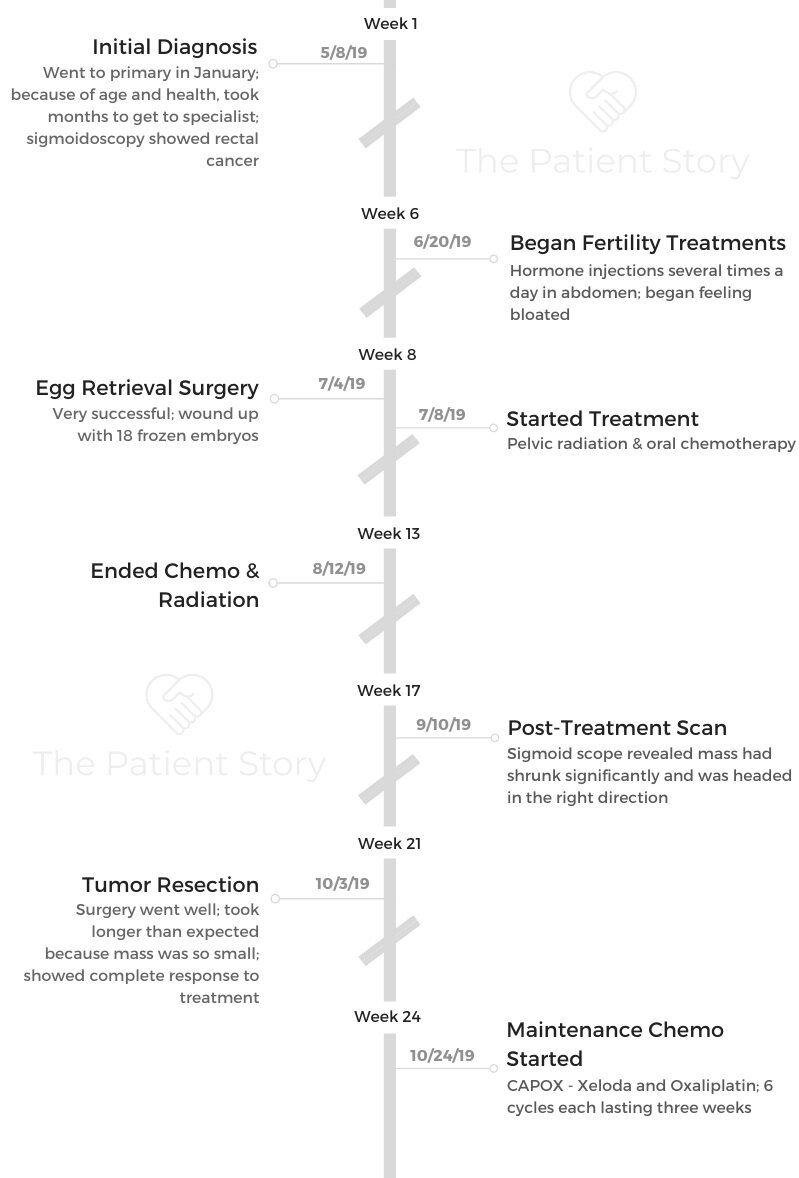
Catherine’s Stage 3 Adenocarcinoma Rectal Cancer Story

Catherine shares her stage 3 rectal cancer story and having to make the gut-wrenching decision to terminate a pregnancy before treatment. She details undergoing fertility preservation treatments, radiation, chemotherapy, surgery, and maintenance chemotherapy.
In her story, Catherine also highlights important quality-of-life issues, including what support was most helpful, the impact of her rectal cancer on her marriage, and the decision to stop working.
- Name: Catherine P.
- Diagnosis:
- Rectal cancer
- Adenocarcinoma
- Staging: 3
- 1st Symptoms:
- Rectal bleeding
- Constipation
- Bloating
- Treatment:
- Fertility treatments
- Successful egg retrieval surgery
- Radiation
- Targeted to pelvis
- Once every week day for a total of 25 sessions
- Chemotherapy
- Xeloda
- Taken orally twice a day for 5 weeks
- CAPOX (Xeloda & oxaliplatin)
- 6 cycles, each lasting 3 weeks
- Oxaliplatin infused on day 1
- 2 weeks of Xeloda orally
- 1 week off
- 6 cycles, each lasting 3 weeks
- Xeloda
- Surgery
- Tumor resection
- Fertility treatments
- Tests & Diagnosis
- Pregnancy & Fertility
- Radiation & Chemo
- Surgery & Maintenance
- Can you talk about the surgery prep?
- How did the surgery go?
- Were you in pain after waking up from surgery?
- How was recovery from surgery?
- Have you adjusted to your ileostomy?
- What’s your advice for someone who’s about to get an ileostomy?
- What’s your maintenance chemo regimen now?
- Are you experience side effects from the maintenance chemo?
- Did your doctor tell you you’re NED?
- Support & Emotions
- What were some ways people were able to support you?
- How has the experience affected your relationship with your husband?
- Do you have any advice for other couples?
- Did you quit working?
- How is the financial aspect of treatment?
- How has cancer changed your perspective on life?
- What is your advice for someone who has just been diagnosed?
This interview has been edited for clarity. This is not medical advice. Please consult with your healthcare provider for treatment decisions.

I know what it’s like to be in that vulnerable position in the beginning when you don’t know what to expect. Reach out to me and other survivors.
We’re here for you. I wish you didn’t have to, and I wish this didn’t happen to you, but you’re not alone, so reach out. We’re all fighting this together.
Catherine P.
Tests & Diagnosis
What were your first symptoms?
In January of 2019, I started getting some rectal bleeding. I went to the doctor, and they said it was probably internal hemorrhoids. They gave me some medication for that and sent me home.
After about a week of that with no relief, she said they would send me for a scope. Because I was young and healthy, she said it would probably take me a while to get in.
I finally got my appointment, and it wasn’t until May 8th. From January until May, the symptoms just got worse. I had some extreme bloating and trouble going to the bathroom. It was persistent right up until the scope when they diagnosed me.
They did a sigmoidoscopy. That goes in to the sigmoid colon. They decided to do that instead of a colonoscopy because of where my doctor thought the problem might be.

I was nervous about it just because I knew something was wrong with my body. I was nervous to find out what it was.
I was excited to get the testing and things out of the way and find out I had Crohn’s or IBS or something and move on. I was 10 weeks pregnant at the time, so I just wanted to get everything over with.
How did you get the diagnosis?
The sigmoidoscopy only took 15 minutes. When she first went in, she mentioned all the risks. I was pregnant, so I had to sign some extra papers. I was like, “It’s okay. Just do it.”
You’re laying there, and of course, you can look at the screen. I’ve never seen the inside of a colon before, but I saw something pretty ugly. I didn’t know what I was looking at, but I knew it didn’t look good. She was taking a lot of pictures and took a biopsy. I got a bad feeling.
When she was done, she was shocked because I was so young. She said, “Okay. I’m just going to take a few notes, and we’ll have a chat after.” She wanted to go somewhere more comfortable.
The nurse said, ‘Did you want your husband to come down for this chat?’
I said, ‘No, that’s okay.”
She said, ‘No, I think he should come down here.’ At that point, I just knew.
The doctor sat us down and said, ‘There’s no easy way to say this, but you have rectal cancer.’
How did you react to the diagnosis?
I was really in shock. I didn’t know what to do. My first thought was, “Do people survive this? Am I dying?” My husband felt more of the emotion in that moment.
We were supposed to go to my mother-in-law’s house for her birthday that night, but we just came home. I was still in shock for a long time. I don’t know how I made it through those days without knowing if it had spread to any other organs.
I didn’t know anything, so I think I remained in shock for a few weeks. That’s probably how I made it through waiting for test results.
»MORE: Patients share how they processed a cancer diagnosis
What was the next step after diagnosis?
I had to wait to find out what stage it was. I had to have a CT, MRI, biopsy results, and a colonoscopy. Typically, they’d wait for the biopsy to come back before giving the initial diagnosis, but my doctor was confident it was cancer.
I had to go to a surgeon who set me up with the other tests to fully diagnose and stage it. It was stage 3 because it hadn’t spread, but it had gone to lymph nodes.
Pregnancy & Fertility
You had to terminate your pregnancy before treatment
Before I started chemo and radiation, we had to terminate my pregnancy. We also went through fertility treatments before starting other treatment. Termination was and still is the hardest part.
When I had the sigmoidoscopy, my doctor said, “Sometimes, if it’s an early stage, they can just go in and cut it out, and you can keep the pregnancy.”
As we started finding out more from the CT and MRI, it became clear that I’d need chemotherapy and probably radiation.
At that point, some doctors were saying, ‘Don’t be so quick to think you need to terminate. Chemotherapy can sometimes be safe.’
The idea of chemo and a pregnancy just didn’t sit well with me.
There are certain studies that say it’s okay in the second trimester, but it wasn’t something I would’ve gone for. When they said I needed radiation, though, that’s radiating the whole pelvic region. That’s when I absolutely had to terminate.
My husband was very supportive. He said, “You’re here. We need you.” I couldn’t hold off on treatment long enough to have the baby, so we decided to go through with termination.
Can you talk about the fertility treatments?
Looking back and having gone through everything else, it probably wasn’t actually that hard, but it was the first step I had taken towards getting better.
At the time, I thought it was so hard. Now that I’ve gone through chemo, radiation, and surgery, it doesn’t seem that hard to me.
I had to get 2 to 4 injections in my abdomen each day. I got super bloated because I was harvesting all these eggs. I did that for about 2 weeks. Then they went in and retrieved the eggs.
The egg retrieval was not a fun process. It was not comfortable, but they got 32 eggs out or something crazy.
No wonder I was so bloated. We ended up with 18 frozen embryos. It’s still uncertain if I’ll be able to carry or not, but at least we have them.

Did you get a break between fertility treatments and radiation?
I had my egg retrieval on Thursday, and I started radiation on Monday. I didn’t feel fully recovered, but my oncologists were really pressuring my fertility doctor. There’s some sickness you can get called ovarian hyperstimulation syndrome after fertility treatment.
My oncologists were very on top of things, trying to make sure I didn’t get OHSS, because I needed to start treatment right away.
I was super bloated for a long time after the fertility treatments. Starting treatment right away didn’t give me enough time to mentally or physically recover, but I had to start immediately.
»MORE: Read a patient’s detailed IVF journal
Radiation & Chemo
What was your radiation schedule like?
I went every day for 5 weeks minus weekends, so it was 25 sessions. I did chemo at the same time. The radiation was targeted to the mass itself, but it got everything it passed through.
It zapped the lymph nodes at the same time. It went through my bladder, my uterus, bladder, ovaries, and it’s getting everything.
What was your chemo regimen?
I started chemo and radiation on the same day, July 8th. It was oral chemo, so it made it a little easier.
The reasoning behind doing chemotherapy at the same time is it makes you more sensitive to the radiation, so I took Xeloda twice a day every day for those same 5 weeks.
Describe the treatment side effects
I think the side effects I had were mostly from radiation. I physically tolerated it really well, but towards the end I got extreme fatigue and diarrhea.
It was in the summer. We went on a weekend getaway, but I refused to get on the boat.
The fatigue was hard because I’ve never experienced something like that before. I just needed to lay down a lot.
Otherwise, physically, I handled it really well. I had a small burn on my tailbone, but that was manageable. It healed really well.
I filled a prescription for whatever it was they recommended, but it really just healed on its own. It felt more like a sunburn than anything else.
When was your next scan after treatment ended?
I finished chemo and radiation on August 12th, and my next scan was on September 10th. I had to wait a while because the radiation continues to work on your body after you’re done, so there was no point in scanning before it was done.
One of the hardest parts of going through radiation was not knowing if it was working. You’re going and getting zapped every day without even knowing if it’s doing anything, and you have to wait until a few weeks after to know.
I had an MRI on September 10th, and I had another sigmoidoscopy, which showed it had shrunk significantly. My surgeon went in and tattooed the area so she knew what she was looking at in surgery.
Surgery & Maintenance
Can you talk about the surgery prep?
The prep day was the worst because they give you all these pre-surgery antibiotics, but you’re already on an empty stomach the day before. I was throwing up the entire night before surgery.
It was hard not eating while I was so nervous. I was already so nervous, and then I was also uncomfortable because I was hungry and nauseous.
This was my first surgery ever, so I didn’t know what to expect. I didn’t know how things really worked. I was really nervous, but looking back, being put to sleep wasn’t so bad.
How did the surgery go?
It was supposed to be about 4 hours, but she took about 5.5, so of course my husband and family were freaking out. Actually, though, the surgery went really well.
The reason it took a bit longer was because it had shrunk so much that she wanted to make sure she got everything. She was so happy she tattooed the area, because it was almost impossible to find the mass and where everything was.
»MORE: Read more patient experiences with surgery
Were you in pain after waking up from surgery?
I had an epidural. I had a constant drip going in my spine. When I woke up, I was in the recovery room, and I couldn’t feel my legs.
They were numb, and I could barely move one of them. I told them I couldn’t feel my legs, and they told me it was normal.
When I went up to my room, I still couldn’t feel them. They called up an anesthesiologist. He didn’t like that I couldn’t feel my legs.
The nerve block was just supposed to be in my abdomen, so they had to turn off the epidural to make sure I didn’t have a bleed in my spinal cord.
Slowly, I started being able to feel my legs. They wound up taking the epidural out because the nerve block was just going too low. For the first day, I didn’t really have pain meds, but then I started Dilaudid, and that was okay.
The pain from surgery really wasn’t too bad. Mine is a bit muffled probably because I was so nauseous and sick. That’s all I was really focused on.

How was recovery from surgery?
The surgery itself went really well, but the aftermath was pretty terrible. I was supposed to be in the hospital for 5 days, but I was there for 2 weeks.
I developed ileus. It’s a combination of being put to sleep for so long that your bowels kind of go to sleep and being so bloated because I have an ileostomy, and nothing was moving downwards.
I was throwing up for days. They finally had to give me an NG (nasogastric) tube in the nose and down to the stomach to empty me out. I could hardly eat or move. I was so uncomfortable because I was so bloated. They didn’t let me go until I was starting to see some output from the ileostomy.
When I left the hospital, I was scared I was going to end up back there with a blockage. I left maybe a day or 2 premature. I just wanted to go home.
I stayed on a soup diet pretty much. Being home was so weird after that whole experience. After about a week, though, I started feeling more like myself.
Have you adjusted to your ileostomy?
At first, it was a huge adjustment. It wasn’t working. Then, one day, it just clicked and started working. It’s been great ever since.
I have a love-hate relationship with it because I know it’s necessary and something that’s essential in saving my life, but at the same time, it’s a pain in the butt.
It took a while to get used to changing it and everything. It was gross to me. It just wasn’t pretty. I’m used to it now. It’s all healed up, so that’s nice.
I’m on the waiting list to get it removed now. With my first surgery, it was a cancer surgery, so I immediately got put on the list. Ileostomy reversals are now considered an elective surgery in Canada, so I’m on a waiting list, which is fine because I’m still in treatment anyway.
I should end chemo in March if I don’t have any delays, and I need a month to recover after that. I’m probably looking at getting it out in May or June.

What’s your advice for someone who’s about to get an ileostomy?
There’s so many different kinds of bags you can use, so figuring out what’s best for you is a process.
Now, I can say I have a routine. No one would know I have it if they don’t know.
At first, it sucks and feels really bad. As things heal, it gets better. My biggest problem with mine was I hated the odor. It was different than a regular bowel movement.
I found these odor eliminating drops called M9 drops, and you can put them right in the bag. They make a world of difference.
If there are any issues or anything that makes you uncomfortable with it, talk to the ostomy nurses or go to the ostomy store, because there’s typically a solution.
You can still do everything you could do before. You can swim and go in hot tubs. You can do everything. It’s not limiting like you might think it is.
What’s your maintenance chemo regimen now?
My pathology from surgery was really good. I had a complete pathological response from the radiation and chemo I did. That means no lymph nodes and even the mass itself didn’t test positive for cancerous cells.
The chemo I’m on now isn’t to get rid of anything else. It’s just preventative. It’s just to make sure that any rogue cells are cleaned right out.
This regimen is CAPOX. It’s Xeloda and oxaliplatin. I did Xeloda before, so I wasn’t worried about that one. Oxaliplatin is the one I had heard nightmare stories about. I was really nervous for that one.
One cycle is 3 weeks, so I go on the first day for my oxaliplatin infusion, and I go home with 2 weeks of Xeloda pills. I have one week off, and then I start again. I’ve got 6 total cycles until March 2020.
Are you experience side effects from the maintenance chemo?
The major thing with oxaliplatin is major cold sensitivity. I didn’t really understand the cold sensitivity. I was like, “Okay, yeah. Sensitivity to cold, whatever.”
You can’t even reach into the fridge, breathe cold air, or anything. My hand tingles if it’s anywhere below room temperature. It’s like a sharp tingling, but it’s also sort of asleep. It happens to all your extremities. My nose, my hands, and my feet get it the worst.
The cold sensitivity lasts about 7 days after the infusion. Of course, this time of year, I’m always bundled up. I go out with a coat and hat, and I have to wear a scarf over my face.
I had these muscle cramps as well. My hands would just claw up and stay there. That was super weird. During the second round, I was still sitting in the chemo chair, and all my muscles tensed up like that.
I couldn’t even walk because the cramps were so bad. It subsided, thankfully, but we’re reducing the dosage for the next round and dripping it over a longer period of time.
Did your doctor tell you you’re NED?
When I was still in the hospital, the pathology came back, and my surgeon was on vacation. She called me, and I didn’t get the phone call. She left me a message and said she wanted to tell me the pathology was so great and that I had a complete response.
My reaction wasn’t what I expected. It was really hard to accept that. On May 8th when I was diagnosed, they turned my life upside down, and then in one phone call they said I had a complete response. I couldn’t accept it in my brain. I’m almost afraid to. When you accept it, it’s like, “What if it comes back?”
I don’t really focus on that part of it. I just focus on the fact that I’m still in treatment. I don’t even tell people I’m NED. Even though I had a complete response and there’s no cancer there, I just have a hard time accepting it. I’m just afraid to accept good news.
I think once I have my first scan after treatment ends, I’ll be able to believe it. I’ll probably have that scan at the beginning of the summer of 2020.
Support & Emotions
What were some ways people were able to support you?
My family is amazing. I couldn’t do it without them. My parents and my husband’s parents were amazing.
If for some reason my husband couldn’t make it to an appointment, I always had a ride. I never went to anything alone. They were always there for me.
The biggest thing has been people bringing food to my house. Cooking isn’t something that’s relaxing for me at all, so when I’m in treatment or post-surgery, cooking is not something I want to do.
Family and friends have just dropped food at my door. They just do it, and I don’t have to feel like I’m asking. It’s been great.
It’s hard for me to ask for help. I’ve always been very independent, so the fact that they just help without me having to ask is amazing.
I’ve learned to speak up about my limits. I’m very independent, but I’ve learned when I just can’t do something.
I’ll ask my husband for help, but I still don’t usually call or ask friends or family for help. They just do it. I don’t know how I would’ve done this by myself.
»MORE: What kind of support cancer patients say helped the most
How has the experience affected your relationship with your husband?
We’ve always been a very strong couple, so we’ve had the mindset that we’re gonna make anything work. We got married after 7 years, and since we committed to each other, that’s just the way it is.
It was hard going from expecting a baby to our whole world being flipped upside down, but we’re both very strong in our belief that we’re going to make it through anything.
If anything, I think the experience brought us closer together. We try to take lessons out of it. We try to enjoy each day. It’s stressful sometimes, but we make it work.
It’s hard sometimes because he’s a caretaker at heart. The hardest thing for him, I think, was coming to terms with the fact that he couldn’t fix this. Men like to fix things.
We just have to deal with heavy stuff, but it hasn’t really affected us negatively. We deal with what we have to deal with. It’s mostly heavy, but we deal with it together.

Do you have any advice for other couples?
Communication is important. Treatment is a long haul. It lasts more than a year in most cases.
You have to just tell them if you’re at your limit. Not every couple has that ability, but it’s something to think about and work on.
If I’m irritable or exhausted, I just say it. Immediately, he then understands.
There’s no guessing or walking around on eggshells not knowing. Same goes for him. He has to tell me things, too.
He sometimes has to tell me he’s worried. We’ll have that moment, talk about it, and move on because we have to. Communication is the number one thing, though, because you’re going through so much together, and so many emotions are flying around. There can’t be any guessing.
We’ve been going to counseling both individually and together as well, and I think that’s been helpful. I highly recommend it. We started right away.
»MORE: 3 Things To Remember If Your Spouse Is Diagnosed With Cancer
Did you quit working?
I’m an accountant. I worked hard for my career. I had just gotten a promotion around the time I started getting sick. When I was diagnosed, I thought, “How am I supposed to go to work?” My doctor wrote a note for 4 weeks off. I haven’t worked since then. It was a hard decision.
My job is hard to work part-time. Also, it’s hard for me to not give one thing my all. If I was working, I wouldn’t be giving it 100%, and I wouldn’t be giving getting better 100%. I took a leave, and my work has been super supportive. I still go and visit them.
Things may have been different if we didn’t have to deal with the pregnancy right away. That was so hard to accept. I sometimes wonder if I wasn’t dealing with that, if maybe work would’ve been a good distraction. I just took a leave and stuck with it.
»MORE: Working during cancer treatment
How is the financial aspect of treatment?
I was a super saver. I always save my money. The first few months, I was on medical leave through government programs. Now I’m on long-term benefits that I’ve been paying into through my work, never thinking I would need. Turns out I do need it, and it’s definitely a godsend.
For the first few months, it was tough. We bought our house based on both of our careers. We made it work for that first bit, and now I’m on long-term disability. We’re very lucky, and we know it.
How has cancer changed your perspective on life?
It’s slowed me down a lot. It totally changes your perspective. I’m happy to be here. I try to spin everything into a positive. Once you have cancer and have to find some way to spin that into a positive, it’s pretty easy to do that with just about anything.
I bought a juicer. I’m going to start juicing. There’s little things like that. I find myself slowing down and thinking about the bigger picture more. It’s easy to say now because I’m not working.
I wonder if when I start working again, I’ll get stuck into the daily grind again. I’m really hoping to keep this mentality of slowing down and enjoying each day when I do go back. That’s my goal.
What is your advice for someone who has just been diagnosed?
I always tell people to find others going through what you’re going through. I know what it’s like to be in that vulnerable position in the beginning when you don’t know what to expect. Reach out to me and other survivors. We’re here for you.
I wish you didn’t have to, and I wish this didn’t happen to you, but you’re not alone, so reach out. We’re all fighting this together.
Don’t overwhelm yourself with information gathering, but make sure you ask questions and pay attention at your appointments. Lean on people throughout the process as well.
I suggest being open and honest about what you’re going through, because there’s nothing to be ashamed about. It’s life. Everyone who fights cancer is a badass. It’s not easy. Be open, because the response and support you get is amazing.
There have been so many people who have reached out to me and wanted to help. The overwhelming support is incredible. You can reform connections because of this. It’s so cool.
Try to find the positives. Even with having an ileostomy bag, it sucks, but it’s life-saving. I can just laugh about it. It doesn’t have to be all bad.
Be positive, connect, be open, and accept support.

Inspired by Catherine's story?
Share your story, too!
Rectal Cancer Stories
Kalei M., Rectal Cancer, Stage 4 (Metastatic)
Symptoms: Presence of mucus and tissue-like substance and blood in stool, stomach cramping
Treatment: Radiation therapy, chemotherapy, surgeries (two lung resections)
Jessica A., Rectal Cancer, Stage 4 (Metastatic)
Symptoms: Changes in bowel movements, blood in stool, abdominal pain, back pain, difficulty sitting comfortably, constipation, feeling of incomplete evacuation (as if some stool remained after bowel movements), mucus-like stool consistency, bloating
Treatment: Immunotherapy under a clinical trial
Shiva S., Rectal Cancer, T2, and Renal Cancer, T3
Symptoms: Pressure and urgency of bowels, back pain
Treatments: Chemoradiation (for rectal cancer), surgery (ileostomy, combined bowel and kidney surgery), immunotherapy (for kidney cancer)
Jeanine B., Rectal Cancer, Stage 3 (T3bN0M0)
Symptoms: Long history of bleeding that was blamed on hemorrhoids, pain in the tailbone, urgent need to use the restroom, unusually narrow stools, presence of mucus in stools, fatigue
Treatments: Chemotherapy, radiation therapy
Devon B., Rectal Cancer, Stage 4
Symptoms: Pain when trying to move bowels, increased frequency of bowel movements alternating with periods of constipation, passing mucus instead of feces, narrow stools
Treatments: Surgery (ostomy surgery), radiation therapy, chemotherapy
James K., Rectal Cancer, Stage 3C/4
Symptoms: Occasional rectal bleeding, increasing fatigue
Treatments: Chemoradiation, surgeries (coloanal pull-through, temporary ileostomy, ileostomy reversal, permanent colostomy), adjuvant chemotherapy






2 replies on “Catherine’s Stage 3 Adenocarcinoma Rectal Cancer Story”
Hi,
I hope this message will go to Catherine P.
My wife was diagnosed with stage 3 rectal cancer in January this year. As her husband I have found dealing with this extremely hard as we are extremely close and I feel I need to be strong for her.
You have good and bad days and moments and last night was one of those bad moments.
Your story has really helped me and i wanted to let you know that so thank you for sharing your experience.
Cheers
Andrew
Andrew, thank you for your kind words and for sharing your own story. As we know, caregivers need so much care, themselves. I hope you have a support system that can provide what you need, as well.