Patient Self-Advocacy
A Conversation on Speaking Up for Ourselves
From the first symptoms of cancer to how we communicate with our doctors, the importance of patients advocating for themselves is key to getting through diagnosis and treatment in the best way possible.
Four incredible Hodgkin lymphoma patients/survivors share how they were able to advocate for themselves throughout their cancer care, including during the beginning of the COVID-19 pandemic!
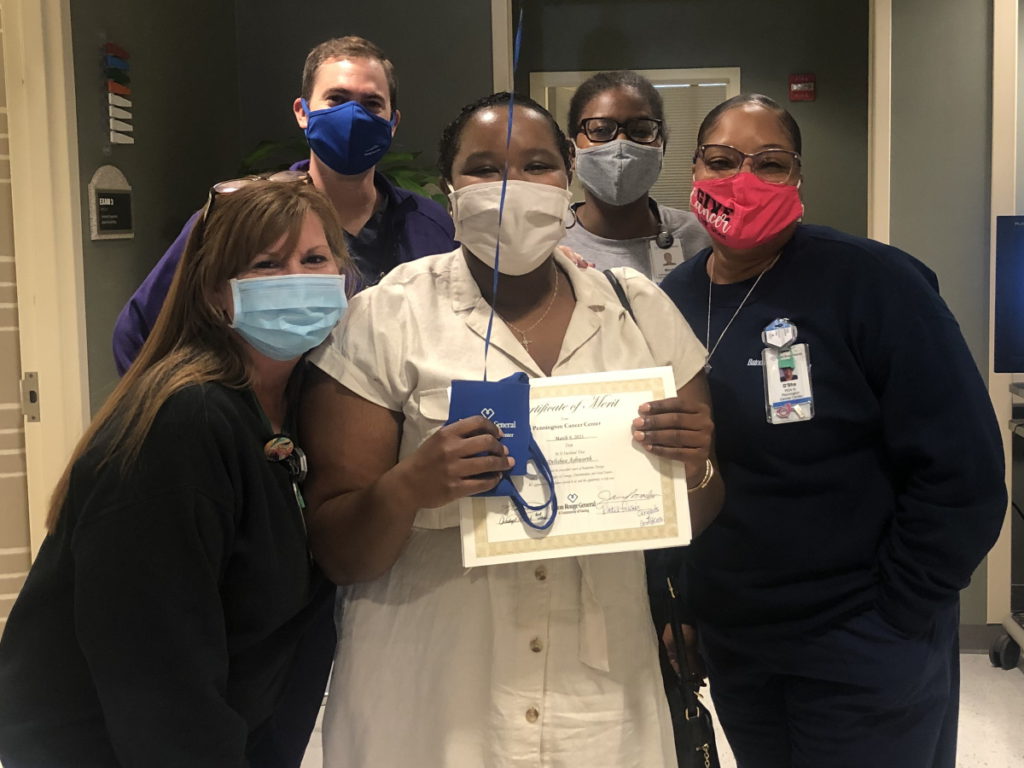
- Delishea A. was 30 and living in the rural South when she was diagnosed with stage 4B Hodgkin lymphoma. She shares the importance of speaking up about first symptoms and the power of getting a second opinion and other options.
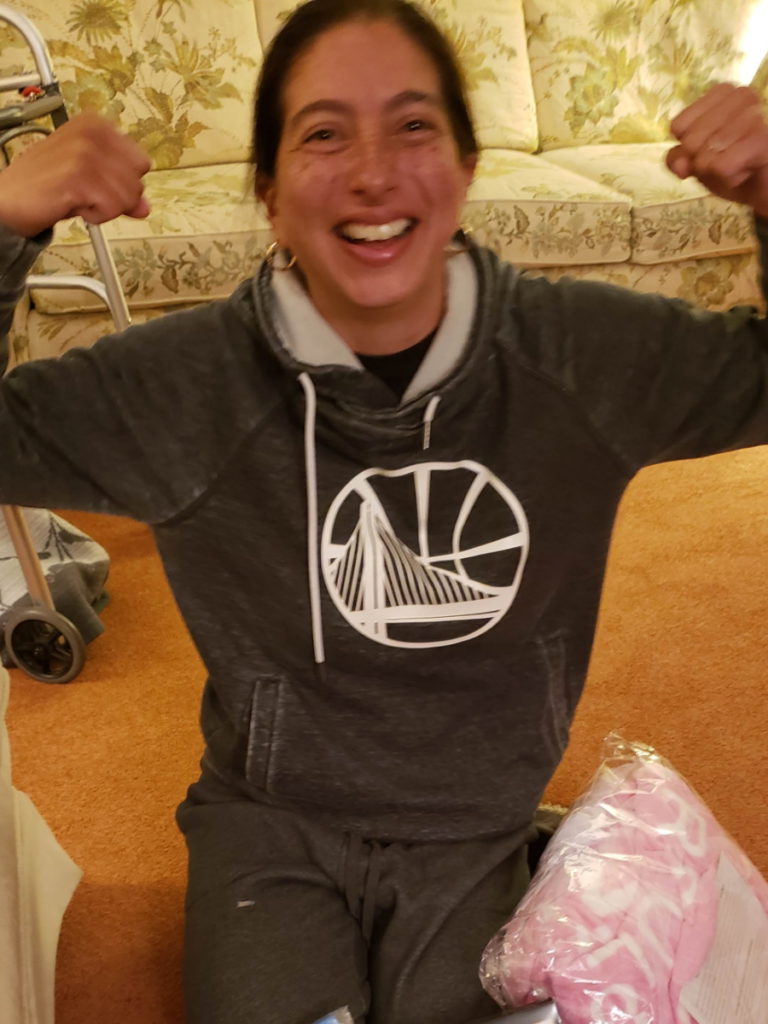
- Kelsey R. was diagnosed with stage 2A Hodgkin’s on her 26th birthday! Five years later, she reflects on how she was able to do her own research to get better treatment for herself and how she was able to develop the confidence to speak up.
- Tylere P. went through treatment twice for Hodgkin lymphoma, first as a 24-year-old and then again a year later. He dives into how drawing boundaries with his own family was an important step in self-advocacy and how he dealt with surprise bills (and financial toxicity).
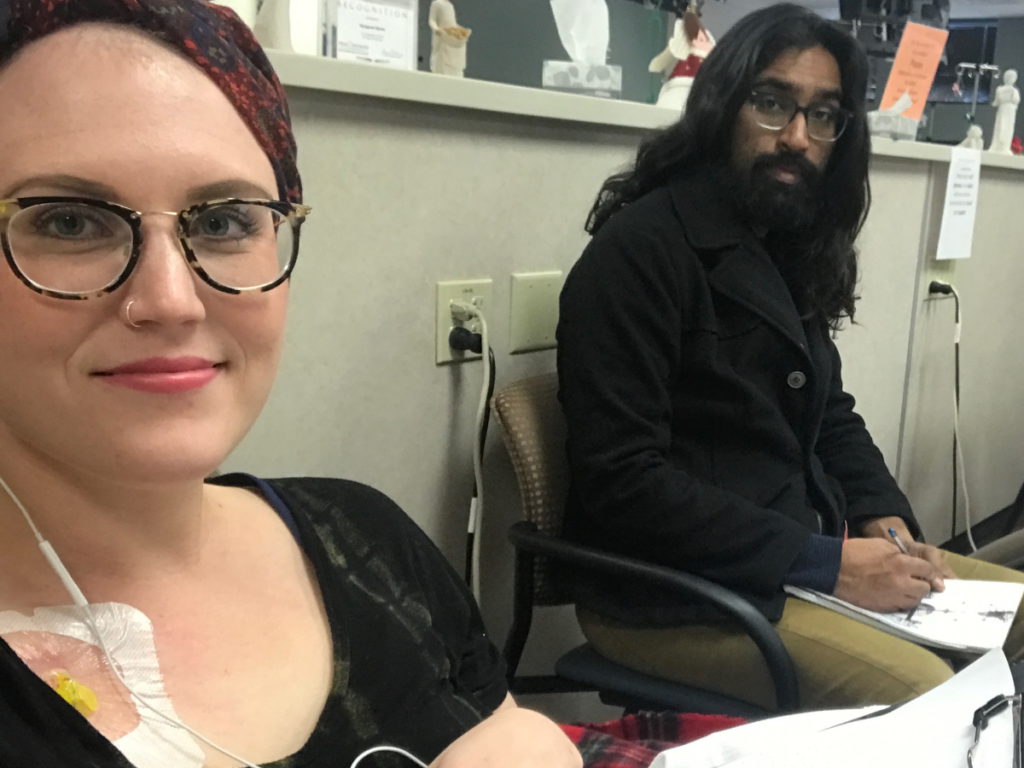
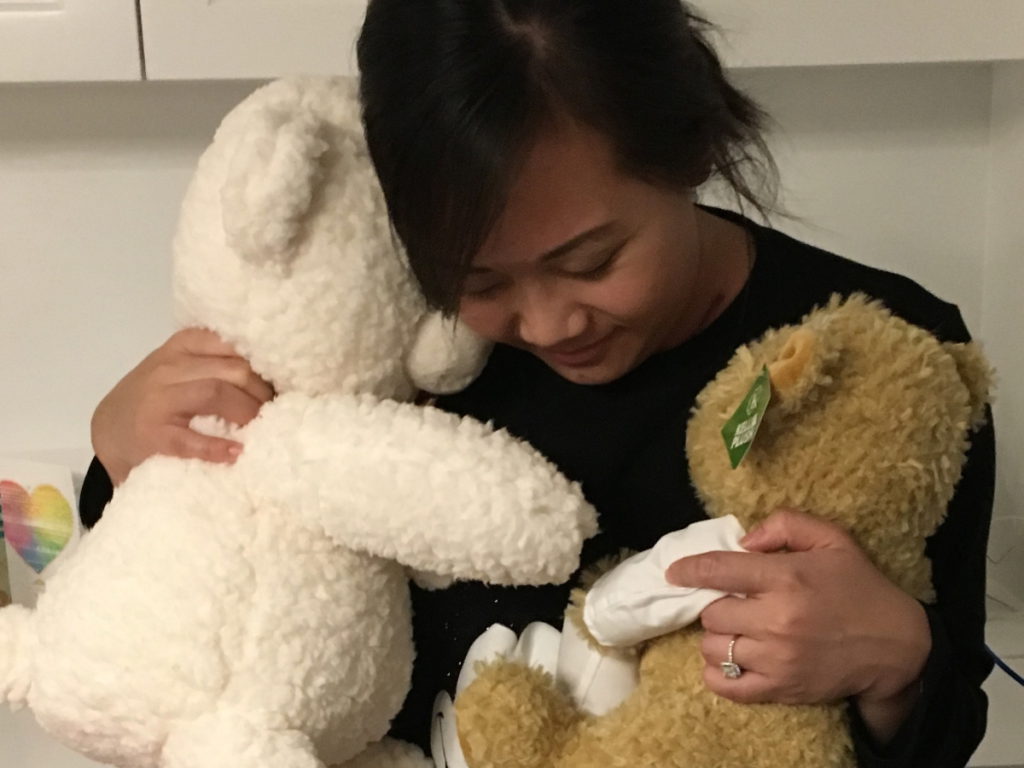
- Erica H. was diagnosed with HL right before the pandemic hit. She talks about her experience as a Latina, feeling dismissed for her cultural concerns about treatment. She also shares the importance of speaking up, especially during the COVID-19 pandemic where there may be medical burnout.
Special thanks to our collaborator, Imerman Angels, and to Seagen for its support of our patient program!
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
Introduction
Stephanie Chuang, The Patient Story: I am the founder of The Patient Story and also a cancer survivor.
I was diagnosed with non-Hodgkin lymphoma a few years ago and I’m grateful to be in remission but this is a topic that is very near and dear to my heart: self-advocacy. This entire conversation will be about speaking up for ourselves.
The Patient Story is created out of my own experience. I wanted to hear from other people and that’s what was going on when I started The Patient Story, where you’ll find hundreds of patient voices and videos and hopefully, that will help with [the] connection.
We’re bringing this to you with our partners, Imerman Angels, an incredible organization. I used Imerman Angels when I was going through my treatment. They help connect you one-on-one with cancer support. Whether you’re a patient, caregiver, care partner, survivor, [or] previvor, they will make sure that you meet someone who’s close to what you’re about to go through.
We want to say thank you to our supporter, Seagen and Hodgkin Hub, for its support of our patient event and program. Incredibly important to get partners on board who believe in this vision of helping patients and care partners everywhere.
The Patient Story and Imerman Angels have full control of the entire content. It’s not intended to be medical advice so please, please consult your healthcare provider and team if you’re having to make medical decisions.




Delishea A.: I’m from Louisiana. I was first diagnosed in June 2020, right before I turned 30. Just graduated as a medical biller and coder, and I’m about to get back [into] the workforce.
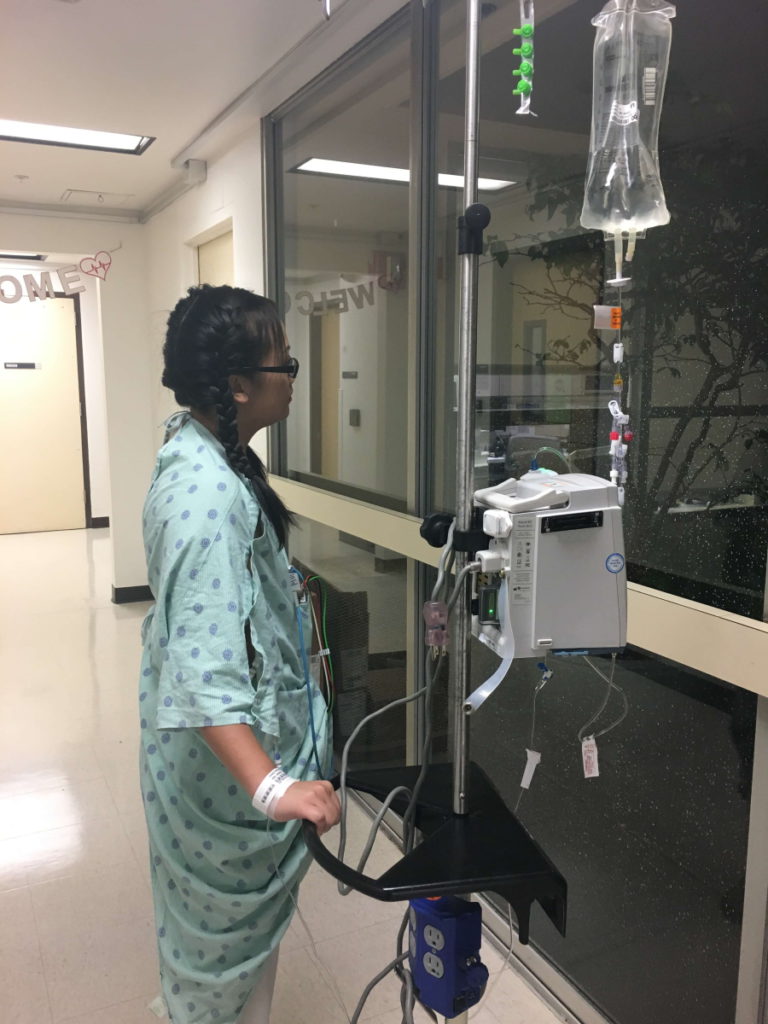
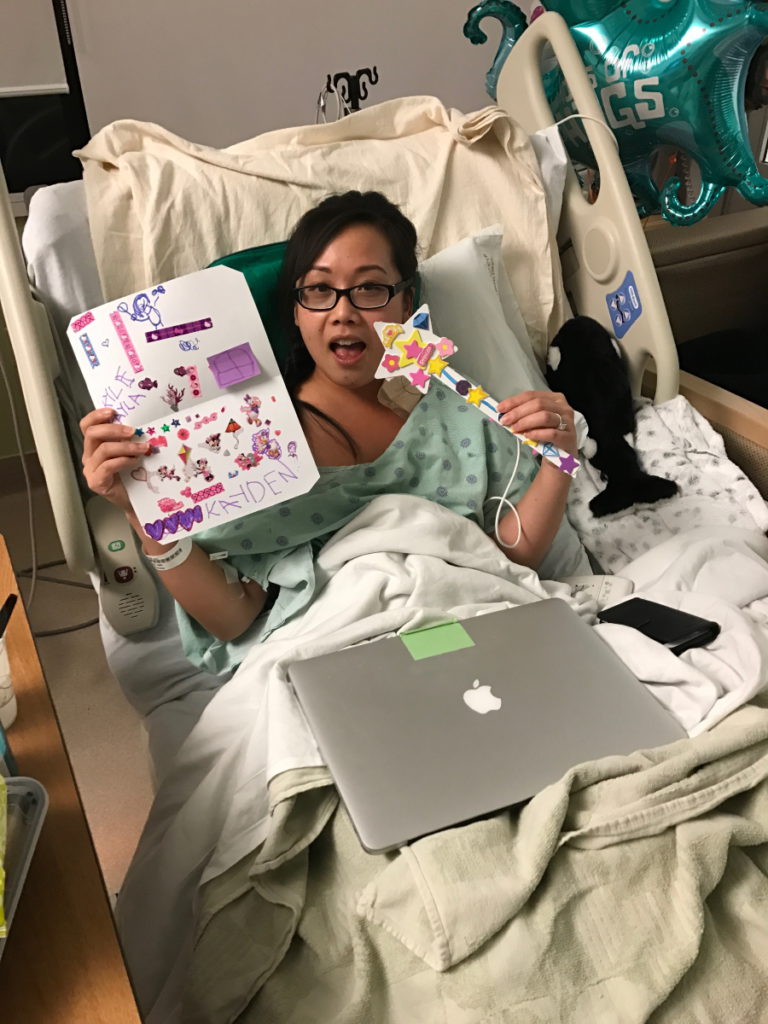
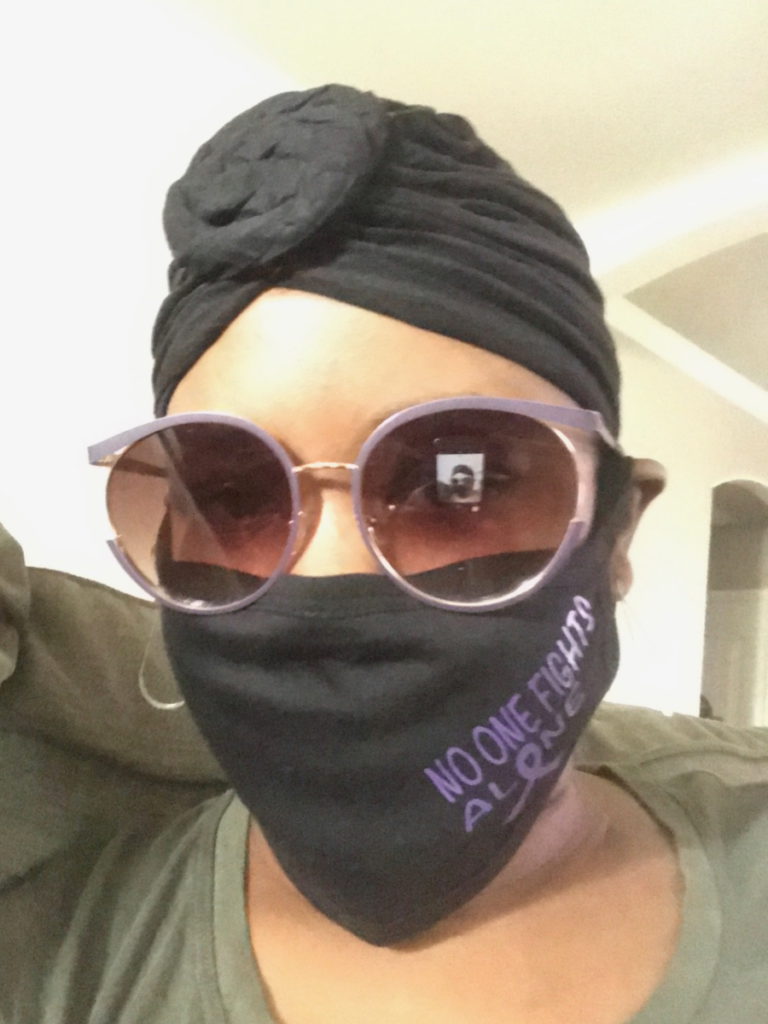
Erica H.: I am from San Francisco, California. I was diagnosed with Hodgkin’s lymphoma stage 3B [in] September 2019 and in remission as of March 2020, right as the pandemic was hitting off. I belong to a runners club and the motto is [to] start slowly and then taper off, so in all things — starting my business but especially doing treatment — that motto was really important.
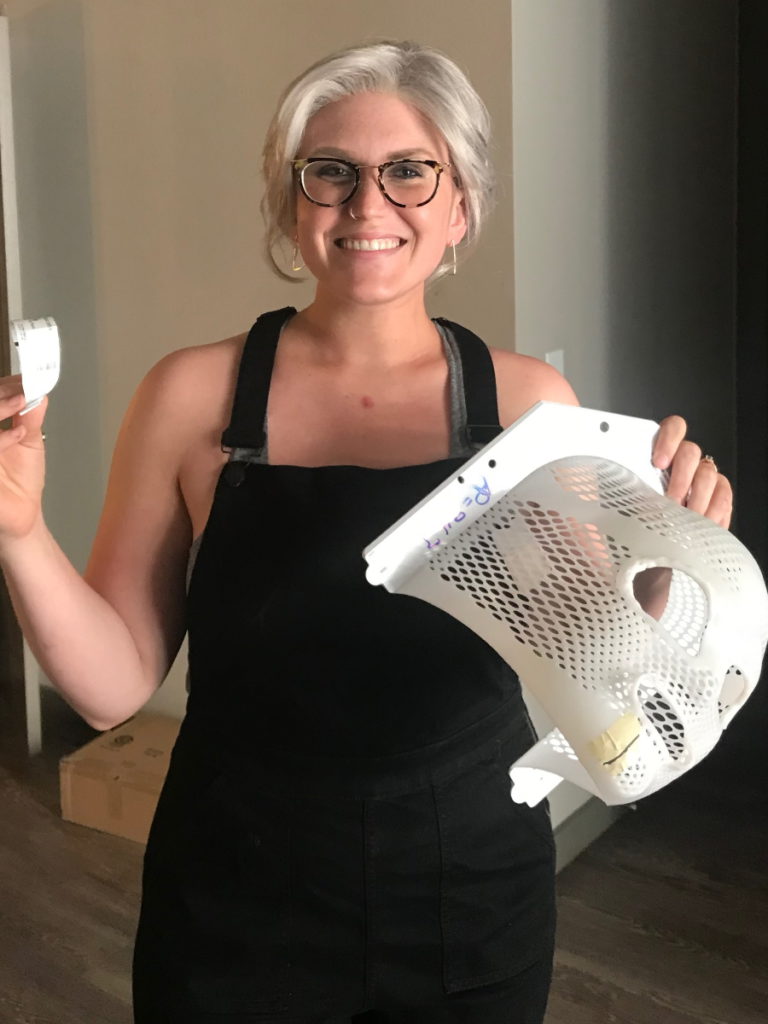
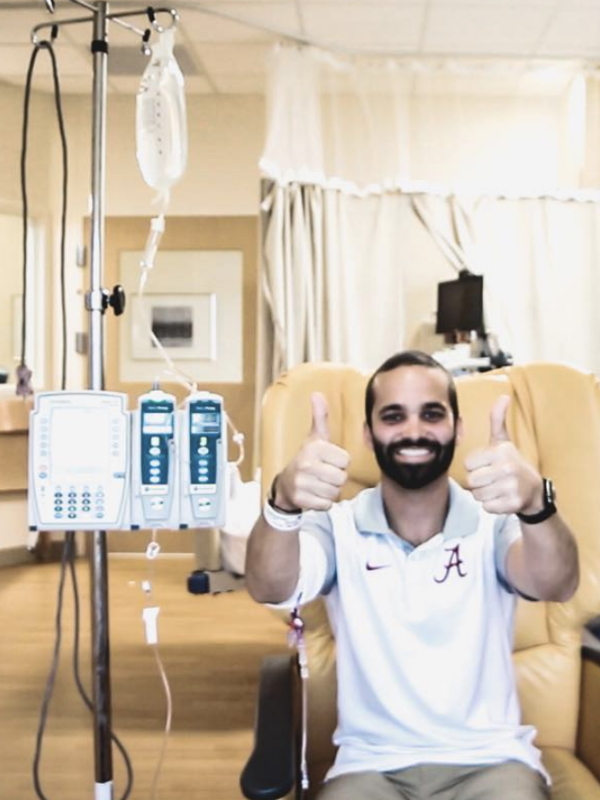
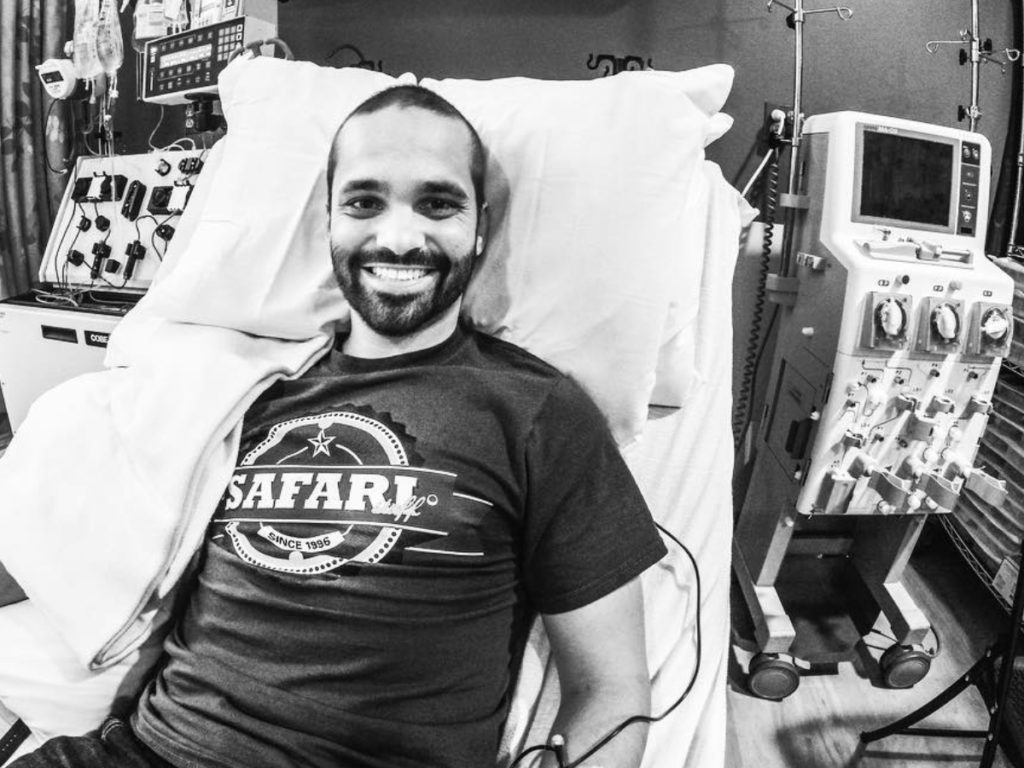
Tylere P.: I’m currently in Grand Rapids, Michigan. I was diagnosed with Hodgkin’s lymphoma in 2014. As of August 1st of [2022], I just hit my five-year anniversary of no chemo so that’s pretty big. I am a videographer and photographer. I also own an insurance agency so I got a lot going on these days.
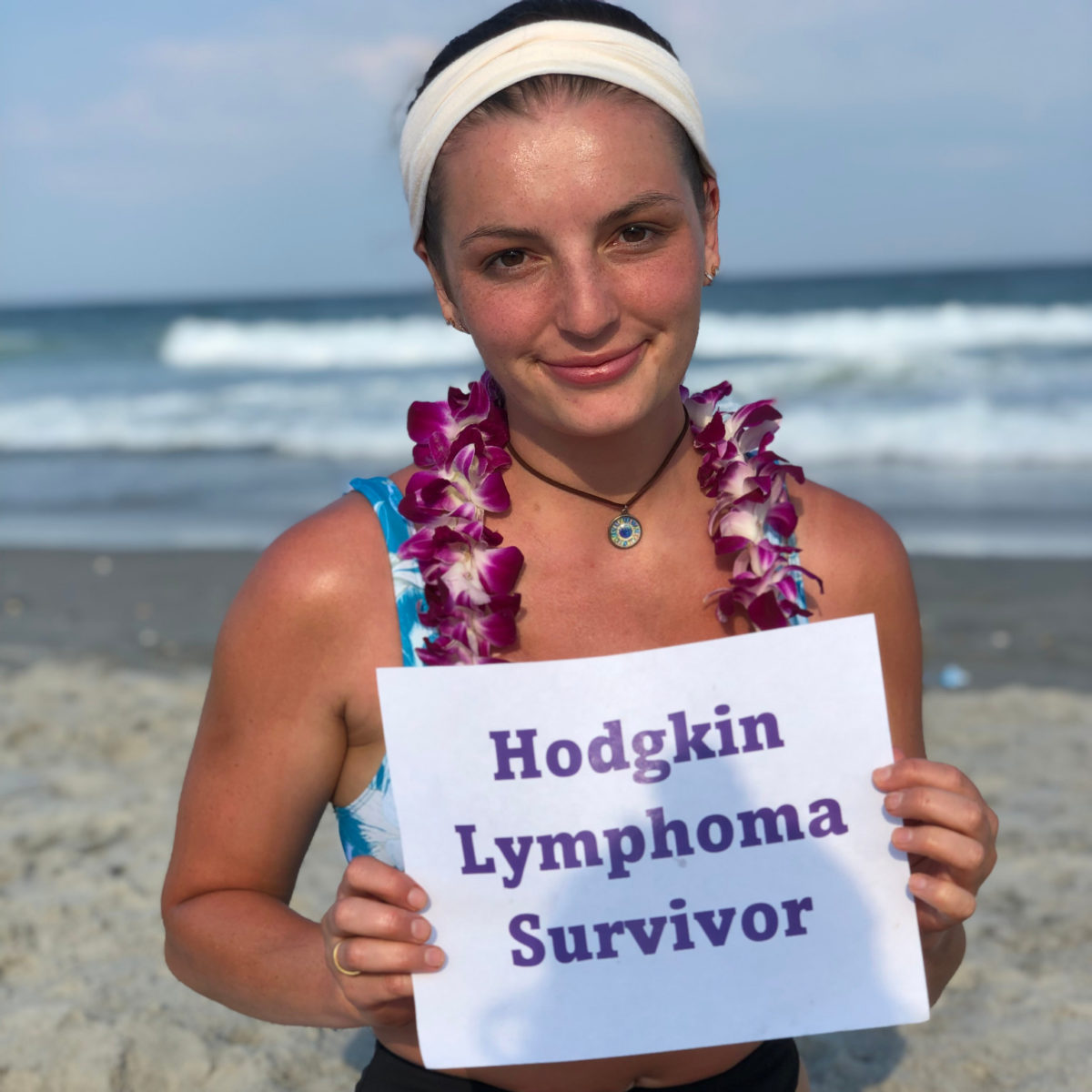
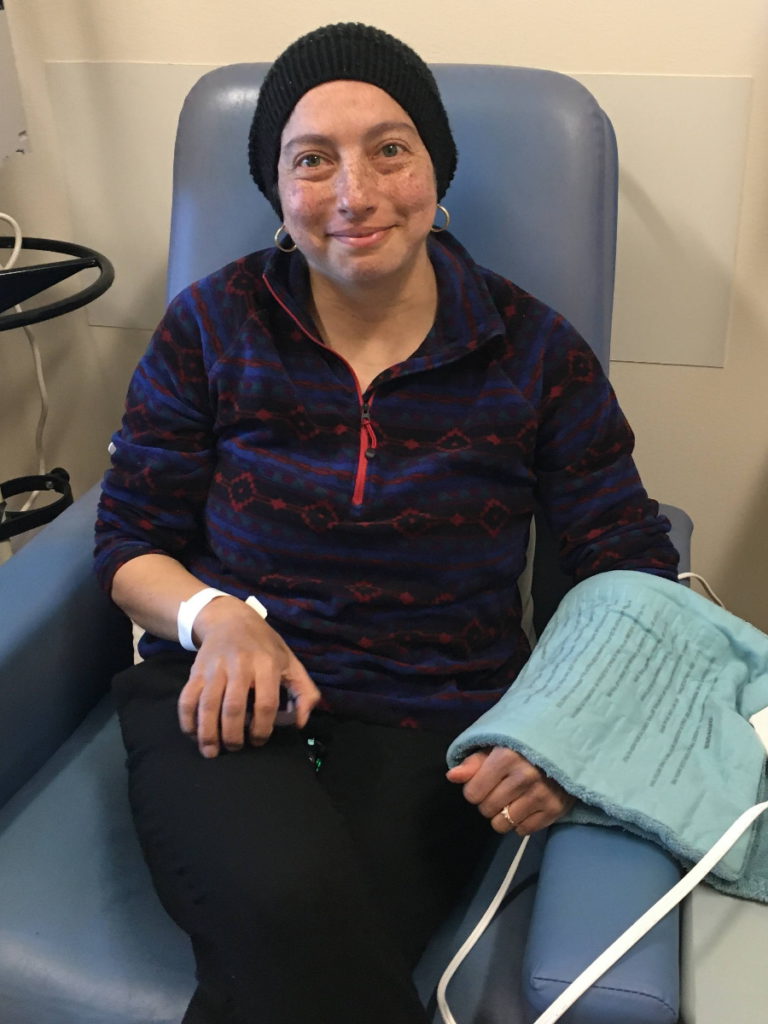
Kelsey R.: I’m from Bentonville, Arkansas, which is my hometown, but I actually live in Austin, Texas. I was diagnosed with stage 2A Hodgkin’s lymphoma in September 2017 and I’ve been in remission since March 2018. I am an architectural historian and a writer. I dabble in comedy writing and screenwriting. I also own a vintage furniture company.
Stephanie, The Patient Story: Each of our panelists really represents a different situation so we’re going to be able to hear a range of experiences.
It felt like I had to really talk my way through it, constantly let them know that this is not normal.
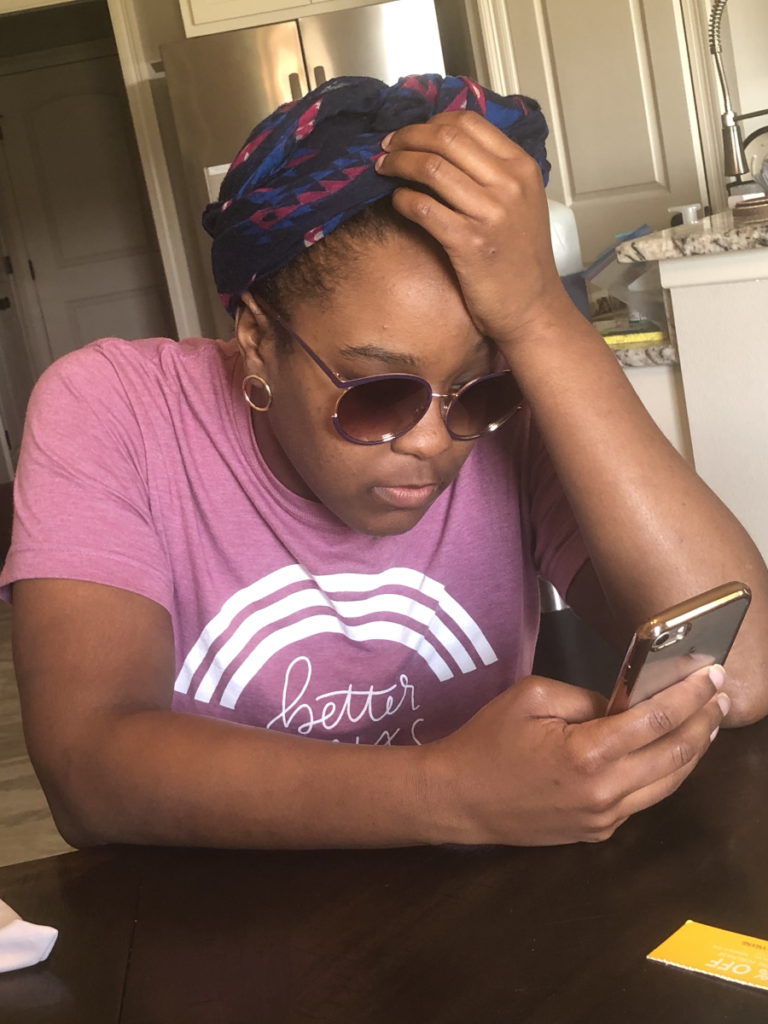
Delishea A.
“Doctor Knows Best”
Stephanie, The Patient Story: I don’t know if you felt that. I’ve definitely felt this, “I don’t want to be that patient.” I don’t want to annoy my doctor. I don’t want to speak up too much. They’re trained; I’m not.
There’s a lot to talk about here when we say self-advocacy because it is our [life] after all. Delishea, there are different instances of this for you, but it took a while to actually get diagnosed. Even before getting diagnosed with Hodgkin lymphoma, can you describe what happened?
Speaking up about 1st symptoms
Delishea: The symptoms lined up with COVID symptoms. I also had uncontrollable itching. At first, I was just discounting the itching as a dermatitis issue. I know I was tired a lot.
During that time, we [had] the stay-at-home order. We weren’t working so I thought it’s just from being tired because I worked, worked, worked before. Each symptom seemed like I could discount the actual symptom for something else.

What really brought me to the doctor was a lump on my neck and he immediately did tests — MRI, bloodwork — and it came back as lymphoma.
Stephanie, The Patient Story: You had described feeling during that time, the run-up to getting the actual diagnosis, like you were trying to tell people, “I have all these things that I’m feeling. I know it’s not right.” Can you describe what that felt like for you?
Delishea: It felt like I had to really talk my way through it, constantly let them know that this is not normal. It took a little bit.
Each symptom seemed like I could discount the actual symptom for something else.
Delishea A.
Stephanie, The Patient Story: It can be hard to fight through that. Erica has a very specific situation, too, in terms of a cultural difference where you felt really unheard. Can you talk about what happened there?
Speaking up about cultural differences (and being listened to!)
Erica: I had symptoms that I did present to my doctor. There wasn’t a lot of lag time between getting seen by my primary and then getting tested. When I finally met with the oncologist, it was really trying because, at that point, I had a feeling I had Hodgkin’s lymphoma. All the signs were there.
I was going into the appointment knowing I was going to get that diagnosis. I wanted to present my needs and that was a lot of cultural… I wanted to have conversations [with] a nutritionist about how I can integrate that care and it wasn’t listened to. There were statements that made me really uncomfortable.
When I stepped out of the appointment, I turned to my husband and said, “I cannot go through this process if I’m not going to be able to have a conversation. I get that I have to have treatment, but I need to know that they’re going to listen to what I need to get through this.”
I wanted to have conversations [with] a nutritionist… and it wasn’t listened to. There were statements that made me really uncomfortable.
Erica H.


I started exploring different doctors until a friend said, “Why don’t you just look within the network that you’re in? Maybe there’s another oncologist.” It’s already uneasy, but my primary concern was that I wanted to be heard.
I was fortunate enough to find a doctor who was willing to do that. Basically, they said the same thing as the first doctor, but their statements were presented [differently]. He explored some of the things that I wanted to look into.
Stephanie, The Patient Story: I want to highlight that because it seems small. At the end of the day, both doctors agreed essentially on the same thing. They had the same opinion about treatments. But one doctor dismissed you right off the bat because they [didn’t] know about this cultural thought process with treatment. The other one, what did it mean? What is that difference? It seems minor, but it’s pretty big.
My primary concern was that I wanted to be heard.
Erica H.
Erica: It was big because it just showed being able to advocate; that was really important for me. I’m an admissions consultant so I teach students how to self-advocate. Now, I was actually putting into practice for [myself] in a health crisis. I know that they are the experts in [the] medical field but I am an expert on how I feel.
Not having my feelings dismissed was so important. I had done readings on all these ideas, like mind-body [connection]. I want it to feel positive and that doctor made me feel positive about this — that it wasn’t going to be as scary as it already was for me.
They understood I had a whole team around me who would voice their concerns and opinions on what I should do and I could have conversations with him about that. Knowing how to respond to those people, he became a partner in this process of treatment and healing.
Stephanie, The Patient Story: I want to highlight that word: partner. That’s what we’re aiming for. Everyone feels like they’re part of this.
Not having my feelings dismissed was so important.
Erica H.


Shared Treatment-Decision Making
Stephanie, The Patient Story: Shared treatment-decision making: what does that mean? It means that it’s not just one-directional. It’s not the medical team only and the doctor only. I’m part of this. This is my life. I know that you have the training, but I want to be empowered in my care.
Kelsey, [your story] is actually a really great example of advocacy. If you could give a little [background] of what your treatment was, the impact, the side effects you were feeling, what got you to research, and the impact of the research.
Doing my own research and changing treatment path
Kelsey: I had stage 2A Hodgkin’s and was prescribed ABVD chemo — I believe it was four cycles, eight treatments total. After, I think, my fourth treatment, I ended up in the hospital with neutropenic fever. I experienced really low white blood cell counts during my entire course of treatment, starting right after my first chemo.
I picked up something small [and] ended up with pneumonia over Christmas.
Kelsey R.
It was the middle of winter [with] a lot of colds going around. I picked up something small [and] ended up with pneumonia over Christmas in Arkansas. I was in the hospital for four or five days dealing with that and that was probably the lowest point in my treatment.
When I got back to Austin, I asked the doctors and nurses if I could add Neulasta to my regimen, which would boost my white blood cell count [and] make me less susceptible to infection. They told me that I could not do that because it would interact with the Bleomycin in the ABVD.
I was already experiencing some side effects from Bleomycin. It can cause lung scarring. I wasn’t having that issue, but I was just scarring all over my body. I could tell it was not great. I was wondering if it’s doing this to my arms, what’s it doing to my lungs?
I found some recent studies that had shown [that] the Bleomycin could be safely removed from the chemo.
Kelsey R.
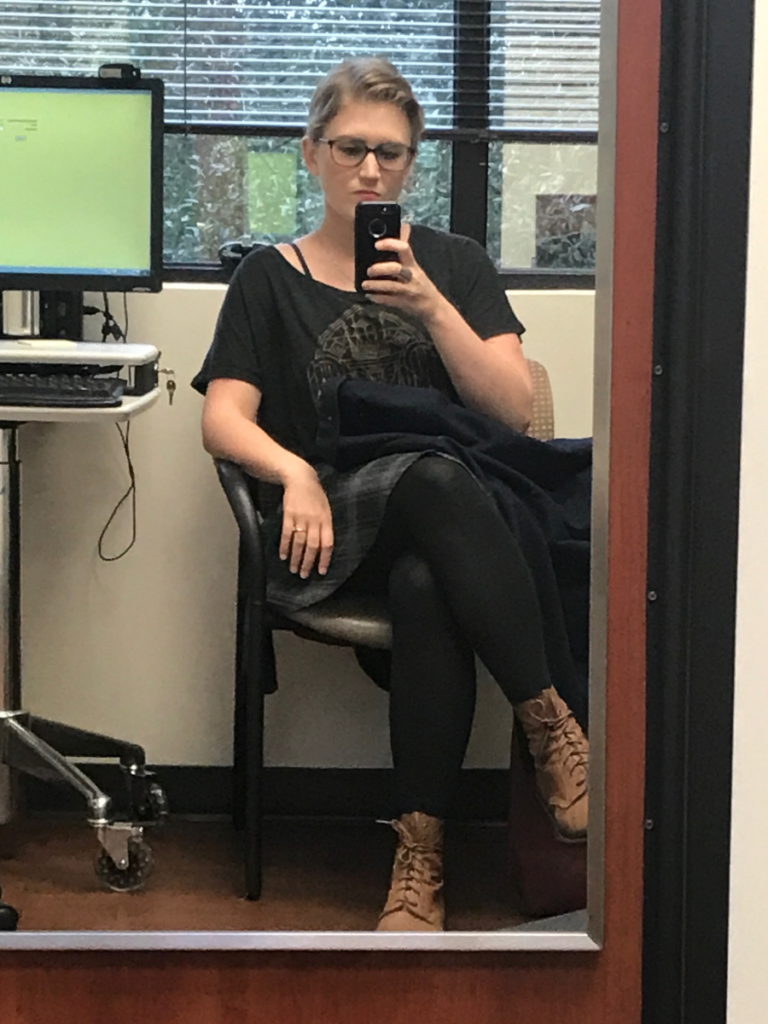
I did some research and I found some recent studies that had shown, I believe, people who had 12 total ABVD treatments, so six rounds, if they were clear after their second cycle, then the Bleomycin could be safely removed from the chemo. I brought that to my doctor and said, “I know this isn’t my exact situation and I have fewer treatments, etc., but do you think that this would work for me so that I could add Neulasta so I don’t end up in the hospital again? Because I feel, at this point — because I’d already had a clear scan — that that’s a greater risk to my health.”
My doctor agreed with me and actually commented that he’d just been discussing that research at a conference he’d just been to. I removed that from my regimen and I’ve been in the clear for five years almost so seems to be fine so far. I remember his wording exactly was, “Yeah, that makes a lot of sense.” That worked out for me and I was able to take the Neulasta to get my white blood cell count up and did not end up in the hospital again.
I was so terrified that someone I would come in contact with had a roommate with the flu or something because that could have been really, really bad for me at that point.
Kelsey R.
Stephanie, The Patient Story: Now we’ve been through COVID, we understand more [about] being immunocompromised and feeling like [we can’t] just go anywhere. Everything’s going to infect me. It could lead to hospitalization, which it did for you. Describe the impact [on] your psyche or just your emotions to feel like I can’t do anything right now because of this treatment.
Kelsey: I don’t think I quite understood — at the beginning of treatment and when my white blood cell count got really low — the impact of that and what that meant for me. I felt like always having to be in a bubble and, [as] you said, a lot of people got a taste of that, especially at the beginning of the pandemic when we were all terrified.


Once I ended up in the hospital — it was a really nasty flu season — the doctors were being so careful with me and that really freaked me out. That time in the hospital was really, really rough. Before I was able to get the Neulasta, I lived in isolation, which I was doing already. I’m pretty sure I picked this up in line at a pharmacy actually.
I remember my dad would wipe down the cup when we stopped at the gas station. You feel extremely vulnerable and I was so terrified that someone I would come in contact with had a roommate with the flu or something because that could have been really, really bad for me at that point.
Stephanie, The Patient Story: You had no defense systems.
Also, you had research experience, being in grad school, so [you had] access [and] the know-how to research this stuff, but what about other people who don’t have access? You were able to empower yourself with that knowledge, you brought it to the doctor, and that started this very important cascade of events. Any last thing you want to say in terms of the ability to research and know? What got you to speak up? Did it take much?
Kelsey: It was just that stay in the hospital. There was a man who was dying in the room next to me and crying out a lot. It was a really, really scary experience. There was a lot of infection around me and the doctors were scared that I was even in the hospital because it could kill me. That fear is when it really hit me how very, very serious this is.
I’m a chronic researcher. I just will research things to the point where it’s not healthy sometimes and so this was something I just really was looking into because I was looking for any option to be able to get the Neulasta. This is why I think sites like The Patient Story are so important because if I had had someone who had been through that before to tell me this, it would be a lot easier and a lot less scary.
It really hit me how very, very serious this is.
Kelsey R.
I remember asking, ‘Can I just not receive the Benadryl?’ The side effects from the Benadryl, I notice more than the side effects from the chemo
Tylere P.
Stephanie, The Patient Story: Tylere, I know for you it was a little bit different. During one of your treatments, they had Benadryl — a very common medication that’s given to help avoid allergic reactions but for you, that was kind of the problem. Can you share that with us?
Speaking up about medication side effects
Tylere: Going through the chemo, I never had any bad side effects. I still had an appetite. The worst thing that happened was losing my hair.
I remember getting Benadryl one day before they were giving me chemo and I was knocked out afterward. I would drive myself to my chemo appointments and the hospital was about an hour away. This is when the cancer relapsed.
It took about an hour, an hour and a half, for the chemo that I was on, and then I’d have to stay for an extra hour and a half just for the nurses to feel comfortable letting me go home because of the Benadryl. They didn’t want me [to fall] asleep while I was driving, which is great, but I also didn’t want to be in the chemo chair any longer than needed.
I remember asking one day, “Can I just not receive the Benadryl? Can we just see what that does? Was that a possibility?” They checked with the doctor. They said, “The doctor said that’s fine. We can forego that.”
After that, getting the chemo treatments was a much easier experience for me. The side effects from the Benadryl, I notice more than the side effects from the chemo, even though I’m sure my body was going through a lot through the chemo.
Stephanie, The Patient Story: I love this example because we know that it’s supposed to help, but you knew your body. You knew that you weren’t having a reaction.
When we talked about this, you said you were so drowsy [that you had] to depend on somebody else. You’re a very independent person. Can you describe that impact for you?
Mentally, it was nice to be able to do things on my own.
Tylere P.


Tylere: Being independent, I like to do things on my own. I didn’t want to have a friend or family have to be with me during chemo and be an inconvenience for them. Mentally, it was nice to be able to do things on my own. If I’m able to go get chemo by myself, that’s fine. I was there every couple of weeks for over a year plus. It wasn’t anything that I wasn’t used to.
The first few times getting treatment, I had friends and family there. After that, I was like, “Well, I don’t want you all waiting around for four or five hours.”
Stephanie, The Patient Story: Being able to speak up for yourself in that instance allowed you to have control of that again because otherwise, you’d be, “I need you to drive me.”
Being independent, I like to do things on my own.
Tylere P.
Protecting Our Boundaries (+ Energy!)
Stephanie, The Patient Story: Protecting boundaries and energy: what does that mean? It’s “I don’t want to offend other people.”
Delishea, you lived with your sister for part of the treatment and you talked about mama bear. Could you just describe what that meant?
Hard conversations with parent caregivers
Delishea: I can’t imagine seeing your child go through [something]. [In] the beginning, she was very hands-on. She was the one that had to take me to the appointments; really wasn’t anybody else stepping in and I just call that mama bear.
But it came to a point where I was like, “Let people help to make things go smoothly.” When I changed doctors, my sister had to be my caregiver and she didn’t really have as much access to coming to the appointments. Instead, we would record the appointments for my parents so they can listen in and if they had questions, they gave us the questions and we would ask for them. But other than that, it was a rollercoaster.

I’m still processing what I’m going through and I don’t have the mental space to nurture your feelings about it, too.
Delishea A.

Stephanie, The Patient Story: Moms are great, but there is a balance, right? It’s wonderful getting that support, but at the same time, does it feel like I have to manage other people’s feelings, too?
Delishea: Yes. Big time. When going through it, your emotions [are] all over the place. I don’t know if it was the chemo, the anxiety, [or] all of it together. My caregivers and my support system [were] going through it with me so I was very cautious of their emotions, too. I don’t think anybody knew how to handle it.
A lot of times, I would bring my earphones and listen to music or just be honest. “I don’t feel like talking. I don’t feel like being bothered.” They know me [and] my personality so I didn’t think they were too offended, but I have to set those boundaries. I’m still processing what I’m going through and I don’t have the mental space to nurture your feelings about it, too.

Stephanie, The Patient Story: I am really thankful that you’re bringing this up. It can be hard to talk about, but it is so true and I’ve talked with many other people who feel the same way. As soon as we get diagnosed, [there’s this feeling] of I don’t want to hurt this person’s feelings. There’s just a lot going on. I appreciate that you set an example of [taking] care of yourself first, [giving] yourself some grace. It’s okay to say no.
Tylere also had an experience having to learn how to protect boundaries and say no. Describe a little bit more about your mom, what she does, and how those first appointments were for you.
Tylere: My mom is a nurse practitioner and she’s actually the one who told me that I have cancer. We noticed I had a swollen lymph node. I asked her, “What does that mean?” She was like, “Well, it could either be just some sort of infection or worst-case scenario, it could be cancer.”
We got that checked out. After a week of antibiotics and then being told I need a CT scan, kind of figured, okay.
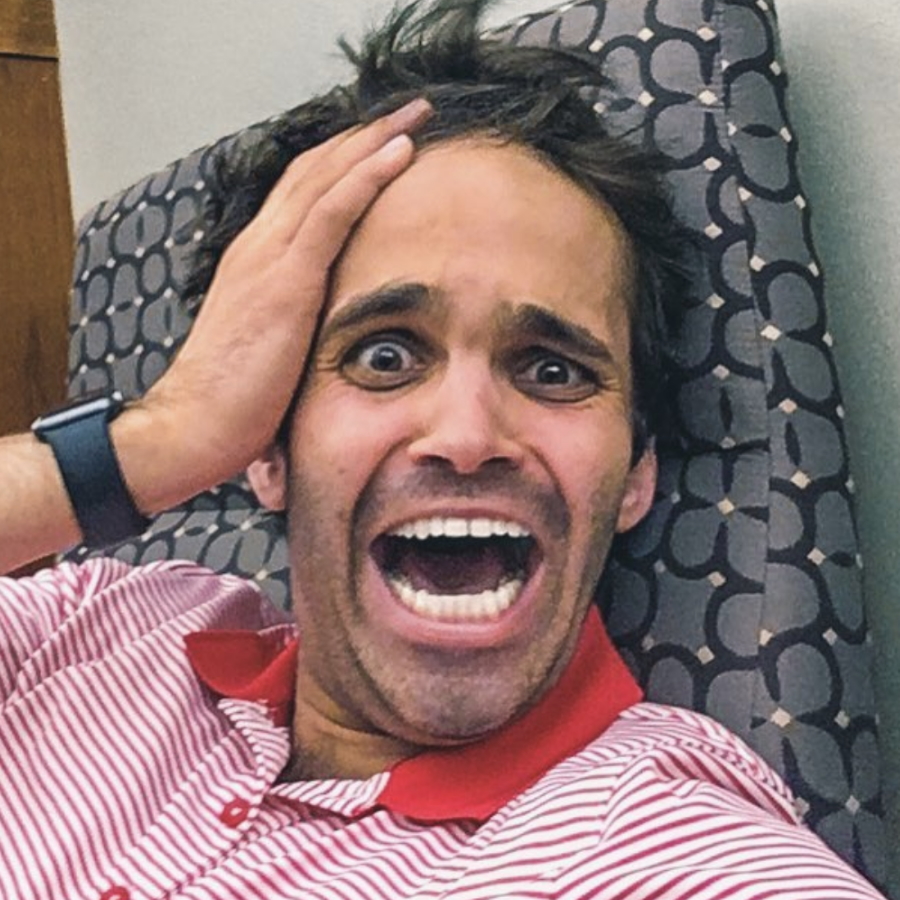
I was in a conference room at work and had all my co-workers around me. She called and said, “You remember when I said worst-case scenario?” I said, “Yep.” She goes, “Yeah, so it’s going to be [the] worst-case scenario.” My response [at] that moment was, “Oh, okay, great!” Because I’m literally surrounded by all my co-workers and I haven’t really told them what’s going on yet.
Dealing with my mom being a nurse practitioner [is] like a blessing in disguise. A lot of the more medical questions or things that could or could not happen, I leave that up to her. If I had questions that the doctors were asking, I ask her in more detail afterward.
She called and said, ‘You remember when I said worst-case scenario? It’s going to be worst-case scenario.’
Tylere P.
I moved back home after the cancer had relapsed. Being independent, being told I had cancer wasn’t the worst part of this process — it was being told that I was going to have to move back home with my parents. That was very hard for me. I didn’t want to be a burden and I just didn’t want to be back home. It wasn’t a place that I wanted to be at 24, 25, living with my parents. But that’s what ended up happening.
My mom was coming to [my] appointments and I told her I can’t have her come anymore. It got to the point where, essentially, if the doctor asked me a question or asked me my name, by the time he said “name,” if I wasn’t saying “Tylere,” she was the one responding.
Being told that I was going to have to move back home with my parents… that was very hard for me.
Tylere P.


We had a long conversation one day [with me] saying, “I just need you to not come to these appointments. It’s not good for me mentally. It’s not good for me emotionally. I just need to be in a good space. Basically, I moved back home to make this easier on you all.” Originally, I was going to go to Houston to be treated but came back to Michigan to make it easier so the family didn’t have to travel in case they needed to be somewhere for me.
I was already withdrawing a lot from my emotional bank to be back home. I said, “If there [are] questions that you feel like I need to be asking the doctor, I will talk. I will tell you after I get back from the doctor.” Give her a summary of what happened [and] what questions I asked… If there’s anything that she wanted to ask going into it, I could ask them. If she didn’t feel [the] questions I was asking were adequate, then we could have another discussion about that.
I wish I would have had that conversation sooner of just being upfront about it.
Tylere P.
I know that was very hard because I told her in that conversation, “I don’t have any children so I don’t know what it’s like to be a parent with a child who’s going through this. I’m assuming as a parent you want to be there for your kids and do everything that you possibly can. But, at this time, I’m a grown adult and I would like to be able to answer these questions from the doctors. I also just need this for my space.”
If that was her process for going through this, I was giving her that space. But that space was impeding my space and I could no longer allow, [at] that time, to take over my space.
Stephanie, The Patient Story: It’s hard. There’s a juggling of things going on here where you’re trying to be mindful. You said something about [not wanting] to rob them of their experience of being parents in this way. At the same time, it’s already hard being home. I want to be independent. I still need to feel like me, like Tylere.
Are there any tips in terms of how you were able to move from “I don’t really want to talk to my mom about this, I know she really cares” to “I’m just going to do it”?


Having a hard conversation
Tylere: I wish I would have had that conversation sooner of just being upfront about it.
We’re coming back from an appointment and she’s like, “Why are you so quiet? You never talk on these rides.” I was like, “Well, I just got chemo. I guess I’m tired and I just had that Benadryl so I’m out of it. I just don’t want to talk about it. I don’t want to think about it. I don’t want to discuss it. I just don’t want to be a part of it.” We pulled in the driveway [and] that conversation turned into an hour and a half about everything.
These are all thoughts that I’ve had before and I was just like, “I don’t know how to express these.” Writing down your thoughts is good, taking inventory of yourself — who you are, what you need — and then having that very uncomfortable conversation.
We had a long conversation one day [with me] saying, ‘I just need you to not come to these appointments. It’s not good for me mentally. It’s not good for me emotionally.’
Tylere P.
Setting boundaries and expectations are huge because I remember my mom was like, “I’ll make you dinner. I’ll go grocery shopping for you. I’ll do your laundry.” I was like, “I don’t want any of those things. Now, I’m not saying I don’t need your help, but when I need it, I’ll ask.”
Stephanie, The Patient Story: Right, and I appreciate you sharing that because, again, it can be very difficult. Sometimes we don’t even know that we’re bothered or that something’s up. If you notice something, just write it down [and] see if it’s a pattern that will be helpful in having these conversations.
Erica had the complete opposite experience. With your parents, it was different.
Speaking up to get support from loved ones

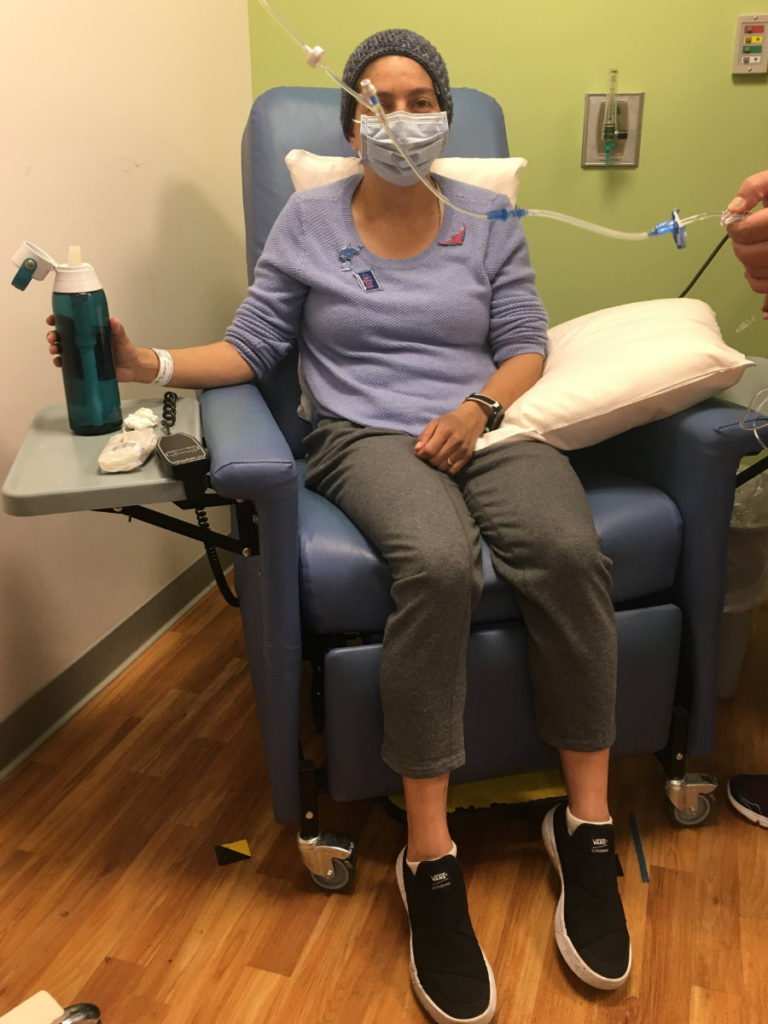
Erica: I’m fortunate my parents live nearby, only 20 minutes away. I do want to be fair to my mom. She did come to my first appointment and then it was too crowded in the room where I was getting treatment. It was a nice way for her not to have to attend since my husband was going to be able to go with me.
I can’t reiterate enough Tylere’s point about writing things down because I wanted to be independent as much as possible and I was able to control that [by] just reflecting on what I would need. Having a doctor as a partner was really helpful in figuring out where those needs would come up but it’s a lot on one caretaker.
I was diagnosed in September 2019 and my treatment was going to fall into the holidays. My husband was awesome. Getting to the appointments, he played a good music playlist and always kept an upbeat, positive environment while I was getting treatment. For the most part, I was able to handle a lot on my own when he was at work, but he was also working full time and it was the holidays. Because you’re immunocompromised, you have to maybe sacrifice a big family gathering.
Having a doctor as a partner was really helpful… but it’s a lot on one caretaker.
Erica H.
They didn’t even realize that I needed them in that way. They were waiting for me to tell them because they thought my husband had it all.
Erica H.
I could see it start to wear on my husband a little bit. He was starting to burn out. I actually told him, “If you are not available to me, I need you to just give yourself a break because it’s not going to be helpful to me.”
My parents, at this point, knew that he was going through a lot but maybe not specifically on how they could support the community that I needed to rally around me. They are emotionally involved and it meant involving them [by] being very specific on how I needed them.
There were things on my task list that I just couldn’t manage, even though I wanted to be independent, [like] disability paperwork. I was still trying to figure out how to get disability checks. I also didn’t know what to cook for myself to deal with the side effects.
I remember just one afternoon telling my parents, “I know that you have a lot going on,” — which they did; there [were] a lot of other things happening in their personal lives — but I said, “I really need you to help me with this paperwork and to help me come up with some good recipes for the side effects. Here’s a list.” They jumped to it. They were so happy and they didn’t even realize that I needed them in that way.
They were waiting for me to tell them because they thought my husband had it all. But once my husband was burnt out, I’m like, I need you now to step in. I was a facilitator of this really difficult process, but it was easier when I was able to direct them on how to help me.
Stephanie, The Patient Story: This is such a great juxtaposition against what we just heard from Delishea and Tylere. When we have this range of experiences, the people around us may or may not know what we need. They may do too much. They may do too little.
In your case, you advocated for yourself because you knew with your husband, “Thank you for all you’ve done, but if you’re not going to have the energy at this next appointment, I need to know so that I can have someone there who can be at 100% for me.” The other thing you did was recognize — my parents, my brother, they don’t really seem to be stepping in. I’m just going to tell them what I need.
It can be hard to be that direct in having those conversations. Did anything help you to have these conversations?
How to bring up and get through tough conversations

Erica: I was really writing intensely — an organization in Berkeley called the Women’s Cancer Resource Center had a writing group. There were things that I was giving to my dad specifically. There’s a cultural component, too. He was having a really hard time adjusting to the fact that I was going through this experience and I really wanted him to hear my needs and concerns. It was just difficult.
In that difficult conversation of being heard of what I needed and what I wanted, I just met what I needed. If he couldn’t respond completely to it, I recognized that and just said, “Okay, I’m going to be direct. Just make me juice. I know you love me and that’s enough. Everything else, we’ll deal with later on.”
Whereas my mom, it’s just different, our relationship, and that was really helpful to her to not get as emotionally charged. It was like, “You know what, there’s some paperwork. I really know you’re good at dealing with this, so can we sit down for an hour?” It was just logical for her to sit down and go through it. I didn’t have to invite her into the emotional piece unless I saw that she was ready for that.
The same was for my brother. Because my husband lives with me, he got all of it, which is why he was dealing with burnout. I couldn’t find any other way than to be direct with him. I said, “I get it was hard for you, and I know you know it’s hard for me, but I need you to go with your brother and watch football. Get away.”
Everyone thought it was weird that [my husband] would go and he was starting to feel guilty. It was the best thing for us because then he came back with energy and I had brought in my parents and my brother to step in for that.
Stephanie, The Patient Story: One huge piece of this is we’re not going through this alone. We are diagnosed with it but along with us is everyone around us — maybe a spouse or partner or family members, friends. Caregivers and care partners need to have care, too. That’s a really, really good message.
Kelsey, you had support, but you also mentioned something about if you’re not in the right place, just don’t be afraid to ask.
Don’t be afraid to ask others for support!
Kelsey: I was lucky that my sister and my husband — at the time, fiancé — and I had some roommates that were very supportive and would help me out. Some grad school friends would make meals.
Sometimes, with such a large support team, it was a lot of breadth, not a lot of depth. There was not a lot of organization so it was difficult for me as a cancer patient going through a lot of mentally taxing medications to figure out what I needed when I needed it.

That was really helpful to me, just being able to identify who can help in what way.
Kelsey R.

I was able to choose [the] most organized, Type A people in my life. One friend put together a meal calendar where people would pay her and she would make me food [during] my chemo weeks.
My husband was not able to come to most of my appointments with me because he had a really unforgiving job at the time and my sister, I enlisted her to come with me because she’s also really Type A.
She actually caught a mistake where a nurse had weighed me incorrectly and was going to give me the wrong dose of my chemo that morning. That was really helpful to me, just being able to identify who can help in what way because my parents weren’t there and my husband was not able to help much.
Stephanie, The Patient Story: Having an extra set of eyes and ears in the room can be so critical. We’re overwhelmed. There’s a lot going on. We’re in the infusion chair and that’s a big mistake that could have happened.
Also, the people you have in your support circle [have] a different language. Some people are better at doing paperwork. Some people may be cooking. People want to help, right?
People want to help
Kelsey: Absolutely. That was the thing that surprised me. I don’t know why because I would gladly help my friends, too. But when my friend organized this meal calendar, people who signed up I maybe had one class with so that kind of community support people were really willing to engage in, which I was very, very appreciative of.
Recording helped because a lot of the times afterward, I couldn’t remember anything.
Delishea A.
Stephanie, The Patient Story: Delishea, you talked about how overwhelming it is [at] the beginning and the importance of having somebody else there. You were going through this during the pandemic. Can you describe how you advocated for yourself to have more support?



Delishea: With my first oncologist, I had to really speak up a lot. It was just a lot going on. Nobody was allowed to come in with me so I had to speak up for myself in the appointments because I didn’t really have anybody with me to remind me what the doctor said. That’s where the recordings came in and recording helped because a lot of the times afterward, I couldn’t remember anything.
Stephanie, The Patient Story: It’s overwhelming. We talked about having someone else there as extra eyes and ears. One thing I learned was you can ask the doctor if it’s okay to record. You can record the appointment on your phone so that you can then share [it] with other people.
As patients, we’re going through a lot — treatment, changes, and then on top of that, sometimes paying for it pops up. Tylere, for you, it’s a little bit of a surprise. Can you share with us [your] experience [with] those hospital bills?
Tylere: I recommend for people who are going through this [to] just keep a three-ring binder — organize your bills [and] your explanation of benefits. I remember getting stacks and stacks of letters and mails. It was all very confusing. This is how much it costs, but you don’t owe anything. Sometimes you do and then sometimes you don’t. It’s weird.
I remember getting a bill for a very large amount of money and I was like, “Why isn’t this paid?” Every three weeks for a year, I was receiving the same treatment and my insurance company decided that out of one of those, they weren’t going to pay for it.
[I had] to talk to the financial office at the hospital about what’s happening [and] what can we do about this. Then [I found] out that there’s an appeal process that you have to do with the insurance company. I did that and then they denied that appeal.
Then [I found] out you can have your doctor make an appeal. The insurance company basically came back and said that [the] chemo treatment I received was not medically necessary and they weren’t going to cover it, even though they covered all the other ones for the past year, so that was interesting.
Then [I come] to find out that there was some financial help. They weren’t going to send me to collections for it. They were actually able to find some sort of grant that was going to help pay for someone in my situation. Luckily, that was taken care of.

Keep a three-ring binder — organize your bills [and] your explanation of benefits. I remember getting stacks and stacks of letters and mails. It was all very confusing.
Tylere P.




Different places, depending on the size of the hospital you’re going to, have different help. The LLS or Leukemia & Lymphoma Society is one organization that does offer some help.
Stephanie, The Patient Story
Tylere: Yes. Make sure you’re having those conversations. I remember having that conversation with our financial department. Why is it on me to appeal this bill? I’m the patient going through all this. Why do I have to deal with these insurance companies about all of this? Figure that out. You’re the one who wants that money. Go after the insurance company. You all deal with this every day. Why is [the] person [who is] going through chemo [the one] having to deal with this or having to put [the] family through this who isn’t versed in any of that?
Stephanie, The Patient Story: Right. Different places, depending on the size of the hospital you’re going to, have different help. Some have patient navigators, some have social workers, and you had talked about, too, researching some of the different resources that could be possible.
The LLS or Leukemia & Lymphoma Society is one organization that does offer some help. If you don’t have the energy, maybe have people around you look for that. [There] are different grants and stipends you can apply for — from co-pay to travel to urgent needs, which [are] rent, mortgage, lodging, child care, food, transportation, [and] so much more.
Mental Health
Stephanie, The Patient Story: A very important topic can get on the back burner a lot. Self-advocacy is speaking up for every part of you, not just treatment and [finances]. Everything is connected to our mental health.
Kelsey, you didn’t really consider the mental health aspect as you were going through treatment. I think that is fairly common. We talk about surviving first. You talk about now, in hindsight, your perspective of mental health.


If you have never really considered your own mental health… do that because that’s been the longest healing process, but the most important.
Kelsey R.
Kelsey: I just really wish I would have, from the get-go, found a therapist [and] taken advantage of any free counseling my cancer center might have had. I had never been to therapy or anything like that before I was diagnosed and I was thinking about it when I got diagnosed.
I asked my oncologist if there were any mental health resources I could look at and I think he was in a bit of a rush to the next patient and he was just like, “Let’s not worry about that right now. Let’s just focus on getting you better.”
I understood his perspective but, [in] hindsight, I wish that he would have said, “Here’s the information for the social worker at our clinic,” or something like that because I think that healing mentally from this has been far [more difficult] than healing physically.
I would really encourage anyone who is recently diagnosed — or even if you are a survivor that’s been out of it for several years: if you have never really considered your own mental health — seeing a therapist, talking to your doctor, or anything like that — to do that because that’s been the longest healing process, but the most important.
Also, the people around me, I didn’t realize until after how difficult it was for my husband because he wasn’t showing how hard it was for him during the process. For caregivers as well, I think that is so important.

Stephanie, The Patient Story: I, again, appreciate highlighting this because we do often forget that. Not just us. As patients, we recognize when our caregivers are burning out or feeling a lot, but it’s everybody else who doesn’t really quite see. It’s not just the person who is diagnosed. It’s the mental health, the physical health, [and] the emotional well-being of these people who are also being the caregivers; that is so important. I really appreciate that.
I didn’t realize until after how difficult it was for my husband because he wasn’t showing how hard it was for him during the process.
Kelsey R.
Sometimes, where you’re going for your medical care can matter, too, because a lot of times, it’s overwhelming. We’ve just been diagnosed with cancer. We’re not thinking about anything other than how are we going to get through this. Am I going to live? Am I gonna lose my hair? What are the side effects?
Delishea, you went to two different medical centers. The first place was a lot more in the community then you ended up going to a big academic center.
Delishea: It was Baton Rouge General.
When I finally moved to a bigger center, I didn’t realize how much everything took a toll on me.
Delishea A.
Stephanie, The Patient Story: Yes, and so you had two very different experiences. The first hospital was very different in talking about mental health compared to the second one. Is that right? Two very different responses when they were talking about mental health.
Delishea: [At] the first hospital, that wasn’t even a discussion. It was basically just this is what you have, this is what treatment you have. The whole experience was lacking.
When I moved to a bigger hospital, they offered counseling. I wish I would have [taken] that opportunity. I didn’t realize how much it affected me.
We went through a hurricane and during that transition, my first hospital oncology center got damaged so I went through a period without getting any treatment — no treatment, not knowing where I was going to go.
When I finally moved to a bigger center, I didn’t realize how much everything took a toll on me. I had a panic attack one night. I knew I needed to talk to my doctor and be on some kind of anxiety medicine. Before that, I never really knew what anxiety was. I never had it that deep to where I was breaking down, so that was a big thing.


Stephanie, The Patient Story: I also appreciate that you’re talking about this because you have these two very different experiences. You didn’t even know what good care looked or felt like [until] you went to Baton Rouge. Was there anything in terms of finally being able to have that conversation? Did you notice an immediate shift [in] yourself? Was your quality of life different after?
Delishea: Oh, yes, very much. I wasn’t used to the small stuff — the snacks, the heated blankets. I didn’t even know it was possible. I felt like I was in luxury and it was just basic common patient care. Before, I didn’t even get that offered.
I love them — my nurses, my doctor. I love that whole team. It was just a big adjustment. Anything I needed, I could just say.
Stephanie, The Patient Story: Amazing. I’m so glad you were able to experience that shift.
Family Planning
Stephanie, The Patient Story: For Hodgkin lymphoma patients, a lot of the mental health piece of it is also being young when you’re diagnosed. [In terms] of family planning, Erica, you talked about being 37 at the time [and] talking to your doctor. Can you share more about what that conversation was like and how you had to advocate for yourself in that discussion and that conversation?
Erica: That first oncologist appointment was, to say the least, dramatic. I was getting diagnosed, not being listened to, and with my notebook in hand, I had a list of questions. My husband and I had just been married for a year and we were in the stages of family planning so that was important for me to ask [about] receiving chemo.
The doctor [said], “You’re too old. This is not going to happen. We need you to get treatment immediately because it’s going to explode.” It just was shocking having to forego an idea that I was planning on. The idea of exploding was really problematic for me.
Self-advocacy really played a role [at] that moment. I didn’t know who my next oncologist was going to be but I knew this was the oncologist who was holding me back from getting a second opinion on fertility treatment.
I asked, “I know this healthcare has a fertility department. Can I at least have a consultation with them?” He put me in touch with the fertility clinic that was part of the network, which was actually a really positive phone consultation. They just said, “We don’t know what happens, but you should go through the opinion of the oncologist.”
When I found my oncologist (that I went with) about two or three weeks later, I had the same conversation with them. Having already talked to the fertility department, he said, “I would just suggest you go through treatment because we don’t know what can happen.” He explained to me the process and I made the decision — just based on that conversation — to withhold it.
My husband and I had just been married for a year and we were in the stages of family planning so that was important for me to ask [about] receiving chemo.
Erica H.
Fortunately, removing Bleomycin was possible through my treatment because his researcher suggested that was going to be helpful afterward to be able to conceive as a possibility, and really respected the conversation throughout.
When I did receive remission, the first thing he said was, “All right, let’s get you healthy so that you can explore that conversation again.” It was just different. I really would say ask just for someone else who is an expert on that piece.
Stephanie, The Patient Story: Right, and don’t be afraid to ask. I think that’s the self-advocacy part.
I just found out that I had cancer so it never crossed my mind. I was just about to turn 30. I never thought about kids.
Delishea A.
It’s interesting. Kelsey talked about Bleomycin and [its] impact [on] the lungs. Now you’re saying that that could have an impact, too, in terms of family planning. All of this is a result of asking questions and digging deeper. The power of that is pretty incredible.
Delishea, you had two very different doctors as well. [Did] a nurse talk to you about that?
Delishea: At the very beginning, she brought up [the] possibility that I wouldn’t be able to conceive. But [I] just [found] out that [I] had cancer so it never crossed my mind. I was just about to turn 30. I never thought about kids. And I was stage 4 so she was like, “You need the treatment. You need it now.” I never explored that conversation of freezing my eggs.


Stephanie, The Patient Story: It’s just all these different experiences. Kelsey, did it cross your mind? You were diagnosed on your 26th birthday so there’s a lot going on. What was the consideration for you?
Kelsey: I was still broke, living with roommates, [and] just finished grad school. It really wasn’t on my mind. It wasn’t something my husband and I — or fiancé at the time — were talking about.
I actually had [the] opposite experience that Erica did. The doctors were really pushing me to explore preserving my eggs. I chose not to do that because I really just wanted to get on with treatment and didn’t want to go through another medical procedure. I was stage 2A so the doctors were able to give me a little bit of leeway there. I just wanted to get on with it. From the research I’d done — at my stage, with my amount of treatment — my chances of remaining fertile were pretty high.
It really wasn’t on my mind. It wasn’t something my husband and I — or fiancé at the time — were talking about.
Kelsey R.
Coming out of one of my biopsies, the nurse was telling me about her friend who’d had cancer and now she’s got like all these kids. At the time, [I was] just thinking, “I don’t care.”
Now, at 30, after having been married for a while, I think I would approach it very differently.
Stephanie, The Patient Story: Thank you for highlighting that. This is a very individual response. It’s all about knowing where you are, what you want, and then advocating for that so that’s going to look different. It doesn’t mean you have to advocate for family planning and freezing eggs and embryos. It also doesn’t mean you shouldn’t be asking. It’s what is good for you.


Tylere, you talked about your experience and your parents supporting that decision.
Tylere: I was 24 when I was diagnosed so this was definitely something that was discussed. My mom was pushing more for it. She would love grandkids, but I have an older brother, younger brother, and younger sister, and none of us have produced a kid for her yet.
The deal was that they would pay for the sperm being frozen. As of today, it is a very expensive child and we don’t even know if we will use that frozen sample or not. But that’s something that we did choose to do. Having the parents’ support in that and saying that they would help financially was a big [deciding] factor.
Stephanie, The Patient Story: Absolutely. There’s a financial consideration to this, [like] their storage fees.
My mom was pushing more for it. She would love grandkids.
Tylere P.
Survivorship
Stephanie, The Patient Story: Having this conversation as AYA or adolescent young adult is just so important.
I found email correspondence between me and someone I was matched to from Imerman Angels. I want to highlight this because having all of you on is a great example of the power of being able to find people who’ve been through it and can share experiences. I feel that’s how we learn what’s possible, by hearing from other people.
What [has] survivorship been like? Any guidance? It’s great. It’s also a huge drop in care for a lot of people; that can be really difficult. Any examples of advocacy during this time of survivorship?

Erica: I’ve now been in remission since March 2020. I take it a day at a time knowing that I can look forward and plan ahead on all things — family planning, building out my business.
What’s now part of my experience is being a resource and advocate for people who are going through cancer. I didn’t know that that was going to be part of my journey. Now that it is, I find it really important to advocate and make sure people know that there’s a whole network of people who are open to [talking] about it and [sharing] their experiences.
Stephanie, The Patient Story: Absolutely. Technology has been a big driver in opening different avenues of communication and figuring out your community.
I take it a day at a time knowing that I can look forward and plan ahead on all things.
Erica H.
Delishea: I [have] just been trying to rediscover what I can and can’t do. I learned that I don’t have the same energy as I did before.
I’d just [graduated] so I’m happy about that. I took time off. I chose not to go back to work [and] I’m fortunate that I didn’t have to. I’m about to try to venture back [into] the workforce because I’ve been having too much lax time.
Stephanie, The Patient Story: I’m biased, but I think you’ve been through it so I think you should take that time. I don’t think you have anything to apologize for there. I think go for it. But congrats on wrapping up school.
Trying to rediscover what I can and can’t do. I learned that I don’t have the same energy as I did before.
Delishea A.


Tylere: I always have a hard time with survivorship, especially having met so many other people who are no longer here with us, who went through similar things that I have. It’s just weird that I’m here, but they’re not.
That’s something that I was unaware of as I’m going through it and just being okay, cool, can’t wait to be done with this, and then we’ll never have to think about it again. Completely wrong. You will always think about this. Anytime you feel anything in your body, now that you are so attuned to what is happening, any little thing, you’re like, “Oh, and it’s back. We’re doing this again. Okay, here we go.”
It is nice being able to think ahead and not worry too much about some things. You can start planning ahead a little bit more. Even if you’re going through it, just plan ahead anyway. Focus on an end goal or on something longer term.
I didn’t know what lymphoma was when I was told and then found out it was cancer. [After] finding out I had it, I realized cancer was everywhere.
Be that person who reaches out and says, “If you ever need to talk, as someone who has gone through it, I would love to just talk to you about my experience,” and not be someone who’s offering solutions. Be a sounding board if you just ever feel stressed out. That’s how I handle it. Being a part of stuff like this is huge as well.
Something that I was unaware of as I’m going through it [was] you will always think about this.
Tylere P.
Stephanie, The Patient Story: Thank you for being a part of this. So much of what you said resonated with me. Being there for people and sharing experiences is very different than giving advice. It feels more like a connection.
I also agree [in that] I thought I’ll be done with this. Congrats on the five years. It’s weird to say because I’m also at five years. At any given time of the day, there’s a moment where I’m [checking my neck] because [it’s] where my lymphoma showed up. I feel like it’s a knee-jerk reaction.
It doesn’t stop just because the treatment stops. There are lasting effects to this that keep going and that mental health piece is also really important. Having people like you share is really critical.
It’s traumatic and there’s a lot going on… allow everybody a chance to just grieve that, process that, and give ourselves grace is so important.
Stephanie, The Patient Story


It’s really easy to downplay in your head the impact that things had on you, especially for Hodgkin’s lymphoma patients.
Kelsey R.
Kelsey: The first couple of years after I finished treatment, I was going through a lot of changes on top of this. I had to push back my wedding so I finally got married. I started my career. I had three of my grandparents die within the next year after so there’s a lot going on at once.
My way of coping with it was just to try to make my life as aggressively normal as possible. I stopped going out, stayed in, was just cooking dinner at home, and just [tried] to be in a domestic, relaxed space. It wasn’t until more recently that I started thinking more about what I [wanted].
I’ve picked up my freelance writing business a little bit more and I started — with my mom and sister — a vintage furniture business that we’re really working hard on. Those things were not things I did at the beginning.
When you’re a young adult with cancer, you really can feel like you’re on an island by yourself. Those little moments of connection have been just massively important to my survivorship.
Kelsey R.
It’s really easy to downplay in your head the impact that things had on you, especially for Hodgkin’s lymphoma patients. It’s easy for us to be, “This [is] cancer with a high survival rate. I don’t deserve to feel so bad about this.” Realizing [that] no, this was a very traumatic event, mentally and physically, and I deserve to acknowledge that. Delishea, don’t beat yourself up for not rushing back into the workforce because you do really deserve that time to heal.
For me, as the rest of you have echoed, just being a contact for other people going through this has been really important. I had no resources. I had one friend who had had Hodgkin’s that I reached out to and then I found a couple of women on [an online community] who had had it. One girl, in particular, was just so kind and gave me so much information that I really made it a point to do the same.
I’ve actually had a lot of friends or friends of friends reach out to me just with cancer in general. I find that when you’re a young adult with cancer, you really can feel like you’re on an island by yourself. Those little moments of connection have been massively important to my survivorship because I don’t feel crazy. I don’t feel like this entire experience was something that I made up in my head.
Stephanie, The Patient Story: I love that everyone [was in agreement] when you were talking about letting everybody have time to heal, that everyone went through a traumatic experience, and not do the thing where it’s like, “Oh, well, it wasn’t as bad as the other person.”
Tylere mentioned losing people and there’s this “a better cancer.” No, it’s traumatic and there’s a lot going on and to allow everybody a chance to just grieve that, [to] process that, and give ourselves grace is so important.
Hodgkin Lymphoma Stories
Jessica H., Hodgkin’s Lymphoma, Stage 2
Symptom: Recurring red lump on the leg (painful, swollen, hot to touch)
Treatment: Chemotherapy
Riley G., Hodgkin’s, Stage 4
Symptoms: • Severe back pain, night sweats, difficulty breathing after alcohol consumption, low energy, intense itching
Treatment: Chemotherapy (ABVD)
Amanda P., Hodgkin’s, Stage 4
Symptoms: Intense itching (no rash), bruising from scratching, fever, swollen lymph node near the hip, severe fatigue, back pain, pallor
Treatments: Chemotherapy (A+AVD), Neulasta