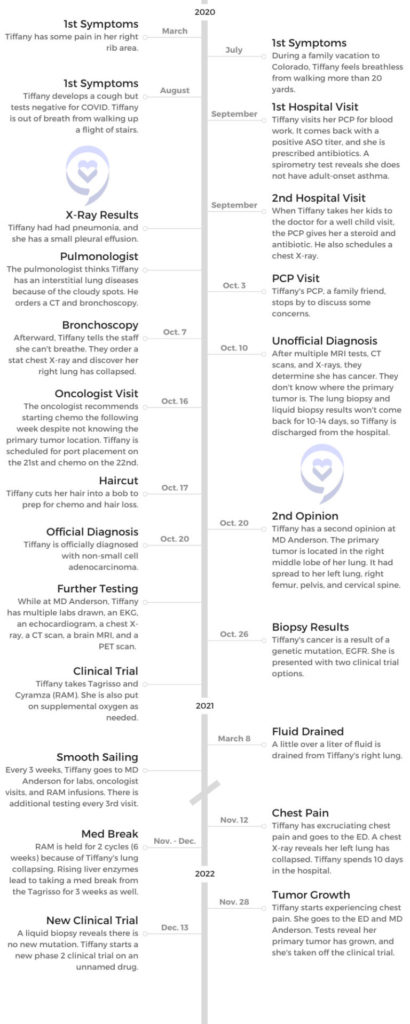
Tiffany’s Stage 4 Non-Small Cell Lung Cancer Story

Tiffany was a nurse and mother of twins when her world was turned upside down with a surprise lung cancer diagnosis.
Despite being otherwise healthy and into fitness, Tiffany started experiencing breathlessness and pain in her right side. After a collapsed lung and many tests, she was diagnosed with non-small cell adenocarcinoma
Tiffany shares her story of undergoing numerous tests to get her diagnosis, how her EGFR genetic mutation affected treatment decisions, and undergoing two clinical trials.
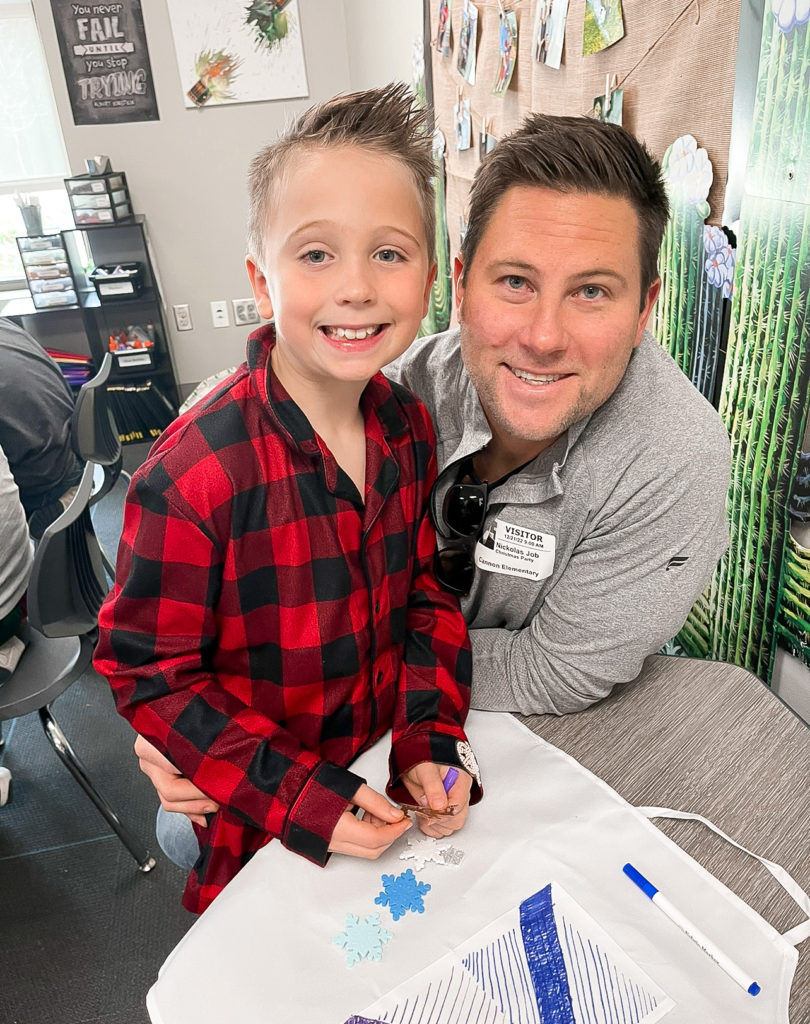
Tiffany and her husband, Nick, also started Ten for Ten Million to raise funding for cancer research at MD Anderson.
We don’t know what’s going to happen to us by the end of the day. We may as well just live for each and every moment.
Tiffany J.
- Name: Tiffany J.
- Diagnosis (DX):
- Lung cancer
- Non-small cell adenocarcinoma
- Biomarker: EGFR
- 1st Symptoms:
- Pain in right side
- Breathlessness
- Persistent cough
- Tests for DX:
- Blood work
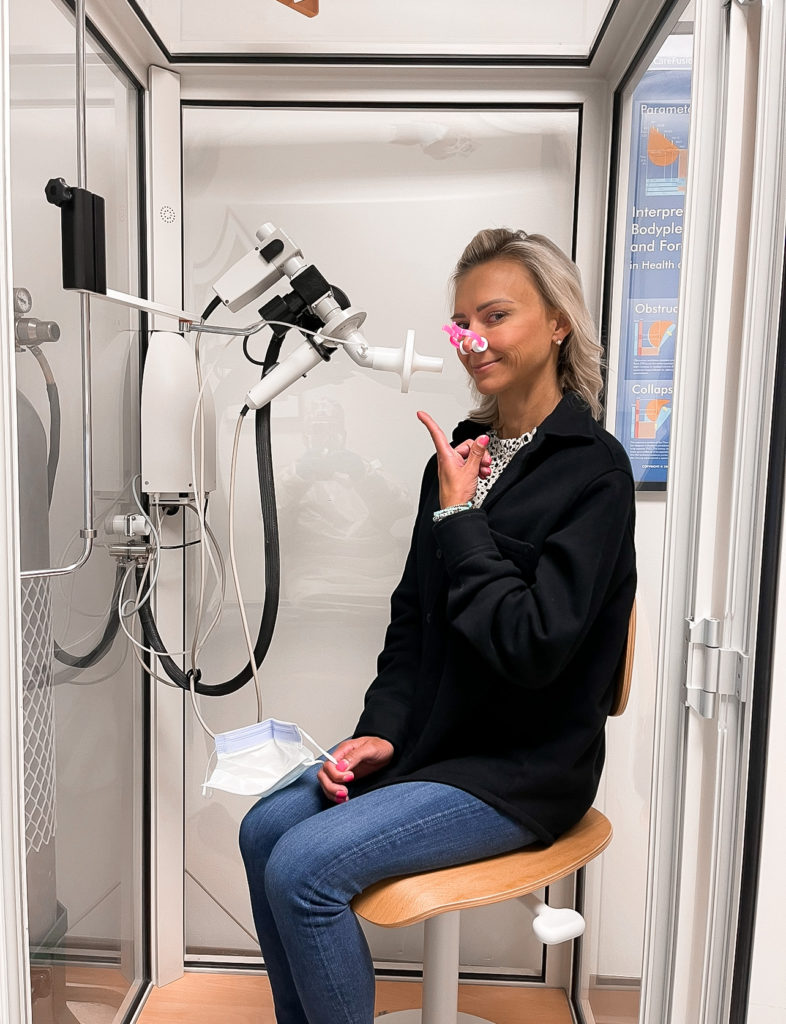
- Spirometry test
- Chest X-rays
- CT scan
- Bronchoscopy
- MRI
- Lung biopsy
- Liquid biopsy
- Treatment:
- Clinical trial #1
- Tagrisso
- TKI inhibitor
- Cyramza (ramucirumab or RAM)
- IV infusion every 3 weeks
- Tagrisso
- Clinical trial #2
- Phase 2
- Clinical trial #1
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Pre-Diagnosis
Introduction to Tiffany
Tiffany: This is my husband, Nick. We met our freshman year of college and started dating into freshman year. We celebrate our 15-year wedding anniversary in May. We’ve been together for a little over 20 years.
We have two 8-year-olds, boys. They’re twins. They’re amazing. I was a labor and delivery nurse for 15 years, and I used to teach Pilates. I love to work out. Fitness, and health, have always been super high on my list of priorities. So this is kind of a shocker, to be honest.

First lung cancer symptoms
Tiffany: I remember 2020, the start of the pandemic, I started having pain in my right rib, and I remember mentioning it to [Nick] several times. But as I said, I work out a lot, so I just thought I pulled a muscle or bruised a rib or something along those lines.
Then in July of 2020, we went hiking in Colorado, and I couldn’t go 20 yards without my heart rate shooting up and just being so short of breath. And I remember telling [Nick], “This isn’t normal.”
Then fast-forward another month, I started getting a cough that just lingered. Went to the doctor, drew blood, tested all that, started me on antibiotics, and did a steroid. Nothing helped.
Along those lines, making sure it wasn’t COVID. I’m still working in the hospital, so going to work and having a cough with the pandemic going on was not ideal. Then September, I went back in, and I told my primary care doctor, who’s also a family friend.
I said, “It’s just not getting better. These steroids aren’t working. The antibiotics aren’t working.” So we did a couple of tests in the office to check pulmonary function, and I failed that miserably.


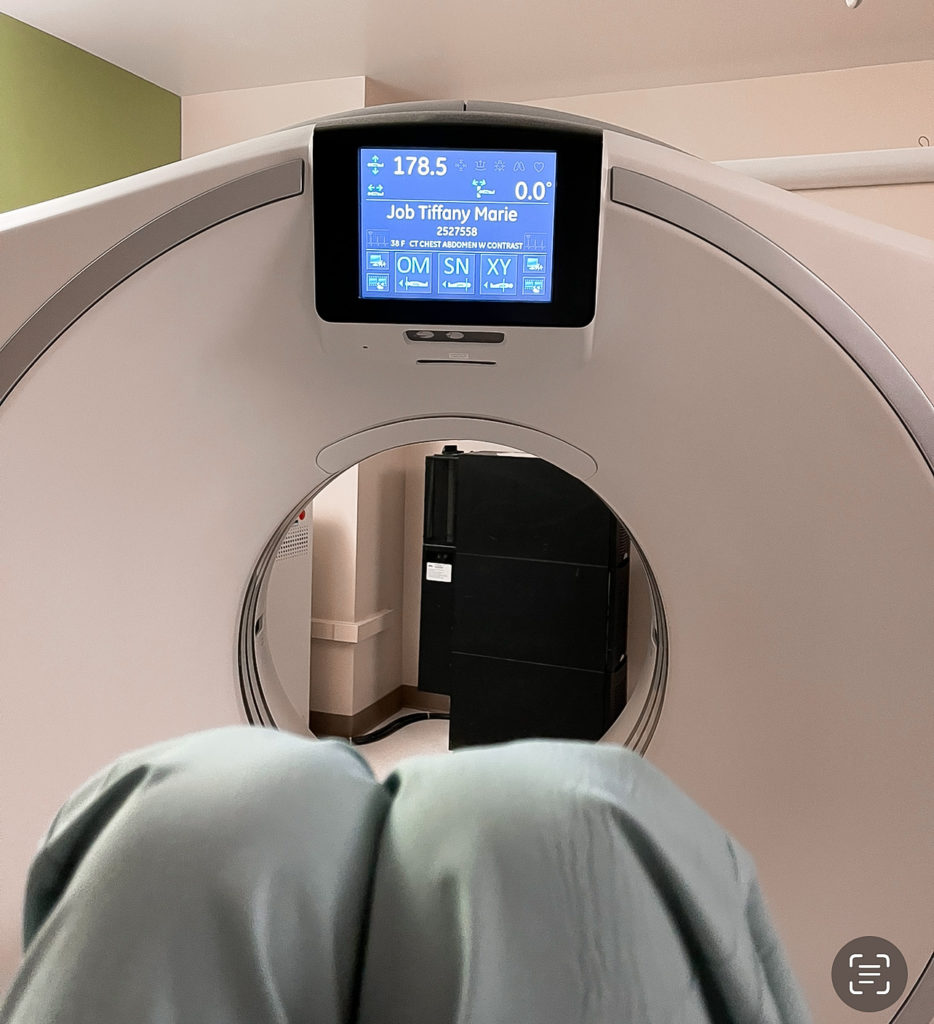
From there it was, “Let’s go see a pulmonologist. Let’s go ahead and get a CT scan, chest X-ray.” Over the course of maybe two weeks.
Nick: I think they said that she had the lung capacity of an 80-year-old. That raised some pretty significant concerns. That was, I think, the first real alarm bell for the primary care doctor, and that’s what sort of initiated the special session.

Did you ever have that feeling before?
Tiffany: I mean, Dr. Google. I kind of tried to self-diagnose myself with adult-onset asthma. After that pulmonary function test, it was obvious that that was not the case. From there, we were sent to a pulmonologist, where they thought it could be sarcoidosis.
Nick: Some type of interstitial lung disease. Nobody ever speculated that lung cancer could even have been an option.
Tiffany: Never smoked. I didn’t have any factors that really made a red flag go up that it could be cancer. I got scheduled for a bronchoscopy in early October 2020. When I came out of the procedure, Nick could hear me in the waiting room.
I was telling the nurses, “I can’t breathe.” The anesthesiologist walked by as I was saying that in order to check the X-ray, and my right lung had collapsed. I went back in, and got a chest tube.
When I came out, I was on the unit, and from there it just became we saw every doctor known to man. Epidemiologist because we had just been to Colorado. They thought maybe I had a fungus in my lung. We saw everybody.
Tests to figure out diagnosis
Nick: I think for a couple of hours, they thought you had tuberculosis.
Tiffany: Yeah, so then I was treated like a COVID patient. I was in isolation. My procedure was October 7th, and then we found out it was cancer October 10th-11th.
Nick: Four, five days of just tests and treatments and poking and prodding. The whole time, she had a chest tube in [while] trying to heal the collapsed lung. Eventually, that happened.



The concerning thing was the pulmonologist who did the bronchoscopy, I think looking back at it, he knew what was really happening. He couldn’t diagnose her, but he saw all these other tests being run, and he saw just the misery that she was in [during] that hospital stay.
We could tell he was frustrated. At one point, when they moved her to the isolation room when they thought she had tuberculosis, he came in and was furious that somebody would be putting her through that and started ripping out all the tubes and starting to get us out of there. That was, for me, the first time I realized it was more serious than that.
Lung Cancer Diagnosis
Did cancer ever cross your mind?
Tiffany: Early on, an oncologist did come into the room, so I think we were already a little bit aware. If we backtrack a little bit, one of the tests that I had prior to the bronchoscopy was a CT scan on my pelvis.
Our primary care doctor had a conversation with us and said, “There are some things that look a little off. It could be nothing, but sometimes it can be. It does look like it could be a little bit cancerous.”
Mine was already kind of a little bit there, but I had just gone to my OB. All of my testing was normal, as it always has been, and so I told him that. I said, “Well, I was just there. Everything there checked out great.”
He was like, “Well, that’s really positive. I love that. But we are seeing [bony masses].” Come to find out the cancer was stage 4, so it had already spread to my pelvis, my right femur, and my cervical spine.
So that’s what he saw. We found that out later, but we kind of had a little bit of an inkling it could be a possibility.

Nick: The primary care doctor’s actually a good friend of ours. When he came to our house, [he had] only the radiologist report. It was concerning, but your mind doesn’t go to advanced-stage, metastatic cancer. Even when you hear the word “cancer,” you don’t immediately assume.
Tiffany: That was October 3rd, I think.
Nick: Primary care doctor raises some concerns. Makes it clear that she has to have a bronchoscopy because they’re going to need to get tissue samples to really figure out what’s happening. That was about a week before she went in for the bronchoscopy, when everything became clear.



Meeting with the oncologist
Tiffany: All the days ran together. It was probably the second or third day that one of them came in, and I was like, “Okay, well, I know what that means, obviously, but I’m not…”
Everybody else is saying, “It could be this; it could be this,” so we were holding tight to all the possibilities that they were giving us and putting that one in the back. Like, “Surely not. That can’t be happening.”
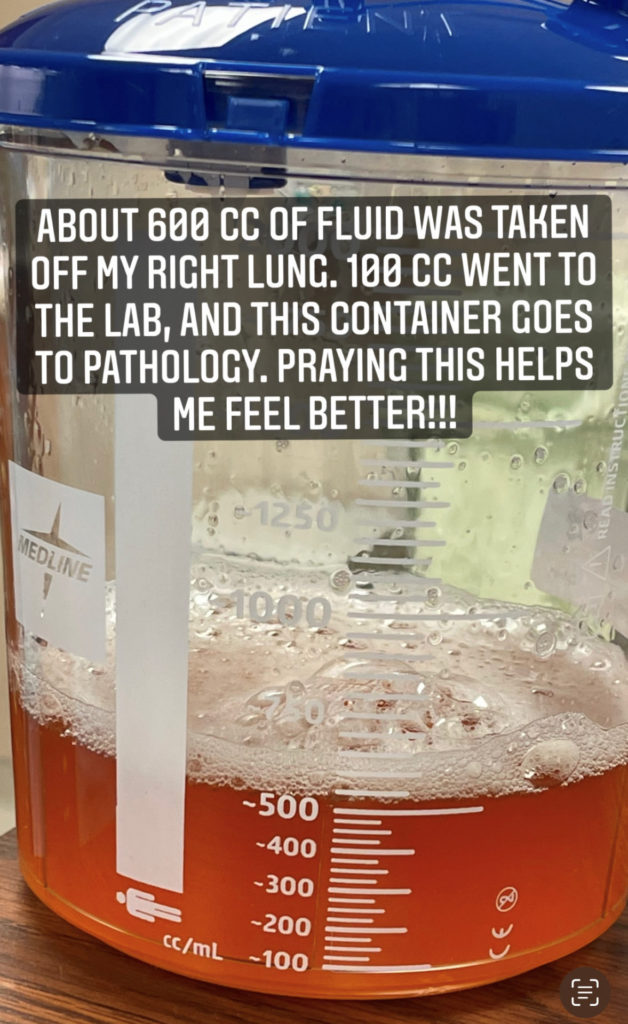
Nick: Even when the oncologist did come in, he never was very direct about it because they were basing their diagnosis on the fluid that had come off of her lung. They didn’t have the tissue results back, which gives us a clearer picture of what type of cancer it is, maybe more the primary.
At the time, they still didn’t see a primary tumor. They were basing it off of fluid, so he used words like, “We’re seeing cancerous cells in your endo fluid. It definitely is cancer, but we don’t know where or what type.”
They didn’t talk about staging or any kind of severity. So we’re sitting there kind of knowing that it’s bad, but not really at that time even still knowing how bad things are or how severe things were. You didn’t find that out until at least a week later.
Waiting for answers
Tiffany: At least a week. I think I was discharged on October 11th. We knew at that point for sure it was cancer. I think on the 10th they tried to tell us in not so many words, but to discharge us, they had to give us a diagnosis.
Because the tissue biopsy takes so long to get back — it’s like 10 to 14 days — our appointment with the oncologist here in town wasn’t until I think Thursday, the following week.
We had almost a week at home to sit there and just marinate on everything. Not knowing where my primary tumor was, what exact type of cancer I had. We just knew I had cancer. We came home, and we had to tell our family. They had so many questions, and we had no answers, which was hard.
»MORE: Patients describe dealing with scanxiety and waiting for results
How did you deal with not having answers?
Tiffany: I think I was just kind of in denial. This is not happening. It was shock. A lot of shock.
Nick: The other thing is she was still in a fair amount of pain from the chest tube. At that time, I think, and looking back at all of the pictures and going back — we do that frequently and see memories from that time — we didn’t realize how sick she really was.
A lot of the symptoms that she was feeling, experiencing, we knew what that was now, and so that was another hard thing. You’re sitting there knowing what this is now, and it just brought a whole new level of anxiety [and] fear.
And not having a treatment plan or answers on what to start was concerning, too. There’s a lot of fear [and] anxiety.
Did you ask for answers?
Tiffany: Their response was, “We have to wait on the pathology to come back because we don’t know enough to be able to give you anything.”
Nick: The original oncologist who diagnosed her didn’t comment on the primary tumor, so they weren’t saying that it’s lung cancer, although that seemed like the obvious answer.
We then went to MD Anderson for a second opinion, which was sort of in that week’s waiting period. We were admitted to MD Anderson, so we drove down to Houston, which is about a four-hour drive. They ran all the tests, all the scans. All the things that she had just gone through the week before in the hospital, they sort of redid in their environment
They basically said, “This is clear, no question. Obviously a mass in your right little lobe. It’s lung cancer, advanced stage. You’ll need to start treatment.” All of the answers kind of smacked in the face in one day.

Tiffany: Remember, this is COVID, so I’m going in there by myself, FaceTiming him. I think it’s hard as anybody getting any news, but trying to separate my nurse brain from my patient brain and really absorb it all was really, really difficult for me.
I’m so glad I had FaceTime and a second set of ears because I honestly think I heard half of what they were telling me, because I was trying to separate. It was a lot. It was a lot to hear, handle, and navigate on my own.
»MORE: How to be a self-advocate as a patient
Not catching lung cancer early
Nick: Yeah, I remember one of those calls. I was sitting in the parking lot outside the hospital at MD Anderson, and she was having this initial conversation with her oncologist whom she had never met before, who we know now really well.



But she didn’t know him from some guy down the street, and he’s sitting here telling her that this is really bad. There are some options, but this is that very frank conversation. And I remember you asked, “But we caught this pretty early, right?” He just very bluntly said, “No, we didn’t.” That was the eye-opener.
Tiffany: Yeah, I think because my symptoms came so fast, from basically July. I don’t really count March, when my ribs started hurting. In reality, that probably is when it happened. But I’m just thinking July, August, September, three months, like I’m here. And he’s like, “No, no, no.”
Nick: The vast majority of lung cancers are diagnosed in the advanced stage because their symptoms don’t present until it’s moved pretty fast.
Lung Cancer Treatment
Starting treatment
Tiffany: Luckily, the oncologist in town was very, very open to getting a second opinion. When we met with her and she told us that I had lung cancer but they couldn’t locate the primary tumor, she was like, “Okay, I’m going to schedule you on Wednesday for a port placement, and we’ll start chemo on Thursday.”
At this point, thankfully, we had already gotten an appointment at MD Anderson. I told her, “I’ll make those appointments, but I’m not going to be here.” I just flat-out told her, “We are going to go get a second opinion, and we were able to get into MD Anderson.”
She was like, “That is wonderful. You absolutely should do that.”


With that being said, I already had it in my head, like, “I’m starting chemo.” That’s what you do when you have cancer. At least in my mind, that’s how I was thinking.
I had really long, beautiful hair that I chopped off into a bob because I thought it would be easier to lose my hair if it was shorter versus all this long hair falling out. I’m in the process of trying to grow it out again because I quickly learned that that was not the route that we were going to take.
How genetic mutations affect treatment
Tiffany: When we went to Houston, my oncologist said, “We’re still waiting on those biopsy results. What I’m hoping for is that you have a genetic mutation.”
We had never heard of anything like that, and so we were like, “What do you mean, genetic mutation?”
He said, “Non-small cell lung cancers, there’s some sort of genetic mutation that we can target. We need targeted therapy to attack that mutation and avoid chemo, for the most part.”
I’m like, “Really? Tell me more.”
We went there, did all the scans, came home for two days, drove back. At that point, the biopsy results were back, and we found out that I have an EGFR mutation.
Thankfully, with that there is a medication that can target it that I was a candidate for, along with a clinical trial that I was a candidate for. They gave us the option to choose between two.
»MORE: Read our interview with a genetic counselor
Starting the clinical trial
Tiffany: I got started on Tagrisso, which targets the EGFR mutation, along with Cyramza, which is an IV medication that I received every three weeks. It’s actually for stomach cancer, but they were seeing what the two combined do together.
Nick: The clinical trial is testing whether or not the combination of those two medications would prolong the effectiveness, and increase the effectiveness. One of the issues that they have, the TKI, the targeted medications, is that they develop antibody resistance over time.
They were hoping that this Cyramza would prolong that or put that off, the resistance, for a certain amount of time. I don’t think they got their results, not from Tiffany’s trial, because her case lasted basically the average amount of time.
I did want to say one thing about that genetic biomarker testing is that if she had started chemo when the local oncologist wanted to … they probably wouldn’t have gotten answers on the genetic mutation.
It would have precluded her from most of the clinical trials that she was a candidate for. So getting the genetic biomarker testing done first, even though it caused some additional waiting, which was tough, was so important.
In hindsight, even now as she’s being considered for other clinical trials, it’s very important because the more lines of treatment that you’ve been exposed to, the more you start to get excluded from more.



What did you think of clinical trials?
Tiffany: When we heard “clinical trial,” I was very open to it. I think being a nurse, I’ve always been pretty open to things like that. I feel like that’s how we learn. We don’t get information if people don’t do it.
It kind of brought me back to nursing school, where I remember our professors would go in and say, “I have a nursing student. Are you okay with her coming in and learning today?”
Some people would say no. I understand that. But when people were open to it, it warmed my heart, because how else am I supposed to learn if I’m not exposed? How else are people supposed to learn if there aren’t people who are willing to do clinical trials?
My grandfather had kidney cancer and agreed to be a part of a clinical trial, and his first round of chemo actually killed him. But I knew it can go one of two ways. You can either have that result, or there’s the potential that this clinical trial could prolong your life. I’m just open to that kind of thing. My heart felt full to go that way.
Nick: You were also saying that the prognosis for lung cancer is pretty bad, and chemo doesn’t have a good track record, especially for her subtype of cancer. I think that makes it easier to be open to trying something experimental.
Genetic testing
Tiffany: With genetic testing, just so people know, you’re going to get pushback, especially from insurance companies. But it is such a huge asset to have and could potentially change the steps going forward. I feel very blessed that my oncologist was a huge advocate for that. He helped us a lot with our insurance.
Nick: The genetic biomarker testing, which is crazy to me, is still considered to be experimental. Maybe it’s changed since this was 2020 when she had that done the first time, but it was denied by insurance three times.
We had to fight with it for a while, and they eventually ended up writing it off. I don’t know who did. I think it was the testing company, actually. It just shocks me that with this being the new age of cancer treatment and it’s so effective and it’s the first line of treatment, the medication that she’s on.
Tagrisso is then the first line of treatment for several years now, and the only way you find out if you’re a candidate for that is this genetic biomarker test. For that to be considered experimental is just a shocker.

Every day, it seems like they’re coming up with new medications that target different mutations. It’s an amazing wave of cancer research that’s happening.
Nick J.
Genetic testing process
Nick: I think it is something people need to know about because I think for a lot of oncologists, the local oncologists, where we were diagnosed, treated it as sort of a backup thing that we can do.
Since we have tissue samples from the bronchoscopy, we might as well do it, but we’re going to start chemo first. In hindsight, again, that would have been a horrible decision.
We had to have that answer upfront, and we didn’t even know to ask for it. The oncologist at MD Anderson, that’s just part of their standard protocol. There are a couple of different ways that you can do it.



There’s actually a liquid biopsy, which is just a blood test now that looks for circulating tumor DNA in the blood. It’s a little bit like finding a needle in a haystack, so it’s harder for them to get a clearer picture of any kind of genetic mutations that are driving cancer from the liquid biopsy.
But it’s still an option that’s less invasive and easier to get done. They literally just drew, what, ten vials of blood?
Tiffany: I just had one done not too long ago again.
Nick: It takes a couple of weeks to get back.
Tiffany: It’s about two weeks.
Nick: The more accurate way to do it is through a tissue biopsy if they can get tissue from the tumor itself or the surrounding areas where there are metastases. Then they get a very clear and accurate picture of what genetic mutations or drivers are causing cancer.
Every day, it seems like they’re coming up with new medications that target different mutations. It’s an amazing wave of cancer research that’s happening.
Importance of education for patients and their caregivers
Tiffany: I think education is so huge. When you get a diagnosis like this, most people go to Google. I wish there was some page that we could put up that just said, “Do these five things right off the bat.”
Like, “Make sure you ask for genetic testing. Here’s what to do next. Make sure you get a second opinion.” I wish there was a checklist for people, like when I get my cancer diagnosis, what do I do now?
We were all over the place, and everybody was Googling things. We were hearing things from left, right, center, and it was really overwhelming. I wish there was a list of, “Make sure you do this, this, this, this, and this.”
We didn’t know what to ask for. Luckily, we just had people who were already doing those things. I don’t know if everybody has that same thing happen for them.
Dealing with insurance
Nick: First of all, we feel very fortunate that we have insurance. A lot of people don’t have that luxury. But it has been that adds stress and dealing with insurance companies and getting things approved.
Every day, we get a stack of letters from the insurance company. Half of them are saying you’re denied for this or that’s been excluded.
MD Anderson does a great job of kind of working and advocating on your behalf with the insurance companies. So a lot of this, the headache, is handled by them.



I always felt like my role is a supporter and caregiver to kind of shield Tiffany from the stress of the insurance and the bills. If you can take that small thing off her plate, one less thing to think about.
I didn’t want to deny the fact that those bills are sitting over there and that there are letters and things to deal with. But the insurance companies, a lot of people think they’re these evil villains that are out to get you. It is a difficult process, but I do think that they’ll work with you.
That’s been my experience. It might take a lot of phone calls and a lot of time and a lot of arguing, but they’re going to figure it out, and you can kind of put it off to the side and deal with it when you can. Nobody’s going to come to repossess your house or take your cars or anything like that.
For us, we tried to put that off to the side and deal with what was most important, which was being with each other and caring for each other and making sure that we have that covered. When we get a minute to take a deep breath, then you can go and open up those letters.
Med Break and 2nd Clinical Trial
What happened after the clinical trial?
Tiffany: I started a clinical trial taking the Tagrisso, which is what Nick was saying, the primary way to treat EGFR mutation with the Cyramza. The Cyramza was an IV every three weeks. Every three weeks we load it up and head to Houston, and I would get my infusion and check-up with the oncologist, get my labs drawn.

It was kind of every third visit, I would have a CT scan, chest X-ray, MRI, brain MRI. Lung cancer tends to go to your bones and your brain, and it had already gone to my bones. We’re just trying to make sure it doesn’t go to my brain.
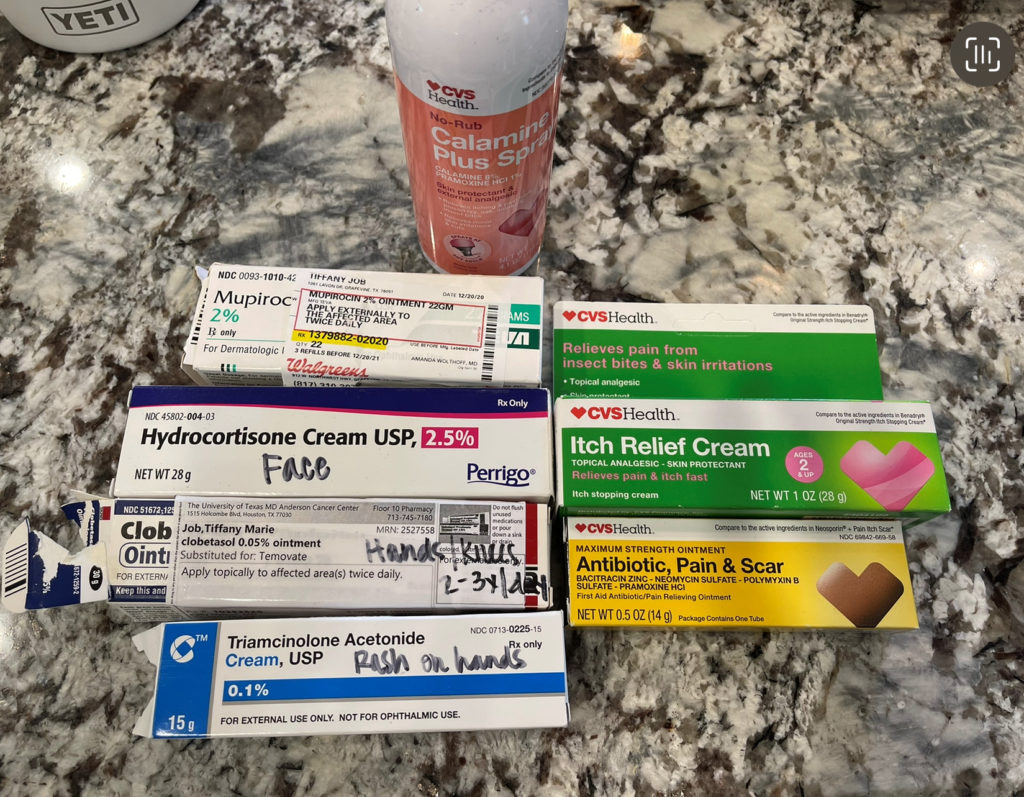
The Cyramza has its own set of side effects, too. I had a lot of bloody noses. The Tagrisso has side effects. Both of them caused headaches. The Tagrisso makes your body break out in a rash, especially as it’s getting built up in your system. That affected me very greatly.
I had just sores. They were everywhere — in my mouth, in between my fingers and my toes, my knees, my elbows. But they’re able to kind of help you with all those things with creams and meds.
»MORE: Cancer patients share their treatment side effects

Collapsed lung
Tiffany: Along this journey, the Cyramza also delays healing. About a year into a treatment, I was just sitting with my mom talking, and my left lung collapsed. I felt just immense pressure like what I would think a heart attack feels like.
[I] tried to walk it off, tried to take some muscle relaxers, anything I could to make the pain go away. Nothing was happening. We’re still in the midst of COVID. It’s not over yet, but it was bad at this point. This is November 2021.
I waited several hours, four or five hours, before I finally was like, “Okay, Nick, I think I need to go to the hospital.” They put me in this back room that was secluded from the waiting room, and we had to wait a couple of hours before we were seen.
They did that chest X-ray, and my left lung was just [shrunk]. Sure enough, it was gone. I got a stat test tube and earned a 10-day stay.

Med break
Tiffany: With that came taking what was a med break from the Cyramza, so we went back to Houston after I got discharged. They held it for two cycles. With the clinical trial, there’s all these things you have to meet.
I was able to take this break, but then I had to get back on it in order to stay on the trial. The caveat with that was if I have another collapsed lung, we’re done.
At the same time as that was happening, Tagrisso could cause liver toxicity, and my liver enzymes were just shooting up through the roof. So we had to take a break.
Nick: Which was really concerning because this is a year into treatment, and everything was actually working phenomenally well. They were shocked, actually, how well everything was controlled.
When Tiffany was diagnosed, we were looking back at pictures, [and] started to remember how sick she really was. We didn’t realize it because it just gradually got to that point.
At the time that this second pneumothorax happened, she was really healthy and strong and doing well. The fear of having to end the clinical trial that was working so well was really like the top of both of our minds.
Tiffany: I had gone from needing supplemental oxygen very regularly — that was in November of 2020 — to by March of 2021, I don’t think I picked it up again until my lung collapsed.
Nick: November of 2021, you were on a treadmill.
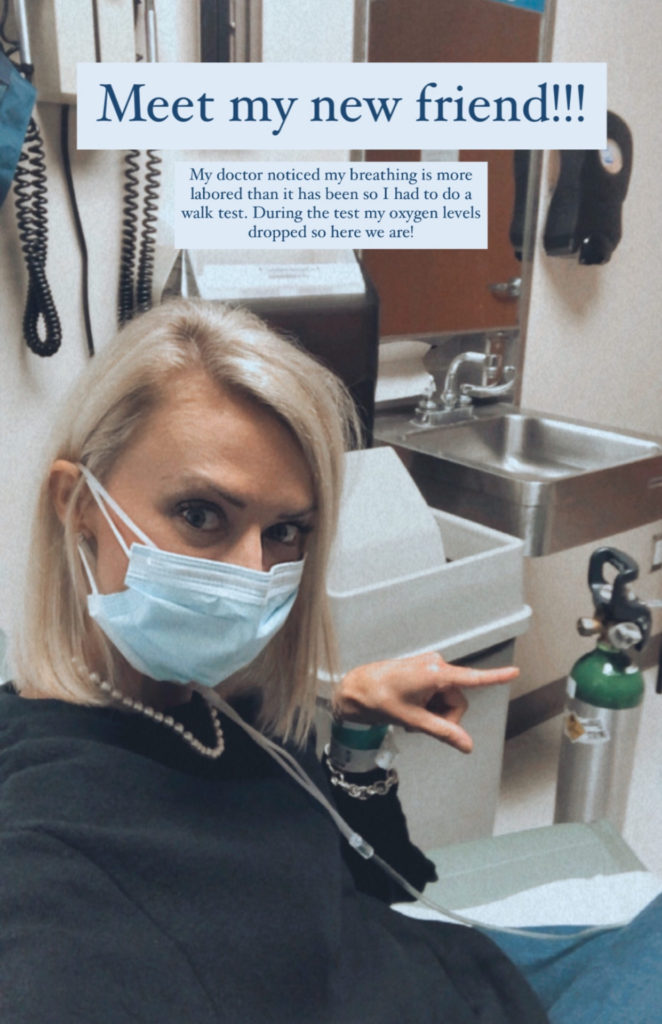

Tiffany: Running a mile a day. I felt like me again. Just every three weeks, we did our thing. That was a huge, like, “Hey, this is really still happening.” Because we had gotten so accustomed to everything working and falling into place.
Chest cramping issues
Tiffany: We took a break from both, huge med break. During that time, the cancer did grow a little bit, so we knew that these treatments were effective. They didn’t grow a lot. Very, very minuscule.
But still, our oncologist was like, “You got to be on this. This is not an option for you.” We restarted in February of 2022, I think, was the end of the med break. Started back on track. Everything was great.
We once again coasted until November. Just not my month. Leading up to Thanksgiving, I had some increased chest cramping, and it just was getting worse and worse and worse and more often.
We were due for a trip anyway, and I started talking to my nurse. I said, “Just having a lot of cramping. I don’t know what’s going on.” Because of the holidays — it was right around Thanksgiving — they were doing things a little bit backwards.
Typically I would go in. I would get my labs drawn. I’d get a CT or chest X-ray. Then I’d see my oncologist, and then I’d get the Cyramza. This time it was labs, oncologist, Cyramza, CT, and I was really uncomfortable with that given the symptoms I was having.
Heading to the ER for scans
Tiffany: She was like, “Why don’t you go to the ER, get checked out? They’ll do that test for you. We’ll have it, and then we can proceed tomorrow.”
I was like, “Okay, sounds good.” So we go in and drove into town, ate because I know how it goes when you go to the doctor. We ate dinner and went to the emergency room. They did a stat chest X-ray. Everything looked great. They did a CT scan.
This ER doctor who is not an oncologist comes booming in our room, and he’s like, “Well, the reason you feel so bad is that your cancer is worse.” We looked at each other, like, this guy’s happy and jolly, and you just told me really, really bad news. What is wrong with you?

We ended up getting admitted. That started a whole slew of more tests.
Nick: What that meant was not just that things were getting worse. It meant that the drugs that she was taking were losing their effectiveness.
We’ve been living in fear of [this] since the day she started taking it, because they’ll tell you, “This will stop working eventually. It’s great when it works, but when it stops, then you have to figure out why.” That was how we found out that.
Current clinical trial
Tiffany: Now we’re starting a new clinical trial. It doesn’t have a name. I don’t even know. The med doesn’t have a name. It’s a true early-stage medicine. I’m taking that in conjunction with the Tagrisso still. I started that second week of December, I believe, and we actually go back on Monday, and we’ll find out if it’s working.
Nick: It’s phase 2. They had a phase 1 to figure out dosing. The type of treatment is called Aurora kinase inhibitor. That thought there, I think, is that the Tagrisso had stopped working and there’s resistance for some reason, and they think maybe that this pathway is the way that.
They didn’t find any new genetic mutations, so the thought is that the existing genetic mutation has just built up some type of survival mechanism that they think that they know why that survival mechanism is happening.



I guess it’ll be pretty obvious this week if it’s working or not working. If it’s working, that’s great; she gets to continue on. But if it’s not working, then it’s back to the drawing board.
»MORE: Learn more about the process of clinical trials from one program director
Reflections
Being a team through lung cancer treatment
Tiffany: Nick’s always been my rock since the beginning. But I think a lot of what we have is our faith is just really strong, and it’s grown even stronger throughout this whole process.
We have an awesome team behind us. Our family is top-notch, incredible. Our friends are amazing, and our church community has just been such a huge blessing. The elders of our church pray over us pretty regularly. I would say our faith is what has helped us the most.
Nick: I think that part of our faith that helps for me is that at some point you just have to stop trying to control things and realize that you’re not in control of anything in life, from the most minuscule things that happen to you in the day to things like this.
You can give up the control a little bit, and we find ourselves trying to control every aspect of it. That’s when we start to get frustrated and mad and sad. I think that we help each other try to let go of that a little bit and realize that there’s a higher power at play.
The plan may not be what we want it to be, but there’s a plan out there that’s going to help somebody, and it’s going to do something because we know that there’s a higher power in control.
Words of advice for patients
Tiffany: Lean into your people. I mean, your family, friends, community, whomever you trust, and just accept help. I think that’s been the hardest part for me. I’m pretty independent, and I like to do things for myself.
Allowing people to help you is huge. You can’t do it all. Like you said earlier, the insurance thing, he’s like, “Don’t even think about it. Don’t worry about it. I got this.” That’s just one little tiny aspect of it all.
Over time, we’ve had so many conversations, and one of the things that is so important to me is that we don’t leave this earth without making an impression. This guy thought about that hardcore. He came up with a really great thing, so we started a nonprofit, which gives us a lot of meaning behind all of this, too.
Nick: Finding purpose was a big thing
Tiffany: A huge thing.



Make every day count
Nick: I also know one of the things Tiffany has done a lot really well, I think better than I would be able to, is finding a way to still smile and have fun and laugh and do stuff with the kids.
Even when she’s hurting or not feeling well, she’s still outside with the kids. She’s still doing things. It’s harder. Especially with COVID, there’s a lot of fear around doing things and being out there. But if you stop living, then you’re passed up.
Tiffany: At least for me, it’s been just trying to maintain normalcy and living life. We have a very big zest for life and just going out and doing it. Don’t hold back. I guess that’s the thing, too.

You always think, “Oh, when I retire, I’ll go do this.” Well, that isn’t going to happen for everybody. We don’t know what’s going to happen to us by the end of the day. We may as well just live for each and every moment.
Nick: Yeah, it’s really cliche — live while you can or make every day count, all that stuff. When you’re kind of forced to do that, it’s a little bit easier for us to say, like, just got to make every day count.
I feel like that’s one of the things we try to help each other do. Make sure that we’re constantly putting things on the calendar and having things to look forward to and planning trips. Half the trips that we’ve planned, we couldn’t do them or fell through, but we just keep putting them out there and keep doing stuff to try to make the most.
Ten for Ten Million
Nick: Like Tiffany said, she was adamant about leaving an impression and making a mark on this world. We did start a nonprofit that’s dedicated to raising funding for cancer research, and the sole beneficiary of our nonprofit is MD Anderson.
The nonprofit is called Ten for Ten Million, and that’s $10 a month for the 10 million people every year who die from cancer. What we do that’s a little bit different is we are trying to collect smaller donations in a recurring format. So that’s why we call it $10 a month for the 10 million people every year.
We have a website where you can go and sign up and make that recurring commitment. What that does is it gives the researchers at MD Anderson a steady, consistent, recurring flow of funds that are constantly growing.
That gives them the ability to more effectively plan their research and plan their trials and their treatment innovations and everything that they do really well. That just gives them the ability to do that better. That’s what our goal is.
At the same time, it raises awareness and helps people realize that you can’t wait until you have cancer to try to make an impact. You have to start now, and everybody should be committed to this.
Tiffany: It’s something that’s really easy. It’s just simple, easy, and we have a recurring email that tells you when it’s about to happen. Then we’re working on getting out a quarterly newsletter to just keep people in the know with where their money is going.
We’re working really closely with some people there. We’re going to be able to tour the lab soon and be able to share that with everybody who has committed. So we’re excited about that.


Inspired by Tiffany's story?
Share your story, too!
More Non-Small Cell Lung Cancer Stories
Ashley C., Non-Small Cell Lung Cancer, HER2+, Stage 4 (Metastatic)
Symptoms: Fatigue, breathlessness, persistent back pain, multiple rounds of bronchitis
Treatments: Chemotherapy, targeted therapy
Emily N., Non-Small Cell Lung Cancer, EGFR+, Stage 4 (Metastatic)
Symptoms: Chronic cough, persistent post-nasal drip, shortness of breath while doing simple activities, changes in voice, rib pain
Treatments: Chemotherapy, targeted therapy (tyrosine kinase inhibitor), radiation therapy
Loryn F., Non-Small Cell Lung Cancer, HER2+, Stage 4 (Metastatic)
Symptoms: Extreme fatigue, persistent back pain, chest pain, joint pain in the feet, hips, legs, shoulders, and elbows
Treatments: Chemotherapy, radiation therapy (foot and elbow to help with mobility), antibody-drug conjugate
Shauna D., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptom: Persistent dry cough following a cold
Treatments: Targeted therapy (tyrosine kinase inhibitors), radiation therapy
Allison Z., Non-Small Cell Lung Cancer, ALK+, Stage 4 (Metastatic)
Symptom: Severe back pain
Treatments: Targeted therapy (ALK inhibitors), radiation therapy





