Esther Schorr’s Cancer Caregiver Story

Esther took a vow to her husband, Andrew, to support him in sickness and in health. Then 10 years into their relationship, Esther was suddenly faced with fulfilling that vow as a young wife and mother two kids. She stuck by Andrew as a care partner when he was suddenly diagnosed with chronic lymphocytic leukemia (CLL).
Esther reflects on their relationship, the importance of taking care of oneself in order to take care of others, and processing all the emotions that come with a cancer diagnosis.
Thank you for sharing your story, Esther!
Andrew’s Patient Story

Cancer survivor Andrew shares his CLL story, including clinical trials, connecting with other CLL patients, treatment side effects, and saying yes to life.
Andrew & Esther’s Story

Andrew and Esther share their CLL story, including reacting to a cancer diagnosis and figuring out their next steps together.
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.
“You need to take care of yourself as well as you take care of the person that you love so much who’s going through it.”
Esther Schorr
Introduction
How did you and Andrew meet?
I actually met Andrew outside of Los Angeles at what at the time was called sort of a singles weekend. I guess that was before all the online stuff. We’re Jewish, so it was sort of a Jewish celebration of the Sabbath.
I met Andrew. He had been very involved with this group for a long time and I was kind of a newbie. When I met him, I thought he would be a great match for one of my best friends at the time. I left that weekend thinking, “Nice guy. Probably not for me, but whatever.”
The long and the short of it is that we met again at a reunion of the people on that weekend. In the meantime, I had broken up with somebody and was dating other people.
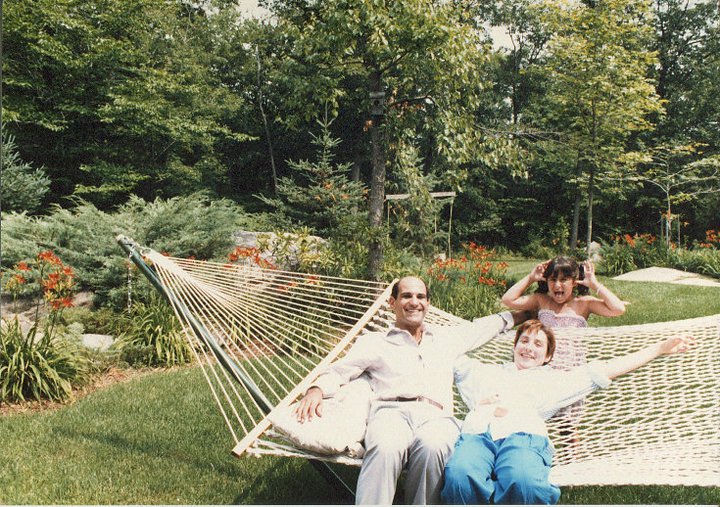
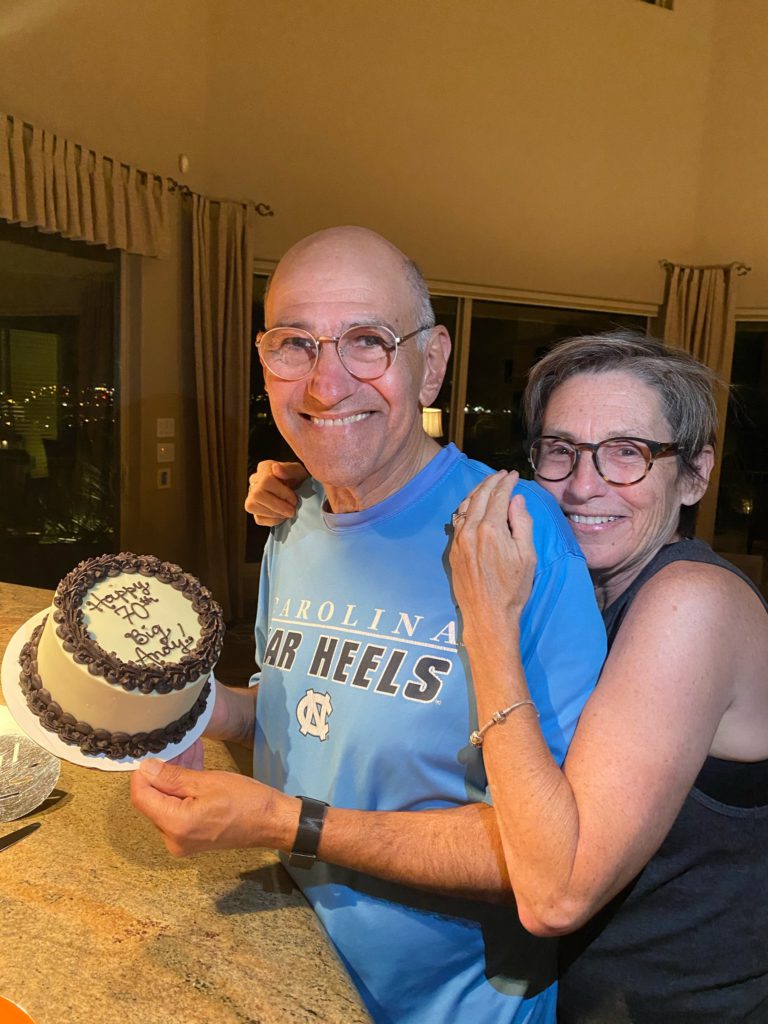
He invited me to go out. We went out and 6 months later, we were married. That’s the story, and that was almost 38 years ago.
It went well. We went to Hawaii together on a trip. I was supposed to go with my mother to Hawaii and instead I went with Andrew. She was okay with it and he proposed to me on top of a volcano. It was very cool.
What were your roles or personalities in the relationship?
Andrew, from the get go, was very much more of an adventurer than I was. I liked to travel, but I hadn’t done as much as I would have liked to, because I just wasn’t doing it on my own.

I’d say it was more of not so much opposites attract, but more Andrew is much more even-tempered and has an even perspective on life than I was and still am. I’m more of an up-and-down emotional relater than he is. That’s carried through our relationship and through the journey we’ve been on with his diagnoses. I’ve just learned to stay more even on a lot of things, and I’m sure we can talk about that.
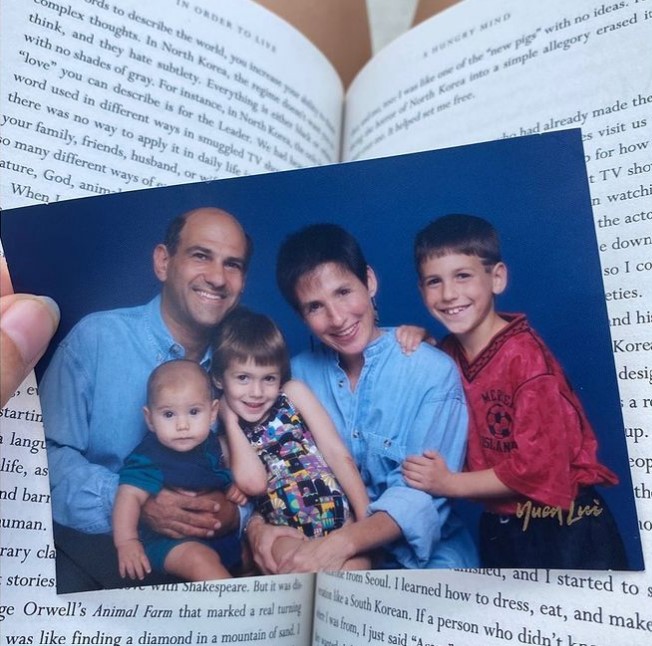
Sort of that fast-forward period in that early part of our marriage, I ended up leaving a corporate job and went into business with Andrew doing videos in the health field. In the middle of all that, we moved to Seattle from Los Angeles and had 2 kids and a dog. We ended up with a dog and a cat. That was the beginning of our married life, and life got hectic.
Health Issues Start
10 years into your relationship, Andrew starts experiencing symptoms
Actually, he was feeling fine, except he was having some nosebleeds out of nowhere. He’s very athletic. He and I were running half marathons, and he was pushing the kids and the little stroller, the jogger.
After a couple of nosebleeds, I said, “You know what? Why don’t you just go to the doctor, let them look up your nose and see what’s going on.” It turned out that the nosebleeds had nothing to do with his first cancer diagnosis.
He ended up having some blood work done.
What, if anything, was going through your head?
Early on, I thought, “We live in a place where the weather is dry.” He wasn’t having any other symptoms. He was exercising, sleeping well, hadn’t gained or lost weight. Up until pretty much the second call from the doctor…
There was a first call of, “How are you feeling?”
“I’m fine.”
The doctor said, “Really? It looks like you may be fighting some kind of an infection. Let’s redo it in 10 days.”
At that point, I wasn’t really concerned when he went back for the second blood test, and then the doctor called and said, “I think we need to do further testing.”
It was then that I was like, “Oh no, what’s going on?” I wasn’t really tipped off until then.
Do you remember the moment of the diagnosis?
I do, and I remember the visceral feeling of being in some kind of strange, very bad dream. It was like I really didn’t believe it. I was like, “What are you talking about?”
Then as I thought about it, I got very, very frightened. Somebody in the Seattle area, a well-known figure, had recently at that time died of chronic lymphocytic leukemia. It was a relatively young guy like Andrew.
I clearly remember Andrew and I just both going, “What?” and being completely gobsmacked. Then, of course, we thought about, “Oh my God, we have 2 young kids.” I think the oldest was maybe 8, and the little one was 4. We were trying to conceive a third child at that time, so it pretty much blew my top off emotionally.
Being a Caregiver
Do you have advice for other caregivers in this situation?
My reaction was one of high anxiety and I would say very close to being incapacitated emotionally. I went and got help. I went into counseling.

I felt that if I couldn’t be there for Andrew and couldn’t be there for the kids and I couldn’t keep it together, then I had to figure out how to get through this in some rational, functional way. What it led to is that I went into counseling.
Andrew and I went into counseling together. We were figuring out what was the treatment, who was the right doctor, etc. I went onto some anti-anxiety medication. That’s not for everybody, so that’s not really advice.
I knew that through talk therapy and through understanding my composition, I needed external help to stay even and rational about what our next steps needed to be. To this day, that has helped me get through some of the other things that have come up along the way.
I’d say the advice is if you’re not dealing, if you’re not on an even keel, it doesn’t mean you can’t feel it and that you’re not going to be upset. But you have to figure out a way to be able to work with your partner or your loved one to make some rational decisions together.
Taking care of yourself so you can be a caregiver
That’s totally it for you as a caregiver, whether you’re a care partner — you’re the person, the main person with the patient — or you’re just part of the support system. The patient is dealing with the patient’s shock, but there are going to be things that a patient has to take care of themselves.
Then there are going to be [things] like in our situation. There were children that didn’t understand what was going on. There was some measure of having to shield them from having them be upset. You have to be present. There are some people who are able to do that without outside assistance, and some just need that additional support for themselves.
Get enough sleep. Don’t stop eating. If you need medication or you need counseling, you need to get them. Do yoga, whatever works to keep you balanced. They’re going to need it.

Support for Caregivers
Value of professional counseling
It’s maybe not even professional counseling, but that’s one outside voice. For me, during some of the latter part, it was my mom. I clearly remember when Andrew first went through treatment, I didn’t want to share with Andrew openly my emotional feelings about that.
He knew that I was concerned, but I needed to have a good cry. I didn’t want to do that when he’s already dealing with his own anxiety or issues. In some cases, it would be somebody who’s in pain. Fortunately for him, it wasn’t.
To have an outlet of somebody else who can support you while you’re supporting your loved one is really important, and it’s not a sign of weakness. It’s that you’re a person, too.

What is the importance of getting support right away?
I think you have to put ego aside. It’s like saying, “I’m strong enough to get through this on my own.” Some people are, but you have to know. You have to look inside and say, “Okay, this is not going to be the even road that we thought it was going to be or that we hoped it would be.”
You have to keep your eye on the end goal. The end goal is for your loved one to get better and for you to be there as fully as you can be to support them. The only way you can do that is for you to be strong and centered as well. You have to know there’s nothing wrong with having human weakness or human emotion.
You just have to figure out how you as an individual have to regulate that and get through it, because it’s going to be a challenge for you in a similar way as it is to the patient, except it’s not happening to you. It’s the emotional part that you’re both going through.
Dealing with Emotions
Processing grief
There’s one other thing I would say. Looking back on it, it’s also dealing with a sense of grief. When somebody dies or when somebody gets very sick, even for the people who are not sick that are watching something like that go on, there’s a grieving process.
For a caregiver or a care partner, as I like to call it, there’s a sense that when somebody you love is diagnosed with something you know is going to disrupt their hopes and dreams in one way or another, it’s going to disrupt yours. You have to kind of let yourself grieve a little bit.
Say, “Okay, this isn’t the hand I wanted to be dealt, but I’m going to have to deal with it along with my loved one. If I need some support in doing that, I need to go get it. Otherwise, I’m not going to be any help.”
Going on anti-anxiety medication
It was for me less depression, but more anxiety. It’s like being immobilized by, “Oh my God, this is something I’m not sure I know how to deal with. Oh my God, my dearest loved one could die from this.”
I didn’t know what treatment was going to be like. Some people, I think, can say, “This is what it is. Let’s move on. Let’s do it together.” For me, I had to process the emotions and the fear. There was a fear as well.

Over time, I’ve learned to put certain feelings in boxes. I think that’s a skill that gets learned along the way, especially with something like a chronic cancer or a chronic disease.
You kind of worry when you have to worry, and otherwise kind of put it in the back of the closet. “I’m not going to worry about this now.” I may be jumping ahead, but that was something that I felt like I needed to learn. Save my real worrying for when I really have to worry.
How were your emotions day to day?
This is just for me how this was. When I would start to think about what could happen, I was looking at a man that looked very healthy to me, but I was told that at some point he’s going to need treatment, that it’s cancer. When somebody still says “cancer,” you don’t want this in your life.
For me, it was trouble getting to sleep at night, palpitations, my heart would race, crying. “I don’t know what to do. I don’t know how to function, trying to keep it together for the kids and not frighten them.” There was a lot of just not feeling good at all.
That was the stuff I felt like I had to get past. I had to figure out how to function normally. Counseling, medication for me and regular exercise helped. Also, having conversations with other loved ones who were supportive, whether it was my mom, my brother, a best friend. What I needed to do is build that network for myself while Andrew was building his network. Sometimes they overlapped.
How did you figure out the right people to talk to?
As far as the people, let’s start there. As far as the support system of friends and family, I chose my mom. She was a social worker, so she was very tuned in to that. She also knew me best.
My father was more of an engineer, pragmatic kind of guy. Not that I couldn’t talk to him, but I had a different relationship with him. I’d always shared very emotional things with my mom, so I chose her for that reason.
I had a couple of friends. My recollection is I had a couple of friends who, in their family, they had dealt in one way or another with a serious condition. They had gone through what we were going through, whether it was with a spouse or a parent or a child. I figured that they could relate and maybe help me kind of pull apart what was going on for me and give me some advice for how to manage that.
Peers are selective because I knew there were certain people in my life, acquaintances, that would just say, “Oh, my God, oh, my God.” That wasn’t going to help me, and it wasn’t going to help Andrew. That was a process of really looking at my relationships and saying, “Where could I safely and effectively get that support?”
Research and Tools
How did you and Andrew approach researching CLL?
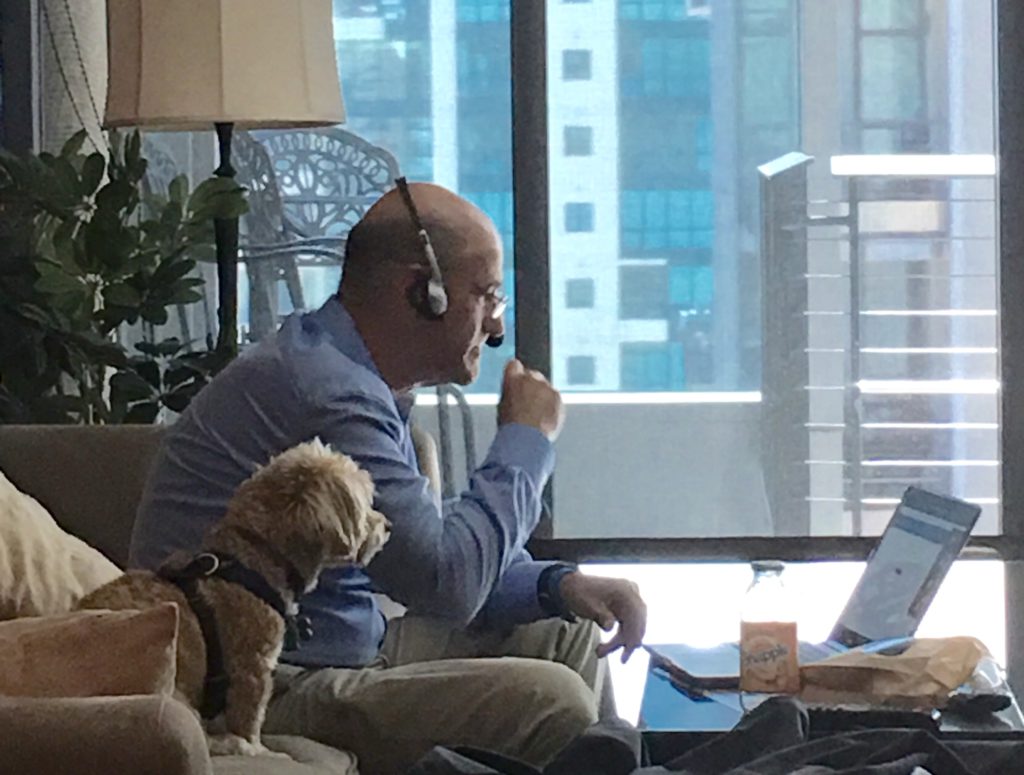
Andrew, by his own nature, was a journalist and wanted to know the answer to everything. I’m a project manager by nature, so I’m a researcher in putting things in order. In that sense, we work together.
One of the first things we knew we needed was, “What the heck is this?” We’re like, “Okay, they said it’s some sort of a chronic cancer. Well, what does that mean?”
We were also told, “You probably aren’t going to need treatment for a while.” We were confused. Our way of together dealing with it is to try to get as much information about what we were dealing with. What is a chronic cancer? What was this cancer, different from that cancer?
At that point, we were working together on it. I think we went back and forth. Andrew’s quite stoic. I don’t mean that he doesn’t feel things, but he’s a pragmatist. He just sort of pushes through them.
There were things that I just said, “Andrew, you find out what we need to do and tell me what I need to do to support you.” In other cases, I said, “You know what? I need to understand this, so I’m going to go and get the answers.” It’s really teamwork.
»MORE: Learn more about supporting a spouse through cancer
Can you describe the tools you’ve developed to help?
Tools first. If you are not functioning well and feeling adrift and feeling anxious, don’t be afraid to look for outside help. You’re probably not going to get that from the patient, because they’re dealing with their own things. You need to seek counseling and seek peers who will understand what’s going on, like family members. Get support.
If you find that there’s physiological things going on, sometimes for some people — whether it’s medicine or marijuana or other supplement, acupuncture, exercise, yoga, meditation — any of the things that can help you feel centered and in control of your own emotions so you can think clearly is really important.
We were talking a little bit about compartmentalizing. Over time, when there were bad milestones [like], “Uh-oh, my person needs treatment or numbers are going in the wrong direction in blood tests,” my tool has been, “Okay, is this something that I need to worry about right now, or can I save my worrying for when there’s something really drastic that warrants pulling out all the stops?”
I’m going to worry, I’m going have a good cry, and I’m going to go back to a counselor. I will get through this. I think that’s the best way for me to describe the compartmentalization. Also, the one other thing is living in the moment.
At my darkest times when I’ve just felt like I could see a potential train wreck coming, I say, “I don’t know if I’m going to get hit by the train, so I’m here right now. My loved one is here right now. We need to live in this moment.” It’s a practiced skill, and I’m not always successful at it, but it’s something to work on.
What is the main takeaway for caregivers?
I would say to anyone who has to support somebody with a serious illness, you need to take care of yourself as well as you take care of the person that you love so much who’s going through it. If you want to be there for them, you need to figure out how to stay stable, how to stay the course, and do what you need for yourself so that you’re fully there to support the person that you love.

Inspired by Esther's story?
Share your story, too!
More Spouse Caregiver Stories
David Garrigues Ronda, Spouse of Laurent Gemenick, Bladder Cancer Patient
“Talk to family, talk to friends. Ask for help. Don't be alone. And above all, don’t miss any doctor's appointments.”
...
Lung Cancer Caregiver Series Episode 2: Stephen and Emily Huff's Candid Conversation
"We talked, and I remember saying, "What if we have kids and what if I die?" And you were like, "What if you live?"
...
Emily Huff, Spouse of Stephen, Lung Cancer Patient
“Emily's the reason why I’m alive today. The treatments have kept the cancer at bay, but she's the one who’s kept me living, breathing, and enjoying life.”
...
Blair D., Spouse of Brain Cancer Patient
“Find other people who are going through the same thing you are. This journey is very isolating and very lonely.”
...
Nat G., Spouse of Bladder Cancer Patient
“You have to become selfless as a caregiver. You have to assure that person that you are there for them.”
...
Kyle Appleford, Spouse of Lung Cancer Patient (Metastatic) with No History of Smoking
“Ask for help. Don’t be too prideful to accept the help. I wouldn’t be here without all the support from family and friends.”
...






