Kevin’s Invasive Transitional Cell Carcinoma Kidney Cancer Story
Kevin shares his transitional cell carcinoma kidney cancer story, undergoing surgery, and the path to recovery.
In his story below, Kevin also highlights how he navigated quality-of-life issues post-diagnosis, including the importance of advocating for himself as a patient, the importance of caregivers, and how he and his spouse managed differences in how to approach kidney cancer treatment.
Thank you for sharing your story, Kevin!
- Name: Kevin R.
- Diagnosis (April 2013):
- Kidney
- Transitional cell carcinoma (urothelial carcinoma)
- Invasive
- High-grade
- Symptoms:
- Blood in urine
- What led to diagnosis:
- Cystoscopy
- CT scan
- Treatment: Surgery
- Diagnosis
- What were your first symptoms?
- How did you get diagnosed?
- When did you get the scan results?
- How long was it between the symptoms and diagnosis?
- Describe the first phone call from your doctor
- How did you break the news to your wife?
- How did you approach telling your daughter?
- Telling your work about the diagnosis
- Path to Treatment
- Surgery and Side Effects
- Surgery Recovery
- Quality of Life
- Advocating for yourself during your cancer experience
- Did you and your caregiver (spouse) have different styles in approaching treatment
- How long were you gone from work
- How important is it to have caregivers
- Did you have help with figuring out work and taking time off
- What were the most emotional moments
- Advice to those who’ve been diagnosed
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

I’m telling you now, there is a way through this. Develop the resources you need around you with your families and your friends and your community now, because they will help you through this.
Kevin R.
Diagnosis
What were your first symptoms?
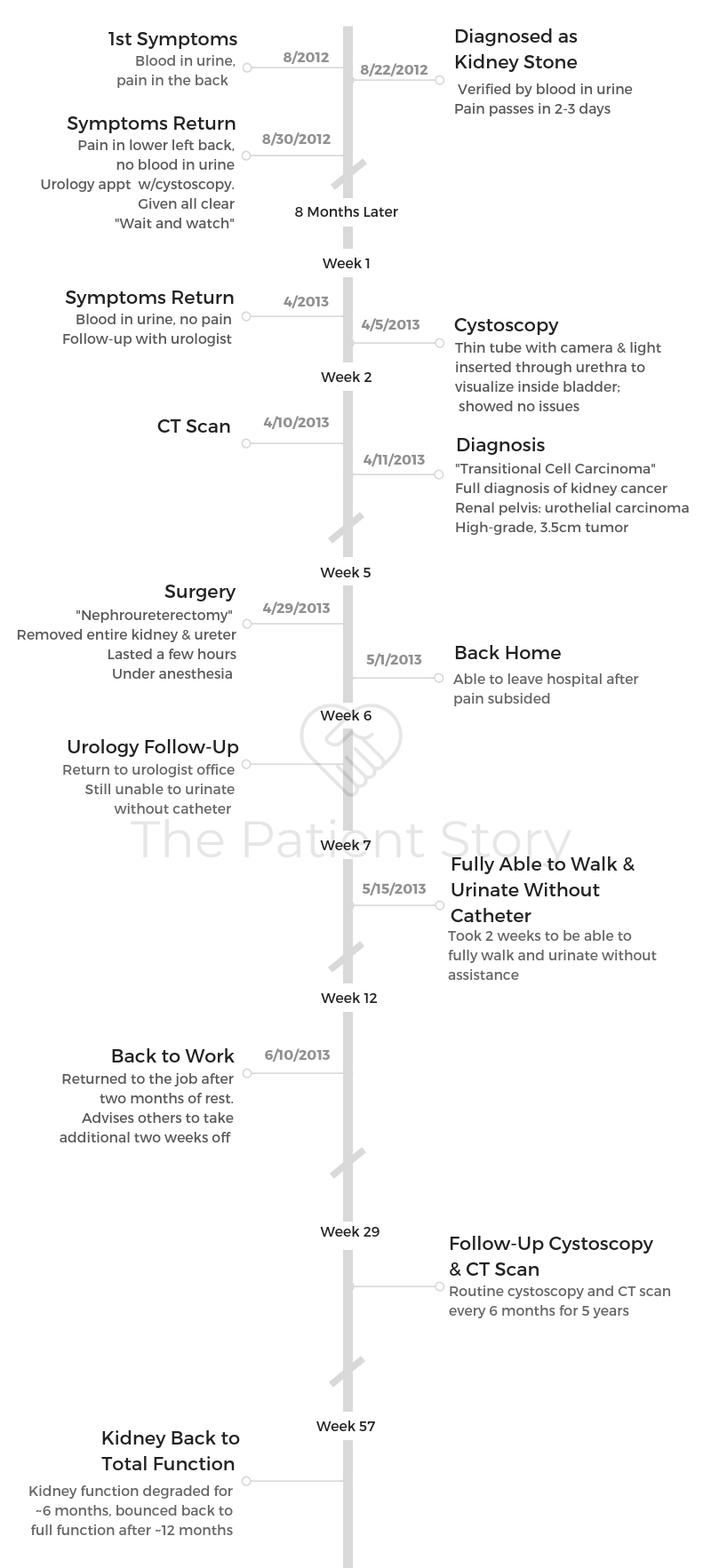
In February of 2013, I thought I had kidney stones. It was the typical pains in exactly the same place it would’ve hurt if I had had kidney stones. Lie on the floor crying in the fetal position pain and blood in the urine.
How did you get diagnosed?
I talked to friends who had kidney stones and they said my first symptoms were typical. I talked to my doctor. He said, “Yeah, it’s typical. We’ll look to see if it passes.” Well, nothing passed; I never got a stone.
The blood stopped. I started feeling great. Didn’t think anything of it. About a week and a half later or 2 weeks later, I saw more blood in my urine.
I thought that was weird. I called again. They said, “It’s probably nothing, probably just residual from the original stone. But why don’t we go in and have it checked?”
I went in and had an initial screen, a cystoscopy, which is where they check your bladder just to see if something is wrong. There wasn’t anything there. They said, “Just in case, why don’t we schedule you for a CT scan.”
I said okay, but it was going to take a couple of weeks. We got it scheduled, and I went in the afternoon. I decided to take a business meeting late in the day.
I was getting ready to go into the meeting, and my phone went off. It said ‘You’ve got an appointment with your urologist.’ I almost clicked ignore.
I almost stayed and went to the meeting, but I said I haven’t really put enough emphasis on my life in the last 4 years. I was at a start-up at the time.
I said I’d cancel the meeting and go to my appointment. I went in, got my scan, met with my urologist. He said, “Again, I don’t think it’s anything, but if it is, I’ll let you know.” So I went home.
When did you get the scan results?
Within 40 minutes of hitting the door, I get a call from my urologist. I said, “Gee, you know, Craig, you don’t call when things are going really well, do you?” He said, “No, I have to tell you, we found something that really has to be looked at.”
I said, “What do you think it is?” He said it looked like it was a tumor, so we decided to go forward and meet with an oncologist and start consulting.
The point of the story is because I was so focused on work, I almost clicked ignore on the reminder and stayed there for a meeting.
Never again. That was the last time I ever put anything for my family or my personal life or my health off for a meeting. It’s a hell of a story.
We might not be having this conversation if I had done that.
How long was it between the symptoms and diagnosis?
It was less than a month. I’m sure it was in February of 2013 when I started feeling pains and noticed it. It was in mid-March I was diagnosed, when I finally went in and had a meeting with my team.
Describe the first phone call from your doctor
I was at the dining room table, and my wife was there. I said, “Hey, guess what, I think I have something I’ll have looked at even further.” At that moment, I probably flushed and was a little worried, but I didn’t think too much about it.
I don’t think they diagnosed it as cancer yet. They had said it was a tumor. I knew there was some work we had to do.

How did you break the news to your wife?
As soon as I told my wife and we got a little conversation started there, my daughter walked home from school. She came into the house. She walked upstairs to the dining room. I saw her walk in, and I thought, “Huh, what in the world am I going to do here?”
She was pretty astute. She actually looked at us and said, “Something’s going on. What’s happening?” She was probably 15 or 16 at the time, so I thought, “Well, I can tell her what’s going on, or I can try to hide it.” I decided to let her know. I did that. I let her know.
»MORE: Breaking the news of a diagnosis to loved ones
How did you approach telling your daughter?
I wanted to be straightforward, even as I described it. I think I tried to concentrate on that, being straightforward.
If you have kids, you surely realize by now that you can’t bluff. You think you’re kidding them, but you’re not. They’re really astute people. They get more astute as they get older.
I just concentrated on saying, “Look, here’s what happened. I was diagnosed with this. This is the scan; here’s what it looks like. It looks like it’s cancer. I’m going to go in and talk to my doctor. The doctor’s called an oncologist; they specialize in cancer. He happens to be a surgical oncologist, so we’re fairly confident he’s going to be able to take care of things. I don’t know anymore than that right now, but do you have any questions?”
She said, “No, okay, got it. What’s for dinner?”
Then through the whole process, as soon as I got the final diagnosis, I told her and said, “Here’s the timing.” She was in school, we didn’t take her out of school, we let her go to school and be as normal as possible in that regard.
At that age and older — she’s 15, so in some ways there’s an adult perspective. Not a lot, but a little bit of adult perspective. I think for me, it was about being straightforward and showing not to be afraid of it. The way you impact the outcome is to do the things that the people who know what they’re talking about tell you to do.
Have a decent attitude about it. Do all the things you can to keep yourself moving and toward some kind of decent conclusion. That’s all I concentrated on. Once she had a question, I’d answer it. If I didn’t have an answer, I’d tell her so.
I think I did show her some of the wounds. Not all, because I was shaved from my neck to my knees practically. That was weird for me. Maybe not for all, but it was for me. I talked to her about that. I let her ask questions about it, this tiny little thing. I shared everything that was in the diagnosis.
I said, “I’m lucky. Here’s why I’m lucky. I did blow off a meeting. I did go to see the doctor. I did act on this. It was tiny. If I hadn’t acted on it, the next time I would’ve known, it would have been the size of a football. I would have had big problems and probably not recovered, so act on things when you can, honey.”
»MORE: Parents describe how they handled cancer with their kids
Telling your work about the diagnosis
The toughest time was when I called my boss and told her I had this diagnosis. I actually broke down a little bit emotionally. Mostly because I think I realized that my life being defined by work was over. A little bit of sense of loss there.
I think it was also a sense that my mortality was there. I was in my office at home. There wasn’t anybody around me, so I didn’t have to worry about how my daughter or my wife would see me reacting to this.
I actually broke down and cried when I talked to her, when I passed on the information and the news. For some reason, that most emotional part was the hardest.
»MORE: Read more on how others dealt with work after a cancer diagnosis

Path to Treatment
How long did it take to get the appointment with the oncologist?
Within a week, I was in with my oncologist. Because of the specific kind of cancer, it was one of those where they know how to treat it. There weren’t a whole lot of options. Chemo, you could do., but there weren’t a ton of options.
I think it could have also been a fluke in schedule, but I think them all being in one hospital probably helped quite a bit. They knew each other.
As soon as they found out I was going to this particular oncologist, my primary care physician called and said, “This is going to be great. I know Max; he’s a fantastic guy. You’re going to be fine.” I think all of that helped, too.
Describe your first meeting with the oncologist
I guess I wasn’t nervous. I didn’t feel nervous. Everybody has trepidation when they finally figure out what the heck is this really. I’m not a dummy. I realize that they wouldn’t have me meet an oncologist if they weren’t pretty sure that was the diagnosis.
My wife went with me. She was there with me during the whole conversation. That helped. Sat down, and he brought up the scans. He said, “This is what we’re talking about.” He showed me where on the kidney it was located.
Then he presented the treatment options. Chemotherapy didn’t really work with this particular type of cancer. He said they could go in try to laser it out, but that was really, really not good because he’d probably miss something.
He offered to do partial nephrectomy, but added that it never worked in his experience [and] that it always recurred in the kidney. Then he said they could pursue the removal of the kidney, so we just talked through that.
I don’t know how long that conversation was. It wasn’t hours; it was probably 45 minutes. It was a very straightforward conversation. I don’t want to say it was businesslike, but it was.
He was so straightforward, and he was not fooling around about it. He wasn’t beating around the bush; he wasn’t trying to blow smoke up my skirt to tell me everything’s going to be fine. He said, “Look, here’s what we have to do if you want to have a successful outcome.”
Did he talk about your prognosis?
He said, “If we remove the kidney and remove the ureter, your survival rate is almost normal.” Whatever normal is. Long-term, we’re all gone, right?
But he said, “You’ll have a dip in kidney function for a period of time: 12, 18 months. Your other kidney will take over the function.” My kidney function isn’t 100%, but it’s probably around 85% or 90% now.
How did you choose which hospital to go to?
In truth, I’ve been there a couple times before. I had already had a heart attack and been treated there. I also had an appendectomy there.
All of our family physicians have been through the UCSF system and healthcare. It’s around the corner from our house. It’s convenient, and we trust them.

What did you like about being at a bigger hospital?
I think that one of the things that gave me a huge amount of confidence was I was being treated by these young people. Max is probably 15 years younger than me.
These people who were just committed to just fixing and understanding and learning and solving problems and not letting go of problems until they had as good a solution as they could. Totally confident. Total confidence the whole time.
As a matter of fact, once I got my diagnosis, I knew, ‘Okay, I have to get this done, this done.’ I treated it kind of blasé. I was reacting to it much less than the world around me.
Surgery and Side Effects
What was your doctor’s recommendation on treatment?
Surgery. Taking out the kidney and ureter. No chemo, no radiation.
Describe the preparation before surgery
There was general anesthetic, so I had to fast. There were so many other things at the time I was thinking about, like being away from my family for a couple days.
I didn’t like the idea of going under. That’s never a good thing. I felt it every time I’d been to a hospital; they took a little bit of me out.
How long was the surgery?
A few hours. I was out. I knew that when I woke up, it was dark. I went in around 10 or 11 in the morning. When I woke up, it was dark. That means it could have been a 4- to 5-hour surgery.

How did your doctor describe the surgery process?
I met with the whole surgical team. There was a pre-meeting before I went in for surgery. I remember meeting all the people on the surgery team.
I met Max, who’s the surgeon. I met his team. He’s got a specific team he works with, 3 to 4 people. It was really interesting, really cool.
They talked about the surgery. They said, “Here’s what’s going to happen.” That’s why I know how it worked.
They didn’t open me up. They did laparoscopic surgery, where they put 3 holes in my abdomen. There was a 2.5- or 3-inch slit cut between my belly button and my groin.
What they do is essentially blow you up with nitrogen, I think because it’s not flammable. They inflate your body cavity, and then another tube has a light and a probe.
The other one is the tool itself that they use to go in. They essentially went up and wrapped this thing in some kind of pillow, encased it, then cinched it down, and pulled the kidney out.
What happened after surgery?
After the surgery, there was a treatment of my bladder. Because of the way the kidney and the ureter and the bladder are connected, there was a chance that a [cancer] cell had broken free and may have started a colony.
Most likely place would have been in the ureter or bladder. I think they used a very heavy antibiotic treatment. For some reason, that’s what they used for the bladder.
A day or so after I came out of surgery, they actually put a strong antibiotic into my bladder. I had a catheter at the time, so they just injected it through the catheter up the bladder. By the way, it’s not the most pleasant experience.
Describe the catheter experience after surgery
The first time they put a catheter in me, it was while I was under anesthesia. I didn’t know that, but afterwards, you can’t leave [the hospital] until you can pee. You have to pee on your own, or they won’t let you out.
Your urethra doesn’t like a tube going in the wrong way, which is not pleasant. It doesn’t really like when a tube is taken out then, so it takes a while before you can pee on your own. They took the catheter out, and of course I couldn’t pee.
Then they had to put another one in, so I had to stay in the hospital for a couple days while they waited to see if I could pee. I got cathed again and went home. I can talk about the experience because I had a cystoscopy twice a year after that, which is using the scope to go up the same route to check out your bladder.
Cathing is mostly just unpleasant.
First of all, you’ve got all these strangers playing with your peep. It’s a little weird, but fortunately I was at an age where I was really comfortable. You get more comfortable in your own skin as you get older, and I think that helped a little bit. You realize this is all a treatment thing. Nevertheless, it’s a little weird having people monkeying around with your private parts.
I don’t remember the first catheters. The second one, I think I had a frustrated physician’s assistant who was really, really trying to get through the process. She was a little frustrated, so that was a little painful.
As I recall, I had cystoscopy, too. There’s a bend in the man’s internal anatomy where your urethra goes in, and somehow it goes up into your bladder, which is where they put the catheter in. It’s a little painful. There’s a little discomfort when they go around the corner there. The rest of it’s just weird, but that actually can hurt a little bit. She was a little rough putting it in.
They used lidocaine, and there’s a little device that allegedly numbs the pain internally. They squirt it into your urethra. It works mostly.
It’s a one-way street, and they’re going the wrong way. No matter if it’s fluids or tubes or something, your body just is not built for that.
I have to say that with the exception of the one frustrated physician’s assistant who’s working on me, I know they were as gentle as they could possibly be. I never felt a lot of pain inflicted on me.
I knew there was going to be stuff from the surgery. Took awhile for the surgery to stop hurting.

Post-surgery side effects
I felt a little pain, but mostly from my diaphragm. The wound itself hurt a little bit. It took a while to get over.
I went home, and I think I got oxycodone or something like that. I don’t remember because I don’t take the stuff. I took it for about 2 to 3 days, and I didn’t like the effects it had on my emotions.
It was just totally unacceptable. I got a little cranky, irritable. I thought this isn’t me, so I figured after a couple of days, I would just take ibuprofen if I had any significant pain. It wasn’t horrible. I had trouble sleeping, so I actually sat up in a comfortable chair in my living room for 2 days.
We live in a house where you have to navigate stairs. I think I did navigate the stairs. That was something I tried to do was get in as much movement as possible while I was recovering from the wound itself and from the surgery.
Pain was a little bit. I think relief — if that’s a side effect. We got this done. Nobody has 100% prognosis, but it was as close as you could get to it in a lot of ways.
I had a clear plan for follow-up. I had my family, my friends, [and] people stopped in. I had more people stop in to see me over the first 2 weeks while I was in the hospital than I can ever remember almost being in the house.
No other side effects. The pain, as soon as I could pee again, was the last of the effects from the surgery except for the healing of the wound. That takes a while. It’s a pretty major incision.
I don’t know how long it took me to get over the anesthetic. That’s always one of those weird things where it takes a while. Most of its off-gasses is in a couple of days, but there’s all this weird follow-on and takes a while for everything to go out in your system.
I had a change in my taste. I have a friend who’s a vintner. Before I went into surgery, I was drinking quite an amount of wine, good wine he had. I liked it quite a bit.
After surgery, I couldn’t drink it. Wine tasted like vinegar to me. But on a happy note, one of the side effects was I actually developed a taste for bourbon and scotch, which I was never able to drink before.
Except for a little bit of pain, healing of the wound, and the resettling of things in my body. There’s a weird little pouch, and I always joke that’s where they put all the leftover stuff, like when they got done they just pushed it down. There’s a little pouch, not really a pouch, an area down below my belt line here that puffs out a little bit.
Surgery Recovery
Reflections on surgical recovery
Most of the time was letting the wound heal and to get over the trauma. There was a lot that happened inside that you didn’t see.
I didn’t lose very much blood. I don’t think I lost a pint of blood during the whole surgery, which is, again, the advantage to the [laparoscopic surgery].
They went in and yanked out a kidney and pulled it through your internal body cavity. They made an incision. They inflated you. They did all these things, so it takes a while for your body to get over that trauma.
How long was recovery?
I was more tired than I thought I’d be. In retrospect, I probably went back to work a little early. I’ve become so much better at work-life balance, and even there, I felt like I had to get back.
I think it was a mistake. I wish I had taken another 2 to 4 weeks off. Not because I didn’t want to work, but I really felt I went back a little too early. I wasn’t quite ready to be back. I think it doesn’t do anybody any good.
I was pretty well recovered by that time, but I think it slowed down the ending stages of my recovery. I probably didn’t perform as well as I could at work, which was not good for anybody.
Don’t rush. There’s nothing more important than getting well.
There’s nothing more important than making sure your family knows you’re fine. My wife, Susan, was worried that I was going back to work. I think that was unfair of me to put that on her.
When could you fully walk again?
Probably within 6 to 7 hours after surgery, I was actually moving. I think I was able to take a walk within about 5 or 6 days. But I really, really pushed myself to do that. That was one of the things I really wanted to start doing, was to get mobile.
To really walk, that was probably a couple of weeks. I remember the first time I made a full city block. I was able to do that and get home. Then I remember the first time I could walk a hill, because we live in San Francisco.
I remember the first time I could walk a hill up and down without being winded. It wasn’t pain for me; it was being winded and the body recovering from the trauma.

How long was it before you could urinate on your own?
I was actually challenged by that. It took a while. I was at home and had a pee bag for awhile. Urine has to go somewhere. You have a catheter, and it comes out and goes into this little bag.
I went in to see the office 3 to 4 days after I got home. They said, “Can you pee?” I said, “I don’t know.” So they took the catheter out and had me try to pee. I couldn’t, so they had to put another catheter in.
It was probably a full week after surgery before I was able to [urinate on my own].
Everybody does, and it hurts like hell the first time you pee. You’re always worried — at least I was. I was thinking, “Please don’t put another catheter in. Please, please, whoever’s listening to me, let me pee here because I just can’t go through this again.”
It’s like performance anxiety. I’m not young, I’ve been around a lot, and I know a lot about medicine. I’m not a doctor, but I know a lot about medicine.
I know how people recover. I knew I would pee. I just knew it. I knew I would, and I would not live the rest of my life with a catheter. I just knew it wouldn’t happen.
But it was just the frustration of, “Oh, come on, this is holding me back from doing things like being really mobile.” Even though I was in no shape to really walk for a full week to really get out of the house, but it was one of those like, “Come on, for goodness sakes.” It’s not pleasant to have this bag you have to empty. It was just the frustration more than anything.
It wasn’t pain; it was frustration of being able to get on with recovery.
Quality of Life
Advocating for yourself during your cancer experience
Before the kidney surgery, the anesthesia team comes in and looks at you. They find all kinds of reasons not to do it. They say, “We can’t do it for another 6 months because you had grapefruit 10 days ago,” or something.
They tried to stop it. They said, “Well, he had aspirin within the last month.” I said, “Yeah, it’s per my regimen for my cardiovascular disease.” I was scheduled on a Monday.
I actually had to say, ‘No, here’s what we’re going to do.’
“You’re going to call, you’re going to talk to my oncologist, and we’re going to get this settled right now because I am not going to reschedule surgery. I’m going to get this taken care of. See if it’s okay.”
In fact, they did. They said, “Okay, all right,” grudgingly.
I think it was a little easier. I said earlier that I was really impressed by the fact that we have all these really young smart people just totally dedicated to the field who are helping to solve these problems. That’s inspiring.
The thing is you can go full dad on them. When you say, “No, here’s what we’re going to do: you’re going to get on the phone and call,” they actually do it.
I did have to advocate for myself. That was the only point where I felt I had to. I had a great meeting with my surgeon, I had a great meeting with everybody who’s going to care for me, the plan went totally forward.
»MORE: How to be a self-advocate as a patient
Did you and your caregiver (spouse) have different styles in approaching treatment
My wife is generally more the question asker. In this case, I really wanted to know. I thought part of dealing with this is understanding 100% what we’re going to do and really asking all the questions about the prep and the surgery, the treatment afterwards.
What’s the prognosis and how long will I be in?
How long will it take me to recover from the surgery?
What’s the follow-up?
It was kind of out of character of me in that particular situation to ask all those questions. She was always there. Part of it was I knew she’d be asking the questions if I didn’t so I thought I’ll give it a shot. If I missed something I knew she would get it.
How long were you gone from work
Six or eight weeks, I don’t remember exactly. It was a couple of months. Call it two months.
I think I went back into the office once, only because they were all so worried about me that I wanted them to see that I was moving and alive and was going to actually come through this and come back. My CEO was happy to see me and my SVP of Engineering was happy to see me. It wasn’t a long trip.
Part of it was I wasn’t allowed to drive. You have to wait for a certain amount of recovery to drive a car. I was working in Mountain View at the time.
I didn’t know if I had the stamina to take a ride so my wife drove me down. I toddled up the stairs and said hi to everybody and was totally exhausted and had to toddle back down the stairs and go home.
How important is it to have caregivers
Of course it’s important. We actually talked about it after this event. Having a partner – all the other parts are important. You love somebody, you’re with them, something to do, somebody to do something with.
When you have an event like this, having a relationship with somebody who – if you need something they can help you get it, if you need.
I didn’t have any emotional reaction afterwards really. Many people might. The support that was there. I didn’t need a whole lot. I really wanted to move on my own. A lot of it was it’s time to take a walk. I tried everyday I tried to walk a little further. Things like that. I was able to bathe myself.
That’s probably why I felt a little bit blasé or less than totally freaked out by the procedure because I could take care of myself. The incision, relative to what happened, there was all this plastic bandage, two by four, covered my whole incision. Then they had these plastic bandaids over the three holes.
It’s like I come out of major surgery and that’s all you see, it doesn’t look that impressive. My daughter, it was great to have her there. We spent a lot of time talking because I couldn’t get up and move a lot. We talked a lot.
Did you have help with figuring out work and taking time off
I had a great team. I was in HR so I just went to my leaves team and it was interesting. The person who helped me solve my leave concerns had a kidney diagnosis too so we actually talked about our respective diagnoses. She was very good.
They set it up and it was totally seamless. Except for the fact that I got a second check from the state, I wouldn’t have known I was on disability. Everything was just so smooth.
That now bothers me. It bothers me because there aren’t a lot of people in this world who can say that. There’s a lot of people that, first of all, the diagnosis I had would be a death sentence. They would not have gotten a diagnosis, they would have died and not known what was going on.
But if they did get the diagnosis, they don’t have access to the care. If they do have access to the care, it’s a death sentence for the finances. Now it bothers me.
I’m grateful, eternally grateful I was born in a place and time and in circumstances where my insurance took care of me. I had very good advocates on my leaves side. I had fantastic advocates that worked to cover for me while I wasn’t there. My home, my friends. Now I’m so grateful.
What were the most emotional moments
I think you always have vulnerable moments. There’s the realization of the mortality is a thing.
I never felt worried I guess. Blasé may be the wrong word. I didn’t feel freaked out by it. I felt okay, we’ve got a course of action. The results will be the results. Really can’t do much about that.
Part of my inner-dialogue as I recall was I saw it as an opportunity to demonstrate for my daughter how to handle something like this. I didn’t feel like freaking out so I didn’t want to freak out in front of her.
I wanted her to see hey you can do something like this with grace and aplomb, accepting the facts that are there, putting a plan together and moving forward.
I think once in awhile I had that. The only time I had something that was memorable was when I woke up in the recovery room. I remember looking up and thinking okay, wow, I’m not dead, this is really good, right? If you’ve had a life-threatening illness or an event like this, you start thinking wow, second chance. That part made it a lot easier for me.
Advice to those who’ve been diagnosed
I grew up in a small town in Ohio with a bunch of coal miners and steel workers, kind of a macho ethic – just work through it. I probably fell prey to that early on in my life.
This time I didn’t. It was a little surprising when I go back and think about it I didn’t just say oh okay, it’s just a little painful but I’ll get over it.
Listen to your body and make time for that. It’s very important.
Again, there’s a few things in life that I won’t describe here that sometimes jar me awake at night. This will jar me awake at night only because what would have happened if I had been dumb and had gone to this meeting that was inconsequential because I’m not even at that company anymore.
What would have happened if I hadn’t a paid attention to the fact that I had a little bit of blood in my urine the second time?
There’s so many different kinds of kidney cancer. On all these things I think I tell people listen to your body. If I had listened to my head I wouldn’t have done anything.

Inspired by Kevin's story?
Share your story, too!
No post found
3 replies on “Kevin’s Invasive Transitional Cell Carcinoma Kidney Cancer Story”
Inspiring story ! 10 years passed. When did this interview with Kevin take place ? Does Kevin live well now ?
Would Kevin mind sharing the hospital and doctors? We live in NC and my husband was just diagnosed Wednesday and today he has biopsy of kidney , bladder, and ureter. Found 2 small tumors in the kidney and more in the tube. Scheduled for a PET scan on the 28th and a visit to an oncologist shortly after. They are already saying chemo! In Kevin’s story he was told chemo don’t work for this type! I am demanding a second opinion no matter what but all the urologist and doctors around here all push one certain oncologist! “ he’s the best in the area “ well we DON’ T have to stay in the area! I am willing to travel out of state! As long as my husband gets the best care from a doctor that knows what he is doing and knows this type of cancer! I have never dealt with cancer and I won’t lie I’m terrified! The first day when we received the news all I could do was cry. Day 2 I was angry at anything and anyone! On day 2 he had gone to work to let the important ones know the situation And got the call that urologist could see him at 215. Things started moving quickly after the day of the diagnosis seemed to not move at all! It took me half my life to find him and we have only had 17 years and it’s not near enough! Please help me. I have so many questions and these doctors speak to me like I’m stupid and I should know all these medical terms they throw at me!
Hi Mandy, first, we are so sorry to hear about the diagnosis. Kevin indicated in his interview he went to UCSF (Univ. of California, San Francisco), but did not name an oncologist. Our patients relay what they went through, but we do encourage people to check first and foremost with medical professionals on what courses of action are best for the patient. On that note, our community definitely encourages second opinions. Best of luck to you and your family.