Shyreece Pompey’s Story: 10 Years Living with Stage 4 Non-Small Cell Lung Cancer
Interviewed by: Alexis Moberger
Edited by: Katrina Villareal

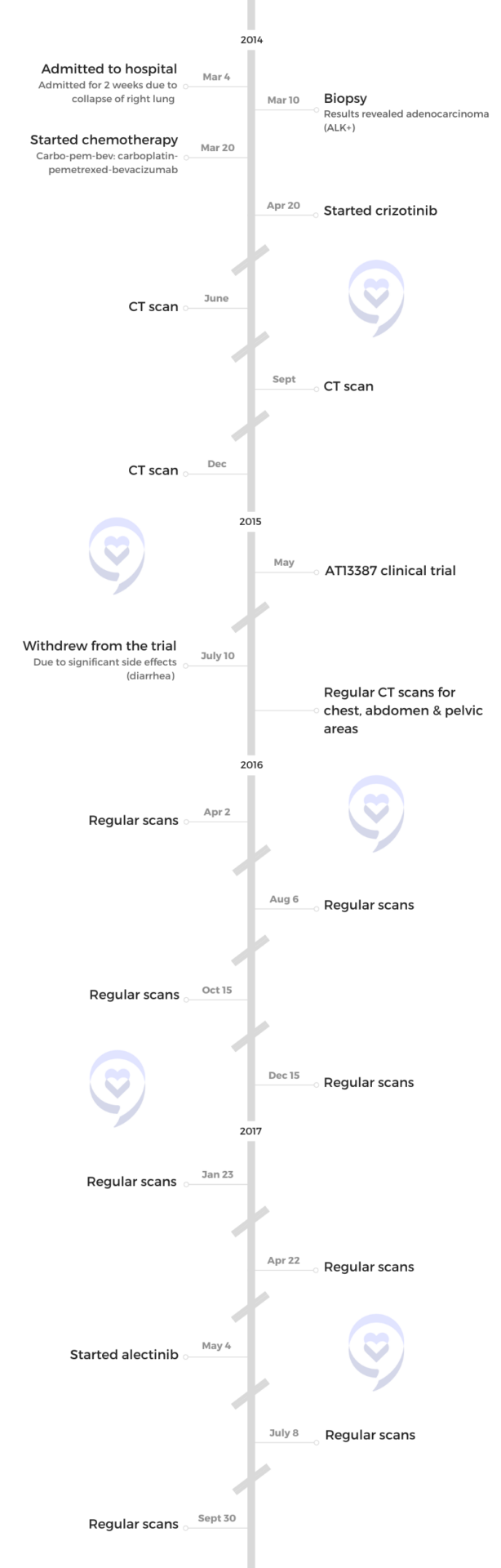
Shyreece’s story began with an unexpected onset of symptoms. After experiencing sudden shortness of breath, she was soon diagnosed with advanced-stage cancer following a series of hospital visits and tests. Visit her first in-depth patient story here.
She underwent various treatments, including chemotherapy and clinical trials, experiencing both successes and setbacks. While some treatments provided relief, others led to significant side effects and the progression of her cancer.
Her cancer journey is marked not only by the challenges of the disease and its treatments but also by her resilience and determination. She stresses the importance of self-advocacy, informed decision-making, and community support. She also became an advocate for understanding biomarker testing and exploring every possible avenue for treatment, including participation in clinical trials for new therapies.
Despite the challenges, Shyreece remained steadfast in her faith and determination to live fully. She shares her story through writing and mentoring, offering hope and encouragement. As she continues her fight, she approaches each day with unwavering resolve and a commitment to living without fear.
In addition to Shyreece’s narrative, The Patient Story offers a diverse collection of non-small cell lung cancer stories. These empowering stories provide real-life experiences, valuable insights, and perspectives on symptoms, diagnosis, and treatment options for cancer.
- Name: Shyreece P.
- Diagnosis:
- Non-Small Cell Lung Cancer (NSCLC)
- ALK+
- Staging:
- 4
- Initial Symptoms:
- Shortness of breath
- Treatments:
- Chemotherapy: carboplatin, pemetrexed & bevacizumab
- Targeted therapy: crizotinib, alectinib
- AT13387 (HSP90 inhibitor)
When cancer hit me, I thought, Who am I? Where do I go from here? What do I take from this battle that I’m in and can’t seem to get out of?


Such heaviness and shortness of breath came over me out of nowhere. I thought, What is this? From that moment, I knew something was wrong
Introduction
It’s been 10 years for me. Before the cancer diagnosis, my answer was, “I’m Shyreece. I’m a teacher and I love kids. I’m so glad to have overcome so many obstacles to teach and do wonderful things.”
When cancer hit me, I thought, Who am I? Where do I go from here? What do I take from this battle that I’m in and can’t seem to get out of? On any given day, I could be floored on my back and the next moment, I’ll be coaxing myself to get up and go to the bathroom.


Pre-diagnosis
Initial Symptoms
My students and I were getting prepared for spring assessments. After they came in from lunch, I said, “Let’s get ourselves ready and do a little brain break dance,” and then everything got heavy. The kids were moving, wiggling their arms, having a good time, and, for whatever reason, I couldn’t do it with them anymore.
I said, “Kids, you guys are going to have to sit down.” I had to hurry and sit down. Such heaviness and shortness of breath came over me out of nowhere. I thought, What is this? From that moment, I knew something was wrong, but I kept pushing past it. That’s what superheroes do, that’s what super teachers do. We push through it. We keep going.
That weekend, my boss came in and said, “We’re moving you to a more administrative role.” I said, “This is great. Now I’m excited again.” But when Monday came, I couldn’t carry my book bags into the office. It was such a short distance from the parking lot to the front door of the school, but I couldn’t do it. When I finally got in and started trying to catch my breath, somebody heard me wheezing and said, “Shyreece, you need to go to the ER.”
I didn’t know what was going on, but that started a two-week journey to being diagnosed.
Going to the ER
My husband picked me up from work at about 7:00 pm and took me to the ER. The doctor said, “You’re not going anywhere. You’re in such a state that we don’t even trust your husband to take you to the hospital. We’re going to take you by ambulance.”
I didn’t know what was going on, but that started a two-week journey to being diagnosed with stage 4 ALK-positive lung cancer. We didn’t even know what ALK meant. I learned that along the 10-year journey.


Diagnosis
Five doctors were standing in my room and they were as confused as I was. The hospitalist said, “We don’t know what’s going on on the surface, but I’m going to send this to the University of Michigan.”
He waited for the results to come back and when he got them, he said, “Oh my goodness.” He came in, held my hand, and told me, “You have cancer,” and then called the local cancer clinic.
Something in my gut said to go to the University of Michigan. When I got there, they said, ‘We have an inhibitor we want you to try. It’s promising.’
Treatments
Carbo-Pem-Bev
They had no idea what to do next, but she said, “Shyreece, I’m going to go ahead and load you up with the best chemotherapy mix that we can possibly give you right now.” I said, “Okay, let’s do it,” so I started with carbo-pem-bev (carboplatin-pemetrexed-bevacizumab) at the local clinic.
I didn’t know what I was asking for. We had to do it overnight. It was a long night, but I took it like a champ. I had the most angelic nurse that night. She was amazing. It was her first time treating me and it was my first time going through such an ordeal.
Crizotinib
Something in my gut said to go to the University of Michigan. When I got there, they said, “We have an inhibitor we want you to try. It’s promising and we want you to start that in April.” That’s when I started crizotinib.


AT13387 Clinical Trial
I joined a clinical trial of AT13387 (HSP90 inhibitor) times two cycles with concurrent crizotinib. I didn’t feel right with that one. I did everything that I was asked to do during the trial, but I withdrew due to significant diarrhea.
In the middle of the night, I would have to drink oral electrolytes quickly enough to stop the spasms. They were out of control. It was a couple of days or so after the cycle. I lived through that and didn’t like it at all. It didn’t give me a good quality of life. After I came off of it, I felt a little bit better, so I was able to enjoy my anniversary around that time.
After withdrawing and feeling a little bit better from the nausea and cramping, according to some scans around the time, there were improvements in some areas. For example, I used to have to do an abdominal CT scan, but I didn’t have to do that anymore, so something got better there, but I didn’t know what. I didn’t have to focus on getting some of the areas scanned.
After the trial, there was some metastasis. The University of Michigan said, “You can’t use crizotinib anymore, so you can stop taking it.”
Alectinib
I waited and had to fight for alectinib. I had to get it approved by insurance so that I could start taking it. The doctor said he was fighting behind the scenes with me to get the insurance to approve it so that I could start taking it. Even though I started panicking, he said, “Shyreece, it’ll be worth the wait.”
Everybody needs to understand what biomarker testing is and how to read certain test results when they come back.
Treatment Decision-Making
When I hear clinical trials, I hear another opportunity to step out in faith. At first, I didn’t want another clinical trial. I would have to be on my deathbed and have 24 hours to live before I do another clinical trial, but that’s not where I’m at right now. I’ve changed. I’m thankful I’ve had 10 years and kept up with enough.
Whatever decision I make, I’m not going to waver on it. I’m solid in my faithfulness. I’m going to make it knowing that this is what I’m choosing today. I hope that this encourages somebody else to live their best life with no fear. I’m not going into any trials with fear. It’s another opportunity to live my life with faith.
Somebody can benefit from me. I need them as much as they need me. I give love to people who need it and the relationship that they have with me, so I’m going to be present and I’m going to live.
Let the medicine do what it’s going to do, but know that it’s not everything. Whatever regimen I’m doing at the moment is what works best. That’s what I keep telling myself.


Biomarker Testing
Something told me that I did not have regular lung cancer. Nothing made sense to me and yet I was this close to dying. Everybody needs to understand what biomarker testing is and how to read certain test results when they come back. When I looked into it, I learned that there were different types of lung cancer. It opened up a whole new window of options.
In my situation, it seemed like biomarker testing was already done but the results weren’t disclosed to me. The test that the hospitalist sent out had some information in there. Stanford didn’t do a repeat biopsy. They trusted all the records from the University of Michigan. When they looked at them, they highlighted: stage 4 ALK, rearranged bronchogenic. That’s when I first heard those terms.
Six years went by before I found out what biomarker testing was. I learned that through LUNGevity, who heard about me through an ALK-positive online cancer group. The doctor at Stanford said, “Shyreece, have you heard of the ALK Positive group? Look them up. I heard that they just had their first summit.”
I started digging. Then-president Gina Hollenbeck and I started conversing. Sad to say, she’s no longer here. She lived eight years with the same cancer that I have. I have a lot of stories about the loss of friends with the same biomarker. That’s how I started talking about biomarker testing and doing a lot of the advocacy work that I’m doing now.
We have to be empowered. For patients who are getting these diagnoses, self-advocacy is a must.
Message to Other Patients & Care Partners
We have to be careful with the words we use regarding remission. The CT scan showed no evidence of disease. Friends and family even thought I was healed because I looked good and didn’t look like I had cancer. I’m so sick of hearing that. I don’t even have the energy for it anymore.
We have to be empowered. For patients who are getting these diagnoses, self-advocacy is a must. If you’ve been shy all your life, then you better grow out of it. I had to grow out of it and quickly.
I moved around all these clinics and doctors, and all of them didn’t want to have a meeting to see what was going on and what was best. I had to piece everything together. Advocate for yourself. You become a self-advocate when the flame of other voices lights you. What are you advocating? Who are you advocating for? What gives you strength and power? Nine times out of ten, it will come from something else that motivates you.

This is the time to just really lock in and go all in. This is war.
Advocating for Yourself
I always say when you’re advocating, get yourself locked arms. I love watching some war movies, like the movie called, “300.” I love it when they get ready to go to battle. Come on, they lock…formation, and then you can see them taking their shields. It’s in front of them. They locked in and they’re ready to go.
When you get ready to advocate, who are you locked in with? Find a group of folks who you can lock in with. This is not for the faint of heart. This is the time to just really lock in and go all in. This is war.
I have made it no secret in my faith. Now, there were some people in the beginning. They knew me as Sister Pompey, Sunday School teacher, and all this. But when I got a diagnosis, they were like,”Where is your faith now?”
I did take a tumble. I did take a hit, but I’m gonna tell you right now, I wouldn’t take [anything else] for my journey now. Look, if I die, I am the Lord’s and if I live, I am the Lord’s, so whether I live or die, I am the Lord’s. I’m going from life to life. I’m going to live my life.
I know this is not Scripture, but Gandhi said learn as if you’ll live forever, so maybe that’s why I keep reading all these reports and stuff. I’m going to learn as if I’ll live forever, but I’m going to live as if I’ll die tomorrow.
I’m living it all. I’m leaving it all out on the field today. Everything that was ever given to me, I’m giving it all, give it all, give it all. I’m not holding nothing. When I go to bed tonight and I’m [worn] out and I’m tired, I don’t have time for depression. I’m too tired.
You’ve got to connect to something bigger than yourself. That’s all I’m saying.Let the medicine do what it’s going to do, but you just know it’s not everything.
I do want to say for you or anybody else who’s watching, please, one of the things that I look for, I love giving back and I love sharing my story and my journey. [Here’s] a link to my book. It’s on Amazon — Fruititude: Growing Spiritual Virtues Through Adversity. I’m always giving back to children and families, so any way that you can support, that would be great and I would really appreciate it.

Inspired by Shyreece's story?
Share your story, too!
More NSCLC Stories
Drea C., Non-Small Cell Lung Cancer, ROS1+, Stage 4 (Metastatic)
Symptoms: Swollen ankle resulting from a deep vein thrombosis or blood clot, mysterious bruising, extreme weight loss, persistent shortness of breath, rattling sound coming from the throat while breathing
Treatments: Radiation therapy, chemotherapy, targeted therapies
Lysa B., Non-Small Cell Lung Cancer, ROS1+, Stage 4 (Metastatic)
Symptom: Severe but intermittent back pain
Treatments: Chemotherapy, radiation therapy, targeted therapy (including through a clinical trial), surgeries (lung resection, metastatic spine tumor surgery)
Ashley C., Non-Small Cell Lung Cancer, HER2+, Stage 4 (Metastatic)
Symptoms: Fatigue, breathlessness, persistent back pain, multiple rounds of bronchitis
Treatments: Chemotherapy, targeted therapy
Emily N., Non-Small Cell Lung Cancer, EGFR+, Stage 4 (Metastatic)
Symptoms: Chronic cough, persistent post-nasal drip, shortness of breath while doing simple activities, changes in voice, rib pain
Treatments: Chemotherapy, targeted therapy (tyrosine kinase inhibitor), radiation therapy
Loryn F., Non-Small Cell Lung Cancer, HER2+, Stage 4 (Metastatic)
Symptoms: Extreme fatigue, persistent back pain, chest pain, joint pain in the feet, hips, legs, shoulders, and elbows
Treatments: Chemotherapy, radiation therapy (foot and elbow to help with mobility), antibody-drug conjugate




