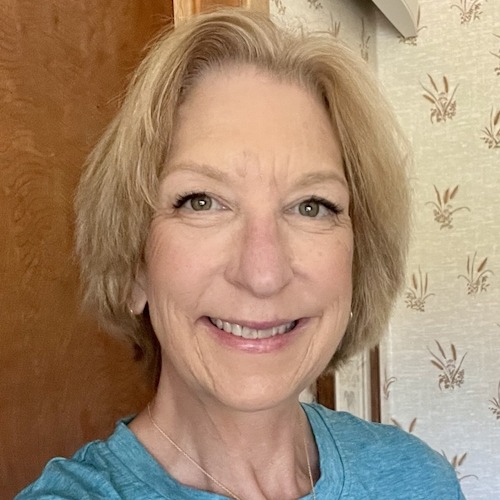
Leah’s Stage 4 Non-Small Cell Lung Cancer with EGFR exon 19 Deletion Story
Interviewed by: Taylor Scheib
Edited by: Katrina Villareal

Leah was diagnosed with stage 4 non-small-cell lung cancer (NSCLC) with EGFR exon 19 deletion at 43. Initially misdiagnosed with a post-viral cough and exercise-induced asthma, her persistent symptoms led to multiple doctor visits and treatments. Despite these efforts, her condition worsened, culminating in a CT scan that revealed metastatic cancer with a bone biopsy confirming stage 4 NSCLC.
Leah began treatment with Tagrisso (osimertinib), a targeted therapy that significantly shrank her primary tumor and healed bone metastases, and also underwent SBRT radiation. Although she faced side effects like gastrointestinal issues, a rash, skin and nail issues, and mouth sores, she remains stable with no progression in her lungs and continues her treatment at Vanderbilt-Ingram Cancer Institute.
Emphasizing the importance of self-advocacy and seeking second opinions, Leah recounts her insistence on further testing and comprehensive care. Her husband’s previous cancer diagnosis highlighted the necessity of thorough medical evaluation. She stresses the importance of enjoying daily life and finding inspiration and new beginnings even after a terminal diagnosis.
- Name: Leah P.
- Diagnosis:
- Lung Cancer
- Mutation:
- EGFR exon 19 deletion (E19del)
- Staging:
- Stage 4
- Symptoms:
- Persistent dry cough
- Shortness of breath
- Heaviness in the chest
- Coughing up blood
- Weight loss
- Right rib pain
- Right shoulder pain
- Treatments:
- Chemotherapy
- Targeted therapy
- Radiation: stereotactic body radiation therapy (SBRT)

This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider to make informed treatment decisions.
The views and opinions expressed in this interview do not necessarily reflect those of The Patient Story.
Introduction
I was born and raised in Louisville, Kentucky, but now live right outside of Louisville. I’ve been a stay-at-home mom for 19 years now. My oldest is 19 and I also have a 17 ½-year-old daughter and an almost 14-year-old son.
In December 2019 at 43 years old, I was diagnosed with stage 4 non-small-cell lung cancer (NSCLC) with a driving mutation of EGFR exon 19.
Pre-diagnosis
Initial Symptoms
In mid-September 2019, I started having persistent dry cough. I didn’t think anything of it, but after about two weeks, I went to my primary care physician because the cough wouldn’t go away. She diagnosed me with what she called a post-viral cough and put me on a steroid. In about a week or so, I started feeling better.

‘I’m feeling worse. Now I’m feeling tired. I’m still coughing, I have a heaviness in my chest, and I feel as if I may have pneumonia.’

Symptoms Worsen
A few weeks later, the cough came back. I also started having shortness of breath. I was a distance runner for many years and I would run 8.5-minute miles with my running group while talking the entire time. I started noticing that I could keep up my pace, but I couldn’t keep up the conversation without feeling winded.
When I went back to the clinic, I saw a different doctor and told him I felt a heaviness in my chest, especially when running. He told me that I had exercise-induced asthma. I know my body and I’ve never had this issue before, so why is this suddenly an issue?
I saw an allergist and he said it wasn’t asthma. I went back to the same doctor, who wasn’t my first choice but was the one available, and said, “I’m feeling worse. Now I’m feeling tired. I’m still coughing, I have a heaviness in my chest, and I feel as if I may have pneumonia. Can I have a chest X-ray?” He said I didn’t need it because I sounded like I was breathing fine. I asked him to do it to make me feel better.” He said, “I’ll do it, but I’m going to call you in 45 minutes and tell you it’s negative for pneumonia. This is either allergies or asthma.”
Forty-five minutes later, he called me and said, “You know what, I can’t believe I’m admitting this, but you have consolidation in your right lung, which means you have pneumonia.” He put me on a Z-Pak and a steroid.
Halfway through the Z-Pak, while at my daughter’s swim meet, I kept feeling worse and worse. When we got back home that night, I started coughing up blood. I thought this wasn’t right. On Monday morning, I called the doctor to let him know what was going on. He thought I needed a stronger antibiotic and more steroids. Every time I was on steroids, I felt better, but I still thought this wasn’t right.

I could hardly walk up the steps without having to sit down because I couldn’t breathe.

Hospitalized for Pneumonia
About mid-November, I went back to the doctor and said, “Can you please do another X-ray? Clearly, this pneumonia is not going away.” They did and it still showed right lung consolidation. They admitted me to the hospital for 4 days to be on round-the-clock IV infusion, high-powered antibiotics, and steroids. By the time I left, I felt pretty good because I had been on steroids through IV.
While I was there, the pulmonologist came in and said, “I’m going to do a bronchoscopy. We’re going in through your nose, down through your throat, and into your lung to look around with a camera and flush it with saline. If I see any masses or nodules, we’ll go ahead and biopsy them.” He did that and everything looked great.
He said, “There’s consolidation in your right lung. It’s residual pneumonia. Pneumonia can hang around for several weeks. I didn’t see anything unusual.”
Seeing a Nurse Practitioner
I could hardly walk up the steps without having to sit down because I couldn’t breathe. I was having right rib pain and right shoulder pain. I was coughing, lost weight, and looked awful.
I called the doctor’s office and they said they didn’t have any appointments, so I drove there and cried to the ladies at the front desk. I told them there was something seriously wrong with me and I needed someone to see me. They ignored me a bit, so I said, “I’m not leaving until someone sees me.”
They sent the nurse practitioner out, but that was more for a mental wellness check because I think they thought I was losing it. She sat down and listened to everything I had been through. I had written down dates and times. She said, “Something’s not right about this. You know your body. I’m going to send you to the hospital for an outpatient CT scan.”

She said, ‘There are some things on your CT that are a little concerning… we need you to go to the emergency room to be admitted to do further testing.’

Getting the CT Scan Results
I got a CT scan while I was in the hospital. After I got home, my original primary care physician called me and kept asking, “Are you having any back pain?” I said no. She asked a few other questions and I explained I had a cough, heaviness in my chest, and shortness of breath.
She said, “There are some things on your CT that are a little concerning. I’m not that worried, but we need you to go to the emergency room to be admitted to do further testing.”
Going to the Emergency Room
My mom and I went to the emergency room. After waiting for my husband to get there, we saw the doctor, who said, “Have you seen your CT results?” This was before test results arrived in real time on MyChart. He showed me the computer screen and said, “This is what we’re concerned about.” It said, “Lytic lesions present on T4 and T5. Highly concerning for metastatic cancer.”
I read that to my husband and mom, looked at the doctor, and said, “That means cancer that spread from where it started.” He said, “Yes, ma’am, you’re correct.” I said, “I don’t understand. What’s going on?” He said, “I don’t know, but we’re going to admit you and figure out where this cancer is coming from.”
They admitted me to the hospital and called in a pulmonologist because I had fluid in my right lung. They said that could be a sign of breast cancer or ovarian cancer, given my age, health, and that I had never smoked.

None of us knew that you could get lung cancer without smoking.

Getting a Thoracentesis
The hospitalist came in and called the pulmonologist to do a thoracentesis to remove some of the fluid from my lung to test for malignancy. Within 24 hours, the test came back as malignant, but it didn’t indicate where it was coming from.
Spinal Biopsy
They sent an oncologist over and he opted to do a bone biopsy of my spine because it was the easiest place to reach.
Diagnosis
Official Diagnosis
When the bone biopsy came back a day or so later, it said stage 4 non-small-cell lung cancer. You could have knocked us over with a feather because none of us knew that you could get lung cancer without smoking.
The oncologist told me that I had 6 to 12 months to live and that I needed to get my affairs in order. I was 43 with young kids. My husband asked him to leave the room, never come back, and to send a different oncologist.
Biomarker Testing
The second oncologist that came in was one of my husband’s fraternity brothers. He said, “I’m not going to say 6 to 12 months yet because you’ve never smoked and you’re healthy. You may have a biomarker or a gene driving this lung cancer, so we need to do biomarker testing.” It was the first time we ever heard of that. I tested positive for the EGFR exon 19 deletion mutation.
How can you tell me that I have metastatic cancer and I’m going to die?

Reaction to the Diagnosis
I burst into tears, thinking this couldn’t be happening. Metastatic cancer is what you die from. I ran the morning that I was admitted to the ER. Even though my breathing was so bad, I still ran 3 miles, so how can you tell me that I have metastatic cancer and I’m going to die when I’m still doing these things? I remember sitting there and crying, “My job is not done here. My job cannot be done here. I still have life to live. I still have kids to raise.”
Treatment
Tyrosine Kinase Inhibitor
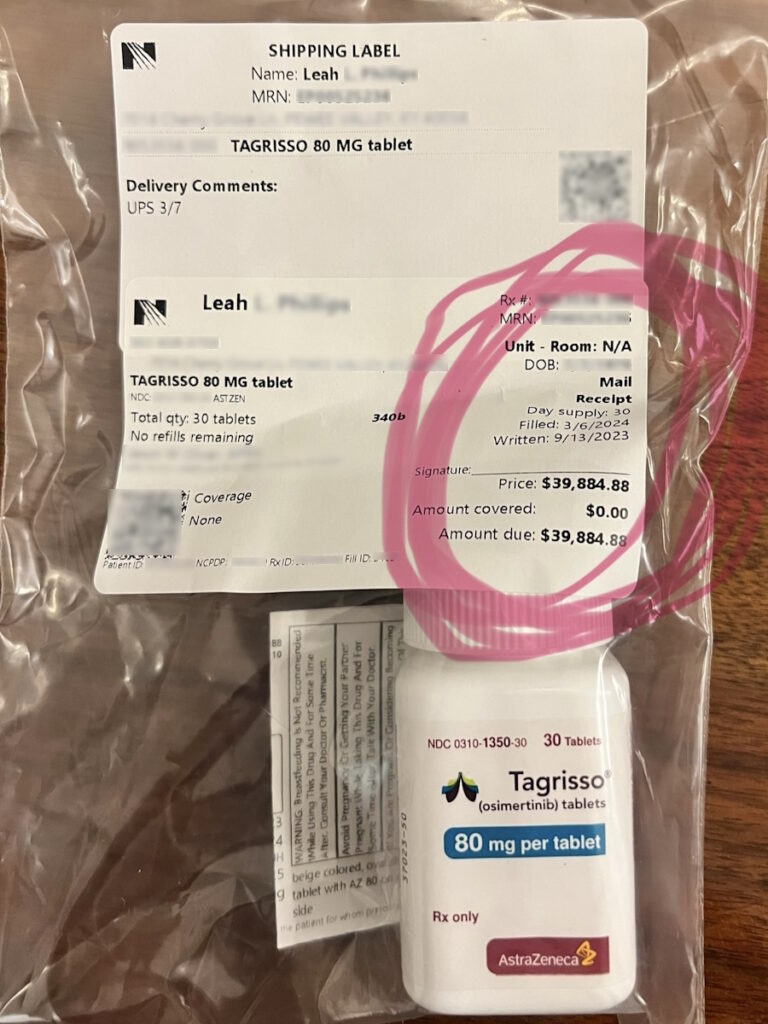
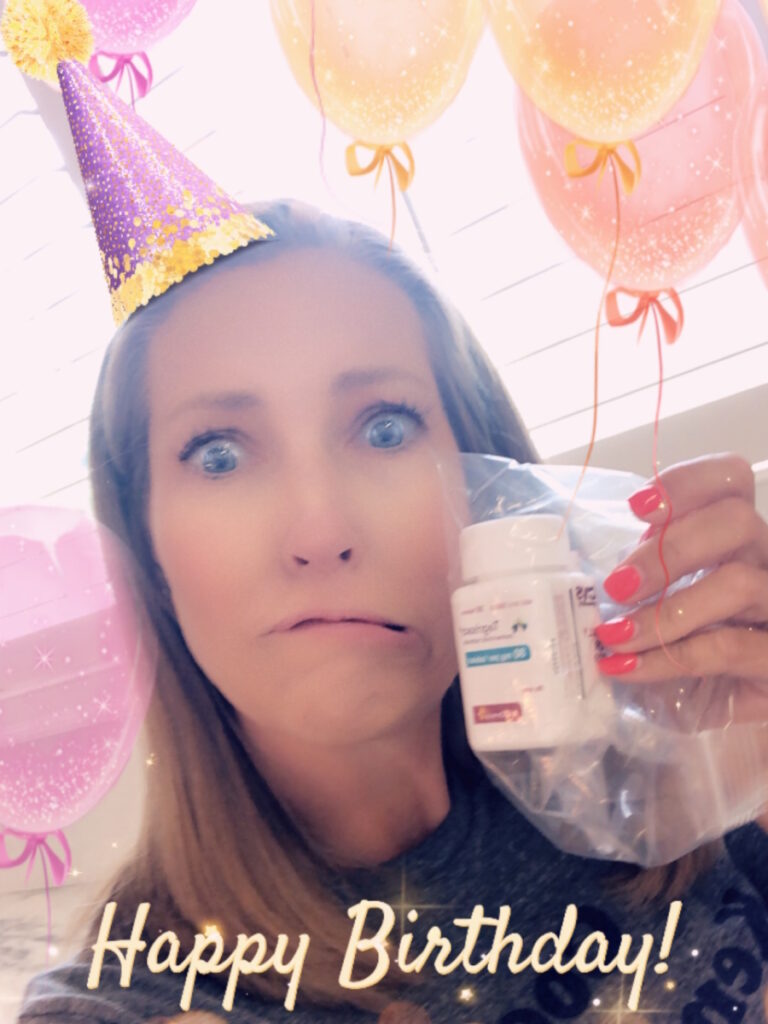
I went to see the local oncologist and was prescribed Tagrisso, which is a targeted therapy (tyrosine kinase inhibitor) for my genetic marker. He had a sample, so I was able to start immediately.
The only places my cancer had spread was to my spine and pelvis. I had one primary tumor in my right middle lobe and about 13 bone metastases in my spine and pelvis. About a year into my treatment, all those bone metastases were sclerotic, meaning they were healing, and my primary tumor had shrunk by 70%.
SBRT Radiation
We wanted to be aggressive and asked what else we could do. They introduced us to a radiation oncologist at the end of November 2021. In the beginning of December, I had eight sessions of SBRT radiation, which is strong, high-powered, and precise, to the primary tumor in my right lung.
About a year into my treatment, all those bone metastases were sclerotic, meaning they were healing, and my primary tumor had shrunk by 70%.
Side Effects of Tagrisso
When you’re prescribed Tagrisso, they give you a laundry list of possible side effects. The most common are gastrointestinal, which is diarrhea, and what they call the Tagrisso rash. You can get it anywhere, but it’s primarily on your face and looks like bad acne.
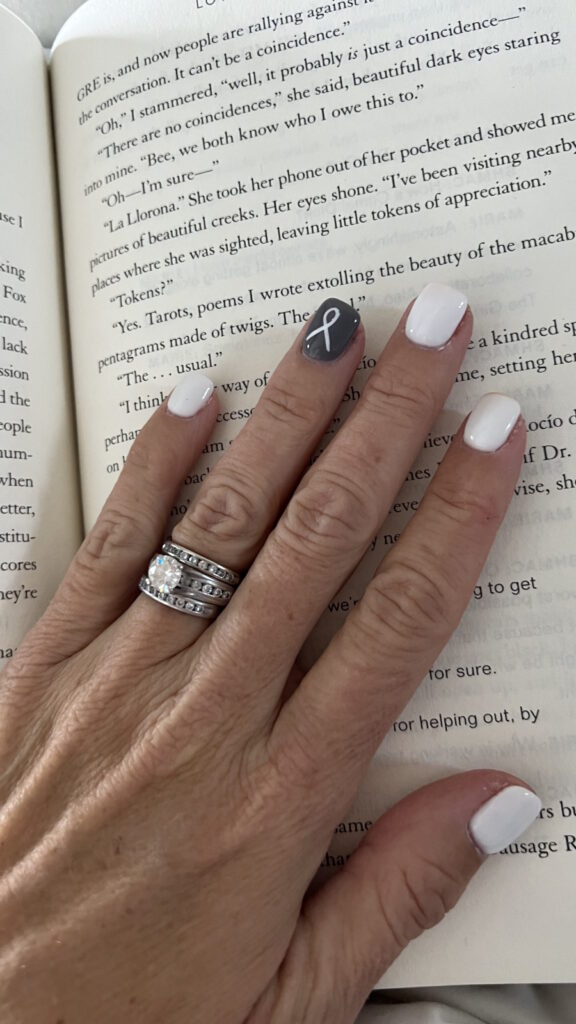
The next most common side effects are skin and nail issues around nail beds because Tagrisso is so drying. You get splits around your nails and they become paper thin. You get little paper cuts, but they hurt worse in the fingers and toes. They also told me to expect some nausea.
When I first started taking Tagrisso, I didn’t have diarrhea as much as I got the rash. I also had zero appetite. Food didn’t taste right, so I was forcing myself to eat. That lasted about two weeks.
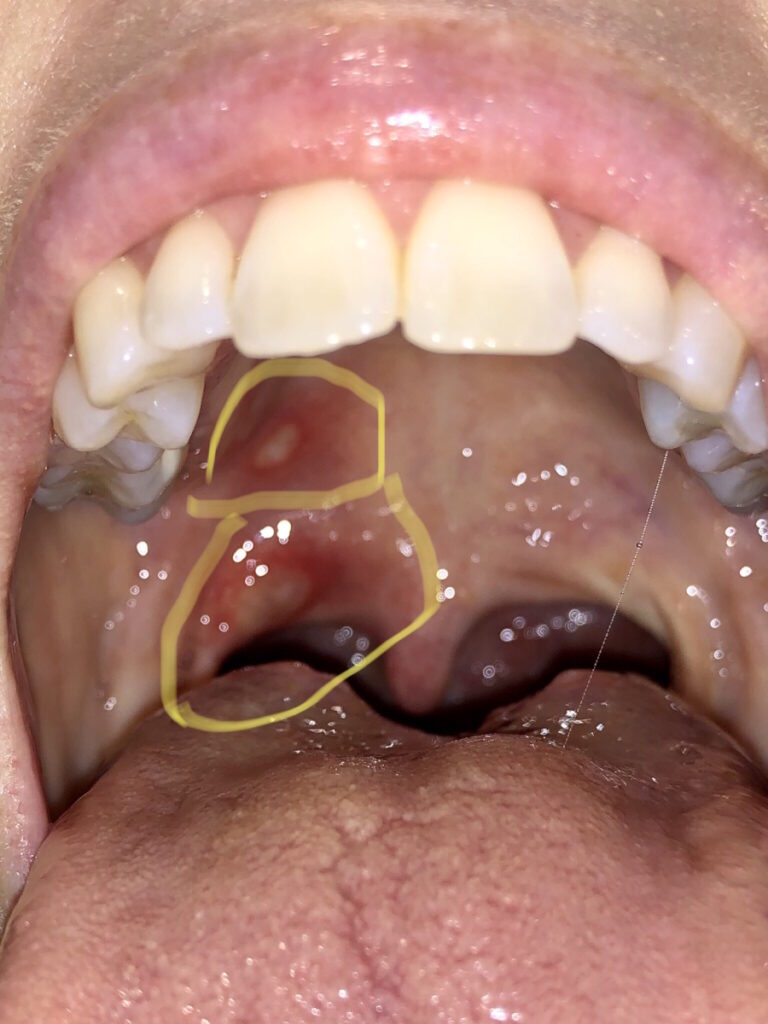
Another possible side effect but not as common are mouth sores. For whatever reason, those came with a vengeance. The first time I got them, they were everywhere in my mouth and on my lips. Some of them were the size of a quarter. They prescribed a specific mouthwash, but I met an oncology dermatologist who is amazing and gets things under control.
Importance of Self-Advocacy
When I was admitted to the floor, I was still in a state of shock, saying the same things over and over, and crying. The nurse practitioner who was getting me situated broke into tears. She apologized and said, “I’m so sorry. I’m being unprofessional. I have kids your age and I understand what you are going through. I must leave the room.” She came back and said, “I’m so proud of you for standing up to these doctors.”
In some ways, I was so disappointed in the medical community. What if I wasn’t educated? What if I didn’t stand up for myself? What if I didn’t have the financial means or the insurance to keep coming back? Those are the people my heart breaks for.

Advocate for yourself and if you don’t feel like you can, find somebody who will advocate for you.
Being dismissed has never been my style. I’m not confrontational, but once I’m passionate about something, I will stand up for what I believe in.
I knew I deserved better care than what I was getting. I knew there was something wrong and we were going to get to the bottom of it.
It’s very easy to put your head in the sand because you don’t want to hear the real story and get the diagnosis. You have to advocate for yourself and if you don’t feel like you can, find somebody who will advocate for you.
Importance of Getting a Second Opinion
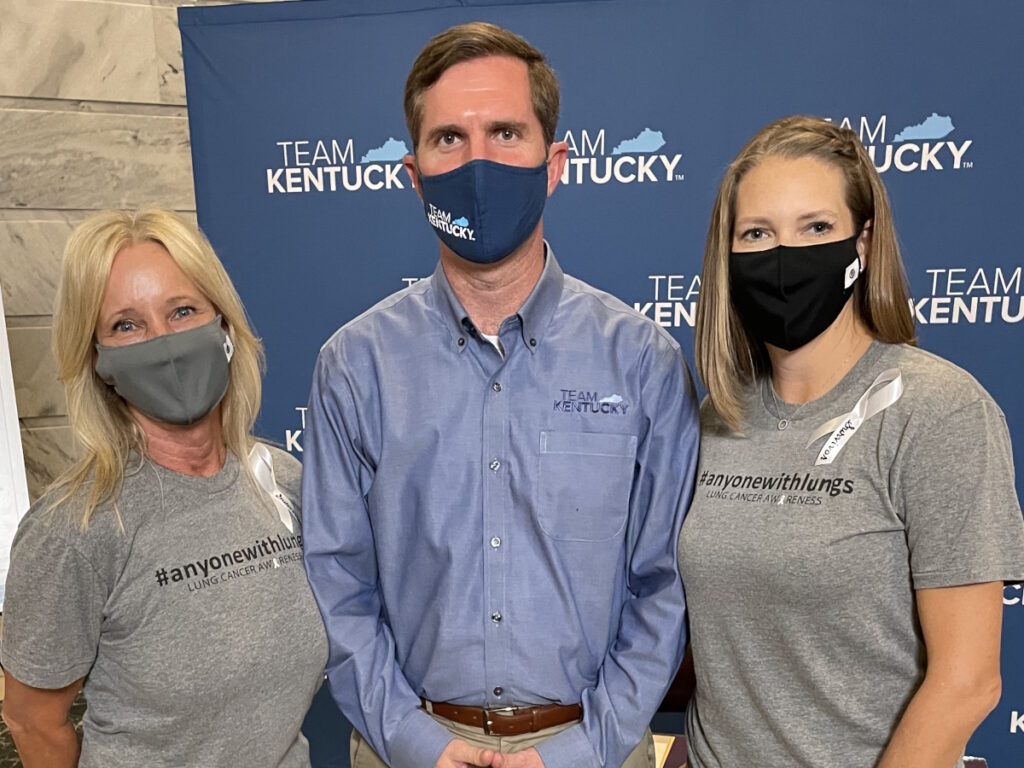
My husband was diagnosed with prostate cancer 18 months before I was diagnosed. That cancer has been taking men in his family for years. Todd’s been cancer-free for 6 years now and he’s great. We knew the importance of seeking a second opinion when he was diagnosed. A second opinion is not a luxury. It’s not a maybe. We didn’t even have a conversation; we knew that was what we needed to do.
As soon as I was diagnosed, my husband was emailing and calling people he knew in the medical field. He doesn’t work in the medical field, but he was asking, “Where do we need to go? What is the best place? We don’t care if it’s international; tell us and we’re going.” That’s how we ended up at Vanderbilt-Ingram Cancer Institute.

I could sit here and dwell on the fact that more than likely, this will end my life earlier than it should or I can choose to live my best life one day at a time.

I’m not going to be in remission. I will never be cured. If you look at lung cancer statistics, 5% of people are still living in 5 years. From day one, I said I will be one of the 5%. Somebody has got to be one of them. Those statistics are so outdated and so skewed. There’s a whole new population of younger lung cancer patients who are being diagnosed under age 50 with genetically-driven mutations and have never smoked.
This puts us in a totally different ballgame than people who are at an average age of 65 with a history of smoking. That’s not to say that I’m any better or my lung cancer is more important. It’s just different. It’s like comparing BRCA breast cancer with HER2 breast cancer. They’re two different types of cancer and we must treat them differently.
Saying I’m not a smoker is not to isolate or make someone feel guilty for the choices they made. No one deserves cancer. I don’t care if they’ve smoked a thousand cigarettes. No one deserves this, but it does put us in a different position for treatment. Everyone should get a second opinion on something this important.
Living a Day at a Time
This is a cruddy hand to be dealt. I could sit here and dwell on the fact that more than likely, this will end my life earlier than it should or I can choose to live my best life one day at a time. That has always been my motto. Every day can be your best day. Some days are better than others, but enjoy the simple things, whether it’s getting to watch your child play a sport or simply having 45 minutes to yourself to read a book.
If I’m going to go through this, I want to be able to help the people behind me. A good friend and I were talking about this and we agreed that it’s always good to have someone ahead of you that you can look to for what’s coming down the road. It’s always good to have someone walking the path next to you who understands what you’re going through. It’s always good to have somebody behind you who you can help lead.

It’s not a matter of if I progress; it’s a matter of when… I’m still getting a response, so I’m technically on borrowed time.
Current Status
Since I started treatment, I’ve had four thoracenteses done to drain fluid. I’ve had numerous PET scans and CTs of my chest and abdomen, which I do every 3 months. I also switched my primary care to Vanderbilt University because it’s a comprehensive care center.
I have remained stable with no progression in my lungs at any of the sites where I had metastases. I take Tagrisso every day and I’m staying on that protocol until I progress. It’s not a matter of if I progress; it’s a matter of when. The average patient can take Tagrisso for 2-3 years with a response. I have been on it for 4 ½ years and I’m still getting a response, so I’m technically on borrowed time.
There’s no official next step. They would redo biomarker testing to make sure I did not develop any other mutations or it hasn’t changed to small cell lung cancer. At that point, we would discuss our next options. Do we radiate depending on how many spots I progress in? Do we add IV infusion chemotherapy to the oral targeted therapy? Do we add another targeted therapy? What we would do is unclear because lung cancer is ever-changing.
Words of Advice
Statistics are not always right and just because it statistically says something does not mean that you’re going to be that statistic.
I firmly believe in alternative modalities to help with the emotional, mental, and physical side effects. I see a Reiki therapist every eight weeks. I get a therapeutic massage every other month. I listen to sound bowls. Maybe they’re working, maybe they’re not. If it’s not going to interfere with your treatment and makes you feel better and live a better life, then it’s worth trying.
Second opinions are priceless. I’m trying to honor each day as a new day and a new gift. No one is guaranteed to live forever. For some of us, it’s going to be sooner than others. We need to remember that, enjoy the small things, and try not to sweat the little things.

Life is not over when they tell you that you have a terminal diagnosis. It’s just the beginning.
We taught our kids that there’s a difference between a small problem and a big problem. A small problem is when they forgot to put ketchup on your burger. A big problem is cancer. A small problem is being disappointed that you didn’t get an A on a test and you got a B; a big problem is cancer.
There are a lot of life lessons that come along with a cancer diagnosis. As many bad things come with this, there are some very good things. You find out there are some good people out there. You make new friends. You become an inspiration to people. Life is not over when they tell you that you have a terminal diagnosis. It’s just the beginning.

Inspired by Leah's story?
Share your story, too!
More Lung Cancer Stories
Maggie M., Non-Small Cell Lung Cancer, EGFR+, MET Amplification & Overexpression, Stage 4 (Metastatic)
Symptoms: Ocular migraines (kaleidoscope vision), partial blood clot (DVT) in the leg, vision and balance problems, minor chest pain
Treatments: Targeted therapy (tyrosine kinase inhibitors or TKIs), radiation therapy (stereotactic body radiotherapy or SBRT), clinical trials, chemotherapy (combined platinum-based regimen)
Clara C., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptoms: Pelvic pain and discomfort, bladder issues related to pelvic tumors, incontinence, pain in the lower back and hip
Treatments: Chemotherapy, immunotherapy, radiation therapy, targeted therapy (lorlatinib)
Shira B., Lung Cancer, EGFR+, Stage 1B
Symptoms: None per se; discovered during a preventative full-body MRI
Treatment: Surgery (thoracotomy)
Phil P., Non-Small Cell Lung Cancer, ROS1+, Stage 4 (Metastatic)
Symptoms: Persistent cough, nasal drip, shortness of breath, inability to speak in full sentences
Treatments: Chemotherapy, targeted therapy, radiation therapy, next-generation ROS1 inhibitor (clinical trial)
Stephanie K., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptoms: Persistent and intense cough, general feeling of sluggishness
Treatments: Chemotherapy, targeted therapy through a clinical trial, radiation therapy