Bladder Cancer Series: Through the Eyes of Black Women
“The Bladder Cancer Series,” focuses on Ebony, who was diagnosed with stage N2 bladder cancer, and LaSonya, who was diagnosed with high-grade bladder cancer.
In this series, they open up about their cancer journey, including their first symptoms, how they processed their diagnosis, how they decided on treatment options, and how they found support.
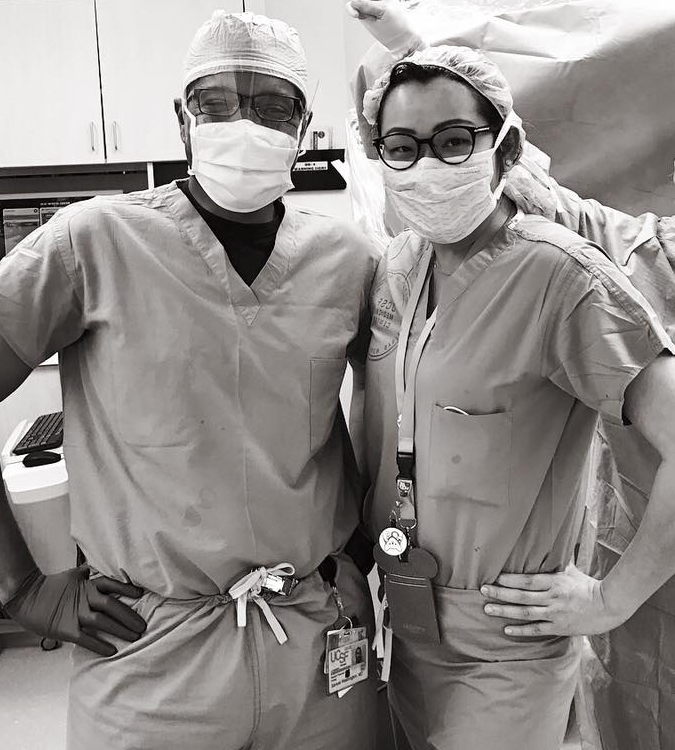
Dr. Samuel Washington, a urologic surgeon who specializes in oncology at the University of California San Francisco, also gives an overview of bladder cancer and its treatments.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

Introduction
Ebony G.: I’m married. I have three sons. I’m an engineer by day.
I just want to live my best life and help others do the same.
LaSonya D.: I’m a variety of things. I’m a black woman, that’s the most obvious when you look at me, but I’m also a mother [and] a wife. I am a professor of nursing.
Initial symptoms
Ebony: After an annual visit with my gynecologist, they noticed a microscopic level of blood in my urine.
LaSonya: I had just recovered from an elective procedure and I was getting ready to go back to my regular work. One day, I noticed that I have blood in my urine.

What was your reaction to the diagnosis?
Ebony: I was 45 when I was diagnosed with bladder cancer. I was like a ball of tears. At that moment, I remember thinking, “I’m going to die.”
It was pretty traumatic by myself in the office, but the nurse tried to reassure me and tell me, “You’re going to be okay.”
LaSonya: It’s devastating. How did I get this? No one in my family on either side has a history of cancer. How could this be? I don’t even know one black person that has this type of cancer.
I was a nervous wreck at that point. I felt so defeated and deflated. I just could not believe that this was happening to me.
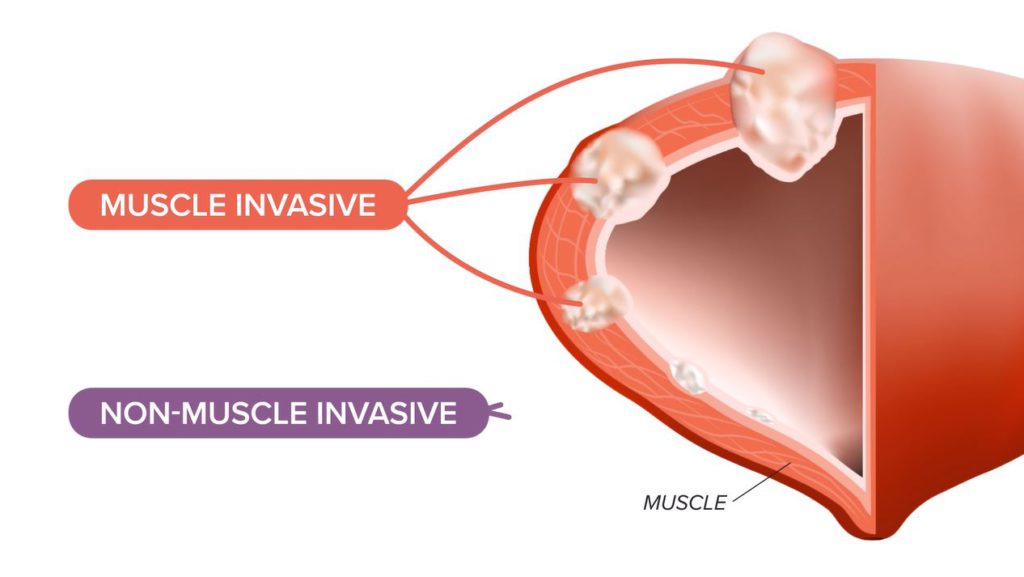
Overview of bladder cancer
Dr. Samuel Washington: In general, we think of bladder cancer as either being muscle invasive, so growing into the muscle wall of the bladder, versus non-muscle invasive, where it’s just on the surface or on the lining of the inside of the bladder itself.

Treatment options for bladder cancer
Dr. Washington: Our treatments are different depending on which group you are in.
We know that patients for whom the bladder cancer has grown into the muscle, across the board, people are not getting what our guidelines say they should be getting. Depending on the cohort you’re thinking about, half will get some guideline-concordant treatment.


Now, there’s a question of guidelines being appropriate versus equitable, but we know that based on where you live, how far you are from a facility that treats bladder cancer routinely, [and] who you are, are all things that can impact the quality of care and the type of care that you get.
I think those are the key things that we see in bladder cancer that we hope to look at with some of our research.
Guidelines in general are a set of recommendations by our overarching governing body telling us, based on the most updated literature in research and the consensus statement of experts, what this patient should have based on the type of cancer or disease that they have. It’s taking the mystery out of medicine, but it’s really an algorithm. We find where these people fit in terms of staging and characteristics, we look at the guidelines, and they tell us what should offer the best outcomes for them.
Information for bladder cancer patients
Dr. Washington: There’s a lot of ongoing research for patients who are interested in more information about bladder cancer, the treatments, support groups, and ongoing research.
There are many outlets out there. Bladder Cancer Advocacy Network is one that is focused entirely on this. Ask your provider. “Are there resources that I can look at? Are there clinical trials or support groups for information?”
Importance of having a support system
LaSonya: Three weeks after diagnosis, I was able to have my surgery for the resection. [While] waiting to have my surgery, I had questions for this doctor. I knew right away that this was going to be very stressful, not just for me but for my family. I knew that in order for me to get through this, I was going to need help.
A lot of times, people think that you have to take everything on yourself, especially being from my culture. Mental health is very taboo. People take it as a weakness when you need to seek out help mentally. You always hear people say, “Be strong. Suck it up. You can do this. Don’t be weak-minded,” those kinds of things.
We are human beings. We are not robots and machines. We have feelings. I joined a bladder cancer support group on Facebook. I just started looking for bladder cancer support.


Ebony: I remember looking in the social media group, trying to just scroll and see: who can I relate to?
The power of connection
LaSonya: There was something in the background of her picture that let me know that she was in the same sorority that I was. When I saw that, I just got so excited, especially because there [are] not very many black people at all [in] the support group. There isn’t a high percentage of black people that have bladder cancer. I was so excited.
Episode 2
The power of connection
LaSonya: When Ebony came on to the bladder cancer support group, she posted something and there was something in the background of her picture that let me know that she was in the same sorority that I was in.
Ebony: [She] was like, “OMG, hi, sorority sister. We’re here together.” That was so encouraging because I was looking for someone that looked like me. [I] hadn’t found anyone [who] looked like me that was fighting and winning at bladder cancer. To find her was huge for me because it’s like, “Yes, we can absolutely identify on even more levels.”
LaSonya: I got so excited, especially because there [were] not very many black people at all in the support group. There’s just not a high percentage of black people that have bladder cancer.
Ebony: It was instant. You know everything that I’m feeling. You can relate specifically to the loss of hair. You can relate specifically to darkening complexions. [The chemotherapy] also made certain parts of my skin darker. You can relate specifically to all those things.
LaSonya: It’s very important. It keeps you going. It empowers you.


Black women have higher stages of the disease & worse survival rates
Ebony: We initially thought it was a UTI so I was prescribed an antibiotic and then thought, “Okay, we’re good to go.” It kept going. What’s going on?
[I felt] despair at some points because I just really didn’t know. I was wondering if there was something underlying. I was Googling things [and] trying to figure [it] out. [I was] just confused and lost as to how the professionals don’t know.
I remember thinking, I trusted you for a year and a half to try to find something. What was it about everything that has gone on in the past year and a half where you didn’t find anything?
LaSonya: It seemed like it was a lot of blood. I saw some blood clots and I was thinking, I know I’m not on my menstrual cycle. What is going on? Maybe it’s something from my surgical procedure.
I called my surgeon and he said, “It doesn’t seem like something related to your surgery. Let’s do a urinalysis and see if you have a urinary tract infection.” I did that [and] it came back negative for infection, but positive for blood.
Signs & symptoms of bladder cancer “tend to be missed” in women
Dr. Samuel Washington: Women who are found to have repeated tests of blood in the urine or see blood in the urine sometimes can be attributed to recurrent urinary tract infections. Whether or not there’s a positive urine culture [or] urine test showing bacteria, they will be routinely treated with antibiotics.
But what is missing is the workup to make sure that it’s not cancer that’s hiding there and causing the bleeding. That can lead to delays as people get treated with antibiotics and you don’t see any change in the symptoms. It’s because we’re not treating it correctly.

Differences in survival: access to care and type of care
Dr. Washington: A lot of the research that I’ve looked at is around race as a social construct, so not just biology and seeing that there’s a [biological] difference and that that is the cause of the differences and outcomes that we’re seeing, but how society is framing these people: black vs. white, insured vs. not, educated vs. not. All these different identities impact one another to lead to these outcomes that we’re seeing that our differences between groups.
I commonly say no one’s intentionally contributing to disparities but also, very few of us are actively monitoring our own outcomes. The educational materials that we use, the required health literacy level for that, how we provide access to care for different patients, things that could help patients in terms of transportation, social work, and so on. Those things are not commonly measured at the same level that we monitor cancer diagnoses.
Representation matters: finding the right doctor
LaSonya: I was looking for a doctor that looked like me because I felt like I could trust a doctor that looked like me.
It’s just the things I don’t have to explain [like] the culture. There are certain things that when you’re holistically looking at a person or a patient, in my perspective, when I’m taking care of patients, I look at them holistically.
Overcoming obstacles
Ebony: I want people to know: you’re not the only one. I have fought through this.
I want to be the evidence, the example. I try to tell people, “I do consider myself a miracle and if you’re ever looking for evidence to help encourage you, let me be your evidence. You can fight this and win.”

Episode 3

The impacts of bladder cancer
Ebony: As a Black woman, it actually takes a long time for our hair to get to the lengths we enjoy.
[I have] a lot of pride and joy in my hair. I call it my crown. For about seven or eight years, I decided to become natural so [I didn’t use] any chemical products in my hair [or] any relaxers to relax my curl pattern.
To find out it’s all going to come out, I think to myself, Is it going to grow back?
I was devastated. How am I going to manage not having hair? That was honestly the tip of all of the side effects that were going to come from it but the initial thought was [losing my] hair.
I remember getting it cut and coming home that night. My husband started crying. He was like, “You’re really having to do this. Here we go.”
3 main paths after the bladder removal surgery
Ebony: There were a few options. I could have the bag outside of the body. My brain was like, Okay, that’s the option. [A] bag outside of my body that I would need to empty.
I was wondering how my clothes are going to fit. Am I going to have to have additional things [I would need] to use the bathroom? Am I going to have to change what I wear? I usually would wear fitted things. Am I going to have this bag that’s going to dictate [that]? Am I still going to be what I thought was attractive? You name it, I thought all those thoughts.
Then there was an Indiana pouch, which my doctor didn’t do, and the neobladder, which is what I decided to go with.


How much life changed after the bladder removal surgery
Ebony: My first appointment with the urologist was accompanied [by] this 3-inch binder [with] tons of information. There were sections [that talked] about what could happen after the surgery. One of those things was you could lose all ability to control how you use the bathroom. Those were the fears that I had.
[It covered] how it could impact your sexual relationships, your sexual relationship with your spouse. I remember thinking, Okay, this is a whole lot more than what I initially bargained for.
LaSonya: When you’re thinking about being married, young, and not having a vagina, that could be traumatic to your relationship. I never would have thought to ask but somebody in my support group brought it up. I talked to her and she became one of my close friends, too.
When she had her bladder removal surgery, they removed all of her vagina except for maybe two inches, which [meant] that she would have to come back later and have a reconstruction of her vagina. I was like, “Oh no, that is what I’m not doing. I don’t have [a] muscle-invasive disease so it’s not out of my bladder. I do not want to have no vagina.”
I was able to consult with the plastic surgeon. He went through the procedure. I said, “If they get in there and there’s a problem, I expect to wake up and still have a vagina.” He said, “If they get in there and they have to remove everything, then I’ll either take part of your muscle from your thigh or from your abdomen and I will make you a vagina. You’re not going to wake up and not have a vagina no matter what.”


It seems like something small when you have cancer, but it’s not. It’s still quality of life.
One of the things I was able to tell Ebony was, “Make sure you talk to them about vaginal sparing [so] you don’t wake up like another friend [who] only [has] a two-inch vagina and nobody told you anything.”
There [have] been a lot of people on the site whose partners left them. They have cancer and their partners leave. Because mentally, they can’t handle it or this situation. They can’t wrap their head around the fact that their sex life is going to be very different.
Ebony: I remember thinking, “As a woman, am I going to be able to help you meet your needs? Are you going to be disappointed still being married to me? Because now this ‘for better or worse’ is looking a whole lot worse than when we started 16 years ago.”
I would find myself stressing [about] what the outcome would be. That’s when my husband would come back and say, “Right here. We’re going to conquer the day. We’re just going to conquer the day.”
LaSonya: This is important. This is quality of life. It’s not just about living. It’s living your life abundantly and having the best life that you can possibly have.

Episode 4

The power of the patient
Ebony: At the end of the day, no one knows your body like you do.
I just challenge everyone out there. Doctors are doctors, but they are practicing medicine. They’re practicing, so they will not know everything. You know your body more than anyone else.
What the medical industry can do is put more faces in the forefront of people who are doing well, who are receiving the treatment, who have found their way, [and] who are winners. Not only people who have won the fight, but put people who are open and willing to help people win the fight.
We need to see that the system cares about us. We need to see that, because for decades, we’ve seen so many systems that don’t.
LaSonya: He had a picture in his mind of who I was and what my life was like. He already had his own stereotypical thoughts about who I was.
I actually worked in the same healthcare organization that he worked in. He did not treat me well as a patient. Thankfully, because I’m a clinician, I was able to identify that right away.
Go with your gut. If you feel like something is not quite right, get a second opinion. You’re entitled to a second opinion and some insurance will even pay for a third opinion. Do not feel like you’re stuck with that person.
I never have been one to put all my trust in another human being. I felt like I needed to do my own research and have my own questions ready so that I know that I’m getting the best care possible. The experience I have with urologists made it even [clearer] to me that my approach is the best approach for me.
You have to do what’s right for you. Get all the information that you possibly can and then you decide what’s best for you. You’re the one that’s going to have to live with your decision.


Black urologists in the U.S. are extremely underrepresented
Dr. Washington: Not infrequently, a Black patient will say that they’re happy to see me or someone that looks like me. It may not be important for everyone, but I think for some patients, it is a game changer in their comfort with the care that they’re getting.
[In] the urologic workforce, less than 3% of us are Black. A much smaller percentage when you start to chip away and look at different subspecialties.
Often, I think what it comes down to is for them, there is a shared life experience that we have that provides more comfort. That doesn’t mean that other practitioners that don’t look like them will not offer good care, but it does potentially provide a level of comfort that is not something that they’ve encountered before.
Bladder Cancer Patient Stories
Laurent Gemenick, Bladder Cancer
Symptom: Presence of blood in urine
Treatment: Surgery: transurethral resection of bladder tumor or TURBT
Jon T., Locally Advanced Muscle-Invasive Bladder Cancer
Symptom: Darkening urine, blood in urine, dull right flank pain
Treatments: Surgery(transurethral resection of bladder tumor or TURBT), antibody-drug conjugate, chemotherapy
Michael V., Bladder Cancer (Non-Invasive High-Grade Papillary Urothelial Carcinoma), Stage 1
Symptoms: Frequent urination, burning sensation when urinating
Treatments: Surgery (transurethral resection of bladder tumor or TURBT), immunotherapy (Bacillus Calmette-Guérin or BCG treatment)
Dorinda G., Bladder Cancer
Symptom: A significant amount of blood in the urine
Treatments: Surgery (transurethral resection of bladder tumor/TURBT, surgery for papillary lesion), immunotherapy (BCG), chemotherapy
Healing Together: A Mother and Daughter Navigate High-Grade Bladder Cancer
Mary Beth’s story about caregiving starts with an important awareness message about female bladder cancer symptoms.
Danny G., Non-Muscle Invasive Bladder Cancer
Symptoms: Fatigue, back pain, erectile dysfunction, nausea
Treatments: Surgery (transurethral resection of bladder tumor or TURBT), chemotherapy, immunotherapy