Ben’s Myelofibrosis with CALR Mutation Story
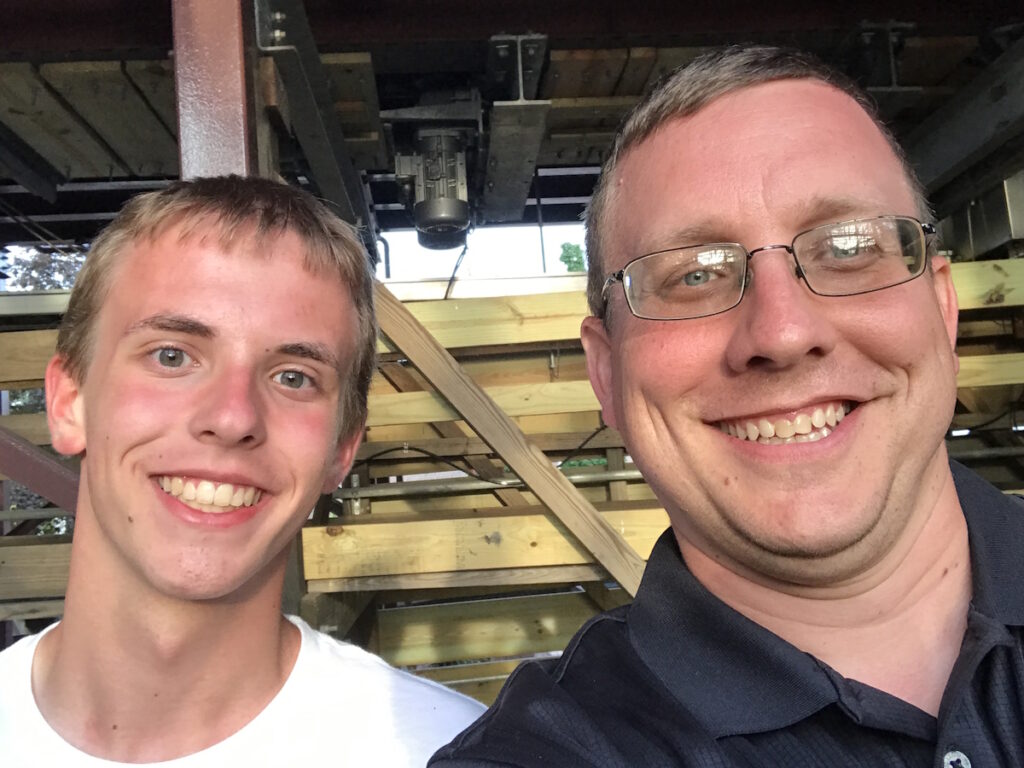
Interviewed by: Taylor Scheib
Edited by: Katrina Villareal

Ben was diagnosed with essential thrombocythemia in 2012 and myelofibrosis in 2023. His ET was discovered during a pre-employment exam that revealed high platelet counts. Initial treatment with hydroxyurea managed his condition, though he experienced kidney issues. Seeking more information, Ben educated himself about ET and later learned about the CALR mutation through a second opinion.
As his symptoms intensified, Ben’s care was transferred to a new hematologist, leading to a myelofibrosis with CALR mutation diagnosis in 2023. Despite significant scarring in his bone marrow, his treatment remained largely unchanged. With an increased symptom burden and feeling unhappy with his doctor’s response, Ben sought a second opinion. His new doctor switched him to ruxolitinib, significantly improving his quality of life.
Ben became an advocate for himself and others, emphasizing the importance of seeking second opinions and connecting with specialists. He joined the MPN Research Foundation’s Patient Impact Council, connecting with other patients and professionals. Grateful for the support from his family, medical team, and the myeloproliferative neoplasms (MPN) community, Ben continues to advocate for better patient education and support. He stresses the importance of patient advocacy and utilizing available resources for support and information.

Thank you to Sobi for its support of our patient education program! The Patient Story retains full editorial control over all content.
This interview has been edited for clarity and length. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
- Name: Ben H.
- Diagnoses:
- Essential Thrombocythemia (ET)
- Myelofibrosis (MF)
- Mutation:
- CALR (calreticulin)
- Initial Symptoms:
- None; caught at a routine blood test
- Treatment:
- Hydroxyurea & aspirin
- Ruxolitinib
I have myelofibrosis [with CALR mutation] but, other than that, I’m healthy and can enjoy things.

Introduction
I’m married with two kids. My oldest is in college and my youngest recently turned 16. They certainly keep me busy along with other family activities.
I was diagnosed with essential thrombocythemia (ET) in 2012 and with myelofibrosis (MF) in 2023.

When I first was diagnosed, there wasn’t a lot of information provided. I was told I had ET and what it was. I did a lot of research on my own.

Essential Thrombocythemia
Initial Symptoms
I found out about it by chance. I had recently switched jobs and was going through pre-employment exams. My blood test results showed that my platelets were extremely high, about 1.2 million at the time. My platelet count was anywhere from 1.2 to 1.5 million. It didn’t keep me from being employed, but they recommended that I follow up on it. I had initial follow-ups with my primary care physician who recommended that I see a hematologist.
Official Diagnosis
I went to a local hematologist from where I’m from, which is a rural area. We did a bone marrow biopsy. They said I had essential thrombocythemia but at that time, they didn’t know the driver mutation.
Treatment
I began treatment with hydroxyurea. We were managing my blood counts and able to stay in the 600,000 to 800,000 range. It’s the sweet spot for me where we weren’t suppressing anything else too much. I managed with that for a number of years.
Side Effects of Hydroxyurea
It was pretty unremarkable at first, but I did have some significant side effects. Initially, I had issues with my kidneys. It was a learning experience for me. I needed to stay much more hydrated to keep everything flushed.

It didn’t feel like there was any plan. I didn’t know if there was anything I needed to watch for or if I needed to do anything differently.

Learning About ET
When I first was diagnosed, there wasn’t a lot of information provided. I was told I had ET and what it was, but I had to do a lot of my own research to figure out what it was and to explain the diagnosis and its impact to my family and friends. I was told that this would be something that I would die with not die from.
I didn’t think too much of it. I continued with the same hematologist for a period of time. There wasn’t a lot of interaction. It was mostly regular blood work and going to see the hematologist. I was kept on hydroxyurea and was told that we’ll adjust as needed. It didn’t feel like there was any plan. I didn’t know if there was anything I needed to watch for or if I needed to do anything differently.
Getting a Second Opinion
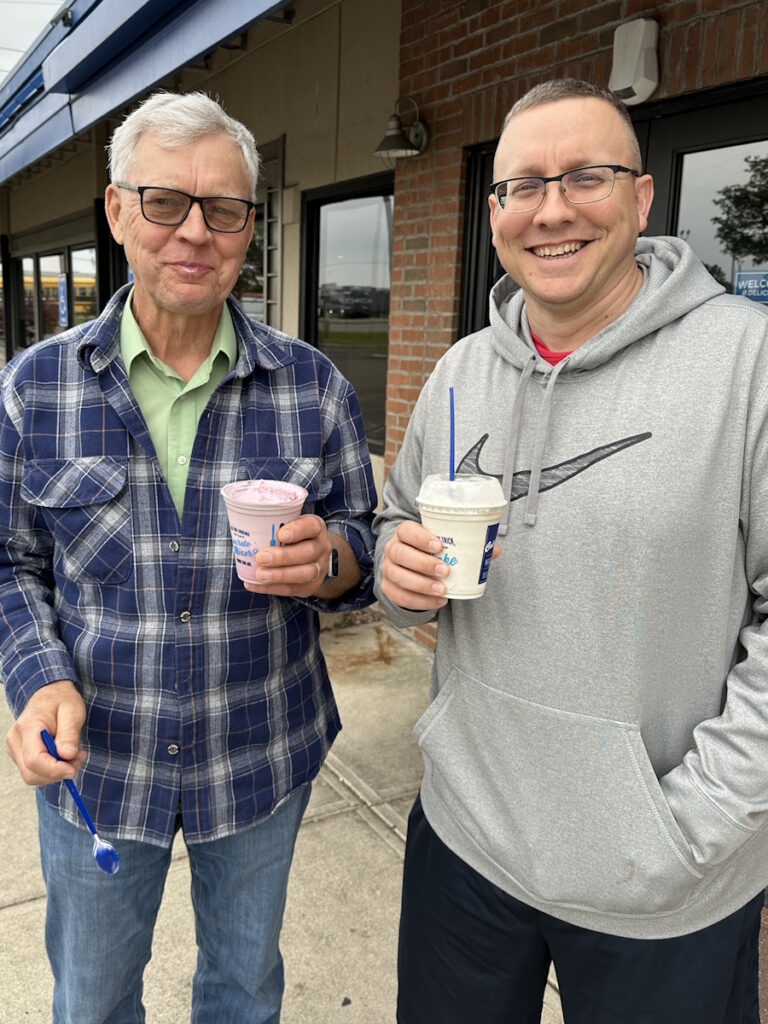
Fortunately, my dad had some contacts through his work. I talked to the head of the hematology group at the hospital that I was visiting and he said that if I wanted to get another opinion, he could hook me up with another location. This is a larger cancer institute that has people who deal more with some of these rare blood cancers.
I connected with a hematologist down there. A couple of years has transpired at this point. I met with the new doctor and went through everything. They got everything sent down, including my original bone marrow slides. They reviewed everything and re-ran some of it.

When I was doing physical activity, I would notice the fatigue and sweating more than before.

CALR Mutation
I learned about the CALR mutation. They explained what it was and its impact. It was more favorable than other mutations, so that gave me some level of comfort.
It didn’t change a whole lot, even with treatment. There was a lot of adjusting as blood counts changed. I took anywhere from 500 mg of hydroxyurea a day up to 2,500 mg plus two baby aspirin.
Symptoms Intensified
When I was doing physical activity, I would notice the fatigue and sweating more than before. It was primarily driven by the blood counts. Nobody tells you about it. Why is it completely different all of a sudden? What’s changed? I managed it pretty well by knowing my limits on different things.
Myelofibrosis with CALR Mutation
New Hematologist
My physician moved to Vanderbilt, so I had my care transferred to one of her colleagues. The transition went well. As we went along, something in the blood work made her decide that we needed to take another look.

At first, it wasn’t bad. There wasn’t a lot of impact. But all of a sudden, I started getting a lot of fatigue and night sweats.

Official Diagnosis
I had my second bone marrow biopsy in 2023 and found out that I had myelofibrosis. What’s great was getting the information in real time as the results came back from different tests, so I was able to research. My son is studying to be a pharmacist, so he was pulling up information as well and we were comparing notes. By the time I had the appointment with my physician, I had a good idea of what was going on.
On the scale of 0 to 3, the fibrosis was in the grade 3 range, so I had a significant amount of scarring in the bone marrow. The treatment wasn’t going to change. I was staying on hydroxyurea and baby aspirin. I was told, “We’ll keep monitoring it. Let us worry about the bad stuff. You keep on living your life.”
Symptom Burden
At first, it wasn’t bad. There wasn’t a lot of impact. But all of a sudden, I started getting a lot of fatigue and night sweats, a lot of the symptom burden that was coming with myelofibrosis.
When I had an appointment with my doctor, I met with the physician’s assistant and went through all the symptoms and the impact on me being able to do things. I was falling asleep by 7 to 7:30 in the evening because I was completely drained after being at work all day.
If I worked in the yard, I’d be going back inside after a couple hours to take a nap because I was physically drained and exhausted. Their response was, “Well, sometimes you just have to deal with it.” I said, “Yeah, you know what? You’re right,” so I dealt with it my way.

Getting a Second Opinion
I reached out to people who I worked with at one of the research foundations and they had contacts throughout the MPN community. I was looking for other options to get a second opinion and was given a number of different places and different physicians.
I made an appointment. My wife goes to a number of things with me. My parents asked if they could come along, so I said, absolutely, come on.
My new physician explained everything from the very beginning with the ET all the way through MF and what MF could become. They explained not just to me but to my family and made sure that there was an understanding that this is what’s going on and this is what we do to treat it.
We talked through different clinical trials and different medications that were available. We went through the symptoms and some of the things that I was dealing with. My hemoglobin was pretty low at the time; I was in the 8 to 9 range.
We were looking at one medication that was getting ready to come to market versus other ones that were available. It kept getting delayed. They said, “Let’s switch medications now and if we need to switch again, we will, no problem. But let’s get you on something different now.”
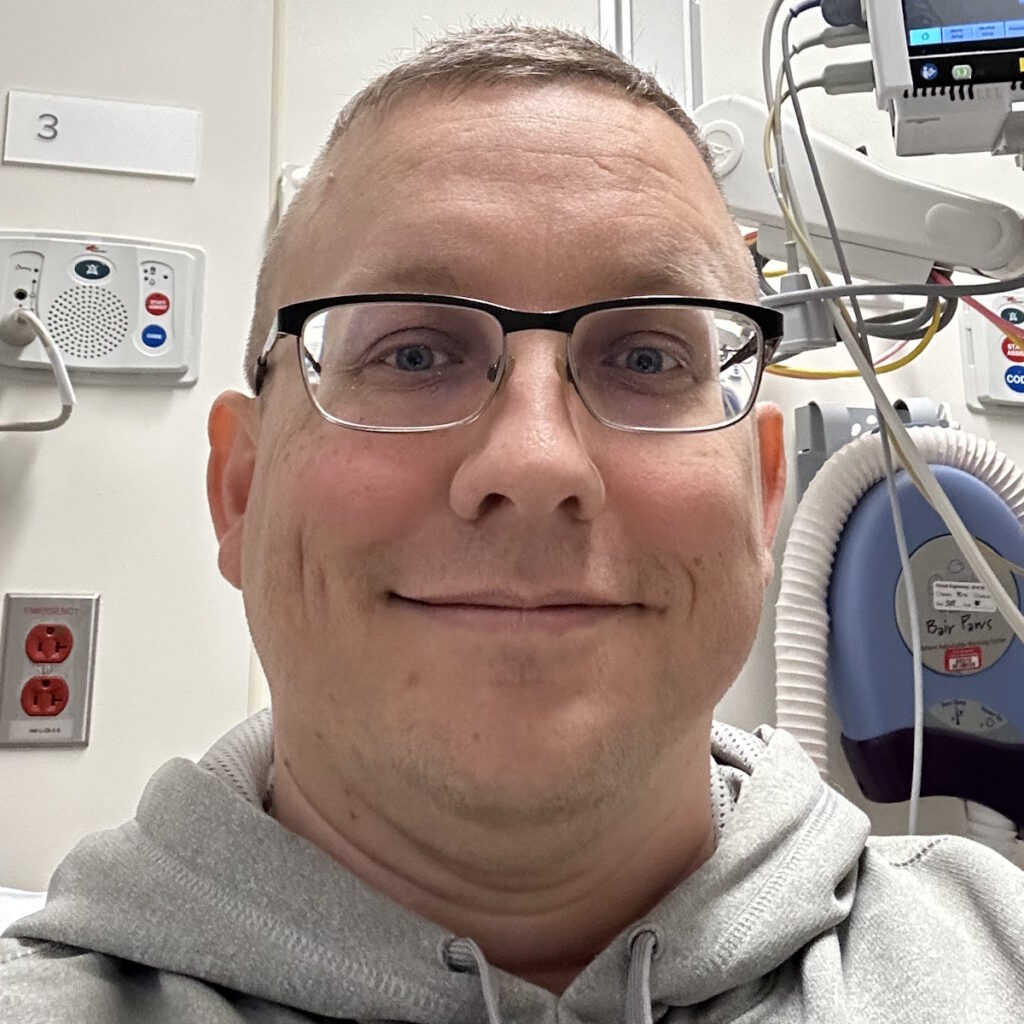
Switching to Ruxolitinib
I made the switch and started on ruxolitinib. It was amazing how quick the symptom burden was reduced. I was able to stay up in the evenings and watch movies without falling asleep. From a quality of life perspective, it was far greater than with the other treatments.

I’m not an expert, but I knew enough to know that there are other options and for those not to be part of the conversation was very, very frustrating.
Patient Advocacy
I was a strong advocate not only for myself but for other patients as well. There are people who don’t have the resources within a reasonable distance to see some of the MPN specialists or may not know who to reach out to for additional input or help.
If we look at how many people are going through something similar, how many cases do some of these hematologists see? I may have been the only one they’ve ever seen with this condition. They may have read about it, but it’s not common. It’s important to make sure that physicians have all of the information available. Personally, I wasn’t satisfied with the doctor saying that they have things covered. I want to know.
There was some frustration at times. When I hit the roadblock of being told to just deal with it, I was informed enough. I’m not an expert, but I knew enough to know that there are other options and for those not to be part of the conversation was very, very frustrating. I left that appointment feeling very unhappy and almost abandoned. You’re putting your trust in your provider and for them to tell you to just deal with it, I’m sorry, but I want something better.
Learning About MPNs
All the way back, even from the ET perspective, I was trying to figure out what it was. At the time, they didn’t even talk about it as blood cancer. It was still a neoplasm. They didn’t elaborate that this was what’s going on. We did a lot of research trying to find out things.
I was connected with some of the folks at the MPN Research Foundation. There are a number of online resources that provide factual information. It’s a balancing act. What are you seeing online and what’s correct?
As I was seeing the results come back, they listed what articles they were citing for the diagnosis, so I found the articles and read them. Because I’m not in the medical field, there are words I’ve never seen before in my life. What do these words mean? Is that good or bad? I was pulling together resources on my own.


Connecting with the MPN Community
I stumbled across and got involved with the MPNRF Patient Impact Council. It was through some of those contacts that led me to other recommendations for where to go.
It was nice being involved with other patients and having conversations. Even though a number of us have had the same diagnosis, there may be different genetic mutations so there are little differences on how it impacts everybody. Having somebody to talk to has been fantastic because you can hear about other people’s journeys, what they went through, treatment options, or things that I’m not aware of that some of my peers would be dealing with.
We have a group where we can sit back and laugh. Everybody was joking about things and having a good time. You’re with people who understand what you’ve gone through, what you’re going through, or people who have gone further through things.

Stem Cell Transplant
After my myelofibrosis diagnosis, we had conversations about stem cell transplant. Although I didn’t need it yet, we did the work to make sure we have things lined up. In the event that there’s a bone marrow failure, I progress into acute myeloid leukemia (AML), or things don’t go as well as we would like them to, we have options.
I went through the matching process and I was very fortunate to have my brother as a full match. We have multiple people on the donor registry that are full matches for me as well, so the prospect is very good in that avenue.
One of my peers who I’ve spent time with is not as fortunate. He has progressed very far through myelofibrosis and has zero matches. You see other people like him who go through struggles. If there’s anything that I can do to help advocate for people and make it easier for the next person, I’m certainly all for it.
We talk about clinical trials at every appointment. We talk about the ones that are currently out there, some that are coming, and why I would or would not be eligible for them.
Clinical Trials
Cleveland Clinic is one of the major centers that has some of the clinical trials. I’m fortunate to be fairly close and to have access to some of the experts in the field. We talk about clinical trials at every appointment. We talk about the ones that are currently out there, some that are coming, and why I would or would not be eligible for them.
It’s balancing risk versus the reward. It’s not necessarily the reward for me but to the larger community. I’m benefiting from medication that other people went through a clinical trial on. If a clinical trial is available and if it fits with what you’re looking for, advocate for that.

Follow-up Protocol
I have follow-up visits and routine blood work every three months. Where I work, we have a clinic on site that can do my blood draws, so I send the results to Cleveland Clinic and my physician for review.
I don’t need to physically go to the Cleveland Clinic every time. I’ve been able to do remote visits, which is quite a time saver. It takes me about three hours to get to the Cleveland Clinic from where I live, so it’s not overly burdensome, but it’s not the most convenient either.
The plan moving forward is to monitor the blood counts and make sure to communicate with the physician if the symptoms return. They are very responsive.
I’m in the middle of switching providers not because I’m unhappy or there were any issues, but because my current physician has taken a different role within the leukemia division and will be handling inpatient care only. I would be happy if I saw him, but I hope I don’t need to. Transitioning care is a very seamless process. They work with you right through it.
I’ve put myself out there by getting involved with different organizations. It’s through those things that I get access to people who are in the know.
Patient Education
From a broader perspective, through the work I’ve done with the MPNRF Patient Impact Council, I was fortunate to spend time with a number of physicians and researchers as they were going through and seeing some of the cutting edge treatments. It was nice hearing from their perspective but also being there to provide the patient perspective on how meaningful and impactful that is to a patient.
A lot of the treatments available improve quality of life by reducing the spleen size and symptom burden, but it’ll be fantastic when we get to the point of disease modification and change the landscape.


Through some of those interactions, I met one of the doctors that chairs a research consortium of some of the major cancer institutes. I have his personal cell phone number and he said, “If you ever need anything, call me.” I’ve put myself out there by getting involved with different organizations. It’s through those things that I get access to people who are in the know about something rare. It provides a level of comfort as you go through it.
One of the things that we were talking about recently was how to get that education into the hands of physicians, patients, and the broader community so that it’s more readily available. It was interesting because as we were talking in a group, one of the physicians said, “I’ve seen hundreds of patients with various MPNs and I’ve hit on some of the things that you, the patients, have brought up in these conversations, but it’s making me rethink my interactions and my dealings with them.” This is an MPN specialist who’s starting to think if he might have missed an opportunity or could have helped a patient in these avenues. It was fantastic. We’re at a point where it’s a conversation of what can we do better for everybody through the community.
Reach out to an MPN specialist. I would advocate for an MPN specialist over another hematologist because you need somebody who understands, studies, and specializes in MPNs.
Words of Advice
Don’t accept any answer that you’re not comfortable with. If you have questions, make sure you’re bringing them up.
Reach out to broader resources. There are a number of organizations that put on different programs. The Leukemia & Lymphoma Society puts on blood cancer meetings where they have specialists who you can interact with. People are afraid to talk to doctors sometimes. They’re normal people. They welcome the interaction. In some of the appointments, they seem very routine and very quick maybe, but if you’re not comfortable with where it is, call a timeout.

Get a second opinion. If you’re not happy with what you’re going through or with what you’re being told, there are tremendous resources available through a number of organizations. Reach out to an MPN specialist. I would advocate for an MPN specialist over another hematologist because you need somebody who understands, studies, and specializes in MPNs. You will get better traction and better information if you can get to one of the major centers that can support that.
I’m very grateful for the connections that I’ve made. It’s not just physicians and researchers but other patients too. The network keeps growing.
Feeling Grateful
I’m eternally grateful for everything that has happened. Even the bad stuff helped drive me to find something better. They say everything happens for a reason. I can’t say how grateful I am for all of the people who have been involved. There are people who are totally unaffected by MPNs personally who have dedicated their work and their time to helping others who are going through this. Pharmaceutical companies get beat up over things, but they are a very integral part in this. They help with the medications.
I’m very grateful for the connections that I’ve made. It’s not just physicians and researchers but other patients too. The network keeps growing. I’m fortunate to live in an area where I’m in fairly close proximity to a number of places with specialists that I can access if necessary.


We’ve had a group chat and there’s a group of people who will share normal, daily life things. Then one day, one of the individuals was going through treatment and said, “I could use some words of encouragement.” When you get tied into it, there are so many wonderful people who will help you through the journey. It’s that community support.
I know the impact that it’s had on my family being on ruxolitinib. It’s completely different. My son was talking about watching a movie one evening with us and he made a spot-on impression of me sleeping on the couch. We were able to laugh about it because it was so true and it’s not that way anymore. I hit my lowest compared to where I am now. Even when it’s bad, I realized that others have it much, much worse. I have myelofibrosis but, other than that, I’m healthy and can enjoy things.

Special thanks again to Sobi for its support of our independent patient education content. The Patient Story retains full editorial control.

Inspired by Ben's story?
Share your story, too!
More Myelofibrosis Stories
How to Support Someone with Cancer: Karina & Jesse's Myelofibrosis Story
“I underwent a lot of sadness, hardship, and difficulty, and all that entails. But I pressed forward in hope for sure. There was a lot of hope that just kept me going all those years.”
Demetria J., Essential Thrombocythemia (ET) progressing to Myelofibrosis
Symptoms: Extreme fatigue, stomach pain (later identified as due to an enlarged spleen), dizziness, shortness of breath
Treatments: Spleen-shrinking medication, regular blood transfusions, bone marrow transplant
Neal H., Prefibrotic Myelofibrosis
Symptoms: Night sweats, severe itching, abdominal pain, bone pain
Treatment: Tumor necrosis factor blocker, chemotherapy, targeted therapy, testosterone replacement therapy
Andrea S., essential thrombocythemia (ET) progressing to Myelofibrosis
Symptoms: Fatigue, anemia
Treatments: Targeted therapy (JAK inhibitor), blood transfusions, allogeneic stem cell transplant



2 replies on “Ben’s Myelofibrosis with CALR Mutation Story”
essential thrombocythemia diagnosed 1/12/24treating With Hydroaurea 1000mg 4Days a wk 1500three Days a wk platelets at 503
I’m also a Post ET MF patient right now. ET found on routine bloodwork during pregnancy in Service. In 1998, platelets up to 1,500. Caused severe neuropathy. Treated wirh Anagrelide, but quit to have 2nd child. Now, 27 years later.. mutated to MF in 2022. Treated wirh Vonjo & now Ojjaara