breast with lump, melanoma: none
Treatments: Surgeries (bilateral mastectomy with reconstruction, lumpectomy, craniotomy, Mohs, surgery, wide local excision), hormone therapy, radiation therapy
...
Jennifer M., Melanoma, Stage 4 (Metastatic)
Symptom: Persistent cough, body and chest aches and pains, night sweats, fatigue
Treatments: Immunotherapy, surgeries (lung resection, pericardiectomy)
...
Cheyenne E., Melanoma, Stage 3B
Symptom: Itchy mole on her back that changed in appearance
Treatments: Surgeries (wide local excision, sentinel lymph node biopsy, lymph node removal), immunotherapy
...
Robin A., Melanoma, Stage 4
Symptom: Appearance of a small bump on the chest
Treatments: Chemotherapy and immunotherapy (under a clinical trial)
...
Megan S., Melanoma, Recurrent (Stage 1A & Stage 4)
Symptoms: New mole, cough, wheezing, chest pain, back pain
Treatments: Surgeries (mole excision, reconstructive surgery, thoracic surgery), immunotherapy, targeted therapy (BRAF inhibitors, MEK inhibitors), radiation therapy
...